Abstract
Frontal sinus fractures are relatively rare maxillofacial injuries (only 5–15% of all facial fractures). The appropriate management of frontal sinus fracture and associated pathology is controversial. Diagnosis and treatment of frontal sinus fractures has improved with the advances of high-resolution computed tomography technology. Treatment of frontal sinus fractures depends on several factors, including contour deformity of anterior table; the presence of CSF leak or air–fluid level in the sinus, likelihood of nasofrontal duct obstruction, and degree of displacement of posterior table. Nasofrontal duct patency should be checked if fracture pattern is highly suspicious of ductal injury. Cranialization is performed in cases of severely comminuted posterior wall fracture. Long-term complication of frontal sinus fracture can occur up to 10 years after initial injury or intervention; so, judicious long-term follow-up is warranted. This article presents the management and complications of frontal sinus fractures.
Keywords: frontal sinus fracture, complications, management, calvarial bone graft
Frontal sinus fractures account for only 5 to 15% of all facial fractures in adult craniomaxillofacial trauma due to the increased thickness of the frontal bone. 1 The frontal bone can withstand 800 to 1,600 pounds of force, 2 thus confers resistance against most forms of traumatic injury. Motor vehicle accidents are the most common cause, followed by assaults and sports-related injuries. The appropriate management of frontal sinus fractures is a controversial and highly debated topic in craniomaxillofacial trauma and a lack of consensus exists in the current literature regarding the preferred treatment of frontal sinus fractures secondary to the fact that most clinical recommendations are derived from single-center retrospective case series with relatively small numbers of patients. Controversies exist in regards to the roles of frontal sinus obliteration, cranialization, and nasofrontal duct stenting in the acute trauma setting.
Anatomy and Physiology
The frontal sinuses are derived from the frontal recess portion of the middle meatus, the eventual location of the ostium of the nasofrontal duct or on occasion from air cells of the ethmoid infundibulum. They are absent at birth, development begins at age 2, becomes radiologically evident by age 8, and reach adult size at around age 12 years. About 4% of the population does not have a frontal sinus, and 10% with only a unilateral frontal sinus. An additional 4 to 5% have only rudimentary supraorbital air cells. 3 The sinuses are not simple chambers, but rather are often subdivided into subcompartments or recesses by incomplete bony partitions. The average height of the frontal sinus is 24 mm (range: 5–66 mm), and length is 29 mm (range: 17–49 mm). The boundaries of the sinus floor include the orbital roof inferiorly and the cribriform plate medially. The intersinus septum, an extension of the crista galli, separates the two sides of the frontal sinus. 4 The anterior wall is much thicker than the posterior wall, especially along the supraorbital buttress. The posterior wall is thinner (0.1–4 mm) and is not part of the transverse buttress system. The posterior wall is of mesodermal origin and due to the similar embryologic origin it is intimately adhered to the dural lining of the anterior cranial fossa. The dura becomes thinner and more adherent along the inferior edge and over the roof of the ethmoid air cells (fovea ethmoidalis). Significant fractures of the frontal bone can propagate easily and extensively along the orbital and nasoethmoid complex areas of lower tolerances to impact force.
The frontonasal ducts provide the drainage into the nasal cavity via the middle meatus. The hourglass-shaped frontonasal duct has an average diameter of 3 to 4 mm and consists of three parts: (1) a wide frontal infundibulum that drains into (2) a short, narrow ostium before expansion into (3) the ethmoid infundibulum. Located in the posteromedial segment of the sinus floor, the course is highly variable in length from a few millimeters up to 2 cm.
The mucosa of the frontal sinus consists of a pseudostratified ciliated columnar epithelium interspersed with goblet cells. Mucus is produced by these goblet cells which are primarily located within the caudal portion of each sinus cavity. A clinically significant anatomical structure of the mucosa of the frontal sinus is the foramina of Breschet. These foramina are sites of venous drainage of the mucosa and can serve as the route of spread of infection intracranially. Since the mucosa deeply invaginates, if not completely cleared from the foramina in sinus obliteration or cranialization, a potential risk of mucocele formation is created. 5
Diagnosis
The presence of a supraorbital ridge, glabella, or forehead laceration should raise suspicion for the presence of a frontal sinus fracture ( Fig. 1 ). Patients with frontal sinus fractures will often have visible depression in the supraorbital region that accompanies the soft-tissue compromise. Palpation over the suspected injury area may reveal crepitus, instability, and step-off. In patients with significant swelling, however, these physical findings are often masked. Sensory deficits are also common secondary to injury of the supratrochlear and or supraorbital nerves.
Fig. 1.
