Abstract
Background
The quality of the learning environment in the operating room (OR) is vital for the training of surgical residents. Tools with validity evidence exist to measure resident perceptions of the operative learning environment, yet to date no studies have assessed this environment for obstetrics and gynecology residency programs in the United Arab Emirates (UAE).
Objective
We explored perceptions of obstetrics and gynecology residents regarding their operative learning environment in 2 hospitals in Abu Dhabi, UAE.
Methods
Our cross-sectional study was conducted in 2018 using the validated Surgical Theater Educational Environmental Measure (STEEM) questionnaire for trainee assessments in the OR learning environment. The 4 STEEM subscales measure teaching and training, learning opportunities, overall atmosphere, and supervision, workload, and support, respectively. Cronbach's alpha and intraclass correlation were used to establish the internal consistence and reliability of the questionnaire. We calculated an overall score and compared scores between the 2 institutions using Student's t test.
Results
Thirty-one residents completed the questionnaire (18 at Corniche Hospital and 13 at Al Ain Hospital). The overall average STEEM score was 142.1. The score for residents at Corniche Hospital was 134.9 and that for Al Ain Hospital was 152.2, with better overall scores on 3 STEEM domains at Al Ain Hospital.
Conclusions
Our study showed that obstetrics and gynecology residents in the UAE have a positive perception of their operative learning environment. We also identified areas for improvement.
What was known and gap
There is a need for tools to assess the operating room learning environment in surgical programs, yet few have been validated in international settings.
What is new
A study used the validated Surgical Theater Educational Environment Measure (STEEM) to assess obstetrics and gynecology residents' perceptions of their operative learning environment in the United Arab Emirates (UAE).
Limitations
Small, single specialty sample limits generalizability.
Bottom line
Obstetrics and gynecology residents in the UAE have positive perceptions of their operative learning environment. Use of the STEEM instrument also identified areas for improvement.
Introduction
The educational environment is an important determinant of resident learning,1,2 In operative specialties the learning environment in the operating room (OR) is critical to the acquisition of surgical skills.3 The Surgical Theater Educational Environment Measure (STEEM) was developed and validated in the United Kingdom as an instrument that measures the learning environment in the OR.3 It consists of 40 questions and includes 4 subscales dealing with teaching and training, learning opportunities, overall atmosphere, and supervision/workload/support.3 The measure has been used to assess the operative learning environment in different settings across the world.4,5
At Corniche Hospital in Abu Dhabi, United Arab Emirates (UAE), internal surveys of obstetrics and gynecology residents showed that they did not feel prepared to practice independently after graduation. Thus, there was a need to evaluate trainees' perceptions of learning in the OR as it is critical for their surgical training and competence in practice. We used the STEEM questionnaire to explore the perceptions of obstetrics and gynecology residents regarding the OR environment in 2 UAE teaching institutions, Corniche Hospital and Al Ain Hospital, and compared resident perceptions of the 2 institutions.
Methods
Between August and November 2018, we conducted a cross-sectional study of obstetrics and gynecology residents at the 2 hospitals (informed consent form provided as online supplemental material). Residents were given access to the STEEM instrument using Google Forms. The cohort included 1 male participant, and respondents' sex was not asked to avoid identification. The STEEM questionnaire consists of 40 statements, graded using a Likert scale (1, strongly disagree, to 5, strongly agree).3 For negative statements, scoring is reversed. For all components, a higher score reflects a more positive perception of the operative learning environment. The STEEM has a maximum score of 200, with scores higher than 120 indicating an acceptable to superior environment and less than 120 suggesting a less than satisfactory learning atmosphere.4
The Ethics Committee at Corniche Hospital exempted the study from ethics review at both institutions.
Data were analyzed using SPSS 24 (IBM Corp, Armonk, NY). We used Cronbach's alpha to determine internal consistency. To evaluate the construct validity of the 4 STEEM subscales, we performed an explanatory factor analysis (principal components analysis) using Varimax rotation. Construct validity was measured using intraclass correlation coefficient to assess the relationship of individual items to the overall score.
We used the independent Student's t test to compare trainee perceptions on the 4 STEEM subscales for the 2 institutions. A P value < .05 was considered statistically significant.
Results
Of 34 residents, 31 (91%) responded, 18 (58%) from Corniche Hospital and 13 (42%) from Al Ain Hospital. The STEEM questionnaire had a Cronbach's alpha of 0.844 overall, with 0.65 for Al Ain and 0.79 for Corniche. We also calculated Cronbach's alpha for the subscales (provided as online supplemental material). Exploratory factor analysis followed by Varimax rotation showed 1 factor with an eigenvalue of 9.84, which accounted for 25% of the variance and 6 factors with eigenvalues between 2 and 3, suggesting the STEEM is a 1-dimensional scale. We also calculated mean and median scores for each question (provided as online supplemental material).
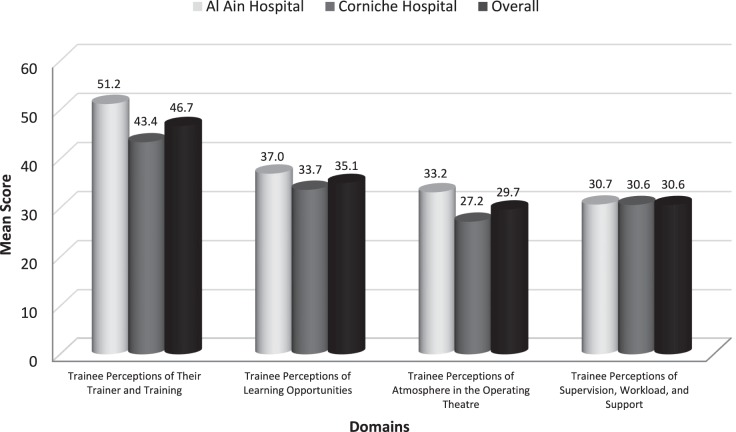
The overall score for the entire sample was 142.1, with a score of 134.9 for Corniche Hospital and 152.2 for Al Ain Hospital, suggesting an acceptable to good operative learning environment in both institutions. The scores for resident perceptions in the 4 subdomains are shown in the Figure.
