Abstract
Background
Investments in training physician specialists through postgraduate medical education (PGME) are critical for Sub-Saharan Africa, given the increasing burden of non-communicable diseases.
Objectives
The objectives of this scoping review were to (1) understand the breadth of publications on PGME from Sub-Saharan Africa, and (2) conduct a thematic analysis of lessons learned by specific training programs.
Methods
We conducted a literature search of 7 databases for PGME literature published between January 1991 and December 2016. Two reviewers independently reviewed titles and abstracts for inclusion. Full-text articles were then reviewed, and bibliometric data were extracted to create a profile of PGME-related publications. Two authors coded the manuscripts to identify articles written about specific PGME programs. These were analyzed for lessons learned.
Results
We identified 813 publications that reported on postgraduate medical education in Sub-Saharan Africa. Most articles were published between 2005 and 2016. Nations leading in publication were South Africa and Nigeria, followed by Ethiopia, Uganda, Kenya, Ghana, and Malawi. The largest number of articles related to general surgery training, followed by family medicine, emergency medicine, and anesthesiology. Thematic analysis revealed advantages of training programs for health facilities, challenges related to teaching, resourcing, and standardizing of training, and lessons learned related to international partnerships, faculty engagement, and research support for trainees.
Conclusions
PGME in Sub-Saharan Africa has evolved over the past 26 years. Future growth will require strategic support to scale programs, support new specialties, trainees, and teachers, and leverage best practice models to sustain PGME programs.
Introduction
In the last decade, improving medical education in Sub-Saharan Africa has been a key component of strengthening health systems in the region. Investments in the health workforce are timely given the increasing burden of non-communicable diseases, the need for transformation of health systems to manage chronic illness, and the desire for improved access and coverage.1–3 Africa's health workforce expansion strategies have relied on scaling up of frontline providers, which results in an increased need and demand for medical specialists to manage complex cases and to provide management and leadership in health systems.3–5
The Sub-Saharan African Medical School Study (SAMSS) published in 2011 estimated there were 168 medical schools in Sub-Saharan Africa.6 Most African medical schools admit directly from high school and training programs range from 5 to 7 years.6 Some countries require compulsory service upon graduation, after which physicians can choose to directly enter the workforce or to embark on postgraduate medical education (PGME), the equivalent of graduate medical education in the United States.6 Reports suggest that 20% to 40% of physicians leave the country after graduating from an African medical school.6,7 The limited PGME capacity in Sub-Saharan Africa plays a significant role in this outmigration, and many who pursue specialty training abroad never return.7–10
PGME positions in the region are sponsored by governments, district hospitals or rural hospitals, or trainees may be self-sponsored.11,12 Most programs are affiliated with universities that confer a Master of Medicine degree. Some programs are affiliated to a regional body such as the West African College of Surgeons (WACS) or the College of East, Central, and Southern African Surgeons (COSECSA).13,14
Over the past 15 years, a substantial scale-up of undergraduate medical education (UME) has occurred in Sub-Saharan Africa, with many governments substantially increasing medical school enrollment.15 In Kenya, the University of Nairobi saw a 3-fold increase in class sizes,16 while the number of medical schools in Ethiopia increased from 5 in 2003 to 23 in 2009, and enrollment at Addis Ababa University grew from 100 to more than 300 per year.17 Capacity was further expanded by the US-funded Medical Education Partnership Initiative (MEPI), which supported workforce investments in Africa with $150 million granted to 12 countries to strengthen medical and health professions education.18
The expansion in UME has not been matched by increases in PGME capacity, and the specialist workforce in Africa is substantially inadequate, with shortages in many specialties.13,15,19,20 The SAMSS study identified only 436 PGME programs in the region.6 Strategic expansion of specialist training programs would benefit from understanding the lessons that can be learned from existing programs.
The objectives of this scoping review were 2-fold: (1) to understand the breadth of PGME publications from Sub-Saharan Africa, and (2) to conduct a thematic analysis of publications that reported on specific training programs and to aggregate lessons that can be learned from their experience.
Methods
We conducted a scoping review using methodological guidelines outlined by the Joanna Briggs Institute.21
Data Sources and Search
We searched 4 major international academic databases (PubMed, Global Health, ERIC, and Embase) and 3 Africa-specific databases for PGME literature published between January 1991 and December 2016. African Indicus Medicus is produced by the Association for Health Information and Libraries in Africa with technical support from the World Health Organization. African Journals OnLine is a non-profit initiated by the International Network for the Availability of Scientific Publications. Bioline is a nonprofit scholarly publishing cooperative committed to providing open access to quality research journals published in developing countries.
For the international academic databases, we used a search strategy built on the premise that relevant literature on PGME would contain title or keywords and be assigned categories that referenced education or training, a specific clinical specialty as well as a country in Sub-Saharan Africa. A list of clinical specialties was constructed by first including all those already identified by the Sub-Saharan African Medical School Survey conducted in 2010,6 and then adding all clinical specialties listed as MESH titles under medicine that were deemed relevant by a process of consensus by the study team. A list of Sub-Saharan African countries was retrieved from the US Library of Congress website.22 An experienced librarian (T.H.) created search strategies based on these lists, which were further refined through team discussion. The final list of specialties and countries included in the search and the final search string used for PubMed are provided as supplemental material.
The 3 Africa-specific databases were searched using word strings of 3 to 5 keywords. We conducted an initial electronic search using the terms “education” or “training” and manually sorted titles to include those that referenced education or training programs in clinical specialties in Sub-Saharan African nations.
Google Translate was used to machine translate titles and abstracts in non-English language journals. Duplicate entries present in more than 1 database were identified using RefWorks web-based bibliographic management software (RefWorks-COS, Bethesda, MD), and removed.
Inclusion Criteria and Screening
Articles eligible for our scoping review were published between 1991 and 2016 and focused on PGME programs in Sub-Saharan Africa that produced graduates eligible for an in-country license to practice. We included editorials and review articles as these may also contain useful information.
At the first level of screening, 2 reviewers independently reviewed titles and abstracts to check if they met inclusion criteria. To ensure interrater reliability, the authors collectively reviewed a smaller subset of articles prior to commencing screening on the full dataset. At the second level of screening, full-text articles were reviewed, and bibliometric data were extracted to create a profile of publications.
The second objective of this study was to understand the lessons learned from the perspective of training programs that were published during the time frame of our analysis. To accomplish this, 2 authors (Z.T. and L.N.) sorted the full dataset, reviewed the title, abstract, and text, and extracted publications referring to specific programs and lessons learned. We excluded publications that reflected broadly on the health system and did not specifically discuss a PGME program.
For the dataset of program-related publications, each full-text manuscript was reviewed by an author (Z.T.) who has experience with medical education in Sub-Saharan Africa, including visiting faculty appointments at 2 African institutions. Lessons learned were extracted and categorized in an Excel spreadsheet according to topics selected by the authors based on common attributes identified during the scoping review, relevance to scaling PGME, and alignment with US GME accreditation requirements.23 These topics included faculty, residents, recruitment and retention, the educational program, financing and planning, resources, and program outcomes. Within each topic, themes were identified and summarized.
