Abstract
Background
The coexistence of overweight mother and stunted child at the same household is a type of Double Burden of Malnutrition at Household Level (DBMHL). This particular public health concern is now emerging at an alarming rate among most of the South Asian and its neighboring lower-and-middle income countries which are going through nutritional transition. This study has examined the prevalence rate and the risk factors of DBMHL along with the socio-economic inequality in DBMHL among Bangladesh, Nepal, Pakistan, and Myanmar.
Methods
Latest Demographic and Health Survey datasets were used in this study. To identify the significant association of DBMHL with socio-demographic characteristics, a multivariate technique named as logistic regression model, and for measuring socio-economic inequalities in DBMHL prevalence, relative index of inequality (RII) and slope index of inequality (SII) were used.
Results
The prevalence rates of DBMHL were 4.10% (urban: 5.57%, rural: 3.51%), 1.54% (urban: 1.63%, rural: 1.42%), 3.93% (urban: 5.62%, rural: 3.20%), and 5.54% (urban: 6.16%, rural: 5.33%) respectively in Bangladesh, Nepal, Pakistan, and Myanmar. The risk ratios (RR) obtained from RII for Bangladesh, Nepal, Pakistan and Myanmar were 1.25, 1.25, 1.14, and 1.09, respectively, and β coefficient from SII were 0.01, 0.004, 0.005, and 0.006 unit respectively. In addition to not breastfeeding [Bangladesh (AOR: 1.55; 95% CI: 1.11–2.15), Myanmar (AOR: 1.74; 95% CI: 1.02–2.95)], respondent’s older age (in Bangladesh, Nepal, and Myanmar), child’s older age (in Pakistan and Myanmar), and middle and rich groups of wealth-index (in Bangladesh and Pakistan) were strong risk factors for DBMHL. On the other hand, female child [Nepal (AOR: 0.50; 95% CI: 0.26–0.95), Pakistan (AOR: 0.58; 95% CI: 0.41–0.84)], higher education [in Pakistan], respondent not participated in decision making [in Bangladesh and Nepal] and media access [Nepal (AOR: 0.44; 95% CI: 0.20–0.98)] had negative association with DBMHL.
Conclusion
The DBMHL persists in all selected countries, with a higher prevalence in urban areas than in rural areas. In order to control the higher prevalence of DBMHL in urban areas, respective countries need urgent implementation of multisectoral actions through effective policies and empowering local communities.
Introduction
Malnutrition, either under-nutrition or over-nutrition, is a persistent global public health concern which causes different types of diet-related non-communicable diseases [1,2]. Recently a report on global child malnutrition documented that most of the low and middle income countries are going through the nutrition transition, and experiencing the coexistence of dual faced malnutrition, i.e. maternal overweight and undernourished child in a family. However, the prevalence of stunting is declining too slowly while maternal overweight continues to rise globally [3]. Although there is a declining trend of child malnutrition in Bangladesh and its neighboring countries (such as Nepal, Pakistan, and Myanmar), the prevalence of child malnutrition is still high in these countries; whereas, overweight and obesity among women have significantly increased [4–10]. These countries are now facing a subtle problem named ‘double burden of malnutrition’, i.e., coexistence of undernutrition and obesity. This double burden of malnutrition has been observed at different level, i.e., country, household, and even individual level [11,12]. In the case of household level, double burden of malnutrition has been defined as the coexistence of stunted child along with overweight mother within the same household [13–18]. This definition of double burden of malnutrition at household level (DBMHL) is the one considered in the analysis. A survey conducted among 131 developing countries found that the magnitude of the coexistence of overweight-mother and undernourished-child pair at households were ranging from as low as 1.8% in Ethiopia to as high as 15.9% in Egypt [19]. At present, the prevalence of DBMHL in Bangladesh is reported to be approximately 4% [15,20].
The most denunciative outcome of DBMHL is that, DBMHL is an important promoter of double burden of diseases [21]. With the aim of achieving one of the Sustainable Development Goals (SDGs) 2.2 (ending all forms of malnutrition), most of the low-and-middle income countries are now focusing to reduce the terrible crisis of both DBMHL and double burden of disease [22]. Moreover, DBMHL confers a serious and negative economic impact on individuals and populations. For example, through its effects on health, DBMHL increases health-care costs of a country, reduces productivity and slows economic growth, which, in turn, can perpetuate a cycle of poverty and ill-health for the long run [23]. Therefore, understanding the factors associated with DBMHL in developing countries are crucial to develop interventions to improve maternal and child health as well as achieving the second goal of SDGs (SDG-2).
Most of the extant literature on DBMHL were limited to small-scale sample and provided little information [18,24–27]. Earlier literatures documented that maternal and child’s older age, sex and birth order of children, disease occurred to children, breastfeeding, working status of mothers, mother’s educational level, decision making autonomy, wealth-index, toilet facility of households, and respondent’s access to all media etc. had significant effect either on child malnutrition or maternal over-nutrition, or, on both [15,20,21,28–33]. This burden of malnutrition have serious developmental, economic, social and medical impacts on individuals as well their families and communities [23]. Such an important issue has hardly been studied in South Asian countries where the prevalence rates of maternal and child malnutrition are reported to be higher than the other regions of the world [34,35]. A nation-wide comparative study among some neighboring countries may depict clear amplitude of DBMHL in the corresponding regions. To the best of our knowledge, no study has been conducted in South Asian region that assessed the prevalence of DBMHL and the factors associated with it. To address this knowledge gap, this study has attempted to find the nation-wide prevalence of DBMHL and its associated risk factors in some selected countries in South Asian region, namely Bangladesh, Nepal, Pakistan and Myanmar.
Methods
Data
In this study, data for Bangladesh, Nepal, Pakistan and Myanmar was extracted from the latest Demographic and Health Surveys (DHS) of the respective countries. Since 1984, MEASURE DHS project has been providing assistance to conduct standardized household sample surveys in low-and-middle income countries with a special focus on health, socioeconomic, nutrition, and fertility-related information from women of reproductive age (15–49 years) [36]. After developing a rigorous area-based sampling design, the DHS program has employed multistage stratification and probabilistic sampling with each unit having a defined probability of selection [37]. In most of the included survey, sampling was stratified according to urban and rural areas, and furthermore in geographic or administrative regions. The DHS sampling framework and sample designs vary from country to country according to its population and other geographical factors [37]. In this study, information of households that have at least one mother-child pair from Bangladesh, Nepal, Pakistan, and Myanmar were used to identify the prevalence and risk factors of DBMHL. The procedure of selecting final sample size for selected countries has been shown in Table 1.
Table 1. Selection of sample size from the latest DHS of Bangladesh, Nepal, Pakistan and Myanmar.
| Country and DHS Year | Bangladesh2014 | Nepal 2016 |
Pakistan 2012–13 |
Myanmar 2015–16 |
|
|---|---|---|---|---|---|
| Total Interviewed households | 17300 | 11040 | 12943 | 12500 | |
| Excluded Households | Households without at least one child-mother pair | 9997 | 5571 | 5955 | 8447 |
| Households with flagged cases of maternal BMI and pregnant women | 54 | 1366 | 167 | 50 | |
| Households out of plausible limits of child stunting | 677 | 1411 | 999 | 418 | |
| Households with women who had twin births and whose children living elsewhere | 36 | 5 | 13 | 16 | |
| Missing information regarding covariates | 58 | 17 | 39 | 28 | |
| Final Sample Size* | 6478 | 2670 | 5770 | 3541 |
* Complete information of overall households with at least one child-mother pair.
Note: Exclusion criteria with numbers have been italicized.
Outcome variable
According to World Health Organization (WHO), the double burden of malnutrition is the coexistence of undernutrition along with overweight, obesity or diet-related non-communicable diseases, within individuals, households and populations, and across the life-course [23]. In this study, double burden of malnutrition at household level (DBMHL), the outcome of interest, is defined as the coexistence of overweight mother and stunted child in the same household. A child was classified as stunted if his/her length/height was at least two standard deviations (< 2 SD) below the mean for their age [38]. Mother with body mass index more than or equal to 25 kg/m2 (BMI ≥ 25 kg/m2) was considered as overweight. A binary variable, DBMHL, was created where a household with an overweight mother and a stunted child was categorized as 1, and 0 if otherwise.
