Abstract
We report on a 13-yr-old boy with acrodysostosis, a review of 30 cases in the literature, and metacarpophalangeal pattern profile (MCPP) analysis. The prominent manifestations (present in >75% of cases) of this condition include nasal and maxillary hypoplasia, peripheral dysostosis, first ray hyperplasia of the foot, acromesomelic brachymelia, decreased interpedicular distance, advanced skeletal maturation and mental retardation. Results of chromosome studies have been normal. An autosomal dominant inheritance pattern was reported in two families. Maternal and paternal ages were 2 and 3 yr, respectively, above the average age of the general parent population, which suggests that advanced parental age may be a factor in the cause of this condition. A characteristically abnormal MCPP was found in our patient and in 16 additional cases studied from the literature. A mean MCPP was developed for the syndrome. MCPP analysis may be useful as a diagnostic tool in patients suspected to have acrodysostosis.
Keywords: acromesomelic brachymelia, first ray hyperplasia of the foot, maxillary hypoplasia, nasal hypoplasia, peripheral dysostosis, skeletal abnormalities
INTRODUCTION
Acrodysostosis is a rare syndrome of peripheral dysostosis, nasal hypoplasia, mental retardation and other skeletal abnormalities [Robinow et al., 1971]. This condition was first delineated in 1968 [Maroteaux and Malamut, 1968; Giedion, 1968a]. Since that time at least 30 cases have been reported [Singleton et al., 1960; Cohen and van Creveld, 1963; Ortolani and Cremonesi, 1963; Steinbach and Young, 1966; Arkless and Graham, 1967; Giedion, 1968b; Garces et al., 1969; Robinow et al., 1971; Ablow et al., 1977; Niikawa et al., 1978; Goodman, 1978; Reiter, 1978; Cerda et al., 1979;Undreineretal., 1981; Frey et al., 1982]. Here we report on a boy with acrodysostosis, and review the literature and development of the metacarpophalangeal pattern profile (MCPP) for the syndrome.
MATERIALS AND METHODS
Clinical Report
C.M. was a 2,185-g infant born at 36 wk of gestation to a 19-yr-old primagravida mother and 20-yr-old father. The pregnancy was complicated by a successfully treated urinary tract infection in the second month, otherwise the pregnancy, labor, and delivery were normal. Consanguinity was denied and the family history was unremarkable. The patient’s psychomotor development was delayed: head up at 6 months, smiled at 8 months, sat up at 9 months, walked alone and had a 4–5 word vocabulary at age 2 yr and was toilet trained at 4 yr.
Physical examination at 47/12 yr showed a pleasant child with a height <3rd centile, weight at the 10th centile, and head circumference >97th centile. He had facial abnormalities of frontal bossing, hypertelorism, maxillary hypoplasia, mild exophthalmus, epicanthal folds, broad depressed nasal bridge, short upturned nose with antever-eted nares, triangular mouth, gingival hyperplasia and a small penis. All limbs appeared short with stubby fingers and toes with broad hands and wrinkling of the dorsal skin. X-ray studies showed peripheral dysostosis, broad, short metacarpals and phalanges with cone-shaped epiphyses, frontal bossing with premature closure of the sagittal suture and platybasia. Urine for metabolic genetic screen was normal. Routine biochemical and laboratory studies, including calcium and phosphorus levels, were normal.
A Peabody Picture Vocabulary Test showed a receptive ability of 2 to 23/12 yr and expressive ability of 2 yr at a chronological age of 47/12 yr. A Stanford Binet Intelligence Test performed at age 9 yr produced an intelligence quotient score of 56.
