Abstract
Background
Access to a trained, competent health care workforce remains a challenge globally, particularly in rural settings. To bridge this gap, the World Health Organization calls for innovations in electronic learning and task shifting. Yet, these approaches are underutilized due to cost, challenges associated with implementing technology, and a lack of suitably educated trainees.
Objective
We explored the feasibility of the Acute Care Providers Project (ACPP) to remotely train community members to be health care providers in 2 sites: Haiti and India.
Methods
The ACP program is an asynchronous curriculum that provides core health content and a structured approach to clinical care through an electronic curriculum. The curriculum is reinforced with case-based practice and hands-on workshops for procedural skills. ACPP was deployed in rural Haiti and India. Evaluation of the program included multiple-choice pretests and posttests, an objective structured clinical examination (OSCE), and direct observation of skills.
Results
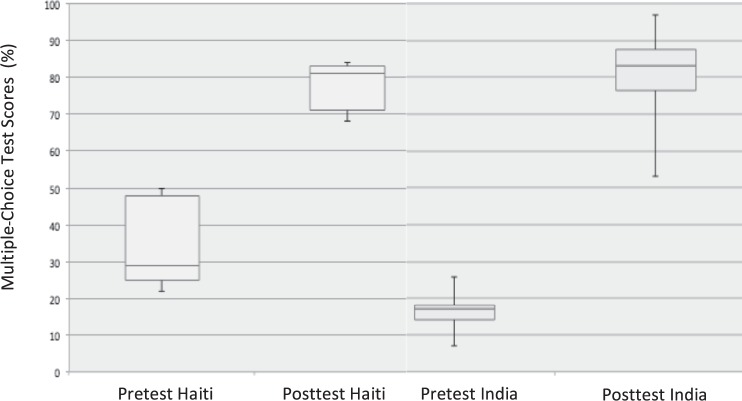
Four Haitian and 55 Indian trainees completed the course. In Haiti, mean scores were 34.8% (SD 12.4) on the pretest and 78.0% (SD 6.5) on the posttest (P = .004). Trainees scored 100% on the OSCE and passed the skills checklist. In India, mean scores were 16.5% (SD 3.9) on the pretest and 81.7% (SD 9.0) on the posttest (P < .001). Trainees scored a median of 91.8% (SD 3.95) on the OSCE and all passed the skills checklist.
Conclusions
The ACPP offers a scalable, replicable asynchronous curriculum to train lay individuals to provide basic health care in rural communities.
What was known and gap
Many areas across the globe lack access to basic acute health care services.
What is new
An asynchronous, electronic education program prepares community members to provide basic health care services.
Limitations
Pilot lacks longer-term outcomes for program graduates and the communities they serve.
Bottom line
The program is affordable, scalable, and transferrable to other communities with lack of access to care, and offers local opportunities for professional advancement.
Introduction
Access to trained health professionals remains a significant challenge in health care delivery worldwide, due to financial and time constraints, suitable trainees, and faculty shortages.1 To bridge this gap, the World Health Organization (WHO) has called for innovations in electronic-based learning that include task shifting from physicians to less specialized health care workers.2 Yet these approaches are vastly underutilized.3 Poor literacy and lack of formalized education make it challenging to broaden the scope of practice for laypersons.4 Many communities have populations of laypersons with limited opportunities for professional advancement. Training them to diagnose and treat patients not only meets community needs, but also offers career advancement opportunities. Traditionally, laypersons have been tasked with disease prevention, health promotion, treatment support, counseling, and linking patients to the health care system,5 while utilization of laypersons for diagnosis and treatment is narrow in scope (eg, the Integrated Management of Childhood Illness).6 Improving access to care in underserved settings requires providers with basic diagnostic and clinical abilities to manage common problems for which community members seek care.
Electronic-based learning formats are well-suited for improving access to training for health care workers in resource-constrained settings.7 Obstacles to using electronic-based learning include poor connectivity, lack of staff and infrastructure to maintain devices, and lack of learner engagement when courses are not taught with live instruction.8 These challenges can impede the success of electronic-based learning platforms.
To meet the need of underserved communities, we designed the Acute Care Providers Project (ACPP) to remotely train previously untrained lay individuals with limited opportunities for advancement. The aim was to prepare them for the diagnosis, treatment, and triage of 30 acute care chief complaints specific to the needs of rural communities lacking access to care. The program utilizes an electronic-based, asynchronous curriculum to reduce faculty time and cost. We implemented ACPP in rural Haiti and India in 2 populations with differing educational backgrounds and spoken languages to explore whether this approach was feasible in different settings.