This review did not involve research with human subjects and was exempt from institutional review board approval.
Results
A search of the 4 international databases yielded 7129 citations. An additional 156 citations were found in the African databases. Following removal of duplicates, 6267 citations remained. The titles and abstracts of each citation were independently screened by 2 authors (Z.T. and L.N.) for eligibility, resulting in the exclusion of 5367 citations. For 900 publications that met initial inclusion criteria, the full text was screened by the same authors, and 87 publications were excluded. The selection schema is shown in Figure 1. Overall, 813 publications met the inclusion criteria, and the final subset of publications relating to specific programs encompassed 140 publications.
Figure 1.
Scoping Review Schematic
Bibliometrics
Most articles identified through the scoping review were published in the latter years of the search window, between 2005 and 2016 (Figure 2). This included a surge in publication in 2005 and 2010, with a continuing trend through 2016. Leading in publication were South Africa (192 articles) and Nigeria (104 articles), followed by Ethiopia, Uganda, Kenya, Ghana, and Malawi (Figure 3). The largest number of PGME articles by specialty related to general surgery training programs, followed by family medicine, emergency medicine, and anesthesiology (Figure 4).
Figure 2.
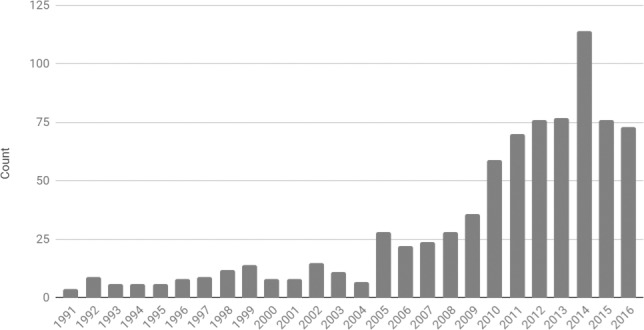
Publications Related to Postgraduate Medical Education in Sub-Saharan Africa (by Year of Publication)a
a N = 813.
Figure 3.

Publications Related to Postgraduate Education in Sub-Saharan Africa (by Country)a
a N = 813.
Figure 4.

Publications Related to Postgraduate Education in Sub-Saharan Africa (by Specialty)a
a N = 813.
Most publications that related to a specific PGME program were published in 2005 or later, and the majority were from the fields of surgery, emergency medicine, and family medicine (provided as supplemental material). Countries represented in this sample included Ethiopia, South Africa, and Nigeria, in addition to articles from Ghana, Rwanda, Uganda, Tanzania, Malawi, and Zambia (provided as supplemental material).
Thematic Analysis of Lessons Learned From Specific PGME Programs
Educational Programs:
Programs reported on efforts to develop locally relevant curricula by reviewing case data from local specialists.24–28 Programs also reflected on the lack of relevant standards to guide education, and the need to ensure locally relevant curricula especially when international partners were involved.26,28,29–38 Suggestions included having partners co-develop curricula to ensure local relevance.30,31,39–44
District hospitals often were described as optimal training sites, especially for procedural skills and more hands-on training.45–50 Some programs reported inadequate case volumes for specialized procedures, and used case simulation and/or off-site rotations (both in and out-of-country) to augment clinical training.51–58 In addition to clinical skills, a number of programs identified a need to improve training in administration and management, finance, and teaching and research.40,43,51,59–69
Research requirements and access to procedures were cited as reasons for graduation delays for some trainees.70 Programs reported residents found research requirements difficult to meet, due to inadequate research skills, lack of mentors, funding, and time.33,69,71–75 Several programs reported that international partnerships provided assistance for research activities.31,75–77 In Uganda, the national Orthopedic Association established a journal to facilitate peer-review dissemination of research findings.71 Another challenge leading to suboptimal training were medical students, who overwhelmed local clinical capacity, and thus limited PGME trainee access to procedures.11,78–80
Resident Recruitment, Support, and Well-Being:
A number of programs reflected on factors that influenced recruitment to their specialty such as perceived workload, quality of life, unpredictability of training duration, and unclear path to licensure.71,81–84
Several publications reported residents experienced high rates of stress and fatigue related to their considerable workload.85–88 One study indicated this occurred for nearly 90% of residents, and attributed it to the lack of facilities and an unstructured program.87 Another study reported surgery trainees worked more than 105 hours per week.88
Supervising Faculty:
Supervision of trainees was provided either by in-country specialists (consultants) or visiting faculty. Challenges related to in-country specialists included inadequate incentives and inconsistent quality and frequency of teaching. Surgical programs, in particular, reported variable supervision of procedures, particularly emergency procedures by on-call residents.62,74,75,78,89–92 Programs described tension between learning and service, with residents reporting inadequate bedside teaching and relying on each other for learning.61,93–96 A challenge faced by some university-based programs was difficulty in influencing the quality of clinical teaching, especially with faculty employed by the ministry of health or the hospital.27,64,75,90,92
A number of publications reflected on the contribution of visiting faculty and factors that influence their contribution, including experience in different practice settings and the time needed to become familiar with the environment.82,83,93,97 Several publications recommended that the optimal approach is to leverage visiting faculty to build local education capacity.19,42,44,98–100
Newer Specialties Face Unique Challenges
Family medicine and emergency medicine services were evolving specialties in the PGME literature from Sub-Saharan Africa, and programs described efforts to garner support from the public, policy makers, regulators, and governments to understand the scope of practice in these specialties and ensure career paths for graduates.11,48,64,66,101–107 Programs discussed the need for international partners to help train an initial critical mass of specialists, including faculty, and ensure that curricula prepared graduates to serve as leaders, teachers, and supervisors in these disciplines.11,48,64–66,108,109
Resources and Financing of PGME
Programs reported on suboptimal resources for training, including accommodations, transportation, electricity, safe drinking water, and access to good quality food.35,61 Programs also reported on suboptimal conditions in health facilities, including inadequately maintained equipment, unreliable drug supplies, and inconsistent availability of laboratory and radiology services.36,55,69,75,96,98,110,111 Programs leveraged private sector health facilities and international partners to bridge these gaps.7,55,63,75 Other publications described suboptimal educational resources, including textbooks and difficulty accessing online lectures and videos due to internet connectivity problems.32,35,82,90,95,112–114
Reflections on financing PGME focused on the need to ensure that external funding was aligned with local capacity to sustain activities when funding ceased. Programs emphasized the need to adequately resource teaching hospitals to facilitate training and the importance of allocating funds to biomedical support as a component of equipment purchases and donations.8,36,76,96,101,103,104,111,115–119
Health Care Workforce Priorities and Retention of Graduates in Region
Programs described the need for targeted research on the burden of non-communicable diseases to advocate for the training of specialists and to counter the previous predominant focus on infectious diseases.24,40,63,71,98,118,120,121 Publications also reported on the benefits of simultaneously establishing training programs in fields that are complementary such as surgery and anesthesia.29,71,98,110,122
Programs reported that retention of graduates was influenced by location of training as well as career prospects and employment opportunities after graduation.8,10,66,74,79,92,98,122–127 In several instances, tracking graduates of PGME programs revealed high rates of in-country retention, especially at academic centers. A study of academic faculty at a large hospital in Kenya reported the majority of surgeons on staff were trained locally.79 In Ethiopia, 95% of 30 psychiatrists trained in-country were retained after graduation.32 Similarly, a network of rural hospital-based training programs in 4 African countries reported that all graduates who completed 1 year of compulsory rural service went on to practice in local underserved areas.128
Impact of PGME on Health Care Provision
A number of articles reflected on the positive impact training programs have had on health facilities.8,129,130 One surgery program reported a 20% increase in surgical cases after starting the training program, another saw a 42% increase in gynecologic cases, and a third reported more efficient and evidence-based care especially with the start of daily morning rounds.129,131 Three programs reported a reduction in morbidity and mortality as a result of training programs.68,102,132
A summary of advantages and challenges faced by PGME programs in the region, and of the lessons learned from their experience is shown in the Box.