At age 13 yr, hypertelorism and gingival hyperplasia were not present, but scoliosis and first ray hyperplasia of the foot were noted. Results of high resolution chromosome studies were normal. There was no evidence of subcutaneous mineralization. The other anomalies noted at 47/12 yr were again observed (Figs. 1, 2). The dermatoglyphic analysis showed three ulnar loops (digits one, three, and five), one radial loop (digit two) and one whorl (digit four) of the right hand while three whorls (digits three, four, and five) and two ulnar loops (digits one and two) were seen on the left hand. The maximal atd angle [reflection of degree of distal displacement of the palmar (t) axial triradius] was 53° on the left and 58° on the right hand. There were no abnormal hypothenar or thenar patterns, although a simian crease was noted on the left hand.
Fig. 1.
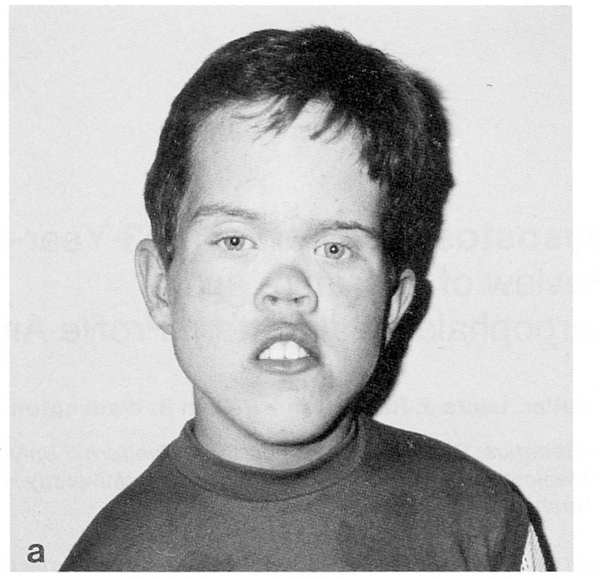
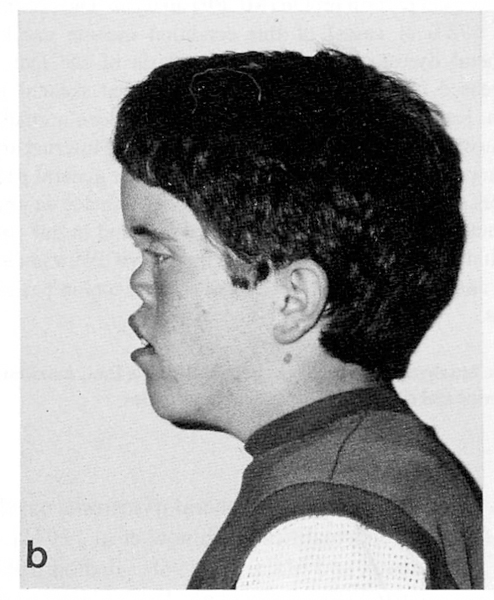
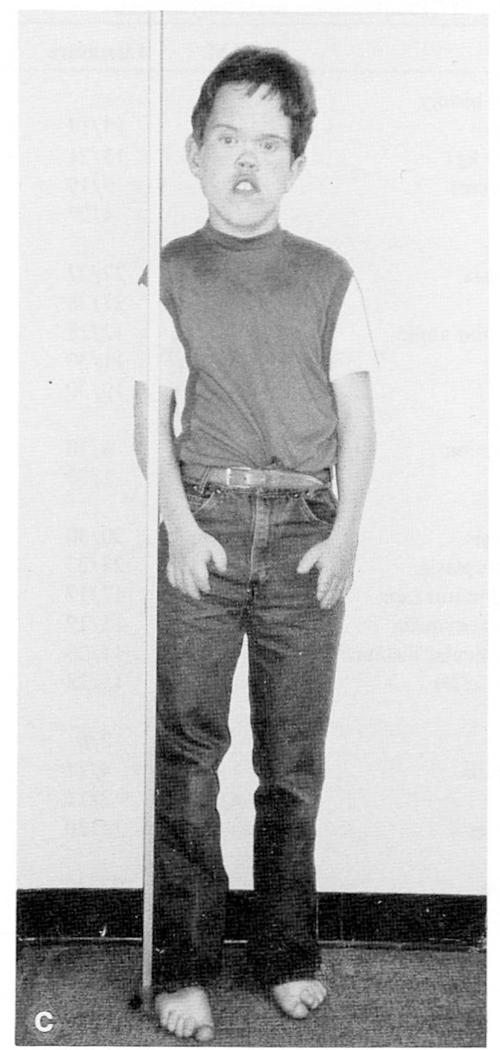
a, b, c. Our patient at age 13 yr.