Covariates
A variety of child and maternal socio-demographic characteristics that have been theoretically or empirically linked to child malnutrition [39–44] or maternal overweight [15,19,20,45–48] were included in the analysis. The children’s characteristics were age, sex, birth order, disease, and breast-feeding status. Age was classified as less than 24 months or 24 months and over. Sex was included because in South Asian Region, male children are valued more than female children, and receive preferential treatment, including better nutrition and care [49]. Birth order was classified as 1st to 3rd order, and 4th order or more [15]. Dichotomous variable indicated whether a child was still breast-feeding, which is strongly associated with child health outcomes in developing countries [35], and whether he or she had suffered from any disease in the last 2 weeks. ‘Had any disease in the last 2 weeks’ indicates that, the children had suffered from either diarrhea or acute respiratory infection or fever in the last 2 weeks before the survey.
Maternal characteristics were age, education, work status, and decision making autonomy. Maternal age was classified as 15–24, 25–34 or 35–49 years. Education was categorized as no education, primary, secondary or higher. Work status was categorized as currently working or not. Maternal household decision-making autonomy was included because earlier literature suggests that enhancing maternal autonomy may be an important intervention for improving maternal and child nutrition [50]. In this study, maternal household decision-making autonomy was measured using mother’s responses to three questions that asked who makes decisions in household regarding obtaining health care for herself, making large purchases, and visiting family and relatives. Response categories were the respondent alone, the respondent and her husband, the respondent and someone other than her husband, her husband alone, someone else or other. For each of the three questions, a value of 1 was assigned if the respondent was involved in making the decision, and 0 if she was not, the values were summed and dichotomized as participated and not participated.
Finally, several household characteristics were included in the analyses. These include wealth-index, toilet facility, place of residence (urban or rural), and media exposure (watching TV, listening radio, and reading newspapers). The wealth-index was calculated as described in the corresponding country’s latest and available DHS reports [8], using principal component analysis of the assets owned by households in urban and rural areas [51,52]. The score was divided into five equal quintiles with the first, representing the poorest 20%, and the fifth, representing the richest 20% [53,54]. The other measures indicated whether the household had sanitary toilet facilities and some degree of media access. For the types of toilet facility, ‘Improved toilet’ refers toilets with flush systems, VIP latrine, pit latrine with slab, and open pit latrine; and ‘Not improved’ refers toilets with no facility/bush, field, bucket toilet, and hanging toilets. Media access refers to those households where there was access to watching TV, listening radio, and reading newspaper at least once a week. For each of the two categories of media access, a value of 1 was assigned if there was access to media, and 0 if there was not.
Statistical analysis
We have calculated the prevalence of DBMHL for Bangladesh, Nepal, Pakistan and Myanmar. Chi-square tests were used to identify the bivariate association between various socio-demographic variables and DBMHL. To measure different direction of socioeconomic inequalities in DBMHL, two regression based methods were used: (i) relative index of inequality (RII); (ii) slope index of inequality (SII). These two measures of inequality were used because the RII and SII took into account the prevalence of DBMHL across the whole socioeconomic distribution in the study population of each country [55]. To compute SII and RII, linear regression and modified poisson approach were used [56]. A positive value of SII means the increment of health indicator with increasing socio-economic status (SES). Again, values of RII < 1 indicate that the poor are more risky to be exposed to adverse SES outcomes compared with the rich. Finally, multivariate logistic regression models were used to assess the association between DBMHL and socio-demographic variables; adjusted odds ratios with 95% confidence interval were estimated to assess the strength of the association of DBMHL with predictor and covariates. In all analyses, the significant level was set at p < 0.05. All the analyses were performed using Stata’s ‘SVY’ command in order to control the effect of the complex survey design. To evaluate the possible collinearity, we used variance inflation factor and found no multicollinearity problem among variables. Stata version 14.2 [57] was used to carry out all the analyses.
Ethical consideration
The surveys were approved by Macro-institutional review board; and the survey protocols were reviewed and approved by National Research Ethics Committee of the respective country [58]. For individual and household interview, verbal informed consent was obtained from the respondents. For anthropometric measurements, informed consent was also obtained after the individual interview. Ethical approvals were obtained by DHS and respective countries prior to the data collections.
Results
The prevalence of DBMHL
From Fig 1, the highest prevalence of DBMHL was observed in Myanmar (5.54%) and the lowest prevalence was in Nepal (1.54%). The prevalence of DBMHL in Bangladesh was 4.10% and in Pakistan 3.93%. This prevalence was found to be higher in urban areas than in rural areas among these four countries.
Fig 1. Prevalence of DBMHL in Bangladesh, Nepal, Pakistan and Myanmar.
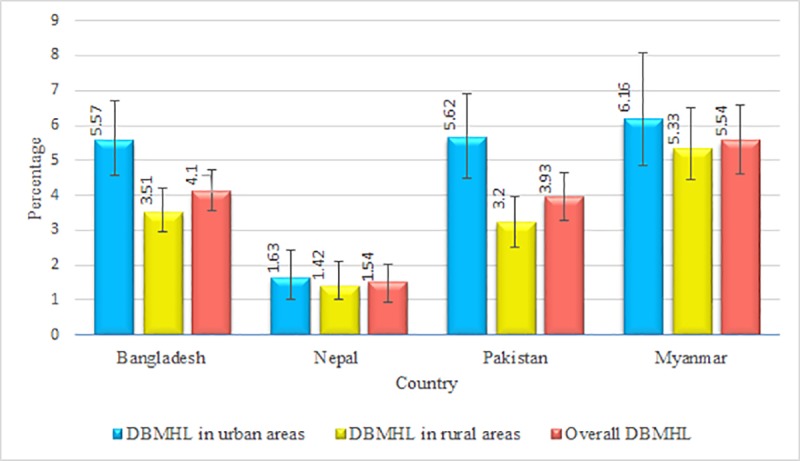
Note: Total observation in Bangladesh, Nepal, Pakistan, and Myanmar was 6478 (rural: 4399, urban: 2079), 2670 (rural: 1144, urban: 1526), 5770 (rural: 3168, urban: 2602), and 3541 (rural: 2728, urban: 813) respectively.
Background characteristics
The percentages of households with stunted children and overweight mothers are presented in Fig 2. In Bangladesh, 34% stunted children and 19% overweight mothers were found at household level. The prevalence rates of stunted children and overweight mothers at household level were higher in Pakistan than other countries.
Fig 2. Percentages of households with stunted children and overweight mothers.
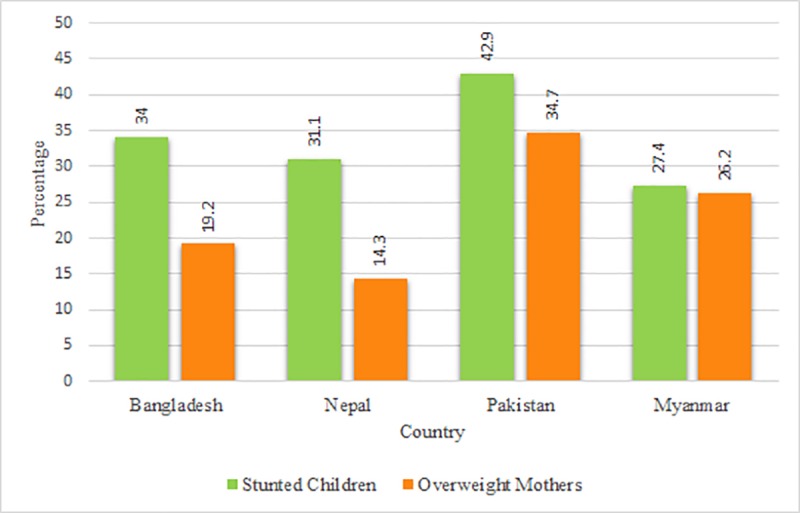
Note: Percentages were weighted; the total number of households of Bangladesh, Nepal, Pakistan, and Myanmar were 6478, 2670, 5770, and 3541 respectively.