Box Lessons From Experience of PGME Programs in Sub-Saharan Africa.
Advantages
Retention: A sizable share of graduates from PGME programs remain in-country, especially at academic centers.
Health outcomes: The presence of PGME programs increased local clinical capacity and resulted in reductions in mortality and morbidity.
Challenges
Clinical training sites: Variable case volumes for specialized procedures, especially at clinical sites that also train medical students.
Locally relevant curricula and standards: The dearth of local PGME standards and lack of relevant curricula in some specialties.
Resource constraints: Inadequate resources and suboptimal learning conditions in settings, including limited access to key clinical and educational resources.
Supervision: Inconsistent supervision and bedside teaching, and residents relying on each other for learning.
Trainees: High rates of stress for many trainees, particularly in specialties with high work hours.
Lessons Learned
Faculty engagement and training: Enhance faculty preparation and incentives for supervising and teaching trainees.
Diversify clinical training sites: District hospital offer rich procedural skills training.
Strategic partnerships: Leverage the contributions of international partners to develop curricula, enhance teaching, and ensure an initial cadre of trained educators in new specialties.
Establish programs in complementary specialties, such as surgery and anesthesiology.
Enhance trainee preparation, assistance, and mentoring for the dissertation and provide peer-reviewed venues for publishing resident research and dissertations.
Provide data on the financial, clinical, and human burden of non-communicable diseases to regulators and policy makers to advocate specialist training.
Discussion
This is the first study that aggregated the PGME literature from Sub-Saharan Africa over a 26-year period (1991–2016) and examined the lessons learned from programs that published on their experience. The vast majority of articles were published after 2010, coinciding with the MEPI program. Poignantly, more than 90% of the articles published after 2014 are from countries that received MEPI funding.
Surgical training programs contributed the greatest number of articles to the literature. This likely reflects the relative maturity of the specialty, and the efforts of WACS and COSECSA and the South African College of Surgeons spanning more than 5 decades.8,14,128 Regulatory bodies and professional associations can be catalysts and resources for new and established programs. Along with internal medicine, the relatively new specialties of emergency medicine and family medicine were commonly mentioned. Publications in these specialties are largely recent and also reflect the efforts and benefits of international partners in medical education research.
The thematic analysis reveals much of what would be expected of physician training in resource-constrained settings, often with little formal organization of PGME programs. A number of expected challenges were reported, but there also are critical gaps in the literature. Little is written about funding models for PGME, particularly approaches that can be scaled up and are sustainable over time. There is a dearth of literature on program oversight, the role of sponsoring institutions, the functions of program directors, and the role of residents in improving and shaping the programs in which they train. In addition, few publications to date have addressed resident well-being and burnout, despite increasing global attention to this topic. Finally, while improvements in health outcomes appear to be correlated to the establishment of physician training, there are no reports in the literature on efforts to track, monitor, or assess the impact of PGME programs, and to date little has been written about educational outcomes, both with respect to graduates' learning attainments and on the impact of their added competencies on health care in the region. More robust research is needed to examine the link between investments in health workforce and improved outcomes for patients and populations.
The review has limitations. Despite the breadth of programs and nations represented, it does not encompass all PGME programs in Sub-Saharan Africa. We also suspect publication bias, with a greater likelihood of publication for programs with international partners, which may have influenced the thematic analysis. The high rate of publication of MEPI-funded projects may reflect the role of external partners in requiring publications as a grant-related activity. Programs and initiatives without international partners and those with limited resources may not have sought publication because of limited capacity and experience with medical education research.
Conclusion
Similar to the United States, the scale-up of graduate medical education is lagging behind medical school expansion. In Sub-Saharan Africa investments will be needed to expand programs, support training in additional specialties, and improve the regulatory environment for specialist training in the region. Regulation, either at the national, regional, or even transnational level, will be critical to ensure trainee well-being, the commitment of teachers, and the use of best practice models in establishing and sustaining PGME programs. Finally, it is important to document current PGME capacity in Sub-Saharan Africa to establish a baseline for strategic investments to meet the demands of evolving health systems, disease patterns, and population health needs.
Supplementary Material
References
- 1.The World Bank. Marquez P, Farrington JL. The Challenge of Non-Communicable Diseases and Road Traffic Injuries in Sub-Saharan Africa. 20152019 http://documents.worldbank.org/curated/en/844381468209068874/The-challenge-of-non-communicable-diseases-and-road-traffic-injuries-in-Sub-Saharan-Africa-an-overview Accessed June 27.
- 2.Abdalla M, Kovach N, Liu C, Damp JB, Jahangir E, Hilliard A, et al. The importance of global health experiences in the development of new cardiologists. J Am Coll Cardiol. 2016;67(23):2789–2797. doi: 10.1016/j.jacc.2015.10.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Global strategy on human resources for health: workforce 2030. 20162019 https://www.who.int/hrh/resources/globstrathrh-2030/en Accessed June 27.