Fig. 2.

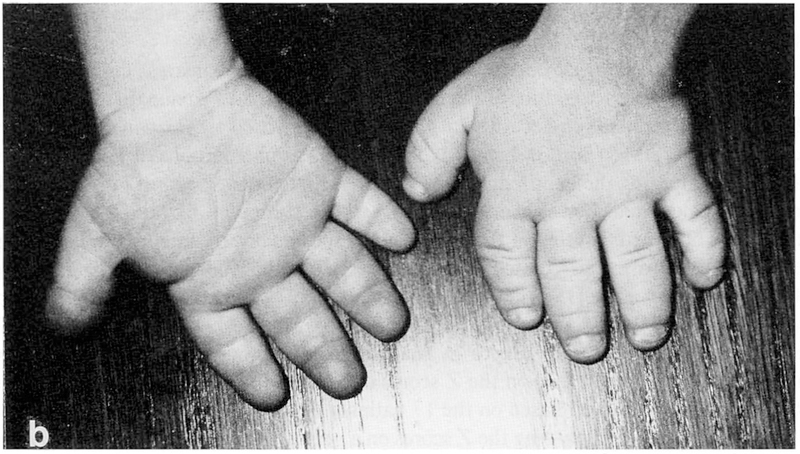
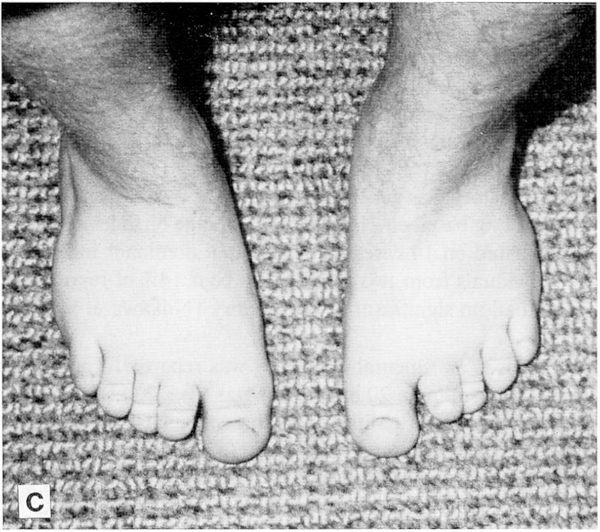
a, b, c. Roentgenograms of the hands and photographs of the hands and feet from our patient at age 13 yr. Bone age was 166/12 yr.
MCPP Analysis
Seventeen patients with acrodysostosis were included in this study. This group included 16 patients from the literature (six males and ten females with average age of 8.8 yr and range of 0.6 to 37 yr) for which acceptable hand radiographs were available and our patient (Table II).
TABLE II.
Correlations Between Acrodysostosis Individual’s MCPP With Group Mean MCPP
| Individual case | Age (years) | Sex | Correlation |
|---|---|---|---|
| C.M. | 13 | M | 0.69b |
| Cerda et al. [1979] | 8 | M | 0.50a |
| Cohen and van Creveld [1963] | 5 | M | 0.40a |
| Reiter [1978] | 41/2 | M | 0.40a |
| Singleton et al. [1960] | 8 | M | 0.80b |
| Niikawa et al. [1978] | 7/12 | M | 0.10 |
| Robinow et al. [1971] | 5 | M | 0.69b |
| Garces et al. [1969] | 5 | F | 0.89b |
| Arkless and Graham [1967] | 37 | F | 0.81b |
| Maroteaux and Malamut [1968] | 15 | F | 0.79b |
| Poznanski [1984] | 2 | F | 0.10 |
| Poznanski [1984] | 14 | F | 0.85b |
| Robinow et al. [1971] | 81/6 | F | 0.84b |
| Giedion [1973] | 10 | F | 0.83b |
| Poznanski et al. [1973] | 4 | F | 0.78b |
| Smith [1982] | 5 | F | 0.75b |
| Singleton et al. [1960] | 9 | F | 0.86b |
P < .05 for one tailed test.