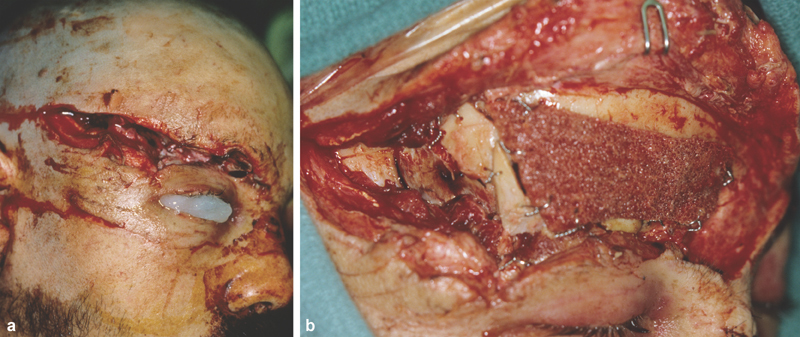
( a ) Lateral views of a patient with large forehead and glabellar laceration and frontal sinus fracture. ( b ) Lateral view of the same patient in a following rigid fixation with split calvarial bone graft.
Forces capable of disrupting the anterior table will frequently injure the posterior table and other elements of the craniofacial skeleton. A complete examination of the entire craniofacial skeleton is warranted. Because of the proximity of the globe, an ocular exam including evaluation of globe integrity, extraocular movements, visual fields, visual acuity, and pupillary response should be done. Fractures of the orbital roof that propagate to the orbital apex can cause superior orbital fissure and orbital apex syndromes. Occasionally, fractures of the frontal sinus will extend to the skull base beyond the anterior cranial into the middle cranial fossa. 6
Persistent clear nasal drainage should raise the suspicion of cerebrospinal fluid (CSF) rhinorrhea. This finding indicates a violation of the posterior table and dura tear that permits direct communication between brain and upper aerodigestive tract. The presence of β-2 transferrin is the gold standard for the diagnosis of CSF leak.
The advances in computed tomography (CT) technology have greatly enhanced diagnosis and treatment planning of frontal sinus fractures. CT scans have improved assessment of posterior wall and nasofrontal outflow tract injury. Nasofrontal outflow tract injury is found in 13 to 55% of the frontal sinus fracture cases 7 ; thus, preoperative determination of patency, if possible, is crucial to management. The two imaging findings of outflow tract obstruction are a sinus air–fluid level and fracture involvement of the tract in the sagittal view. 8 9 The index of suspicion should be high of an injury to the drainage tract in the presence of associated nasoethmoid fractures ( Fig. 2 ).
Fig. 2.
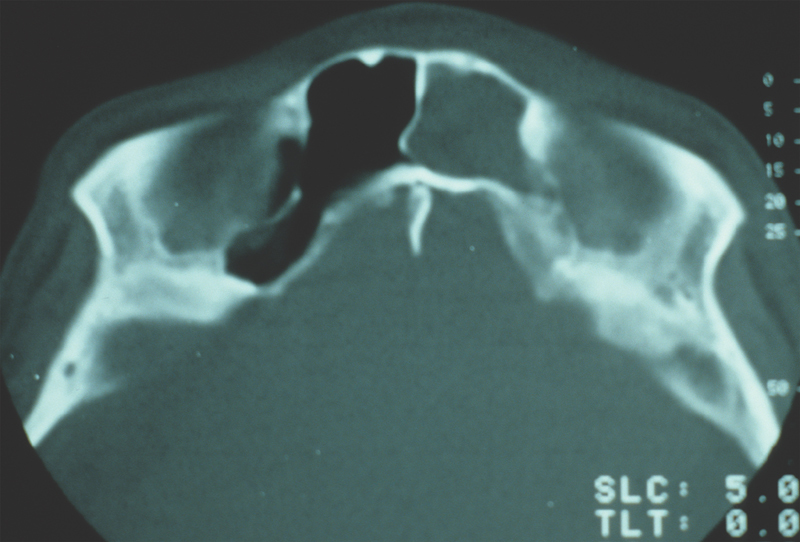
Axial computed tomographic image of a patient with disrupted nasofrontal duct.
Treatment
The ultimate goals in the management of frontal sinus fractures are restoration of form and function such as forehead contour and structural integrity, and prevention of early and late complications. Short-term complications include CSF leak, meningitis, and epidural abscess. Long-term complications include frontal bone osteomyelitis, mucocele, mucopyocele, and brain abscess. In 1954, Lewin demonstrated the risk of subsequent meningitis to be at least 25% in patients with CSF rhinorrhea and posterior table fracture in the absence of dural repair. 10 Surgical repair of dura reduced the overall risk of meningitis from 30% preoperatively to 4% after surgery with a reduction in the cumulative risk at 10 years from 85% before dural repair to 7% after dural repair. 11 In their 1998 publication, Sakas et al identified several factors on neuroimaging that were linked to high long-term risk of developing posttraumatic meningitis 12 :
Proximity of the fracture to the midline cribriform plate.
Large fracture displacement (>1 cm).
Prolonged rhinorrhea (>8 days).