Table 2 shows the background characteristics of the selected households in Bangladesh, Nepal, Myanmar, and Pakistan. The prevalence of younger children (0 to 23 months) was the highest (72%) in Nepal. More than half of the children had suffered from diseases (either diarrhea or acute respiratory infection or fever) in the last 2 weeks before the survey, and they were currently breastfed. But, the prevalence of practicing breastfeeding was significantly the highest (93%) in Nepal. Almost half of the mothers were aged below 25 years in Bangladesh and Nepal, however, in Myanmar and Pakistan most of the mothers were aged between 25–34 years. Again, more than half of the respondents were not currently working (except Myanmar), and were not participating in making household decisions.
Table 2. Basic characteristics of the households with at least one child-mother pair in Bangladesh, Nepal, Myanmar, and Pakistan.
| Basic characteristics | Bangladesh | Nepal | Pakistan | Myanmar |
|---|---|---|---|---|
| N (%)a | N (%)a | N (%)a | N (%)a | |
| Child’s age | ||||
| 0 to 23 months | 2914 (45.77) | 1910 (71.98) | 3093 (54.98) | 1733 (47.01) |
| 24 to 59 months | 3564 (54.23) | 760 (28.02) | 2677 (45.02) | 1808 (52.99) |
| Had any disease in the last 2 weeks | ||||
| No | 2242 (34.27) | 851 (33.02) | 2501 (40.34) | 1403 (43.81) |
| Yes | 4236 (65.73) | 1819 (66.98) | 3269 (59.66) | 2138 (56.19) |
| Birth order | ||||
| 1–3 | 5480 (84.72) | 2257 (84.90) | 2958 (51.32) | 2596 (77.51) |
| ≥ 4 | 998 (15.28) | 413 (15.10) | 2812 (48.68) | 945 (22.49) |
| Sex of child | ||||
| Male | 3382 (52.74) | 1454 (53.45) | 2984 (52.52) | 1845 (51.21) |
| Female | 3096 (47.26) | 1216 (46.55) | 2786 (47.48) | 1696 (48.79) |
| Respondent’s age | ||||
| 15–24 | 3134 (48.49) | 1322 (48.40) | 1126 (20.08) | 655 (18.26) |
| 25–34 | 2812 (43.77) | 1191 (45.75) | 3132 (55.13) | 1797 (51.77) |
| 35–49 | 532 (7.74) | 157 (5.85) | 1512 (24.79) | 1089 (29.96) |
| Currently breastfeeding | ||||
| Yes | 3657 (56.68) | 2495 (92.78) | 2835 (50.79) | 1956 (54.91) |
| No | 2821 (43.32) | 175 (7.22) | 2935 (49.21) | 1585 (45.09) |
| Highest educational level | ||||
| No education | 953 (15.58) | 761 (29.67) | 3187 (56.92) | 548 (15.50) |
| Primary | 1749 (27.26) | 514 (19.94) | 794 (15.91) | 1559 (45.93) |
| Secondary | 3046 (47.30) | 969 (35.00) | 1035 (17.55) | 1145 (29.98) |
| Higher | 730 (9.86) | 426 (15.39) | 754 (9.61) | 289 (8.59) |
| Work-status | ||||
| Not working | 4893 (74.45) | 1364 (53.81) | 4659 (73.76) | 1621 (43.15) |
| Working | 1585 (25.55) | 1306 (46.19) | 1111 (26.24) | 1920 (56.85) |
| Wealth-index | ||||
| Richest | 1317 (19.84) | 340 (14.68) | 1162 (16.69) | 503 (15.65) |
| Richer | 1332 (20.32) | 508 (20.43) | 1070 (18.43) | 643 (18.25) |
| Middle | 1268 (20.05) | 552 (21.99) | 1061 (18.97) | 644 (17.36) |
| Poorer | 1216 (18.77) | 580 (21.42) | 1159 (21.49) | 778 (21.89) |
| Poorest | 1345 (21.03) | 690 (21.48) | 1318 (24.43) | 973 (26.86) |
| Media access | ||||
| No | 2400 (37.13) | 569 (22.50) | 3141 (54.56) | 615 (17.29) |
| Yes | 4078 (62.87) | 2101 (77.50) | 2613 (45.44) | 2926 (82.71) |
| Household decision making autonomy | ||||
| Respondent participated | 2778 (45.81) | 658 (25.96) | 2541 (48.42) | 2308 (64.70) |
| Not participated | 3700 (54.19) | 2012 (74.04) | 3229 (51.58) | 1233 (35.30) |
| Types of toilet facility | ||||
| Improved | 5557 (85.27) | 2023 (71.44) | 4559 (70.16) | 2831 (80.63) |
| Not improved | 921 (14.73) | 647 (28.56) | 1211 (29.84) | 710 (19.37) |
| Place of residence | ||||
| Urban | 2079 (25.82) | 1526 (53.92) | 2602 (30.26) | 813 (22.98) |
| Rural | 4399 (74.18) | 1144 (46.08) | 3168 (69.74) | 2728 (77.02) |
| Total | 6478 | 2670 | 5770 | 3541 |
N, Number of observation
a Percentages are weighted.
Association of DBMHL with socio-demographic characteristics
Table 3 presents the results of association of DBMHL with selected socio-demographics in Bangladesh, Nepal, Pakistan, and Myanmar. The proportion of DBMHL was higher among older children in Bangladesh (4.9% vs 3.0%), Nepal (2.4% vs 1.2%), Pakistan (6.1% vs 2.2%), and Myanmar (8.3% vs 2.4%). The households with no breastfeeding practice have higher proportion of DBMH than the households with breastfeeding practice; e.g., Bangladesh (5.4% vs 3.0%), Nepal (3.2% vs 1.4%), Pakistan (5.7% vs 2.2%), and Myanmar (8.5% vs 3.3%).
Table 3. Bivariate association (percentage) and adjusted associations (odds ratio) between different socio-demographic determinants and the DBMHL for the respective countries.