Methods
Project Design and Evaluation
At the core of ACPP is a 3-step education program that encompasses (1) delivering health care content, (2) developing a clinical approach, and (3) learning procedural skills. The electronic, asynchronous curriculum uses animated video modules preloaded on tablets, eliminating the need for infrastructure, connectivity, and maintenance. Animation with minimal text allows synchronized translation of the narration to trainees' native language. Clinical care is simplified using a heuristic approach, basing decisions on a few relevant predictors that are easy for laypersons to identify and that can be pictorially represented to minimize the need for literacy and translation.9,10 Each module has criteria to transfer a patient to a hospital if they exhibit “red flag” signs portending clinical deterioration. Patterns are reinforced by case-based practice. Physician trainers lead a 2-week live skills workshop on basic airway maneuvers, suturing, traction, splinting, cervical spine protection, and transportation.
We separately assessed trainees at each step of the curriculum, requiring them to obtain a passing score before advancing to the next phase. We tested the efficacy of the core content module using 2 to 4 multiple-choice questions for each learning objective, divided equally into test A and test B. Four US emergency physicians reviewed and validated the questions, and piloted the tests for equivalency. Half of the trainees took test A prior to the project and half took test B, each receiving the opposite test for postevaluation. We a priori determined a passing grade of 75%.
We evaluated trainees' clinical approach, diagnostic skill, and practice safety using an objective structured clinical examination (OSCE) of 15 standardized, simulated cases. Project faculty randomly administered 3 cases to each trainee. Critical actions were determined a priori as “could not miss” portions of the examination, including identifying an unprotected airway, abnormal vital signs, and “red flags” that mandate transfer to a higher level of care. We used a compensatory standard; trainees had to complete 3 cases with a score of 80% or higher. Missing even 1 critical action resulted in case failure. Workshop moderators evaluated procedural skills using direct observation and a performance checklist.
We calculated test score means, standard deviations, and P values using paired t tests and Microsoft Excel software (Microsoft Corp, Redmond, WA).
Study Setting 1: Haiti
After the project received approval from the Haitian Ministry of Health, we initiated training in a rural area of Fort Liberté with a population of approximately 34,000. This community had 1 general physician, 1 obstetrician and gynecologist, 1 general surgeon, and sporadic visits from health professionals of an American church group.
Recruitment of trainees used a public announcement, and our partner organization, the Baptist Church in Fort Liberté, chose 31 applicants. Prerequisites included an interest in health care, socioeconomic disadvantage, and lack of resources for advanced education. Because education quality varies among localities, we tested literacy and numeracy using a custom-created reading comprehension and mathematics examination. Three members of the research team chose 6 trainees from 31 applicants based on examination performance, and individual, group, and working interviews (Table 1).
Table 1.
Trainee Characteristics
| Characteristic | Haiti | India |
| Initial number of trainees | 6 | 55 |
| Sex | ||
| Male | 3 | 0 |
| Female | 3 | 55 |
| Age group | ||
| Mean age | 24 | 39 |
| < 30 | 6 | 0 |
| 30–45 | 0 | 52 |
| > 45 | 0 | 3 |
| Mean years of education | 12 | 8 |
| Marital status | ||
| Single | 6 | 0 |
| Married | 0 | 55 |
| Widowed | 0 | 0 |
Over 8 months, the Haitian trainees completed 39 modules as a self-study project (Table 2). They discussed modules weekly, and a member of the research team conducted case-based practice with trainees weekly for 1 hour via video conference. The cost of training for each trainee was $933, covering the tablets, translation of video narration and workbook, implementation, and travel.
Table 2.
Haiti Acute Care Providers Project Module Topics
| Introduction | Patient Care | Gastrointestinal (GI) System | Genitourinary (GU) System |
| Introduction to being a provider | General history | Critical signs and abdominal pain | GU and sexually transmitted infections |
| Basic cell physiology | Vital signs | Diarrhea | Women's GU |
| Circulatory system | General examination | Hernias | |
| Respiratory system | Chest and lung examination | ||
| Nervous system | Abdominal examination | ||
| GI system | The critical patient | ||
| GU system | Medications | ||
| Respiratory System | Infectious Disease | Trauma | Pediatric Diseases |
| Introduction to respiratory disease | Malaria | Being a first responder | Introduction to pediatrics |
| Asthma and COPD | Ameobiasis | Major trauma | Malaria |
| Pneumonia | Dengue | Minor trauma | Cough |
| Cellulitis | Splinting | Respiratory infections | |
| Impetigo | Wheezing | ||
| Scabies | Dengue | ||
| Medications | Rashes | ||
| Scabies |
Abbreviation: COPD, chronic obstructive pulmonary disease.
Study Setting 2: India
Following approval by the Ethics Board of India, we initiated the program in rural villages in Uttar Pradesh and Bihar. Each village encompassed 500 to 1000 people and lacked a trained health care provider, with the nearest facility being a primary health center staffed during the day by a nurse located within 15 kilometers of the village.
