Setting and Problem
“The limited number of health professionals in many low- and middle-income countries are not distributed evenly across the population. In general, deploying doctors, nurses, and other professionals to remote rural areas is difficult and care givers tend to be concentrated in major urban areas.”1 This statement rings very true in Papua New Guinea (PNG), where the proportion of the population living in rural areas is 86%, the second highest in the world.2 The health challenges facing rural populations are summed up by the “inverse care law” of Julian Tudor Hart: “Availability of good medical care tends to vary inversely with the need of the population served.”3 To improve access to health care in rural areas, health professionals must be moved to where these great needs exist (see the Figure for the current distribution of physicians).
Figure.
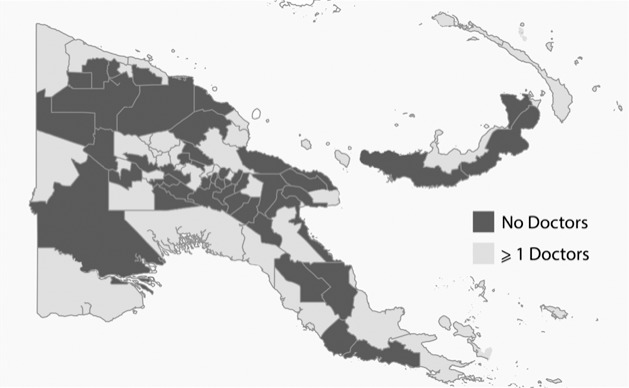
Physicians in Papua New Guinea by District
Postgraduate training of physicians can be strategically positioned in rural communities to facilitate the provision of services and increase the likelihood that graduates of these programs will continue serving in these areas. The generalist or primary care physician is the focal point of this effort, and should be capable of dealing with a wide variety of clinical problems as well as promoting community health and managing a health care facility.
Intervention
A new rural graduate medical education program to train rural specialists began in PNG in 2008. The aim is to provide physicians who are capable of managing a rural health facility for the large underserved rural population of this nation. “The awarding of this degree follows supervised experience and demonstration of general and specific competencies in the clinical disciplines, supervised postgraduate training in a district hospital setting, and postgraduate training in aspects of public health and health administration.”4 In addition to supervised clinical instruction and maintaining a log of cases and clinical problems, curriculum elements are specific to PNG's rural health care needs, such as practical skills training in ultrasonography, solar power module and radio installation, and management and leadership training. Candidates are given 4 to 8 years to complete the curriculum while providing services under the sponsorship of a district hospital. Completion of the training and recognition as a specialist in rural medicine also requires completion and presentation of a research project accepted by the University of Papua New Guinea (UPNG) postgraduate committee and passing a 2-part examination, including a common core and a specialty-specific component. The MMed (Rural) degree is recognized by the National Department of Health and holds pending approval of the PNG Medical Board as a specialist qualification equivalent to the MMed in any other discipline.4
Outcomes to Date
Fifteen PNG physicians have trained in the MMed (Rural) program since 2008. In a nation with as few as 333 physicians and 36 graduating physicians per year, this represents almost 5% of the physician workforce.5 To date, 6 have graduated and all are currently practicing outside of the capitol city of Port Moresby, where the majority of the country's physicians are located. Five physicians are currently enrolled in the program, undertaking their postgraduate education in rural or district hospitals, and 4 left training before completing the program. The UPNG postgraduate selection committee is currently considering applications for 2 additional rural posts at Misima Island and Kainantu (personal correspondence, PNG Society for Rural & Remote Health, November 22, 2018).
In 2009, the PNG Society for Rural & Remote Health was formed in an effort to generate interest in and discussion about the health needs of rural Papua New Guineans. The society meets annually around the time of the PNG Medical Symposium and provides a forum for individuals practicing in rural health and residents in the training program to leverage ideas.
The challenges of shifting the physician workforce to areas that serve PNG's rural majority are significant. The creation of the MMed (Rural) postgraduate program is an important new step to address this problem, which could serve as a template for other nations facing similar difficulties.
References
- 1.Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, et al. Priorities in Health. Washington, DC: The World Bank; 2006. [PubMed] [Google Scholar]
- 2.The World Bank Group. Papua New Guinea. 2019 https://data.worldbank.org/country/papua-new-guinea Accessed June 24.
- 3.Black N, Gruen R. Understanding Health Services. Maidenhead, England: Open University Press;; 2005. [Google Scholar]
- 4.University of Papua New Guinea School of Medicine and Health Sciences. The Master of Medicine. Rural Health Training Handbook. 20112019 http://www.pngruralsociety.org/mmed-rural-program Accessed June 24.