- 4.Malope S, Nkholongo E, Shaw K, Penti B, Schumacher R, Markuns J, et al. Development of a family medicine specialty training program in Lesotho. Lancet. 2016;4(suppl 13):39–40. doi: 10.1016/S2214-109X(16)30018-3. [DOI] [Google Scholar]
- 5.Bac M, Bergh AM, Etsane ME, Hugo J. Medical education and the quality improvement spiral: A case study from Mpumalanga, South Africa. African J Prim Heal Care Fam Med. 2015;7(1):1–10. doi: 10.4102/phcfm.v7i1.738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen C, Buch E, Wassermann T, Frehywot S, Mullan F, Omaswa F, et al. A survey of Sub-Saharan African medical schools. Hum Resour Health. 2012;10(1):4. doi: 10.1186/1478-4491-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greysen SR, Dovlo D, Olapade-Olaopa EO, Jacobs M, Sewankambo N, Mullan F. Medical education in Sub-Saharan Africa: a literature review. Med Educ. 2011;45(10):973–986. doi: 10.1111/j.1365-2923.2011.04039.x. [DOI] [PubMed] [Google Scholar]
- 8.Qureshi JS, Young S, Muyco AP, Borgstein E, Charles AG, Mulwafu W, et al. Addressing Malawi's surgical workforce crisis: A sustainable paradigm for training and collaboration in Africa. Surgery. 2013;153(2):272–281. doi: 10.1016/j.surg.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 9.Rubagumya F, Hrdy M, Uwase MA, Kamanzi B. Physician brain drain in Sub-Saharan Africa: the career plans of Rwanda's future doctors. Rwanda Med J. 2016;53(1):5–10. [Google Scholar]
- 10.Clinton Y, Anderson FW, Kwawukume EY. Factors related to retention of postgraduate trainees in obstetrics-gynecology at the Korle-Bu Teaching Hospital in Ghana. Acad Med. 2010;85(10):1564–1570. doi: 10.1097/ACM.0b013e3181f09112. [DOI] [PubMed] [Google Scholar]
- 11.Martel J, Oteng R, Mould-Millman NK, Bell SA, Zakariah A, Oduro G, et al. The development of sustainable emergency care in Ghana: physician, nursing and prehospital care training initiatives. J Emerg Med. 2014;47(4):462–468. doi: 10.1016/j.jemermed.2014.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mandeville KL, Ulaya G, Lagarde M, Gwesele L, Dzowela T, Hanson K, et al. Early career retention of malawian medical graduates: a retrospective cohort study. Trop Med Int Heal. 2015;20(1):106–114. doi: 10.1111/tmi.12408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rickard J. Systematic review of postgraduate surgical education in low- and middle-income countries. World J Surg. 2016;40(6):1324–1335. doi: 10.1007/s00268-016-3445-x. [DOI] [PubMed] [Google Scholar]
- 14.Bode CO, Nwawolo CC, Giwa-Osagie OF. Surgical education at the West African College of Surgeons. World J Surg. 2008;32(10):2162–2166. doi: 10.1007/s00268-008-9710-x. [DOI] [PubMed] [Google Scholar]
- 15.Kilmarx PH, Katz F, Razak MH, Palen J, Cheever LW, Glass RI. The medical education partnership initiative: strengthening human resources to end AIDS and improve health in Africa. 2018] doi: 10.1097/ACM.0000000000002489. [published online ahead of print October 16, [DOI] [PMC free article] [PubMed]
- 16.Kibore MW, Daniels JA, Child MJ, Nduati R, Njiri FJ, Kinuthia RM, et al. Kenyan medical student and consultant experiences in a pilot decentralized training program at the University of Nairobi. Educ Heal (Abingdon) 2015;27(2):170–176. doi: 10.4103/1357-6283.143778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Derbew M, Animut N, Talib ZM, Mehtsun S, Hamburger EK. Ethiopian medical schools' rapid scale-up to support the government's goal of universal coverage. Acad Med. 2014;89(suppl 8):40–44. doi: 10.1097/ACM.0000000000000326. [DOI] [PubMed] [Google Scholar]
- 18.Mullan F, Frehywot S, Omaswa F, Sewankambo N, Talib Z, Chen C, et al. The Medical Education Partnership Initiative: PEPFAR'S effort to boost health worker education to strengthen health systems. Health Aff (Millwood) 2012;31(7):1561–1572. doi: 10.1377/hlthaff.2012.0219. [DOI] [PubMed] [Google Scholar]
- 19.Sherman CB, Carter EJ, Braendli O, Getaneh A, Schluger NW. The East African training initiative: a model training program in pulmonary and critical care medicine for low-income countries. Ann Am Thorac Soc. 2016;13(4):451–455. doi: 10.1513/AnnalsATS.201510-673OC. [DOI] [PubMed] [Google Scholar]
- 20.Osanjo GO, Oyugi JO, Kibwage IO, Mwanda WO, Ngugi EN, Otieno FC, et al. Building capacity in implementation science research training at the University of Nairobi. Implement Sci. 2016;11(1):30. doi: 10.1186/S13012-016-0395-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peters MD, Godfrey CM, Khalil H, Mcinerney P, Parker D, Soares BC. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–146. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 22.The Library of Congress. Africana Collections. List of Sub-Saharan African Countries. 2019 https://www.loc.gov/rr/amed/guide/afr-countrylist.html Accessed June 27.
- 23.Accreditation Council for Graduate Medical Education. Common Program Requirements. 2019 https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRs_2017-07-01.pdf Accessed June 27.
- 24.Brouillette MA, Kaiser SP, Konadu P, Kumah-Ametepey RA, Aidoo AJ, Coughlin RC. Orthopedic surgery in the developing world: workforce and operative volumes in Ghana compared to those in the United States. World J Surg. 2014;38(4):849–857. doi: 10.1007/s00268-013-2314-0. [DOI] [PubMed] [Google Scholar]
- 25.Cunningham S, McFelea J. Graduating residents' perspectives of the influence of orthopedic residency training on professional development in Nairobi, Kenya. Man Ther. 2016;25(1009):e164. doi: 10.1016/j.math.2016.05.604. [DOI] [Google Scholar]
- 26.Baird R, Poenaru D, Ganey M, Hansen E, Emil S. Partnership in fellowship: comparative analysis of pediatric surgical training and evaluation of a fellow exchange between Canada and Kenya. J Pediatr Surg. 2016;51(10):1704–1710. doi: 10.1016/j.jpedsurg.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 27.Mutabdzic D, Bedada AG, Bakanisi B, Motsumi J, Azzie G. Designing a contextually appropriate surgical training program in low-resource settings: the Botswana experience. World J Surg. 2013;37(7):1486–1491. doi: 10.1007/s00268-012-1731-9. [DOI] [PubMed] [Google Scholar]