P < .005 for one tailed test.
Metacarpophalangeal bone lengths were measured to the nearest millimeter with a vernier caliper from photographs of the hand roentgenograms of each patient. Bone length determination was made in accord with the method proposed by Poznanski et al. [1972] and Kaler et al. [1981] for applying MCPP analysis to photographs of hand roentgenograms. By comparing the bone lengths to normal mean lengths, Z scores for the individual bones were calculated. For a given bone, a Z score is computed by taking the difference between the observed length and the mean length specific for age and sex and dividing by the standard deviation associated with the mean length. The normal standards were published by Garn et al. [1972] (white Americans, age 2 yr to adulthood) and Poznanski [1974] (Gefferth Hungarian sample, from birth to age 15 months). The Z score of the first metacarpal was made equal to zero in analyzing the photographs and the MCPP was derived for each patient based on the Z scores of the remaining 18 bone lengths. A mean pattern profile was derived based on the 17 patients by calculating the average Z score of each of the 18 bones and plotting the Z scores on a graph. For hand pattern comparisons in this study, a correlation program was employed to produce a Pearsonian r value between each patient’s hand profile and the mean profile derived from the 17 patients.
RESULTS AND DISCUSSION
Acrodysostosis is characterized by short hands with peripheral dysostosis, nasal hypoplasia, skeletal abnormalities of the skull, mandible and spine and mental deficiency. We present an additional patient with this rare disorder, review 30 previously reported cases (Table I) and derive the MCPP of our patient and for the syndrome (Fig. 3).
TABLE I.
Summary of Manifestations in Acrodysostosis
| Trait | C.M. | Literature | Total | % |
|---|---|---|---|---|
| Gestation and family history | ||||
| Normal pregnancy | − | 13/17 | 13/18 | 72 |
| Birth weight (<2.5 kg) | + | 13/21 | 14/22 | 64 |
| Birth length (<46 cm) | ? | 9/19 | 9/19 | 47 |
| Family history | − | 4/27 | 4/28 | 14 |
| Craniofacial | ||||
| Maxillary hypoplasia | + | 22/22 | 23/23 | 100 |
| Nasal hypoplasia | + | 27/28 | 28/29 | 97 |
| Increased mandibular angle | + | 12/18 | 13/19 | 68 |
| Epicanthal folds | + | 11/30 | 12/31 | 39 |
| Hypertelorism | + | 10/30 | 11/31 | 35 |
| Dental abnormalities | ||||
| Delayed tooth eruption | + | 6/30 | 7/31 | 23 |
| Hypodontia | − | 1/30 | 1/31 | 3 |
| Musculoskeletal | ||||
| Peripheral dysostosis | + | 30/30 | 31/31 | 100 |
| Foot, first ray hyperplasia | + | 23/23 | 24/24 | 100 |
| Advanced skeletal maturation | + | 17/17 | 18/18 | 100 |
| Acromesomelic brachymelia | + | 15/19 | 16/20 | 80 |
| Decreased interpedicular distance | + | 17/23 | 18/24 | 75 |
| Short stature (< –2SD) | + | 15/28 | 16/29 | 55 |
| Urogenital | ||||
| Cryptorchidism | − | 2/6 | 2/7 | 29 |
| Hypoplastic genitalia | + | 4/17 | 5/17 | 29 |
| Irregular menses | n/a | 2/11 | 2/11 | 18 |
| Renal abnormalities | − | 1/30 | 1/31 | 3 |
| Other | ||||
| Mental retardation | + | 23/30 | 24/31 | 77 |
| Hearing abnormalities | − | 10/14 | 10/15 | 67 |
Fig. 3.