| Determinants | Bangladesh (n = 6478) | Nepal (n = 2670) | Pakistan (n = 5770) | Myanmar (n = 3541) | ||||
|---|---|---|---|---|---|---|---|---|
| (%)a | AOR (95% CI)b | (%)a | AOR (95% CI)b | (%)a | AOR (95% CI)b | (%)a | AOR (95% CI)b | |
| Breastfeeding | ||||||||
| Yes | 3.00 | 1 (Ref) | 1.40 | 1 (Ref) | 2.20 | 1 (Ref) | 3.00 | 1 (Ref) |
| No | 5.40 | 1.55* (1.11–2.15) | 3.20 | 1.93 (0.64–5.85) | 5.70 | 1.46 (0.85–2.51) | 8.50 | 1.74* (1.02–2.95) |
| P-value (χ2) | P = 0.001 | P = 0.067 | P < 0.001 | P < 0.001 | ||||
| Respondent’s age | ||||||||
| 15–24 | 2.70 | 1 (Ref) | 1.20 | 1 (Ref) | 1.80 | 1 (Ref) | 2.90 | 1 (Ref) |
| 25–34 | 5.30 | 1.83** (1.19–2.82) | 1.60 | 1.27 (0.63–2.57) | 3.70 | 1.71 (0.89–3.30) | 4.80 | 1.22 (0.62–2.39) |
| 35–49 | 5.50 | 2.01* (1.06–3.81) | 3.70 | 3.63 (0.93–14.11) | 6.30 | 2.64** (1.27–5.52) | 8.30 | 2.03* (1.04–4.11) |
| P-value (χ2) | P < 0.001 | P = 0.054 | P < 0.001 | P = 0.001 | ||||
| Child’s age | ||||||||
| 0 to 23 months | 3.00 | 1 (Ref) | 1.20 | 1 (Ref) | 2.20 | 1 (Ref) | 2.40 | 1 (Ref) |
| 24 to 59 months | 4.90 | 1.13 (0.72–1.76) | 2.40 | 1.59 (0.76–3.32) | 6.10 | 1.92** (1.18–3.11) | 8.30 | 2.12* (1.16–3.83) |
| P-value (χ2) | P = 0.021 | P = 0.042 | P < 0.001 | P < 0.001 | ||||
| Had disease in the last 2 weeks | ||||||||
| No | 4.30 | 1 (Ref) | 0.90 | 1 (Ref) | 4.10 | 1 (Ref) | 4.40 | 1 (Ref) |
| Yes | 3.90 | 0.81 (0.55–1.16) | 1.90 | 1.74 (0.79–3.83) | 3.80 | 0.99 (0.69–1.44) | 6.40 | 1.05 (0.71–1.54) |
| P-value (χ2) | P = 0.608 | P = 0.044 | P = 0.627 | P = 0.054 | ||||
| Sex of child | ||||||||
| Male | 3.70 | 1 (Ref) | 2.00 | 1 (Ref) | 4.80 | 1 (Ref) | 5.10 | 1 (Ref) |
| Female | 4.40 | 1.16 (0.82–1.65) | 1.00 | 0.50* (0.26–0.95) | 3.00 | 0.58** (0.41–0.84) | 5.90 | 1.15 (0.82–1.58) |
| P-value (χ2) | P = 0.374 | P = 0.032 | P = 0.004 | P = 0.343 | ||||
| Birth order | ||||||||
| 1–3 | 3.90 | 1 (Ref) | 1.50 | 1 (Ref) | 3.30 | 1 (Ref) | 5.40 | 1 (Ref) |
| ≥ 4 | 4.80 | 1.17 (0.76–1.81) | 1.60 | 0.97 (0.35–2.70) | 4.60 | 0.98 (0.63–1.53) | 5.90 | 0.91 (0.57–1.46) |
| P-value (χ2) | P = 0.282 | P = 0.864 | P = 0.056 | P = 0.616 | ||||
| Work status of Mother | ||||||||
| Not working | 4.20 | 1 (Ref) | 1.40 | 1 (Ref) | 4.00 | 1 (Ref) | 4.30 | 1 (Ref) |
| Working | 3.80 | 0.89 (0.62–1.27) | 1.70 | 1.16 (0.57–2.36) | 3.60 | 0.92 (0.60–1.41) | 6.50 | 1.22 (0.79–1.86) |
| P-value (χ2) | P = 0.705 | P = 0.654 | P = 0.546 | P = 0.035 | ||||
| Educational status of mother | ||||||||
| No education | 3.50 | 1 (Ref) | 1.10 | 1 (Ref) | 3.80 | 1 (Ref) | 3.60 | 1 (Ref) |
| Primary | 3.80 | 1.16 (0.76–1.77) | 1.40 | 2.04 (0.73–5.72) | 4.60 | 0.92 (0.53–1.57) | 6.70 | 1.66 (0.94–2.91) |
| Secondary | 4.20 | 1.08 (0.68–1.75) | 2.10 | 4.44**(1.52–12.91) | 4.30 | 0.63 (0.34–1.16) | 4.50 | 1.10 (0.53–2.26) |
| Higher | 4.60 | 0.93 (0.53–1.63) | 1.50 | 2.31 (0.56–9.52) | 3.00 | 0.35** (0.16–0.77) | 6.20 | 1.33 (0.51–3.43) |
| P-value (χ2) | P = 0.726 | P = 0.251 | P = 0.591 | P = 0.075 | ||||
| Wealth-index | ||||||||
| Poorest | 1.90 | 1 (Ref) | 1.50 | 1 (Ref) | 2.50 | 1 (Ref) | 4.20 | 1 (Ref) |
| Poorer | 2.80 | 1.49 (0.86–2.58) | 0.60 | 0.40 (0.09–1.78) | 2.90 | 1.20 (0.63–2.24) | 5.10 | 1.09 (0.63–1.88) |
| Middle | 5.90 | 2.90***(1.59–5.27) | 1.70 | 1.43 (0.47–4.38) | 4.00 | 1.58 (0.72–3.44) | 8.40 | 1.73 (0.97–3.10) |
| Richer | 4.30 | 1.87* (1.06–3.25) | 2.20 | 1.58 (0.50–4.98) | 5.70 | 2.48* (1.16–5.30) | 4.70 | 0.89 (0.45–1.76) |
| Richest | 5.40 | 2.02* (1.08–3.82) | 1.80 | 1.11 (0.28–4.30) | 5.30 | 2.59* (1.07–6.26) | 6.00 | 1.12 (0.44–2.87) |
| P-value (χ2) | P < 0.001 | P = 0.385 | P = 0.007 | P = 0.051 | ||||
| Household Decision making autonomy | ||||||||
| Respondent Participated |
4.90 | 1 (Ref) | 3.10 | 1 (Ref) | 4.10 | 1 (Ref) | 5.80 | 1 (Ref) |
| Not participated | 3.30 | 0.73* (0.55–0.98) | 1.00 | 0.34** (0.16–0.71) | 3.80 | 1.02 (0.69–1.50) | 5.10 | 0.91 (0.60–1.37) |
| P-value (χ2) | P = 0.005 | P = 0.001 | P = 0.664 | P = 0.511 | ||||
| Toilet Facility | ||||||||
| Improved | 4.00 | 1 (Ref) | 1.80 | 1 (Ref) | 4.50 | 1 (Ref) | 5.90 | 1 (Ref) |
| Not improved | 4.40 | 1.52 (0.73–3.12) | 1.00 | 0.72 (0.25–2.04) | 2.70 | 1.02 (0.60–1.71) | 3.80 | 0.83 (0.47–1.45) |
| P-value (χ2) | P = 0.779 | P = 0.218 | P = 0.018 | P = 0.071 | ||||
| Media Access | ||||||||
| No | 2.60 | 1 (Ref) | 1.80 | 1 (Ref) | 3.80 | 1 (Ref) | 3.60 | 1 (Ref) |
| Yes | 4.90 | 1.48 (0.98–2.23) | 1.50 | 0.44* (0.20–0.98) | 4.10 | 1.03 (0.71–1.48) | 5.90 | 1.40 (0.82–2.39) |
| P-value (χ2) | P = 0.001 | P = 0.553 | P = 0.682 | P = 0.041 | ||||
| Place of residence | ||||||||
| Urban | 5.60 | 1 (Ref) | 1.60 | 1 (Ref) | 5.60 | 1 (Ref) | 6.20 | 1 (Ref) |
| Rural | 3.50 | 0.73 (0.53–1.01) | 1.40 | 1.16 (0.52–2.60) | 3.20 | 0.72 (0.45–1.18) | 5.30 | 0.82 (0.46–1.48) |
| P-value (χ2) | P = 0.002 | P = 0.727 | P = 0.003 | P = 0.495 | ||||
Ref., reference; AOR, Adjusted Odds Ratio; n, total observation; P-value (χ2), P-value obtained from chi-square estimation
aPrevalence of DBMHL in percentage obtained from chi-square estimation
b95% confidence intervals
Level of significance
*p<0.05
**p<0.01
***p<0.001
Not breastfed children had 1.55 and 1.74 times higher odds of suffering from DBMHL than the breastfed children in Bangladesh and Myanmar, after adjusting for all covariates. Surprisingly, female child were negatively associated with DBMHL in Nepal [AOR, 0.50; 95% CI, 0.26–0.95] and Pakistan [AOR, 0.58; 95% CI, 0.41–0.84]. Compared to poorest households, Bangladeshi rich (both richer and richest) and middle income households were experiencing higher DBMHL, and in Pakistan, only the rich (both richer and richest) had experienced it. However, secondary educated mothers (only in Nepal), older maternal age (except Nepal), and older children (except Bangladesh and Nepal) had significant and positive association with DBMHL. Respondent who did not participate in making household decision (in Bangladesh and Nepal) and media access (only in Nepal) was less likely to be associated with DBMHL.