- 28.Rickard JL, Ntakiyiruta G, Chu KM. Identifying gaps in the surgical training curriculum in Rwanda through evaluation of operative activity at a teaching hospital. J Surg Educ. 2015;72(4):73–81. doi: 10.1016/j.jsurg.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 29.Lipnick M, Mijumbi C, Dubowitz G, Kaggwa S, Goetz L, Mabweijano J, et al. Surgery and anesthesia capacity-building in resource-poor settings: description of an ongoing academic partnership in Uganda. World J Surg. 2013;37(3):488–497. doi: 10.1007/s00268-012-1848-x. [DOI] [PubMed] [Google Scholar]
- 30.Swan MC. Plastic surgery fellowships in the developing world: a Ugandan experience. Ann Plast Surg. 2011;67(4):326–328. doi: 10.1097/SAP.0b013e3182069ae8. [DOI] [PubMed] [Google Scholar]
- 31.Freudenberg S, Mkony C, Wilhelm T, Post S. The role of inter-institutional cooperation in surgical training and practice: a German-Tanzanian model. Inter-Institutional Cooperation Surg Train Pract. 2004;9(2):5–8. [Google Scholar]
- 32.Cadotte DW, Blankstein M, Bekele A, Dessalegn S, Pain C, Derbew M, et al. Establishing a surgical partnership between Addis Ababa, Ethiopia, and Toronto, Canada. Can J Surg. 2013;56(3):19–23. doi: 10.1503/cjs.027011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Love TP, Martin BM, Tubasiime R, Srinivasan J, Pollock JD, Delman KA. Emory global surgery program: learning to serve the underserved well. J Surg Educ. 2015;72(4):46–51. doi: 10.1016/j.jsurg.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 34.Pust R, Dahlman B, Khwa-Otsyula B, Armstrong J, Downing R. Partnerships creating postgraduate family medicine in Kenya. Fam Med. 2006;38(9):661–666. [PubMed] [Google Scholar]
- 35.Ogundipe RM, Mash R. Development of family medicine training in Botswana: views of key stakeholders in Ngamiland. Afr J Prim Heal Care Fam Med. 2018;7(1):1–9. doi: 10.4102/phcfm.v7i1.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zebenigus M, Zenebe G, Bower JH. Neurology training in Africa: the Ethiopian experience. Nat Clin Pract Neurol. 2007;3(7):412–413. doi: 10.1038/ncpneuro0531. [DOI] [PubMed] [Google Scholar]
- 37.Yarmoshuk A, Bocking A, Spitzer R, Caloia D, Orango O, Were E, et al. Improving women's reproductive health in Western Kenya: a North American/African academic model. Int J Gynecol Obstet. 2009;107:S609. doi: 10.1016/S0020-7292(09)62175-5. [DOI] [Google Scholar]
- 38.Teshima J. Teaching child psychiatry in Ethiopia: challenges and rewards. J Can Acad Child Adolesc Psychiatry. 2008;17(3):145–149. [PMC free article] [PubMed] [Google Scholar]
- 39.Lillie E, O'Donohoe L, Shamambo N, Bould D, Ismailova F, Kinnear J. Peer training and co-learning in global health care. Clin Teach. 2015;12(3):193–196. doi: 10.1111/tct.12292. [DOI] [PubMed] [Google Scholar]
- 40.Kaddumukasa M, Katabira E, Salata RA, Costa MA, Ddumba E, Furlan A, et al. Global medical education partnerships to expand specialty expertise: a case report on building neurology clinical and research capacity. Hum Resour Health. 2014;12(1):1–9. doi: 10.1186/1478-4491-12-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hill W, Small M, Magriples U, Chazotte C, Judge N, Tropper P, et al. 242: global health opportunities for the MFM specialists in the human resources for health (HRH) program in Rwanda. Am J Obstet Gynecol. 2015;212(1):S133. doi: 10.1016/j.ajog.2014.10.288. [DOI] [Google Scholar]
- 42.Mangezi WO, Nhiwatiwa SM, Cowan FM, Chibanda D, Hakim J, Lund C, et al. Improving psychiatric education and research capacity in Zimbabwe. Med Educ. 2014;48(11):1132–1132. doi: 10.1111/medu.12554. [DOI] [PubMed] [Google Scholar]
- 43.Alem A, Pain C, Araya M, Hodges BD. Co-creating a psychiatric resident program with Ethiopians, for Ethiopians, in Ethiopia: the Toronto addis ababa psychiatry project (TAAPP) Acad Psychiatry. 2010;34(6):424–432. doi: 10.1176/appi.ap.34.6.424. [DOI] [PubMed] [Google Scholar]
- 44.Bould MD, Clarkin CL, Boet S, Pigford AA, Ismailova F, Measures E, et al. Faculty experiences regarding a global partnership for anesthesia postgraduate training: a qualitative study. Can J Anesth. 2015;62(1):11–21. doi: 10.1007/s12630-014-0252-4. [DOI] [PubMed] [Google Scholar]
- 45.Sanders DL, Bell DC. Worlds apart: training in rural South Africa. Clin Teach. 2012;9(2):99–104. doi: 10.1111/j.1743-498X.2011.00503.x. [DOI] [PubMed] [Google Scholar]
- 46.Yogeswaran P, O'Mahony D, Mfenyana K. Community-based education for registrars in family medicine at Walter Sisulu University. South African Fam Pract. 2011;53(3):287–288. doi: 10.1080/20786204.2011.10874101. [DOI] [Google Scholar]
- 47.Du Plessis D, Kapp PA, Jenkins LS, Giddy L. Postgraduate training for family medicine in a rural district hospital in South Africa: appropriateness and sufficiency of theatre procedures as a sentinel indicator. Afr J Prim Health Care Fam Med. 2016;8(1):1–7. doi: 10.4102/phcfm.v8i1.1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sanders J, Goma F, Kafumukache E, Ngoma M, Nzala S. Developing a family medicine postgraduate training program in Zambia. Fam Med. 2016;48(7):517–522. [PubMed] [Google Scholar]
- 49.Drislane FW, Akpalu A, Wegdam HHJ. Establishment of a general medicine residency training program in rural West Africa. Yale J Biol Med. 2014;87(3):327–339. [PMC free article] [PubMed] [Google Scholar]
- 50.Ghebre R, Magriples U, Bagambe P, Petersen R, Ellis D, Small M, et al. Human resources for health (HRH) program in Rwanda: in the gynaecology clinic: an African perspective. Int J Gynaecol Obstet. 2015;5:74–75. [Google Scholar]
- 51.Ekenze SO, Ameh EA. Evaluation of relevance of the components of pediatric surgery residency training in West Africa. J Pediatr Surg. 2010;45(4):801–805. doi: 10.1016/j.jpedsurg.2009.10.051. [DOI] [PubMed] [Google Scholar]
- 52.Martins D, Amado V, Johnson B, et al. Case volume distribution in the Mozambican pediatric general surgery training unit. J Surg Res. 2014;186(2):550–551. doi: 10.1016/j.jss.2013.11.452. [DOI] [Google Scholar]
- 53.Lakhoo K, Msuya D. Global health: a lasting partnership in paediatric surgery. Afr J Paediatr Surg. 2015;12(2):114. doi: 10.4103/0189-6725.160351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wen LS, Nagurney JT, Geduld HI, Wen AP, Wallis LA. Procedure competence versus number performed: a survey of graduate emergency medicine specialists in a developing nation. Emerg Med J. 2012;29(10):822–825. doi: 10.1136/emermed-2011-200584. [DOI] [PubMed] [Google Scholar]
- 55.Caruso N, Chandra A, Kestler A. Development of emergency medicine in Botswana. African J Emerg Med. 2011;1(3):108–112. doi: 10.1016/j.afjem.2011.08.002. [DOI] [Google Scholar]