Our partner organization, Healing Fields Foundation, chose 55 female trainees from 55 unique villages in Uttar Pradesh and Bihar based on previous participation in a health educator program (Table 1). Using health educators ensured basic literacy and family permission to work outside the home, as the village patriarchy may not allow women to leave the house. We did not screen for numeracy because the pilot excluded pediatrics, the only module that required math.
Delivery of education in India used a modified pilot curriculum of 14 modules over 4 months (Table 3). Modules were selected based on common illnesses reported in the village. We removed pediatric modules to eliminate dose calculations. Four India-based facilitators with bachelor's degrees and technology literacy navigated the modules to view as a group. The cost of training each trainee was $355, covering facilitator salaries, tablets, translation, implementation, and travel.
Table 3.
India Acute Care Providers Project Module Topics
| Introduction | Patient Care | Gastrointestinal (GI) System | Genitourinary (GU) System |
| Introduction to being a provider | Approach to the patient | Minor trauma | GU and sexually transmitted infections |
| Basic cell physiology | Abdominal examination | Contusions, sprains, strains, and back pain | Women's GU |
| Circulatory system | |||
| Respiratory system | |||
| Nervous system | |||
| GI and GU systems |
The overall study protocol was approved by the Institutional Review Board of Stanford University School of Medicine (IRB 43510).
Results
In Haiti, 4 students completed the ACPP. Of 6 students who started the curriculum, 1 dropped out prior and 1 failed the posttest. Data for the 5 trainees who completed the pretest and posttest were included in analysis. Pretest scores averaged 34.8% (SD 12.4) and posttest scores averaged 78% (SD 6.5), with this difference statistically significant (P = .004; Figure). The 4 students who completed the ACPP scored 100% on the OSCE and passed the procedural performance checklist.
Figure.
Written Examination Results
In India, 55 students completed the pretest and posttest. The mean pretest score was 16.5% (SD 3.9) and the mean posttest score was 81.7% (SD 9.0, P < .001). Fifty of the original 55 trainees passed the OSCE on the first attempt with a median score of 91.8% and a SD of 3.95 (Table 4). Appropriate diagnosis and management were the areas where points were frequently lost. All trainees passed the procedural performance checklist. Graduates of the program are currently providing basic acute services in both nations.
Table 4.
Objective Structured Clinical Examination Results
| Assessment | Haiti | India |
| Case specifics | n = 12 | n = 165 |
| Recognized red flag | 100% | 98.7% |
| Acted on red flag | 100% | 98.2% |
| ABCD | 100% | 99.3% |
| Vital signs | 100% | 98.2% |
| Appropriate history of the present illness | 100% | 97.6% |
| Asked permission and privacy for examination | 100% | 99.3% |
| Appropriate physical examination | 100% | 96.3% |
| Appropriate diagnosis | 100% | 95.7% |
| Appropriate management | 100% | 87.9% |
Discussion
These results demonstrate the feasibility of an electronic-based, asynchronous educational intervention to train lay individuals as acute care providers capable of providing basic services with minimal involvement by formally trained health professionals. The success of our curriculum is due to its ability to address 3 challenges: providing training of adults with little formal education and poor literacy; using technology as a platform for learning; and making the curriculum applicable to 2 different cultural and geographic settings.
We overcame barriers to training adult learners with poor literacy through the use of heuristics. Many common acute complaints can be distilled to key objective findings, enabling heuristic approach. This is nearly equivalent to physicians using probabilistic inputs.9,11,12 We emphasized recognition of emergencies related to airway, breathing, circulation, and mental status, and diseases outside the scope of trainees' practice. To reduce availability bias as a source of diagnostic errors, we taught common complaints familiar to trainees prior to starting the course.13,14 Additionally, we compensated for the lower basic knowledge of the Indian trainees by increasing the time for each module from 3 days to 2 weeks, and devoting the extra time to group discussions and workshops illustrating basic scientific principles using familiar analogies (eg, a water pump was analogous to the heart and different-sized hoses explained blood pressure and flow).
Allowing sufficient time to solidify concepts and using a heuristic model, trainees made few diagnostic errors, and none that would have resulted in unsafe treatment. Trainees' management mistakes also did not result in unsafe situations; 15 involved simply forgetting to counsel on prevention and follow-up.
Our curriculum was designed to overcome challenges of using technology for electronic learning in developing nations. Tablets do not require the network or physical infrastructure often lacking in austere environments, and preloading course content eliminates reliance on connectivity, which may be poor in many settings. Separate video and audio tracks allow narration to be replaced with the local language. Tablets are less expensive than other devices and the cost of labor to translate and facilitate is low. Cost will vary by locale. Expenses associated with training in India were less than half compared to Haiti due to lower labor costs. In both nations, the cost to train a health worker using ACPP is significantly lower than the cost to train a nurse, physician, or other advanced health professional.