Summary measures of SES inequality
Table 4 shows summary measures of SES inequality in DBMHL for the selected countries. Significant RII for Bangladesh, Nepal, and Pakistan were 1.25, 1.25, and 1.14 respectively, indicating that a move from the poorest to the richest of the SES distribution was associated with a 25%, 25%, and 14% increase in DBMHL in Bangladesh, Nepal, and Pakistan. And, SII indicated that one unit change from the poorest to the richest of the SES group was associated with 0.01, 0.004, and 0.005 unit increase in DBMHL in Bangladesh, Nepal, and Pakistan, respectively.
Table 4. Summary measures of Socio-economic status (SES) inequality in DBMHL in Bangladesh, Nepal, Myanmar, and Pakistan.
| Country (n) | Relative index of inequality (RII) RR (95% CI) |
Slope index of inequality (SII) β coefficient (95% CI) |
|---|---|---|
| Bangladesh (n = 6478) | 1.25 (1.16,1.37) | 0.0100 (0.0070,0.0130) |
| Nepal (n = 2670) | 1.25 (1.01,1.54) | 0.0040 (0.0002,0.0070) |
| Pakistan (n = 5770) | 1.14 (1.04,1.24) | 0.0050 (0.0020,0.0070) |
| Myanmar (n = 3541) | 1.09 (0.99,1.20) | 0.0060 (-0.0001,0.0110) |
n, total number of observation
Discussion
This study has investigated and compared the amplitude of the DBMHL, and the significant risk factors those are accountable for occurring DBMHL especially the socio-economic inequality in Bangladesh, Nepal, Pakistan, and Myanmar. It is documented from this study that the current prevalence rate of DBMHL is fairly high in these countries. The current prevalence rate of DBMHL in the African, Asian, and Latin American countries are as follows: Ethiopia (1.8%), Senegal (3%), Chad (3.5%), Uganda (3.6%), Tanzania (4.1%), Rwanda (4.4%), Kazakhstan (2.5%), Vietnam (5%), Uzbekistan (4.1%), Jordan (3.6%), Cambodia (4%), and Columbia (4%) [12,19]. Compared to the above countries, the prevalence of DBMHL is higher in Myanmar (5.54%). It is noteworthy that, the prevalence of overall DBMHL in Bangladesh (4.10%) is almost the same as the earlier estimates [14,15,20]. Moreover, our study has revealed that DBMHL in Bangladesh is higher than the other South Asian countries, Nepal (1.54%) and Pakistan (3.93%); where the previous literatures have supported it too [20,59].
Our study has shown that, there is a positive association between higher wealth-index of the households and DBMHL, especially in Bangladesh and Pakistan. Some other studies have also supported our result by revealing that, child malnutrition and maternal overweight were highly observed among middle income families [60,61]. The positive association between higher wealth-index and DBMHL are in line with one of the previous studies conducted in Bangladesh and its neighboring countries [15], but appears to be contradicted with the studies from Latin American countries, where the prevalence of DBMHL is more common in lower wealth-index groups. In South Asian region, such contrast can be due to the fact that, practices like- excessive intake of processed energy-dense foods, lack of physical exercise, and soft drinks consumptions are more common in middle and high (richer and richest) income households [62].
We have found that, older mothers were more associated with the increased risk of DBMHL than the younger mothers in the study countries except Nepal. This is in a line with other studies that showed women aged 30 years or older were overweight and obese in Bangladesh, Myanmar, and Pakistan [4,9,63,64]. Because of sedentary lifestyle and reduction of metabolic rates, obesity is increasing with age among women [65]. Following this issue, among Myanmar and Bangladeshi households, our findings indicated that, not breastfeeding mothers showed positive association with DBMHL than those continuously breastfed their children. Breastfeeding burns extra calories of mothers; so, long term breastfeeding not only helps mothers to lose pregnancy weight faster, but also provides all essential micronutrients a baby needs [47,66]. Thus, poor breastfeeding practices can contribute to both maternal overweight and child malnutrition. Though the breastfeeding has become universal in almost all Asian countries with extended median duration of breastfeeding, surprisingly our study has revealed that, among the children aged 24 to 59 months old, Myanmar and Pakistani households are facing more DBMHL significantly than the 0 to 23 months old children. As breastfeeding has a protective effect on both stunting in children and overweight in mothers, it is plausible to have higher rates of DBMHL among children 24–59 months when breastfeeding has a low impact on child’s dietary adequacy and is less practiced by mothers. Recent studies have supported this outcome by investigating that, along with Pakistan, other countries of Asia are experiencing malnutrition among older children because of bypassing continuous breastfeeding practices [39,42,67,68]. The latest DHS report of Pakistan brought out that, only 1% children (18 to 23 months) were continuing breastfeeding and other complementary foods, and no information was found regarding breastfeeding practice among older children [9]. Such malnutrition among older children in Pakistan and Myanmar is dangerously shaping DBMHL. In our study, the prevalence of overall DBMHL in Nepal was comparatively lower than other countries; and it is partly due to higher prevalence of practicing breastfeeding mother and of younger children (0 to 23 months) in Nepal.
Female children of Nepal and Pakistani households have exhibited less association with DBMHL significantly than the male children. The prevalence of exclusive breastfeeding was higher among female children than male in both Pakistan and Nepal, which probably decreased DBMHL of the households with female children [7,9].
The Nepalese households with access to media showed significant negative association with DBMHL. Several studies conducted in Indian Subcontinent revealed that, children whose mothers did not have any access to mass media (i.e., newspapers, radio & TV) possessed higher probability of having severe and moderate malnutrition [69,70]. It was also found that, exposure to media increased the likelihood that mothers gave complementary foods and offered it at least twice daily with increased meal frequency and diversity [71]. On the other hand, at present, most of the countries have launched different types of media campaign to dispense child nutrition information and to reduce the consumption of oily and sugar-sweetened beverages in homes as a strategy to combat both malnutrition and obesity [71,72]. As, in Nepal, more than one-third households had access to media, and it is plausible to consider media access as one of the important protective factors against DBMHL in Nepal.
This study found a mixed result of the prevalence of DBMHL according to maternal education. While higher maternal education were positively associated with DBMHL in Pakistan, the Nepalese sample shows a negative impact of higher education on DBMHL in household. A similar study conducted in Myanmar reported that, among the women with secondary education, about 28% were overweight and 14% were obese [4]. Another study from Nepal [73] reported that, most of the educated mothers, who entered into employment had higher chance of being overweight than the general population; and, more than half of the population consider ‘being overweight’ as a symbol of ‘prosperity’. This could possibly explain the linkage between secondary educated mothers and increased DBMHL in Pakistan.
According to WHO [23], the DBMHL can be seen as a dual nutrition challenge for any country; addressing this DBMHL and its risk factors will be one of the major priorities in achieving SDG-2. The indicator 2.2 of the SDG-2 has pointed out to end all forms of malnutrition by 2030. Aiming this issue, this study has brought out the prevalence rates of DBMHL and the underlying determinants of DBMHL of the selected countries. If the risk factors of DBMHL, obtained from our study, can be averted by the respective countries with proper interventions, programmes, and policies, the prevalence of malnutrition of mother-child pair can be checked. And eventually, the way of achieving SDG-2 will be smoother for those countries.
This study has several strengths and limitations. The main strengths are: it is based on nationally representative surveys with large sample sizes and low percentages of missing information which provide sufficient statistical power to give more reliable and unalloyed results with greater precision and power. The strengths of the DHS data for studying population health of any country include very high response rates, national coverage, standard data collection procedures, and interviewer training [74–76]. However, because of cross-sectional nature of our data, causality cannot be suspected properly. This study is also unable to include other apparently important variables concerning DBMHL such as daily dietary pattern, physical activity, caregiving practices, cultural influences, pregnancy and birth information etc. due to unavailability of information in the DHS. Finally, we have used BMI, to assess the nutritional status of mother. However, the use of standard WHO definitions for overweight and obesity may have introduced bias since they do not consider the ethnic and region specific recommendations for BMI cut off values for overweight and obesity [77]; because, some of the mothers, still at risk for overweight and obesity from lower BMI values, may have been overlooked.