- 56.Stalsberg H, Awuah B, Ibarra JA, Nsiah-Asare A. Re-establishing a surgical pathology service in Kumasi, Ghana: case report and discussion of barriers and key elements of a successful collaboration between low- and high-resource countries. Cancer. 2008;113(suppl 8):2338–2346. doi: 10.1002/cncr.23830. [DOI] [PubMed] [Google Scholar]
- 57.Bosland M, Titiloye N, Quayson S, Wiley E, Awuah B. Pathology capacity building in Ghana. Ann Glob Heal. 2015;81(1):139–140. doi: 10.1016/j.aogh.2015.02.821. [DOI] [Google Scholar]
- 58.Bueno J, Gay S. Support to radiology residency programs in developing countries: our experience in Uganda with the Mbarara University of Science and Technology. J Am Coll Radiol. 2016;13(9):1121–1125. doi: 10.1016/j.jacr.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 59.Ademuyiwa A, Ameh E, Bode C, Adejuyigbe O. Survey of teaching, research and conference experiences of paediatric surgical trainees in Nigeria. Afr J Paediatr Surg. 2011;8(1):4. doi: 10.4103/0189-6725.78659. [DOI] [PubMed] [Google Scholar]
- 60.Dreyer J, Hannay J, Lane R. Teaching the management of surgical emergencies through a short course to surgical residents in East/Central Africa delivers excellent educational outcomes. World J Surg. 2014;38(4):830–838. doi: 10.1007/s00268-013-2320-2. [DOI] [PubMed] [Google Scholar]
- 61.Anyaehie U, Anyaehie U, Nwadinigwe C, Emegoakor C, Ogbu V. Surgical resident doctor's perspective of their training in the southeast region of Nigeria. Ann Med Health Sci Res. 2012;2(1):19–23. doi: 10.4103/2141-9248.96931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bekele A, Kotisso B, Shiferaw S, Seyoum N. The gap between surgical resident and faculty surgeons concerning operating theatre teaching: report from Addis Ababa, Ethiopia. East Cent Afr J Surg. 2013;18(2):3–6. [Google Scholar]
- 63.De Beer MM, Karusseit VOL, Pienaar BH. Perspectives of South African general surgeons regarding their postgraduate training. South African J Surg. 2014;52(3):67–71. doi: 10.7196/SAJS.1993. [DOI] [PubMed] [Google Scholar]
- 64.Wen LS, Geduld HI. Tobias Nagurney J, Wallis LA. Africa's first emergency medicine training program at the University of Cape Town/Stellenbosch University: history, progress, and lessons learned. Acad Emerg Med. 2011;18(8):868–871. doi: 10.1111/j.1553-2712.2011.01131.x. [DOI] [PubMed] [Google Scholar]
- 65.De Villiers MR, Cilliers FJ, Coetzee F, Herman N, Van Heusden M, Von Pressentin KB. Equipping family physician trainees as teachers: A qualitative evaluation of a twelve-week module on teaching and learning. BMC Med Educ. 2014;14(1):1–10. doi: 10.1186/1472-6920-14-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gossa W, Wondimagegn D, Mekonnen D, Eshetu W, Abebe Z, Fetters M. Key informants' perspectives on development of family medicine training programs in Ethiopia. Adv Med Educ Pract. 2016:261. doi: 10.2147/AMEP.S94522. [DOI] [PMC free article] [PubMed]
- 67.Owolabi MO, Afolabi AO, Omigbodun AO. Performance of residents serving as clinical teachers: a student-based assessment. J Grad Med Educ. 2014;6(1):123–126. doi: 10.4300/JGME-D-13-00130.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Anderson FWJ, Obed SA, Boothman EL, Opare-Ado H. The public health impact of training physicians to become obstetricians and gynecologists in Ghana. Am J Public Health. 2014;104(suppl 1):159–165. doi: 10.2105/AJPH.2013.301581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Abas MA, Nhiwatiwa SM, Mangezi W, Jack H, Piette A, Cowan FM, et al. Building mental health workforce capacity through training and retention of psychiatrists in Zimbabwe. Int Rev Psychiatry. 2014;26(4):453–459. doi: 10.3109/09540261.2014.924487. [DOI] [PubMed] [Google Scholar]
- 70.Sulafa KMA. Paediatric cardiology programs in countries with limited resources: how to bridge the gap. J Saudi Hear Assoc. 2010;22(3):137–141. doi: 10.1016/j.jsha.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.O'Hara NN, O'Brien PJ, Blachut PA. Developing orthopaedic trauma capacity in Uganda. J Orthop Trauma. 2015;29(10):20–22. doi: 10.1097/BOT.0000000000000409. [DOI] [PubMed] [Google Scholar]
- 72.Cancedda C, Riviello R, Rhatigan J, Williams A, Tetuja M, Barrow J, et al. Participation of Harvard Medical School and Brigham and Women's Hospital to a major academic global health initiative: benefits to faculty, trainees, and institutions. Ann Global Health. 2015;81(1):17–18. doi: 10.1016/j.aogh.2015.02.553. [DOI] [Google Scholar]
- 73.Elobu AE, Kintu A, Galukande M, Kaggwa S, Mijjumbi C, Tindimwebwa J, et al. Research in surgery and anesthesia: challenges for post-graduate trainees in Uganda. Educ Health (Abingdon) 2015;28(1):11–15. doi: 10.4103/1357-6283.161826. [DOI] [PubMed] [Google Scholar]
- 74.Wen LS, Geduld HI. Tobias Nagurney J, Wallis LA. Perceptions of graduates from Africa's first emergency medicine training program at the University of Cape Town/Stellenbosch University. Can J Emerg Med. 2012;14(2):97–105. doi: 10.2310/8000.2012.110639. [DOI] [PubMed] [Google Scholar]
- 75.Mocumbi AO, Carrilho C, Aronoff-Spencer E, Funzamo C, Patel S, Preziosi M, et al. Innovative strategies for transforming internal medicine residency training in resource-limited settings: the Mozambique experience. Acad Med. 2014;89(suppl 8):78–82. doi: 10.1097/ACM.0000000000000331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Elobu AE, Kintu A, Galukande M, Kaggwa S, Mijjumbi C, Tindimwebwa J, et al. Evaluating international global health collaborations: perspectives from surgery and anesthesia trainees in Uganda. Surgery. 2014;155(4):585–592. doi: 10.1016/j.surg.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 77.Kakoma JB. Postgraduate and research programmes in medicine and public health in Rwanda: an exciting experience about training of human resources for health in a limited resources country. Pan Afr Med J. 2016;23:1–5. doi: 10.11604/pamj.2016.23.171.8788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ojuka DK, Macleod J, Nyabuto CK. Operative exposure of a surgical trainee at a tertiary hospital in Kenya. Surg Res Pract. 2015;2015:724506. doi: 10.1155/2015/724506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Magoha GA, Ngumi ZW. Training of surgeons in Kenya at the University of Nairobi teaching hospital. East Afr Med J. 1999;76(8):462–464. [PubMed] [Google Scholar]