In addition to providing trained health care workers to communities that lack access to care, our project enables individuals with limited opportunities for advancement an avenue to education and employment. For this reason, we adapted the program to the cultural and educational needs of the local setting. To us, it was important to train village women in India, who are often disregarded citizens after childbearing, and overcome their lack of familiarity with technology that made it challenging to navigate the program as a self-study course. While having sessions facilitated by 4 local college-educated trainers added costs and reduced flexibility, we felt this adjustment was beneficial. An added benefit was that using local facilitators improved trainees' engagement by increasing face-to-face contact. Those wishing to implement this curriculum in new populations should begin with surveying local culture and needs, and leveraging the adaptability of our modular, mixed-methods curriculum to suit their community.
Conclusion
ACPP utilizes a scalable, replicable, electronic-based curriculum to train laypersons as health care workers in areas with low provider-to-patient ratios. This curriculum can meet the educational requirements and language needs of local communities at a low cost, and can educate and increase professional advancement in resource-poor communities.
References
- 1.World Health Organization. Global health workforce shortage to reach 12.9 million in coming decades. 2019 November 11, 2013. http://www.who.int/mediacentre/news/releases/2013/health-workforce-shortage/en Accessed June 10.
- 2.Bollinger R, Chang L, Jafari R, O'Callaghan T, Ngatia P, Settle D, et al. Levering information technology to bridge the health workforce gap. Bull World Health Organ. 2013;91:890–891. doi: 10.2471/BLT.13.118737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization; Global Health Workforce Alliance. Global Experience of Community Health Workers for Delivery of Health Related Millennium Development Goals: A Systematic Review, Country Case Studies, and Recommendations for Integration into National Health Systems. 2010. 2019 http://www.who.int/workforcealliance/knowledge/resources/chwreport/en Accessed June 10.
- 4.Siribié M, Ajayi IO, Nsungwa-Sabiiti J, Afonne C, Balyeku A, Falade CO, et al. Training community health workers to manage uncomplicated and severe malaria: experience from 3 rural malaria-endemic areas in sub-Saharan Africa. Clin Infect Dis. 2016;63(suppl 5):264–269. doi: 10.1093/cid/ciw624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crowley T, Mayers P. Trends in task shifting in HIV treatment in Africa: effectiveness, challenges and acceptability to the health professions. Afr J Prim Health Care Fam Med. 2015;7(1) doi: 10.4102/phcfm.v7i1.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Integrated Management of Childhood Illness (IMCI) global survey report. 2017. 2019 https://www.who.int/maternal_child_adolescent/documents/imci-global-survey-report/en Accessed June 10. [PubMed]
- 7.Razzak JA, Kellermann AL. Emergency medical care in developing countries: is it worthwhile? Bull World Health Organ. 2002;80:900–905. [PMC free article] [PubMed] [Google Scholar]
- 8.Frehywot S, Vovides Y, Talib Z, Mikhail N, Ross H, Wohltjen H, et al. E-learning in medical education in resource constrained low- and middle-income countries. Hum Resour Health. 2013;11(1):4. doi: 10.1186/1478-4491-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Green L, Mehr DR. What alters physicians' decisions to admit to the coronary care unit? J Fam Pract. 1997;45(3):219–226. [PubMed] [Google Scholar]
- 10.World Health Organization Regional Office for the Eastern Mediterranean. Child health and development. IMCI adaptations. 2019 http://www.emro.who.int/child-health/IMCI/adaptation-principles#p2l4 Accessed June 10.
- 11.Fischer JE, Steiner F, Zucol F, Berger C, Martignon L, Bossart W, et al. Use of simple heuristics to target macrolide prescription in children with community-acquired pneumonia. Arch Pediatr Adolesc Med. 2002;156(10):1005–1008. doi: 10.1001/archpedi.156.10.1005. [DOI] [PubMed] [Google Scholar]
- 12.Marewski JN, Gigerenzer G. Heuristic decision making in medicine. Dialogues Clin Neurosci. 2012;14(1):77–89. doi: 10.31887/DCNS.2012.14.1/jmarewski. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science. 1974;185(4157):1124–1131. doi: 10.1126/science.185.4157.1124. [DOI] [PubMed] [Google Scholar]
- 14.Khan A, Penoff BT, Pirrotta EA, Hosang R. Shifting the paradigm of emergency care in developing countries. Cureus. 2018;10(2):e2219. doi: 10.7759/cureus.2219. [DOI] [PMC free article] [PubMed] [Google Scholar]