Conclusion
This is the first study where the overall diversity and the risk factors of DBMHL were separately and comparatively identified for Bangladesh, Nepal, Pakistan, and Myanmar. The overall results suggested that maternal and child age as well as poor breastfeeding were risk factors for DBMHL with varying risk factors among countries; such as- secondary education of mothers was the risk factor for DBMHL in Nepal, whereas, higher education was the protective factor in Pakistan. Again, richer and richest wealth-index were found to be positively associated with DBMHL in Bangladesh and Pakistan. Media access at least once a week showed negative association with DBMHL in Nepal. In such complex circumstances, for introducing effective long-term recommendations and proactive actions against DBMHL, further studies have to be conducted by respective countries. Even though, simultaneously some actions along with the existing policies can be taken to reduce this burden, such as- providing education on the importance of equilibrium between energy intake and expenditure; promoting and supporting breastfeeding; ensuring conditions for optimal fetal and early child development; ensuring access to optimal maternal and antenatal nutrition and care; raising awareness among the rich people by highlighting the benefits of physical exercises; advertising campaigns through mass media on nutritional issues for sound feeding practices; and reducing poverty through empowering local communities. Finally, in order to achieve SDG-2, most of the Asian countries need to pay heed upon the risk factors of DBMHL to inhibit the spread of DBMHL.
Acknowledgments
We are thankful to the MEASURE DHS for serving us with the latest BDHS, NDHS, PDHS, and MDHS dataset. A special thanks and heart-full gratitude goes to Thomas W. Pullum, Ph.D., (Director of Research, The Demographic and Health Surveys Program, ICF) for his unconditional help and consultation during conceptualizing the research.
Abbreviations
- AOR
Adjusted Odds Ratio
- BDHS
Bangladesh Demographic and Health Survey
- BMI
Body Mass Index
- CI
Confidence Interval
- DBMHL
Double Burden of Malnutrition at Household Level
- DHS
Demographic and Health Survey
- MDHS
Myanmar Demographic and Health Survey
- NDHS
Nepal Demographic and Health Survey
- PDHS
Pakistan Demographic and Health Survey
- RII
Relative Index of Inequality
- RR
Risk Ratio
- SDG
Sustainable Development Goal
- SES
Socio-Economic Status
- SII
Slope Index of Inequality
- WHO
World Health Organization
Data Availability
The relevant data was obtained from MEASURE DHS and are available from the Demographic Health Surveys Program (Bangladesh Standard DHS, 2014- https://dhsprogram.com/data/dataset/Bangladesh_SPA_2014.cfm?flag=0; Nepal: Standard DHS, 2016- https://dhsprogram.com/data/dataset/Nepal_Standard-DHS_2016.cfm?flag=0; Myanmar: Standard DHS, 2015-16, https://dhsprogram.com/data/dataset/Myanmar_Standard-DHS_2016.cfm?flag=0; Pakistan: Standard DHS, 2012-13, https://dhsprogram.com/data/dataset/Pakistan_Standard-DHS_2012.cfm?flag=0).
Funding Statement
The authors received no specific funding for this work.
References
- 1.Ahmed T, Mahfuz M, Ireen S, Ahmed AMS, Rahman S, Islam MM, et al. Nutrition of Children and Women in Bangladesh: Trends and Directions for the Future. J Health Popul Nutr. 2012. March;30(1):1–11. 10.3329/jhpn.v30i1.11268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. Malnutrition. 2018. Available from: http://www.who.int/news-room/fact-sheets/detail/malnutrition
- 3.Hayashi Chika, Krasevec Julia, Kumapley Richard, Mehra Vrinda, de Onis Mercedes, Borghi Elaine, Blössner Monika, Urrutia Monica Flores, Prydz Espen Beer, Serajuddin Umar. Joint Malnutrition Estimates 2017 Edition—Worldwide. UNICEF-WHO-WB; 2017. May Available from: http://public.tableau.com/views/JointMalnutritionEstimates2017Edition-Wide/WB [Google Scholar]
- 4.Hong SA, Peltzer K, Lwin KT, Aung LS. The prevalence of underweight, overweight and obesity and their related socio-demographic and lifestyle factors among adult women in Myanmar, 2015–16. PLoS ONE. 2018. March 16;13(3). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5856399/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hussain MI, Naqvi BS. Current trends in treatment of obesity in Karachi and possibilities of cost minimization. Pak J Pharm Sci. 2015. March;28(2 Suppl):765–72. [PubMed] [Google Scholar]
- 6.Ministry of Health and Sports—MoHS/Myanmar, ICF. Myanmar Demographic and Health Survey 2015–16. Nay Pyi Taw, Myanmar: MoHS and ICF; 2017. Available from: http://dhsprogram.com/pubs/pdf/FR324/FR324.pdf [Google Scholar]
- 7.Ministry of Health—MOH/Nepal, New ERA/Nepal, ICF. Nepal Demographic and Health Survey 2016. Kathmandu, Nepal: MOH/Nepal, New ERA, and ICF; 2017. Available from: http://dhsprogram.com/pubs/pdf/FR336/FR336.pdf [Google Scholar]
- 8.National Institute of Population Research and Training—NIPORT/Bangladesh, Mitra and Associates, ICF International. Bangladesh Demographic and Health Survey 2014. Dhaka, Bangladesh: NIPORT, Mitra and Associates, and ICF International; 2016. Available from: http://dhsprogram.com/pubs/pdf/FR311/FR311.pdf [Google Scholar]
- 9.National Institute of Population Studies—NIPS/Pakistan, ICF International. Pakistan Demographic and Health Survey 2012–13. Islamabad, Pakistan: NIPS/Pakistan and ICF International; 2013. Available from: http://dhsprogram.com/pubs/pdf/FR290/FR290.pdf [Google Scholar]
- 10.Vaidya A, Shakya-Vaidya S, Krettek A. Obesity Prevalence in Nepal: Public Health Challenges in a Low-Income Nation during an Alarming Worldwide Trend. Int J Environ Res Public Health. 2010. June 1;7:2726–44. 10.3390/ijerph7062726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delisle H, Batal M. The double burden of malnutrition associated with poverty. The Lancet. 2016. June 18;387(10037):2504–5. [DOI] [PubMed] [Google Scholar]
- 12.Rachmi CN, Li M, Baur LA. The double burden of malnutrition in Association of South East Asian Nations (ASEAN) countries: a comprehensive review of the literature. Asia Pac J Clin Nutr. 2018;27(4):736–55. 10.6133/apjcn.062018.02 [DOI] [PubMed] [Google Scholar]
- 13.Fernald LC, Neufeld LM. Overweight with concurrent stunting in very young children from rural Mexico: prevalence and associated factors. Eur J Clin Nutr. 2007. May;61(5):623–32. 10.1038/sj.ejcn.1602558 [DOI] [PubMed] [Google Scholar]
- 14.Jehn M, Brewis A. Paradoxical malnutrition in mother-child pairs: untangling the phenomenon of over- and under-nutrition in underdeveloped economies. Econ Hum Biol. 2009. March;7(1):28–35. 10.1016/j.ehb.2009.01.007 [DOI] [PubMed] [Google Scholar]
- 15.Oddo VM, Rah JH, Semba RD, Sun K, Akhter N, Sari M, et al. Predictors of maternal and child double burden of malnutrition in rural Indonesia and Bangladesh. Am J Clin Nutr. 2012. April 1;95(4):951–8. 10.3945/ajcn.111.026070 [DOI] [PubMed] [Google Scholar]
- 16.Saibul N, Shariff ZM, Lin KG, Kandiah M, Ghani NA, Rahman HA. Food variety score is associated with dual burden of malnutrition in Orang Asli (Malaysian indigenous peoples) households: implications for health promotion. Asia Pac J Clin Nutr. 2009;18(3):412–22. [PubMed] [Google Scholar]
- 17.Doak CM, Adair LS, Monteiro C, Popkin BM. Overweight and Underweight Coexist within Households in Brazil, China and Russia. J Nutr. 2000. December 1;130(12):2965–71. 10.1093/jn/130.12.2965 [DOI] [PubMed] [Google Scholar]
