Abstract
Background
High rates of burnout have been reported in physicians in training, with contributing factors including stress, lack of coping skills, and attributes of the learning environment. The interrelationships among these factors and how they affect versus mitigate burnout in an international cohort of residents have not been studied.
Objective
We examined the interrelationships between stress, perceptions of the learning environment, and coping strategies used in a cohort of psychiatry residents in Singapore, using burnout as the dependent variable. We hypothesized that perceptions of the learning environment and coping strategies influence the relationship between residency-related stress and burnout in psychiatry residents.
Methods
From June 2016 to September 2017, 67 of 75 (89%) psychiatry residents from a single program in Singapore were assessed on their levels of stress and burnout, perceptions of their learning environment (including role autonomy, teaching, and social support), and the coping mechanisms they used.
Results
Psychiatry residents in this Singaporean program perceived their overall learning environment to be positive. Perceptions of the learning environment, not coping strategies, significantly mediated the relationship between stress and burnout.
Conclusions
Findings from this study suggest that perceptions of the learning environment mediate the relationship between stress and burnout. Approaches to evaluate and improve resident perceptions of aspects of their learning environment may be an effective strategy to manage burnout in psychiatry residency programs.
What was known and gap
The interrelated effects of stress, coping skills, and the learning environment on burnout in residents have not been fully examined.
What is new
A study examined the relationships among stress, coping, and residents' perceptions of their learning environment on burnout in Singaporean psychiatry residents.
Limitations
Single specialty study reduces generalizability.
Bottom line
Perceptions of the learning environment mediated the relationship between stress and burnout in psychiatry residents.
Introduction
Burnout is a syndrome that encompasses exhaustion, cynicism toward work, and reduced professional efficacy in the workplace.1 Burnout rates are high in physicians and range from 27% to 87% in samples that include psychiatry residents.2,3 There are various factors that contribute to or mitigate burnout, such as stress,4 coping skills,5,6 and perceptions of the learning environment.7 Several studies have identified factors unique to psychiatry that can contribute to increased stress for residents, including physicians' close and personal nature of involvement in the difficulties of patients, professional caseload, and case complexity, such as the management of homicidal or suicidal patients.8,9 To date, the interrelationships among these factors have not been studied within psychiatry residents in an international setting.
Stress is defined as a disruption in the equilibrium of the cognitive-emotional-environmental system via external factors that can potentially affect individuals negatively10,11 and can be a precursor to burnout.4 Positive associations have been observed between stress and burnout in residents and medical students.12,13 Specifically, it was found that residents are susceptible to burnout because of the stress they face during residency, which affects their personal well-being.13
Coping strategies has been suggested to influence the relationship between stress and burnout. In one study, negative coping strategies and job stress preceded emotional exhaustion,6 and in another study, positive and negative coping strategies mediated the relationship between stress and burnout.5 A study of counselors working with abused populations found that use of disengagement coping strategies mediated job stress and burnout.14
Perceptions of the learning environment have also been found to be significantly correlated with burnout, including a negative correlation between perceptions of the learning environment and emotional exhaustion/depersonalization, and a positive correlation with the personal accomplishment domain of burnout.15 A negative correlation was also observed between perceptions of the learning environment and mental distress in medical residents in an Asian setting.16
In this study, we examined the relationship between stress, perceptions of the learning environment, coping strategies used, and burnout in residents in a single psychiatry residency in Singapore. We aimed to identify the relationship between these variables, with burnout as the dependent variable. Based on previous studies, we hypothesized that both residents' perceptions of the learning environment and their adopted coping strategies influence the relationship between stress and burnout.
Methods
Study Sample and Data Collection
From June 2016 through September 2017, 67 of 75 psychiatry residents (89%) in the National Psychiatry Residency Program in Singapore were recruited prior to their centralized teaching sessions, which residents attend as a single group within their different levels of training. Eight residents did not consent to join the study.