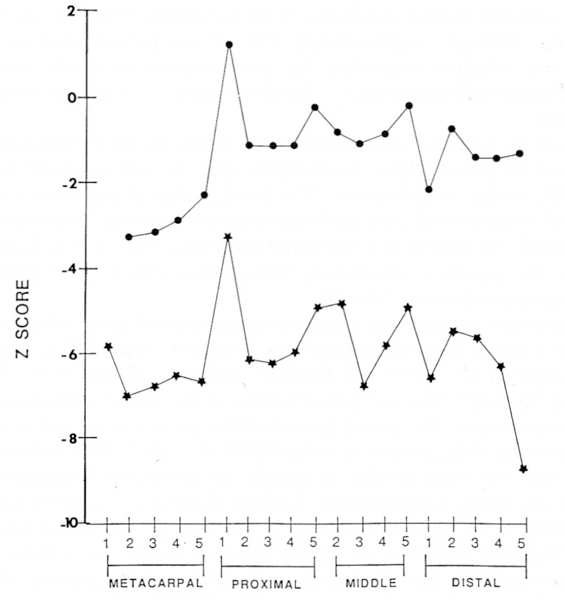
Mean MCPP for 17 individuals with acrodysostosis established from published cases (top) and MCPP from our patient (bottom).
The average age at diagnosis for all cases was 11.7 yr for 19 females and 12 males, including our patient. The average age at the time of birth was 27 yr for 15 mothers and 31 yr for 13 fathers. The maternal and paternal ages were 2 and 3 yr, respectively, above the average age for the general parent population [Van Dyke et al., 1983] and suggests that advanced parental age may be a factor in the condition.
The pregnancy history was generally normal. The average birth weight was 2.47 kg with a range of 1.8–3.2 kg based on 21 cases. The average birth length was 46.5 cm with a range of 43–49 cm based on 14 cases. An autosomal dominant inheritance pattern was reported in four individuals from two families or about 14% of reported cases, while the remaining 24 cases had no significant family history [Niikawa et al., 1978; Frey et al., 1982].
In 24 of 31 cases (77%) mental deficiency was reported. The average intelligence quotient and standard deviation in 20 individuals was 61+20 with a range of 24–85.
Several craniofacial abnormalities including maxillary hypoplasia (100%); nasal hypoplasia (97%); and increased mandibular angle (68%) were observed in this syndrome. Hearing abnormalities were reported in 67% of the cases. Less frequent findings include epicanthal folds (35%), hypertelorism (35%) and delayed tooth eruption (23%). At least seven individuals, including our patient, have been reported with cranial hyperostosis.
Skeletal abnormalities were frequently identified in this syndrome. The most common bone changes were peripheral dysostosis (100%); first ray hyperplasia of the foot (100%); and advanced skeletal maturation in all individuals with bone age information reported in the literature. Approximately 75% of the patients had acromesomelic brachymelia and vertebral anomalies, the most common of which was decreased interpedicular distance. Short stature (< − 2 SD) was observed at the time of evaluation in 55% of the cases.
Because of the peripheral dysostosis and short hands, the MCPP was generated from our patient and 16 patients from the literature (Fig. 3) and compared to that from syndromes with similar manifestations. The hand profiles of published acrodysostosis patients as well as our patient were uniformly abnormal with four prominent peaks (1st and 5th proximal, 5th middle and 2nd distal phalanges, Fig. 3). The hand profile in acrodysostosis also appears to be relatively homogeneous with 15 of 17 patients having significant positive correlations (Table II).