Figure.
Mean Scores on the 4 STEEM Domains
The most highly rated items were “I get enough opportunity to assist” (score 4.3), “the operating theater staff is friendly” (score 4.1), and the reverse scored item “I [do not] feel discriminated against in theater because of my sex” (score 4.2). The areas with the lowest perception were “my trainer is in too much of a rush during emergency cases to let me operate” (score 2.0), “my trainer immediately takes the instruments away when I do not perform well” (score 2.6), and “more senior trainees take my opportunities to operate” (score 2.7).
Comparison of mean scores for the 2 hospitals showed a statistically significant difference between the perception of residents for trainers and training (P < .0001), learning opportunities (P = .032), and the atmosphere in the operating room (P < .0001), with more positive perceptions of the operative environment by residents at Al Ain Hospital. No differences between the 2 institutions were found in residents' perceptions of supervision, workload, and support (P = .92).
Discussion
In our application of the instrument in 2 settings in Abu Dhabi, the STEEM questionnaire showed a high Cronbach's alpha, suggesting it is a reliable tool for assessing the OR learning environment in an international setting. Our values are comparable to the study by Cassar conducted in the United Kingdom,3 and higher than those in the study by Al-Qahtani and Al-Sheikh, conducted in Saudi Arabia.4 In keeping with a single dimension instrument, there was a high correlation of each item to the total score (provided as online supplemental material).6
The overall scores suggest that obstetrics and gynecology residents have positive perceptions of the OR environment in Abu Dhabi. The highest score for Corniche Hospital was in the perception of supervision, workload, and support, while data for Al Ain Hospital suggested a superior resident perception of the working atmosphere in the OR. We found a healthy learning environment in both hospitals' operating rooms, with lower-scoring items highlighting areas in need of improvement, including trainee perceptions that trainers are in a rush, and may not allow trainees to continue to operate if they perform poorly. Willingness to let trainees operate is 1 criterion to define a successful surgical trainer.7
A potential reason for the different perceptions at the 2 hospitals is a difference in workload, with Corniche Hospital having significantly more deliveries annually.8,9 This may contribute to less faculty time available for resident education. Additionally, at Al Ain Hospital, residents focus exclusively on obstetrics during their first 2 years, providing junior residents with more OR time and opportunity to improve surgical skills. In contrast, at Corniche Hospital, residents start training in obstetrics and gynecology simultaneously, leaving them with less OR time early in training.
Limitations of our study include its small sample, the exclusive focus on obstetrics and gynecology residents, and our findings may not generalize to other specialties. Further studies of UAE residents from multiple specialties could broaden the information about trainee perceptions of the OR environment, and qualitative research could deepen our understanding of the factors that influence resident perceptions.
Conclusion
Our study using the STEEM instrument showed obstetrics and gynecology residents in 2 UAE hospitals perceive their learning environment in the OR to be healthy and encouraging. Using the instrument we were able to identify program strengths and areas for improvement. The tool may be generalizable to the assessment of the operative learning environment in other surgical specialties.
Supplementary Material
References
- 1.Genn JM. AMEE Medical Education Guide No. 23 (Part 1): curriculum, environment, climate, quality and change in medical education-a unifying perspective. Med Teach. 2001;23(4):337–344. doi: 10.1080/01421590120063330. [DOI] [PubMed] [Google Scholar]
- 2.Schönrock-Adema J, Bouwkamp-Timmer T, van Hell EA, Cohen-Schotanus J. Key elements in assessing the educational environment: where is the theory? Adv Health Sci Educ Theory Pract. 2012;17(5):727–742. doi: 10.1007/s10459-011-9346-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cassar K. Development of an instrument to measure the surgical operating theatre learning environment as perceived by basic surgical trainees. Med Teach. 2004;26(3):260–264. doi: 10.1080/0142159042000191975. [DOI] [PubMed] [Google Scholar]
- 4.Al-Qahtani MF, Al-Sheikh M. Assessment of educational environment of surgical theatre at a teaching hospital of a Saudi university: using Surgical Theatre Educational Environment Measures. Oman Med J. 2012;27(3):217–223. doi: 10.5001/omj.2012.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahoney A, Crowe PJ, Harris P. Exploring Australasian surgical trainees' satisfaction with operating theatre learning using the ‘surgical theatre educational environment measure.'. ANZ J Surg. 2010;80(12):884–889. doi: 10.1111/j.1445-2197.2010.05430.x. [DOI] [PubMed] [Google Scholar]
- 6.Statistics How to. Intraclass correlation. 2019 https://www.statisticshowto.datasciencecentral.com/intraclass-correlation Accessed May 31.
- 7.Dean B, Jones L. Garfield Roberts P, Rees J. What is known about the attributes of a successful surgical trainer. J Surg Educ. 2017;74(5):843–850. doi: 10.1016/j.jsurg.2017.01.010. [DOI] [PubMed] [Google Scholar]
- 8.SEHA Abu Dhabi Health Services Co. Introducing Corniche Hospital. 2019 https://www.seha.ae/corniche/English/aboutus/Pages/About-CornicheHospital.aspx Accessed May 31.
- 9.SEHA Abu Dhabi Health Services Co. Annual Report 2010. 2019 https://www.seha.ae/English/aboutus/annualreport/Pages/AR%202010/pdf/seha_ar10_en.pdf Accessed May 31.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.