- 80.Tolhurst H. Australian medical students' intentions in relation to practice location: their short- and long-term time frame. Aust J Rural Health. 2006;14(2):88–90. doi: 10.1111/j.1440-1584.2006.00769.x. [DOI] [PubMed] [Google Scholar]
- 81.Loefler IJ. Are generalists still needed in a specialised world? The renaissance of general surgery. Br Med J. 2000;320(7232):436–438. doi: 10.1136/bmj.320.7232.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ahrens T. Creating change through collaboration: a twinning partnership to strengthen emergency medicine at Addis Ababa University/Tikur Anbessa Specialized Hospital—a model for international medical education partnerships. Missiology An Int Rev. 1977;5(2):141–173. doi: 10.1111/acem.12265. [DOI] [PubMed] [Google Scholar]
- 83.Lockwood J, Azaj A, Berman S, Vaillancourt S, Maskalyk J, Landes M. Examining the current health care milieu of the new Ethiopian emergency medicine system: a qualitative analysis of Ethiopian emergency medicine residents. Can J Emerg Med. 2014;15(suppl 1):97. [Google Scholar]
- 84.Zoumenou E, Lokossou T, Assouto P, Chobli M. Le Polain De Waroux B, Baele P. Anesthesiologists' demography in French-Speaking Sub-Saharan Africa: the impact of fifteen years of Belgo-Beninese cooperation. Acta Anaesthesiol Belg. 2013;64(2):81–89. [PubMed] [Google Scholar]
- 85.Ogundipe OA, Olagunju AT, Lasebikan VO, Coker AO. Burnout among doctors in residency training in a tertiary hospital. Asian J Psychiatr. 2014;10(2014):27–32. doi: 10.1016/j.ajp.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 86.Makama JG, Garba ES. Stress and distress of surgical practice: the trainee's view. Niger J Med. 2008;17(4):383–386. doi: 10.4314/njm.v17i4.37416. [DOI] [PubMed] [Google Scholar]
- 87.Adebamowo CA, Ezeome ER, Ajuwon AJ, Adekunle OO. Job stress associated with surgical training in Nigeria. Afr J Med Med Sci. 1998;27(3–4):233–237. doi: 10.15389/agrobiology.2016.4.475eng. [DOI] [PubMed] [Google Scholar]
- 88.Vadia S, Kahn D. Registrar working hours in Cape Town. S Afr J Surg. 2005;43(3):62–64. [PubMed] [Google Scholar]
- 89.Peer S, Fagan J. Do South African universities provide the required training platforms for otolaryngology specialist training? S Afr Med J. 2012;102(8):691–692. doi: 10.7196/SAMJ.5545. [DOI] [PubMed] [Google Scholar]
- 90.Isaacson G. Framework for advancing otolaryngology: head and neck surgery in Ethiopia. Otolaryngol Head Neck Surg. 2014;151(4):634–637. doi: 10.1177/0194599814542591. [DOI] [PubMed] [Google Scholar]
- 91.Ajao OG, Ajao OO, Ugwu BT, Yawe K, Ezeome ER. Factors determining the results of the examination of the West African College of Surgeons in general surgery. J West Afr Coll Surg. 2014;4(4):1–26. [PMC free article] [PubMed] [Google Scholar]
- 92.Mbuka DO, Tshitenge S, Setlhare V, Tsima B, Adewale G, Parsons L. New family medicine residency training programme: residents' perspectives from the University of Botswana. Afr J Prim Health Care Fam Med. 2016;8(1):e1–e8. doi: 10.4102/phcfm.v8i1.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cadotte DW, Sedney C, Djimbaye H, Bernstein M. A qualitative assessment of the benefits and challenges of international neurosurgical teaching collaboration in Ethiopia. World Neurosurg. 2014;82(6):980–986. doi: 10.1016/j.wneu.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 94.Deckelbaum DL, Gosselin-Tardif A, Ntakiyiruta G, Liberman S, Vassiliou M, Rwamasirabo E, et al. An innovative paradigm for surgical education programs in resource-limited settings. Can J Surg. 2014;57(5):298–299. doi: 10.1503/cjs.001514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yusufu LM, Ahmed A, Odigie VI, Delia IZ, Mohammed AA. Residency training program: perceptions of residents. Ann Afr Med. 2010;9(2):91–94. doi: 10.4103/1596-3519.64745. [DOI] [PubMed] [Google Scholar]
- 96.Enright A. Anesthesia training in Rwanda. Can J Anaesth. 2007;54(11):935–939. doi: 10.1007/BF03026799. [DOI] [PubMed] [Google Scholar]
- 97.Hill W, Ellis D, Kress C, Washington S, Kitessa D, Erber S, et al. The role, opportunities, accomplishments, and implications worldwide of the obstetrician-gynecologist in the human resources for health (HRH) program in Rwanda. Int J Gynecol Obstet. 2015;131(suppl 5):E100. [Google Scholar]
- 98.Riviello R, Ozgediz D, Hsia RY, Azzie G, Newton M, Tarpley J. Role of collaborative academic partnerships in surgical training, education, and provision. World J Surg. 2010;34(3):459–465. doi: 10.1007/s00268-009-0360-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cook M, Howard BM, Yu A, Grey D, Hofmann PB, Moren AM, et al. A consortium approach to surgical education in a developing country: educational needs assessment. JAMA Surg. 2015;150(11):1074–1078. doi: 10.1001/jamasurg.2015.2205. [DOI] [PubMed] [Google Scholar]
- 100.Myers J. Challenges of developing a formal subspecialty pulmonary training program in Kenya. R I Med J. 2013;96(10):20. [PubMed] [Google Scholar]
- 101.Nicks BA, Sawe HR, Juma AM, Reynolds TA. The state of emergency medicine in the United Republic of Tanzania. Afr J Emerg Med. 2012;2(3):97–102. doi: 10.1016/j.afjem.2012.06.002. [DOI] [Google Scholar]
- 102.Mbanjumucyo G, DeVos E, Pulfrey S, Epino HM. State of emergency medicine in Rwanda 2015: An innovative trainee and trainer model. Int J Emerg Med. 2015;8(1):2–4. doi: 10.1186/s12245-015-0067-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Oteng RA, Donkor P. The Ghana emergency medicine collaborative. Acad Med. 2014;89(suppl 8):110–111. doi: 10.1097/ACM.0000000000000319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ramalanjaona G. Emergency medicine in madagascar. Ann Emerg Med. 1998;31(6):766–768. doi: 10.1016/S0196-0644(98)70237-9. [DOI] [PubMed] [Google Scholar]
- 105.Teklu S, Azazh A, Seyoum N, Woldetsadik A, Tupesis JP, Wubben R, et al. Development and implementation of an emergency medicine graduate training program at Addis Ababa University School of Medicine: challenges and successes. Ethiop Med J. 2014;(suppl 2):13–19. [PubMed] [Google Scholar]
- 106.A-Rahman NHA, Jacquet GA. The state of emergency care in the Republic of the Sudan. Afr J Emerg Med. 2014;4(2):55–60. doi: 10.1016/j.afjem.2013.12.002. [DOI] [Google Scholar]