Hand profiles of patients with pseudo- or pseudopseudohypoparathyroidism, which may represent a milder form of acrodysostosis [Poznanski et al., 1973], acromesomelic dysplasia [Langer et al., 1977] and Robinow syndrome [Butler et al., 1987] were compared with the profile from our patient because of the similar clinical manifestations found in these syndromes. The up and down deviation pattern in our patient is similar to that of acrodysostosis with a correlation value of 0.69 (P < .005). The correlation values of our patient with the mean profiles of pseudo- or pseudopseudohypoparathyroidism [Poznanski et al., 1973], acromesomelic dysplasia [Langer et al., 1977] and Robinow syndromes [Butler et al., 1987] were 0.51 (P < .05), 0.42 (P < .05), and 0.14 (P > .05), respectively. Therefore, MCPP of our patient was more similar with a higher correlation value with acrodysostosis than in pseudo- or pseudopseudohypoparathyroidism, acromesomelic dysplasia, or Robinow syndromes. The MCPP analysis of our patient was useful in ruling out other syndromes with similar clinical characteristics. Therefore, we propose that MCPP analysis is a useful tool for diagnosis in this syndrome similar to the analysis employed with several other conditions such as Prader-Willi and Sotos syndromes [Butler and Meaney, 1985; Butler et al., 1986; Butler et al., 1988].
ACKNOWLEDGMENTS
The authors are grateful to American Academy of Pediatrics Memorial Endowment Fund For Children for support in this research.
REFERENCES
- Ablow RC, Hsia YE, Brandt IK (1977): Acrodysostosis coinciding with pseudohypoparathyroidism and pseudopseudohypoparathyroidism. Am J Roentgenol 128:95–99. [DOI] [PubMed] [Google Scholar]
- Arkless R, Graham CB (1967): An unusual case of brachydactyly. Am J Roentgenol 99:724–735. [PubMed] [Google Scholar]
- Butler MG, Dijkstra PF, Meaney FJ, Gale DD (1988): Metacarpophalangeal pattern profile analysis in Sotos syndrome: A follow-up report on 34 subjects. Am J Med Genet 29:143–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler MG, Gale DD, Meaney FJ, Wadlington WB, Robinow M (1987): Metacarpophalangeal pattern profile analysis in Robinow syndrome. Am J Med Genet 27:219–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler MG, Meaney FJ (1985): Metacarpophalangeal pattern profile analysis in Prader-Willi syndrome: A follow-up report on 38 cases. Clin Genet 28:27–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler MG, Meaney FJ, Kaler SG (1986): Metacarpophalangeal pattern profile analysis in clinical genetics: An applied anthropometric method. Am J Phys Anthropol 70:195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerda AP, Cazorla ZN, Martinez R, Tellez AM, Cantü JM (1979): Acrodysostosis. Bol Med Hosp Infant Mex 36:453–462. [PubMed] [Google Scholar]
- Cohen P, Van Creveld S (1963): Peripheral dysostosis. Br J Radiol 36:761–765. [DOI] [PubMed] [Google Scholar]
- Frey VG, Martin J, Diefel K (1982): Die akrodysostose-eine autosomal-dominant verebte periphere dysplasie. Kinderarztl Prax 3:149–153. [PubMed] [Google Scholar]
- Garces LY, Blank E, Drash AL, Kenney FM (1969): Peripheral dysostosis: Investigation of metabolic and endocrine functions. J Pediatr 74:730–737. [DOI] [PubMed] [Google Scholar]
- Garn SM, Hertzog KP, Poznanski AK, Nagy JM (1972): Metacarpophalangeal length in the evaluation of skeletal malformation. Radiology 105:375–381. [DOI] [PubMed] [Google Scholar]