Participants were administered 4 self-rated questionnaires: (1) the Postgraduate Hospital Educational Environment Measure (PHEEM)17,18 to assess residents' perceptions of their learning environment; (2) the Perceived Stress Scale (PSS)19 to assess stress levels; (3) the Oldenburg Burnout Inventory (OLBI)20 to measure burnout; and (4) the Brief COPE Inventory21 to assess residents' coping mechanisms. The scales are provided as online supplemental material.
The study was approved by the Institutional Review Board of the National Healthcare Group, Singapore. All participants provided written consent.
Statistical Analyses
We used principal component analysis (PCA) with Varimax (orthogonal) rotation of the coping strategies to identify the 2 main factors (maladaptive and positive coping strategies), and used multivariate (partial least squares path modeling method) analyses to examine the relationships between stress, the learning environment, coping strategies, and burnout. Partial least square structural equation modeling (PLS-SEM)22 was used to identify the pathway relationship between the variables (perceptions of the learning environment, stress, coping method), with burnout as the dependent variable.
Pathway modeling was conducted using SmartPLS 3.23 All other statistical analyses were conducted using SPSS 23 (IBM Corp, Armonk, NY). Statistical significance was set a priori at an alpha of .05 (2-tailed).
Results
Sixty-seven participants completed the questionnaires (60% male, mean age 30.2). Thirty were junior year residents (PGY-1 and PGY-2), and 37 were senior year residents (PGY-3–5). Slightly over half (54%, 36 of 67) were single. Stress level as rated by PSS had a total mean score of 15.97 (± 5.21); the OLBI exhaustion mean score was 2.50 (± 0.45), and disengagement was 2.27 (± 0.43). Overall perception of the learning environment measured with total PHEEM score was in the “more positive than negative range” (111.53 ± 1.771).
Adaptive and Maladaptive Coping Identified by Factor Analysis
Within principal component analyses, an examination of the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy suggested that the sampling was satisfactory (KMO = 0.739).24 Items with a loading higher than 0.4 were included25 and a 2-factor model emerged. We identified them as adaptive and maladaptive coping strategies (Table).
Table.
Two-Factor Model of Coping Strategies From Factor Analysis
| Coping Strategies | Factor 1 (Adaptive Coping) | Factor 2 (Maladaptive Coping) |
| Planning | 0.874 | 0.090 |
| Positive reframing | 0.778 | -0.090 |
| Active coping | 0.763 | 0.072 |
| Acceptance | 0.709 | 0.230 |
| Use of instrumental support | 0.602 | 0.077 |
| Use of emotional support | 0.491 | -0.082 |
| Behavioral disengagement | -0.112 | 0.866 |
| Use of alcohol and medications | -0.014 | 0.683 |
| Denial | 0.335 | 0.576 |
| Self-blame | 0.398 | 0.500 |
| Religion | 0.015 | -0.106 |
| Venting | 0.312 | 0.270 |
| Self-distraction | 0.341 | 0.378 |
| Humor | 0.223 | -0.019 |
Note: Bold text indicates the item loads comparatively more on that factor.
The first factor, “adaptive coping,” is marked by loadings of 6 coping strategies, namely planning, positive reframing, active coping, acceptance, use of instrumental support, and use of emotional support. The second factor, “maladaptive coping,” consists of high loadings of 4 strategies that include behavioral disengagement, use of alcohol and other medications, denial, and self-blame.
Pathway Analyses
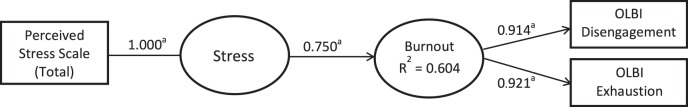
Using pathway modeling, the baseline model (Figure 1) established a relationship between perceived stress level and burnout, with 60% of the variance in burnout explained by stress. The path relationship between stress and burnout is significant (β = 0.750), suggesting stress is a strong predictor of burnout.
Figure 1.
Baseline Model Showing Significant Path Relationship Between Stress and Burnout
Abbreviation: OLBI, Oldenburg Burnout Inventory.
a P < .001.