- 107.Malope S, Nkholongo E, Shaw K, Penti B, Schumacher R, Markuns J. Development of a family medicine specialty training program in Lesotho. Lancet Global Health. 2016;4:S13. doi: 10.1016/S2214-109X(16)30018-3. [DOI] [Google Scholar]
- 108.Kabeza AB, George N, Nyundo M, Levine AC. Development of emergency medicine in Rwanda. African J Emerg Med. 2013;3(3):103–109. doi: 10.1016/j.afjem.2012.11.004. [DOI] [Google Scholar]
- 109.Odundo GO, Ngwiri T, Otuoma O, Laigong P, Mukhwana R, Limbe MS, et al. The impact and successes of a paediatric endocrinology fellowship program in Africa. Int J Endocrinol. 2016;2016:1560248. doi: 10.1155/2016/1560248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Fuller A, Tran T, Muhumuza M, Haglund MM. Building neurosurgical capacity in low and middle income countries. eNeurologicalSci. 2016;3:1–6. doi: 10.1016/j.ensci.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mohamed KG, Hunskaar S, Abdelrahman SH, Malik EM. Scaling up family medicine training in Gezira, Sudan—a 2-year in-service master programme using modern information and communication technology: a survey study. Hum Resour Health. 2014;12:3. doi: 10.1186/1478-4491-12-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Rabinowitz DA, Pretorius ES. Postgraduate radiology training in sub-Saharan Africa: a review of current educational resources. Acad Radiol. 2005;12(2):224–231. doi: 10.1016/j.acra.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 113.Obura T, Rees J, Brant W, Parboosingh J, Miller F. Supporting a community of learners by e-mentoring, experiences drawn from a residency program. Int J Gynecol Obstet. 2009;107(suppl):292. doi: 10.1016/S0020-7292(09)61067-5. [DOI] [Google Scholar]
- 114.Adeyekun A. Residents' perception of postgraduate radiology training in Nigeria. West Afr J Med. 2010;29(5):314–317. doi: 10.4314/wajm.v29i5.68251. [DOI] [PubMed] [Google Scholar]
- 115.Osman NB, Almeida ML, Ustá MB, Bique C, David E. Development of a strategic plan by the Mozambican Association of Obstetricians and Gynaecologists: direct and indirect effects. Int J Gynecol Obstet. 2014;127(S1):10–12. doi: 10.1016/j.ijgo.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 116.Babich LP, Bicknell WJ, Culpepper L, Jack BW. Social responsibility, international development, and institutional commitment: lessons from the Boston University experience. Acad Med. 2008;83(2):143–147. doi: 10.1097/ACM.0b013e3181609456. [DOI] [PubMed] [Google Scholar]
- 117.Young S, Banza L, Mkandawire N. The impact of long term institutional collaboration in surgical training on trauma care in Malawi. Springerplus. 2016;5(1) doi: 10.1186/s40064-016-2050-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chillo P, Humphrey SH, Meda J, Kerry VB. Cardiac critical care in resource-limited environments: lessons from Tanzania. Glob Heart. 2014;9(3):311–318. doi: 10.1016/j.gheart.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 119.Magesa P, Makubi A, Makani J, Reid C, Davis B. Poster sessions: General Haematology Dar-Oxford-London link for health: providing postgraduate haematology training (MMed and MSc in haematology) An open label study for the assessment of response to oral ferrous salt supplement in the treatment of ir. 2011. 8(May 2007):2011.
- 120.Twagirumugabe T, Carli F. Rwandan anesthesia residency program: a model of north-south educational partnership. Int Anesthesiol Clin. 2010;48(2):71–78. doi: 10.1097/AIA.0b013e3181dd4f65. [DOI] [PubMed] [Google Scholar]
- 121.Shigidi MM. A nephrology fellowship training program in Sudan: the goals and challenges. Arab J Nephrol Transplant. 2011;4(3):107–108,178,179. [PubMed] [Google Scholar]
- 122.Kinnear JA, Bould MD, Ismailova F, Measures E. A new partnership for anesthesia training in Zambia: Reflections on the first year. Can J Anesth. 2013;60(5):484–491. doi: 10.1007/s12630-013-9905-y. [DOI] [PubMed] [Google Scholar]
- 123.Aswani J, Baidoo K, Otiti J. Establishing a head and neck unit in a developing country. J Laryngol Otol. 2012;126(6):552–555. doi: 10.1017/S0022215112000333. [DOI] [PubMed] [Google Scholar]
- 124.Derbew M, Laytin AD, Dicker RA. The surgical workforce shortage and successes in retaining surgical trainees in Ethiopia: A professional survey. Hum Resour Health. 2016;14(suppl 1):29. doi: 10.1186/s12960-016-0126-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Franey C, Evensen A, Bethune C, Zemenfes D. Emergence of family medicine in ethiopia: an international collaborative education model. Educ Prim Care. 2016;27(3):241–243. doi: 10.1080/14739879.2016.1181531. [DOI] [PubMed] [Google Scholar]
- 126.Martey JO, Elkins TE, Wilson JB, Adadevoh WK, MacVicar J, Sciarra JJ. Innovative community-based postgraduate training for obstetrics and gynecology in West Africa. Obstet Gynecol. 1995;85(6):1042–1046. doi: 10.1016/0029-7844(95)00066-Z. [DOI] [PubMed] [Google Scholar]
- 127.Wilmshurst JM, Morrow B, du Preez A, Githanga D, Kennedy N, Zar HJ. The African Pediatric Fellowship Program: training in Africa for Africans. Pediatrics. 2016;137(1):e20152741. doi: 10.1542/peds.2015-2741. [DOI] [PubMed] [Google Scholar]
- 128.Kingsnorth A, Gyoh S. Is it possible to train surgeons for rural Africa? A report of a successful international program. World J Surg. 2012;36(6):1439–1440. doi: 10.1007/s00268-012-1442-2. [DOI] [PubMed] [Google Scholar]
- 129.Khambaty FM. Surgery in the horn of Africa. Arch Surg. 2010;145(8):749. doi: 10.1001/archsurg.2010.125. [DOI] [PubMed] [Google Scholar]
- 130.Anderson FWJ, Johnson TRB. Capacity building in obstetrics and gynaecology through academic partnerships to improve global women's health beyond 2015. BJOG An Int J Obstet Gynaecol. 2015;122(2):170–173. doi: 10.1111/1471-0528.13176. [DOI] [PubMed] [Google Scholar]
- 131.Kendig C, Tyson A, Young S, Mabedi C, Cairns B, Charles A. The effect of a new surgery residency program on case volume and case complexity in a sub-Saharan African Hospital. J Surg Educ. 2015;72(4):e94–e99. doi: 10.1016/j.jsurg.2014.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Klufio CA, Kwawukume EY, Danso KA, Sciarra JJ, Johnson T. Ghana postgraduate obstetrics/gynecology collaborative residency training program: success story and model for Africa. Am J Obstet Gynecol. 2003;189(3):692–696. doi: 10.1067/S0002-9378(03)00882-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