- 18.Garrett JL, Ruel MT. Stunted child-overweight mother pairs: prevalence and association with economic development and urbanization. Food Nutr Bull. 2005. June;26(2):209–21. 10.1177/156482650502600205 [DOI] [PubMed] [Google Scholar]
- 19.Dieffenbach SD. Are Stunted Child/Overweight Mother Pairs a Distinct Entity or a Statistical Artifact? Demographic and Health Surveys, 1991–2009. [MPH: ]. Emory University; 2012. [Google Scholar]
- 20.Hauqe SE, Sakisaka K, Rahman M. Examining the relationship between socioeconomic status and the double burden of maternal over and child under-nutrition in Bangladesh. Eur J Clin Nutr. 2019. April;73(4):531–540. 10.1038/s41430-018-0162-6 Epub 2018 Apr 25 [DOI] [PubMed] [Google Scholar]
- 21.Kolčić I. Double burden of malnutrition: A silent driver of double burden of disease in low–and middle–income countries. J Glob Health. 2012. December;2(2). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3529312/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bhutta ZA. Nutrition: How will the next “Decade of Nutrition” be different from the past one? Nat Rev Gastroenterol Hepatol. 2016. August;13(8):441–2. 10.1038/nrgastro.2016.102 [DOI] [PubMed] [Google Scholar]
- 23.WHO. The double burden of malnutrition: policy brief. Geneva; 2017, p. 10. Report No.: WHO/NMH/NHD/17.3. Available from: http://www.who.int/nutrition/publications/doubleburdenmalnutrition-policybrief/en/
- 24.Bassete MN, Romaguera D, Giménez MA, Lobo MO, Samman NC. Prevalence and determinants of the dual burden of malnutrition at the household level in Puna and Quebrada of Humahuaca, Jujuy, Argentina. Nutr Hosp. 2014. February 1;29(2):322–30. 10.3305/nh.2014.29.2.7075 [DOI] [PubMed] [Google Scholar]
- 25.Khor GL, Sharif ZM. Dual forms of malnutrition in the same households in Malaysia—a case study among Malay rural households. Asia Pac J Clin Nutr. 2003;12(4):427–37. [PubMed] [Google Scholar]
- 26.Lee J, Houser RF, Must A, de Fulladolsa PP, Bermudez OI. Socioeconomic disparities and the familial coexistence of child stunting and maternal overweight in Guatemala. Econ Hum Biol. 2012. July;10(3):232–41. 10.1016/j.ehb.2011.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sarmiento OL, Parra DC, González SA, González-Casanova I, Forero AY, Garcia J. The dual burden of malnutrition in Colombia. Am J Clin Nutr. 2014. December;100(6):1628S – 35S. 10.3945/ajcn.114.083816 [DOI] [PubMed] [Google Scholar]
- 28.Corsi DJ, Finlay JE, Subramanian SV. Global Burden of Double Malnutrition: Has Anyone Seen It? PLOS ONE. 2011. September 28;6(9):e25120 10.1371/journal.pone.0025120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Doku DT, Neupane S. Double burden of malnutrition: increasing overweight and obesity and stall underweight trends among Ghanaian women. BMC Public Health. 2015. July 16;15:670 10.1186/s12889-015-2033-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Binns C, Lee M, Low WY. The Long-Term Public Health Benefits of Breastfeeding. Asia Pac J Public Health. 2016. January 1;28(1):7–14. 10.1177/1010539515624964 [DOI] [PubMed] [Google Scholar]
- 31.Sarma H, Saquib N, Hasan MM, Saquib J, Rahman AS, Khan JR, et al. Determinants of overweight or obesity among ever-married adult women in Bangladesh. BMC Obes. 2016. March 1;3:13 10.1186/s40608-016-0093-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shrimpton R, Rokx C. The double burden of malnutrition: a review of global evidence. The World Bank; 2012 Nov, p. 1–74. Report No.: 79525. Available from: http://documents.worldbank.org/curated/en/905651468339879888/The-double-burden-of-malnutrition-a-review-of-global-evidence
- 33.Tzioumis E, Kay MC, Bentley ME, Adair LS. Prevalence and trends in the childhood dual burden of malnutrition in low- and middle-income countries, 1990–2012. Public Health Nutr. 2016. June;19(8):1375–88. 10.1017/S1368980016000276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aguayo VM, Menon P. Stop stunting: improving child feeding, women’s nutrition and household sanitation in South Asia. Matern Child Nutr. 2016;12 Suppl 1:3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet Lond Engl. 2013. August 3;382(9890):427–51. [DOI] [PubMed] [Google Scholar]
- 36.MEASURE DHS (2009) Demographic and Health Surveys. CalvertonMD: MEASURE DHS; Available from: https://dhsprogram.com/Who-We-Are/upload/MEASURE_DHS_Brochure.pdf [Google Scholar]
- 37.Macro International Inc. Sampling Manual. CalvertonMD; 1996. (DHS III Basic Documentation; vol. No.6.). Available from: https://dhsprogram.com/pubs/pdf/AISM5/DHS_III_Sampling_Manual.pdf
- 38.WHO. Nutrition Landscape Information System (NLIS) country profile indicators: interpretation guide. 2010; 38p, ISBN: 9789241599955; Available from: http://apps.who.int/iris/handle/10665/44397
- 39.Akhtar S. Malnutrition in South Asia-A Critical Reappraisal. Crit Rev Food Sci Nutr. 2016. October 25;56(14):2320–30. 10.1080/10408398.2013.832143 [DOI] [PubMed] [Google Scholar]
- 40.Chantry CJ, Howard CR, Auinger P. Full Breastfeeding Duration and Associated Decrease in Respiratory Tract Infection in US Children. Pediatrics. 2006. February 1;117(2):425–32. 10.1542/peds.2004-2283 [DOI] [PubMed] [Google Scholar]
- 41.Mahgoub S, Nnyepi M, Bandeke T. Factors affecting prevalence of malnutrition among children under three years of age in Botswana. Afr J Food Agric Nutr Dev ISSN 1684-5358 Vol 6 Num 1 2005. November 30;6. [Google Scholar]
- 42.Mangasaryan N, Martin L, Brownlee A, Ogunlade A, Rudert C, Cai X. Breastfeeding Promotion, Support and Protection: Review of Six Country Programmes. Nutrients. 2012. August 14;4(8):990–1014. 10.3390/nu4080990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Simoes EAF, Cherian T, Chow J, Shahid-Salles SA, Laxminarayan R, John TJ. Acute Respiratory Infections in Children In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, et al. , editors. Disease Control Priorities in Developing Countries. 2nd ed Chapter: 25; ISBN: 9780821361795; Washington (DC): World Bank; 2006. Available from: http://www.ncbi.nlm.nih.gov/books/NBK11786/ [Google Scholar]
- 44.WHO. Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: a pooled analysis. WHO Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality. Lancet Lond Engl. 2000. February 5;355(9202):451–5. [PubMed] [Google Scholar]
- 45.Andrade RG de, Chaves OC, Costa DA da S, Andrade AC de S, Bispo S, Felicissimo MF, et al. Overweight in men and women among urban area residents: individual factors and socioeconomic context. Cad Saúde Pública. 2015. November;31:148–58. 10.1590/0102-311X00102714 [DOI] [PubMed] [Google Scholar]
- 46.Neupane S, K.C. P, Doku DT. Overweight and obesity among women: analysis of demographic and health survey data from 32 Sub-Saharan African Countries. BMC Public Health. 2016. January 13;16 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4710980/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Oddy WH, Li J, Landsborough L, Kendall GE, Henderson S, Downie J. The association of maternal overweight and obesity with breastfeeding duration. J Pediatr. 2006. August 1;149(2):185–91. 10.1016/j.jpeds.2006.04.005 [DOI] [PubMed] [Google Scholar]
- 48.Sarki M, Robertson A, Parlesak A. Association between socioeconomic status of mothers, food security, food safety practices and the double burden of malnutrition in the Lalitpur district, Nepal. Arch Public Health. 2016. September 13;74(1). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5020528/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ackerson LK, Subramanian SV. Intimate partner violence and death among infants and children in India. Pediatrics. 2009. November;124(5):e878–89. 10.1542/peds.2009-0524 [DOI] [PubMed] [Google Scholar]