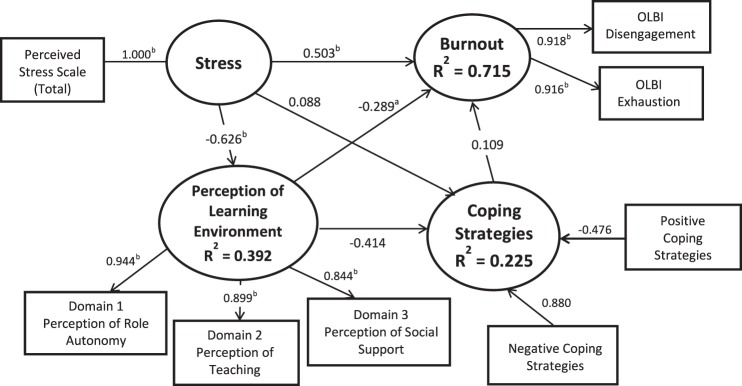
A serial multiple mediator model was used to test the hypothesized mediating roles of perceptions of the learning environment and coping strategies on the relationship between stress and burnout,26 showing 72% of the variance in burnout was explained by stress and perceptions of the learning environment. As shown in Figure 2, the indirect path was significant with inverse relationships found between stress and perceptions of the learning environment (β = -0.626), and learning environment perceptions and burnout (β = -0.289). In contrast, the path relationships between stress, coping strategies, and burnout were not statistically significant, suggesting perceptions of the learning environment played a more important role in mediating the relationship between stress and burnout compared to coping strategies.
Figure 2.
Model Testing Mediating Effects of Perceptions of Learning Environment and Coping Strategies on Relationship Between Stress and Burnout
Abbreviation: OLBI, Oldenburg Burnout Inventory.
a P < .05.
b P < .001.
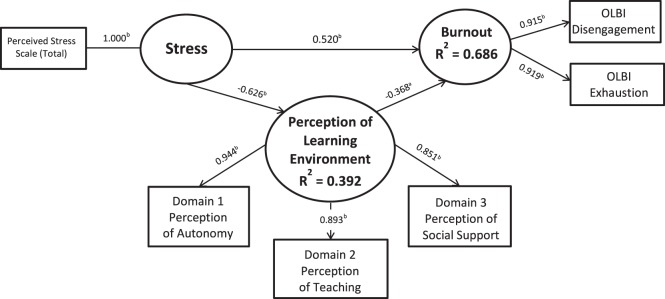
In our final model to examine the role of perceptions of the learning environment on the relationship between stress and burnout (Figure 3), 69% of the variance in burnout was explained by stress and perceptions of the learning environment. Learning environment perceptions partially mediated the effect stress had on burnout, as shown by the lowered path coefficient value between stress and burnout in the final model (β = 0.520), compared to the baseline model (β = 0.750).
Figure 3.
Final Model Showing Partial Mediation of Perceptions of Learning Environment on Effect of Stress on Burnout
Abbreviation: OLBI, Oldenburg Burnout Inventory.
a P < .01.
b P < .001.
Discussion
Our study has 2 main findings. First, psychiatry residents generally perceived their learning environment favorably, and the stress and burnout scores were comparable to those in other studies.27–29 Second, pathway analysis revealed that perceptions of the learning environment, but not coping strategies, mediated the relationship between stress and burnout within psychiatry residents.
Our findings are consistent with the interactionist model of stress that ties stress with context (learning environment) as well as potential outcome (burnout).30 We found that all 3 learning environment dimensions (perceived role autonomy, teaching, and social support) contributed to the relationship between stress and burnout. Other studies have identified perceived social support as a defense against life stressors.31,32
For role autonomy, adult learning theory posits that learners learn best if they are actively involved,33 and residents in another study reported that increasing levels of autonomy affirmed their competence and helped them recover from burnout, and that mindset and opportunities that focused on learning contributed to enjoyment derived from work.34
Residents in our program perceived their learning environment as positive. Attributes of our program that may increase resident perceptions of autonomy and competence and enhance social support include residents being enlisted to organize outreach and social bonding events as well as provide feedback through the resident representatives to improve the program. We encourage interactive learning, use of narratives, and active discussions to engage and equip learners for different requisite topics. Finally, we underscore the importance of fatigue and stress management, work-life balance, availability of “buddy network,” and direct access to supervisor/core faculty and program directors whenever needed for discussion of training or personal issues.