- Giedion A (1968a): Die periphere dysostose (PD): Ein Sammelbegriff. Fortschr Roentgenstr 110:507–524. [PubMed] [Google Scholar]
- Giedion A (1968b): Zapfenepiphysen: Naturgeschichte und diagnostische bedeutung des enchondralen Wachstums. Ergeb Med Radiol 1:59–124. [Google Scholar]
- Giedion A (1973): Acrodysplasias. Prog Pediatr Radiol 4:325–345. [Google Scholar]
- Goodman JR (1978): Acrodysostosis: A case report. Br Dent J 145:105–106. [DOI] [PubMed] [Google Scholar]
- Kaler SG, Bixler D, Yu PL (1981): Metacarpophalangeal pattern profile in ACPS type II (Carpenter syndrome). J Craniofac Genet Dev Biol 1:373–381. [PubMed] [Google Scholar]
- Langer LO, Beals RK, Solomon IL, Bard PA, Bard LA, Rissman EM, Rogers JG, Dorst JP, Hall JG, Sparks RS, Franken EA (1977): Acromesomelic dwarfism: Manifestations in childhood. Am J Med Genet 1:87–100. [DOI] [PubMed] [Google Scholar]
- Maroteaux P, Malamut G (1968): L’acrodysostose. Presse Méd 76:2189–2192. [PubMed] [Google Scholar]
- Niikawa N, Matsuda I, Ohsawa T, Kajii T (1978): Familial occurrence of a syndrome with mental retardation, nasal hypoplasia, peripheral dysostosis, and blue eyes in Japanese siblings. Hum Genet 42:227–232. [DOI] [PubMed] [Google Scholar]
- Ortolani M, Cremonesi M (1963): Su di un caso di acromicria vera. Clin Orthop 15:193–203. [Google Scholar]
- Poznanski AK (1974): “The Hand in Radiological Diagnosis.” 1st ed Philadelphia: W.B. Saunders, pp 29–35. [Google Scholar]
- Poznanski AK (1984): “The Hand in Radiological Diagnosis.” 2nd ed Philadelphia: W.B. Saunders, pp 361–363. [Google Scholar]
- Poznanski AK, Garn SM, Nagy JM, Gall JC (1972): Metacarpophalangeal pattern profiles in the evaluation of skeletal malformations. Radiology 104:1–11. [DOI] [PubMed] [Google Scholar]
- Poznanski AK, Werder EA, Giedion A (1973): The pattern of shortening of the bones of the hand in PHP and PPHP—A comparison with brachydactyly E, Turner syndrome, and acrodysostosis. Pediatr Radiol 123:707–718. [DOI] [PubMed] [Google Scholar]
- Reiter S (1978): Acrodysostosis: A case of peripheral dysostosis, nasal hypoplasia, mental retardation and impaired hearing. Pediatr Radiol 7:53–55. [DOI] [PubMed] [Google Scholar]
- Robinow M, Pfeiffer RA, Gorlin RJ, McKusick VA, Renuart AW, Johnson GF, Summitt RL (1971): Acrodysostosis: A syndrome of peripheral dysostosis, nasal hypoplasia, and mental retardation. Am J Dis Child 121:195–203. [PubMed] [Google Scholar]
- Singleton EB, Daeschner CW, Teng CT (1960): Peripheral dysostosis. Am J Roentgenol 84:499–505. [PubMed] [Google Scholar]
- Smith DW (1982): “Recognizable Patterns of Human Malformation.” Philadelphia: W.B. Saunders, p 323. [Google Scholar]
- Steinbach H, Young DA (1966): The roentgen appearance of pseudohypoparathyroidism (PH) and pseudopseudohypoparathyroidism (PPH). Am J Roentgenol 97:49–66. [DOI] [PubMed] [Google Scholar]
- Undreiner F Pflieger H, Ludwiczak R, Beyer P (1981): L’acrodysostose: A propos d’un cas avec étude tomodensitométrique cranio-cérébrale. Ann Pédiatr 28:429–432. [PubMed] [Google Scholar]
- Van Dyke DL, Miller MJ, Weiss L (1983): The origin of inverted tandem duplications, and phenotypic effects of tandem duplication of the X chromosome long arm. Am J Med Genet 15:441–450. [DOI] [PubMed] [Google Scholar]