- 50.Ruel MT, Alderman H. Nutrition-sensitive interventions and programmes: how can they help to accelerate progress in improving maternal and child nutrition? The Lancet. 2013. August 10;382(9891):536–51. [DOI] [PubMed] [Google Scholar]
- 51.Filmer D, Pritchett LH. Estimating Wealth Effects without Expenditure Data-or Tears: An Application to Educational Enrollments in States of India. Demography. 2001;38(1):115–32. 10.1353/dem.2001.0003 [DOI] [PubMed] [Google Scholar]
- 52.Rutstein SO, Johnson K. The DHS wealth index. Calverton, Maryland, USA: ORC Macro; 2004. (DHS Comparative Reports No. 6). Available from: http://dhsprogram.com/pubs/pdf/CR6/CR6.pdf
- 53.Howe LD, Hargreaves JR, Huttly SRA. Issues in the construction of wealth indices for the measurement of socio-economic position in low-income countries. Emerg Themes Epidemiol. 2008. January 30;5:3 10.1186/1742-7622-5-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006. November;21(6):459–68. 10.1093/heapol/czl029 [DOI] [PubMed] [Google Scholar]
- 55.Mackenbach JP, Stirbu I, Roskam A-JR, Schaap MM, Menvielle G, Leinsalu M, et al. Socioeconomic Inequalities in Health in 22 European Countries. N Engl J Med. 2008. June 5;358(23):2468–81. 10.1056/NEJMsa0707519 [DOI] [PubMed] [Google Scholar]
- 56.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004. April 1;159(7):702–6. 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 57.StataCorp. 2015. Stata Statistical Software: Release 14. Available from: https://www.stata.com/support/faqs/resources/citing-software-documentation-faqs/
- 58.DHS Program. The DHS Program—Protecting the Privacy of DHS Survey Respondents. Available from: https://dhsprogram.com/What-We-Do/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm
- 59.Bates K, Gjonça A, Leone T. Double burden or double counting of child malnutrition? The methodological and theoretical implications of stuntingoverweight in low and middle income countries. J Epidemiol Community Health. 2017. August;71(8):779–85. 10.1136/jech-2017-209008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Meshram II, Arlappa N, Balakrishna N, Laxmaiah A, Mallikarjun Rao K, Gal Reddy C, et al. Prevalence and Determinants of Undernutrition and its Trends among Pre-School Tribal Children of Maharashtra State, India. J Trop Pediatr. 2012. April 1;58(2):125–32. 10.1093/tropej/fmr035 [DOI] [PubMed] [Google Scholar]
- 61.Paul E, Mtumwa AH, Ntwenya JE, Vuai SAH. Disparities in Risk Factors Associated with Obesity between Zanzibar and Tanzania Mainland among Women of Reproductive Age Based on the 2010 TDHS. J Obes. 2016;2016:1420673 Epub 2016 Sep 18. 10.1155/2016/1420673; Available from: https://www.hindawi.com/journals/jobe/2016/1420673/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rahman M, Nakamura K, Kizuki M. Socioeconomic differences in the prevalence, awareness, and control of diabetes in Bangladesh. J Diabetes Complications. 2015. April 23;29. [DOI] [PubMed] [Google Scholar]
- 63.Biswas T, Uddin MJ, Mamun AA, Pervin S, P Garnett S. Increasing prevalence of overweight and obesity in Bangladeshi women of reproductive age: Findings from 2004 to 2014. PLoS ONE. 2017. July 28;12(7). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5533452/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mia MN, Rahman MS, Roy PK. Sociodemographic and geographical inequalities in under- and overnutrition among children and mothers in Bangladesh: a spatial modelling approach to a nationally representative survey. Public Health Nutr. 2018. May 2;1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Muhihi AJ, Njelekela MA, Mpembeni R, Mwiru RS, Mligiliche N, Mtabaji J. Obesity, Overweight, and Perceptions about Body Weight among Middle-Aged Adults in Dar es Salaam, Tanzania. Volume 2012, Article ID 368520, 6 pages; 10.5402/2012/368520 ISRN Obesity, 2012. Available from: https://www.hindawi.com/journals/isrn/2012/368520/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Krause KM, Lovelady CA, Østbye T. Predictors of Breastfeeding in Overweight and Obese Women: Data From Active Mothers Postpartum (AMP). Matern Child Health J. 2011. April 1;15(3):367–75. 10.1007/s10995-010-0667-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Asim M, Nawaz Y. Child Malnutrition in Pakistan: Evidence from Literature. Children. 2018. May 4;5(5). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5977042/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Faruque ASG, Ahmed AMS, Ahmed T, Islam MM, Hossain MI, Roy SK, et al. Nutrition: Basis for Healthy Children and Mothers in Bangladesh. J Health Popul Nutr. 2008;26(3):325–39. 10.3329/jhpn.v26i3.1899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rahman A. Significant risk factors for childhood malnutrition: evidence from an Asian developing country. Sci J Public Health. 2016;4(1–1):16–27. [Google Scholar]
- 70.Brennan L, McDonald J, Shlomowitz R. Infant feeding practices and chronic child malnutrition in the Indian states of Karnataka and Uttar Pradesh. Econ Hum Biol. 2004. March;2(1):139–58. 10.1016/j.ehb.2003.09.003 [DOI] [PubMed] [Google Scholar]
- 71.Malhotra N. Inadequate feeding of infant and young children in India: lack of nutritional information or food affordability? Public Health Nutr. 2013. October;16(10):1723–31. 10.1017/S1368980012004065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jordan A, Taylor Piotrowski J, Bleakley A, Mallya G. Developing Media Interventions to Reduce Household Sugar-Sweetened Beverage Consumption. Ann Am Acad Pol Soc Sci. 2012. March 1;640(1):118–35. [Google Scholar]
- 73.Simkhada P, Poobalan A, Simkhada P, Raja E, Aucott L. Knowledge,Attitude, and Prevalence of Overweight and Obesity Among Civil Servants in Nepal. Asia-Pac J Public Health Asia-Pac Acad Consort Public Health. 2009. October 1;23:507–17. [DOI] [PubMed] [Google Scholar]
- 74.Assaf S, Kothari MT, Pullum T. An assessment of the quality of DHS anthropometric data, 2005–2014. Rockville, Maryland, USA: ICF International; 2015. (DHS Methodological Reports No. 16). Available from: http://dhsprogram.com/pubs/pdf/MR16/MR16.pdf
- 75.Vaessen M. The potential of the demographic and health surveys (DHS) for the evaluation and monitoring of maternal and child health indicators. Demogr Eval Health Programme. 1996;65–74. [Google Scholar]
- 76.Wirth M, Wirth E, Delamonica E, Sacks D, Balk A, Minujin A. Monitoring health equity in the MDGs: a practical guide. N Y: CIESINUNICEF; 2006; [Google Scholar]
- 77.Rahman M, Berenson AB. Accuracy of current body mass index obesity classification for white, black, and Hispanic reproductive-age women. Obstet Gynecol. 2010. May;115(5):982–8. 10.1097/AOG.0b013e3181da9423 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The relevant data was obtained from MEASURE DHS and are available from the Demographic Health Surveys Program (Bangladesh Standard DHS, 2014- https://dhsprogram.com/data/dataset/Bangladesh_SPA_2014.cfm?flag=0; Nepal: Standard DHS, 2016- https://dhsprogram.com/data/dataset/Nepal_Standard-DHS_2016.cfm?flag=0; Myanmar: Standard DHS, 2015-16, https://dhsprogram.com/data/dataset/Myanmar_Standard-DHS_2016.cfm?flag=0; Pakistan: Standard DHS, 2012-13, https://dhsprogram.com/data/dataset/Pakistan_Standard-DHS_2012.cfm?flag=0).