Our study has limitations, including its cross-sectional design. Extension to a longitudinal design would allow for better determination of causal relationships between the variables of interest. We also limited our assessment of the learning environment to resident perceptions. Incorporation of other perspectives, like those of faculty, might complement and support our findings.
Conclusion
Our findings suggest that residents' positive perceptions of their learning environment mediated the relationship between stress and burnout. Approaches to assess and improve resident perceptions of aspects of their learning environment may be an effective strategy in reducing burnout in psychiatry residency. These findings may be generalizable to programs in other specialties. Future research should assess the impact of positive changes in the learning environment on the relationship between stress and burnout.
Supplementary Material
References
- 1.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. Palo Alto, CA: Consulting Psychologists Press;; 1996. [Google Scholar]
- 2.Domaney NM, Torous J, Greenberg WE. Exploring the association between electronic health record use and burnout among psychiatry residents and faculty: a pilot survey study. Acad Psychiatry. 2018;42(5):648–652. doi: 10.1007/s40596-018-0939-x. [DOI] [PubMed] [Google Scholar]
- 3.Ishak WW, Lederer S, Mandili C, Nikravesh R, Seligman L, Vasa M, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236–242. doi: 10.4300/JGME-D-09-00054.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans-Turner T, Milner P, Mirfin-Veitch B, Gates S, Higgins N. The Maslach Burnout Inventory and its relationship with staff transition in and out of the intellectual disability workforce. Presentation to the NZASID Conference; August 24–26, 2010; Dunedin. https://www.asid.asn.au/Portals/0/Conferences/NZ2010/Maslach%20Burnout_Terese%20EvansTurner.pdf Accessed May 30, 2019.
- 5.Hutchinson TA, Haase S, French S, McFarlane TA. Stress, burnout and coping among emergency physicians at a major hospital in Kingston, Jamaica. West Indian Med J. 2014;63(3):262–266. doi: 10.7727/wimj.2013.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Isaksson Ro KE, Tyssen R, Hoffart A, Sexton H, Aasland OG, Gude T. A three-year cohort study of the relationships between coping, job stress and burnout after a counselling intervention for help-seeking physicians. BMC Public Health. 2010;10:213. doi: 10.1186/1471-2458-10-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan CY, Sum MY, Lim WS, Chew NW, Samarasekera DD, Adoption Sim K. and correlates of Postgraduate Hospital Educational Environment Measure (PHEEM) in the evaluation of learning environments—a systematic review. Med Teach. 2016;38(12):1248–1255. doi: 10.1080/0142159X.2016.1210108. [DOI] [PubMed] [Google Scholar]
- 8.Kumar S. Burnout in psychiatrists. World Psychiatry. 2007;6(3):186–189. [PMC free article] [PubMed] [Google Scholar]
- 9.Rathod S, Roy L, Ramsay M, Das M, Birtwistle J, Kingdon D. A survey of stress in psychiatrists working in the Wessex Region. Psychiatr Bull. 2000;24:133–136. [Google Scholar]
- 10.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer;; 1984. [Google Scholar]
- 11.McGrath JE. Stress and behavior in organizations. In: Dunnette M, editor. Handbook of Industrial and Organizational Psychology. Chicago, IL: Rand McNally Co Inc; 1976. pp. 1351–1395. [Google Scholar]
- 12.El-Masry R, Ghreiz SM, Shams TM, Helal RM. Perceived stress and burnout among medical students during clinical period. Ibnosina J Med BS. 2012;5(4):179–188. [Google Scholar]
- 13.Pantaleoni JL, Augustine EM, Sourkes BM, Bachrach LK. Burnout in pediatric residents over a 2-year period: a longitudinal study. Acad Pediatr. 2014;14(2):167–172. doi: 10.1016/j.acap.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 14.Wallace SL, Lee J, Lee SM. Job stress, coping strategies, and burnout among abuse-specific counselors. J Employ Couns. 2010;47(3):111–122. [Google Scholar]
- 15.Llera J, Durante E. Correlation between the educational environment and burnout syndrome in residency programs at a university hospital. Arch Argent Pediatr. 2014;112(1):6–11. doi: 10.1590/S0325-00752014000100003. [DOI] [PubMed] [Google Scholar]
- 16.Tsai JC, Chen CS, Sun IF, Liu KM, Lai CS. Clinical learning environment measurement for medical trainees at transitions: relations with socio-cultural factors and mental distress. BMC Med Educ. 2014;14:226. doi: 10.1186/1472-6920-14-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roff S, McAleer S, Skinner A. Development and validation of an instrument to measure the postgraduate clinical learning and teaching educational environment for hospital-based junior doctors in the UK. Med Teach. 2005;27(4):326–331. doi: 10.1080/01421590500150874. [DOI] [PubMed] [Google Scholar]
- 18.Mahendran R, Broekman B, Wong JC, Lai YM, Kua EH. The educational environment: comparisons of the British and American postgraduate psychiatry training programmes in an Asian setting. Med Teach. 2013;35(11):959–961. doi: 10.3109/0142159X.2013.815707. [DOI] [PubMed] [Google Scholar]
- 19.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 20.Demerouti E, Mostert K, Bakker AB. Burnout and work engagement: a thorough investigation of the independency of both constructs. J Occup Health Psychol. 2010;15(3):209–222. doi: 10.1037/a0019408. [DOI] [PubMed] [Google Scholar]
- 21.Carver CS. You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 22.Hair JF, Ringle CM, Sarstedt M. Partial least squares structural equation modeling: rigorous applications, better results and higher acceptance. Long Range Planning. 2013;46(1):1–12. [Google Scholar]
- 23.Ringle CM, Wende S, Becker JM. SmartPLS 3. 2015 http://www.smartpls.com Accessed May 30, 2019.
- 24.Hutcheson G, Sofroniou N. The Multivariate Social Scientist: Introductory Statistics Using Generalized Linear Models. London, UK: SAGE Publications Ltd;; 1999. [Google Scholar]
- 25.Stevens JP. Applied Multivariate Statistics for the Social Sciences. Hillsdale, NJ: Erlbaum;; 1992. [Google Scholar]
- 26.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 27.Alosaimi FD, Kazim SN, Almufleh AS, Aladwani BS, Alsubaie AS. Prevalence of stress and its determinants among residents in Saudi Arabia. Saudi Med J. 2015;36(5):605–612. doi: 10.15537/smj.2015.5.10814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldhagen BE, Kingsolver K, Stinnett SS, Rosdahl JA. Stress and burnout in residents: impact of mindfulness-based resilience training. Adv Med Educ Pract. 2015;6:525–532. doi: 10.2147/AMEP.S88580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Navines R, Olive V, Ariz J, Lopez J, Tortajada M. Stress and burnout during the first year of residence training in a university teaching hospital: preliminary date. Dual Diagn Open Acc. 2016;1:17. doi: 10.21767/2472-5048.100017. [DOI] [Google Scholar]
- 30.Dunham J. Stress in Teaching 2nd ed. London, UK: Routledge;; 1992. [Google Scholar]
- 31.Fernet C, Austin S, Trépanier SG, Dussault M. How do job characteristics contribute to burnout? Exploring the distinct mediating roles of perceived autonomy, competence, and relatedness. Eur J Work Organ Psychol. 2013;22(2):123–137. [Google Scholar]
- 32.Steese S, Dollette M, Phillips W, Hossfeld E, Matthews G, Taormina G. Understanding girls' circle as an intervention on perceived social support, body image, self-efficacy, locus of control, and self-esteem. Adolescence. 2006;41(161):55–74. [PubMed] [Google Scholar]
- 33.Knowles M. The Adult Learner: A Neglected Species. Houston, TX: Gulf Publishing Co;; 1979. [Google Scholar]
- 34.Abedini NC, Stack SW, Goodman JL, Steinberg KP. “It's not just time off”: a framework for understanding factors promoting recovery from burnout among internal medicine residents. J Grad Med Educ. 2018;10(1):26–32. doi: 10.4300/JGME-D-17-00440.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.