Treatment decisions depend on fracture type, comminution, degree of posterior table fracture, nasofrontal duct injury, neurological status, and CSF leak. 13 Rodriguez et al developed a treatment algorithm based on the fracture patterns with consideration for nasofrontal outflow tract injury. 14 In nondisplaced fractures of frontal sinus with a patent nasofrontal duct, only clinical observation with head elevation and sinus precaution is needed. For frontal sinus fractures with nasofrontal duct outflow obstruction, either sinus obliteration or cranialization is indicated depending on posterior wall involvement. In displaced frontal sinus fractures with no obstruction of the nasofrontal duct, reconstruction of the anterior wall is indicated.
Adequate exposure of the affected region is crucial for intraoperative assessment of the fracture. Existing lacerations are useful only in cases of minor isolated anterior table fractures. Most commonly, the fractures should be exposed with a bicoronal incision. The coronal flap is elevated in the subgaleal plane, and dissection extends inferiorly to supraorbital rims and nasoglabellar junction medially and frontozygomatic suture line laterally. Some consideration should be given to the necessity of a pericranial flap. If so, the dissection at a point 6 to 8 cm from the supraorbital rims shifts from subgaleal to the subperiosteal plane. If not, the subperiosteal plane is entered 2 cm superior to enable protection of the supraorbital nerve and artery.
For isolated displaced anterior table fractures, standard reduction and rigid fixation is sufficient. Low profile 1.0-mm microplates are used in palpable areas. If frontonasal duct injury is suspected, the duct is first examined for patency prior to fixation. Fragments are disimpacted and removed to visualize the base of the sinus frontonasal ducts. Methylene blue is injected into the duct with a polyethylene catheter and a cotton tip applicator or cottonoids are placed into the nose near the middle meatus ( Fig. 3a ). If dye is detected, the frontonasal ducts are patent ( Fig. 3b ). If no dye is visualized or if significant doubt exists about frontonasal patency, the sinus should be obliterated. Frontal sinus obliteration is defined as obliteration of the aerated frontal sinus cavity during the maintenance of intact bony walls. Sinus mucosa is removed and mucosal curettage is performed with high speed burr. Attention is directed particularly along the posterior sinus wall toward the foramina of Breschet. The frontonasal duct can be plugged with a pericranial flap 15 ( Fig. 4 ). The optimal method for frontal sinus obliteration has been the subject of great debate. Many graft options exist including fat, dermis, fascia, muscle, bone, and alloplastic material such as silicone, Surgicel, and hydroxyapatite. 16 17 18 However, alloplastic material is not recommended because the surgical site is considered a contaminated area and the increased risk of postoperative infection. Spontaneous osteoneogenesis has been described for frontal sinus obliteration in which nothing is placed in the sinus to allow fibrous tissue ingrowth and formation of new bone. 19 In the experimental setting, the obliteration is often incomplete and complicated by infection. Rohrich and Mickel compared frontal sinus obliteration using fat, muscle, bone, and spontaneous osteoneogenesis in a cat model and literature review found no differences in the material used. 20 They concluded that successful obliteration of frontal sinus by either spontaneous osteoneogenesis or the implantation of autogenous fat, muscle, or bone depends on meticulous extirpation of the frontal sinus mucosa with the aid of an operating microscope, removal of the inner cortex of bone, and permanent occlusion of the nasofrontal duct. 20 21 Cranialization should be considered when the anatomic barrier between the sinus and intracranial cavity has been disrupted secondary to fractures of the posterior wall and dural tears. 22 Cranialization involves removal of the entire posterior sinus wall and debridement of all sinus mucosa, followed by frontonasal duct blockade with pericranial flap and/or autogenous bone ( Fig. 5a–d ).
Fig. 3.
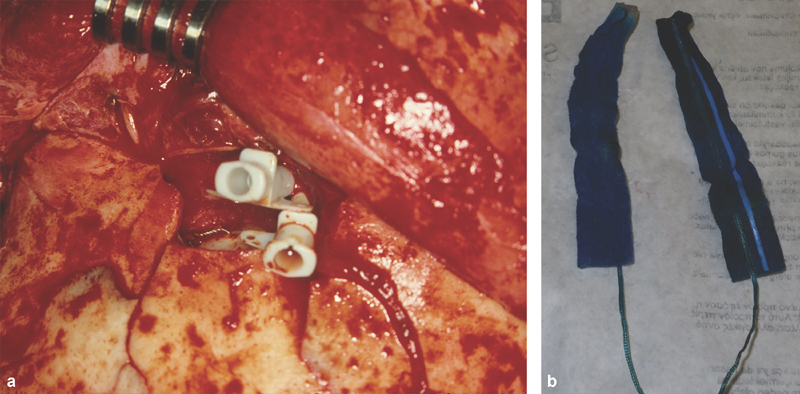
( a ) Intraoperative view demonstrates polyethylene catheters cannulating nasofrontal ducts. ( b ) Cottonoids with stained methylene blue demonstrating patent nasofrontal ducts.
Fig. 4.
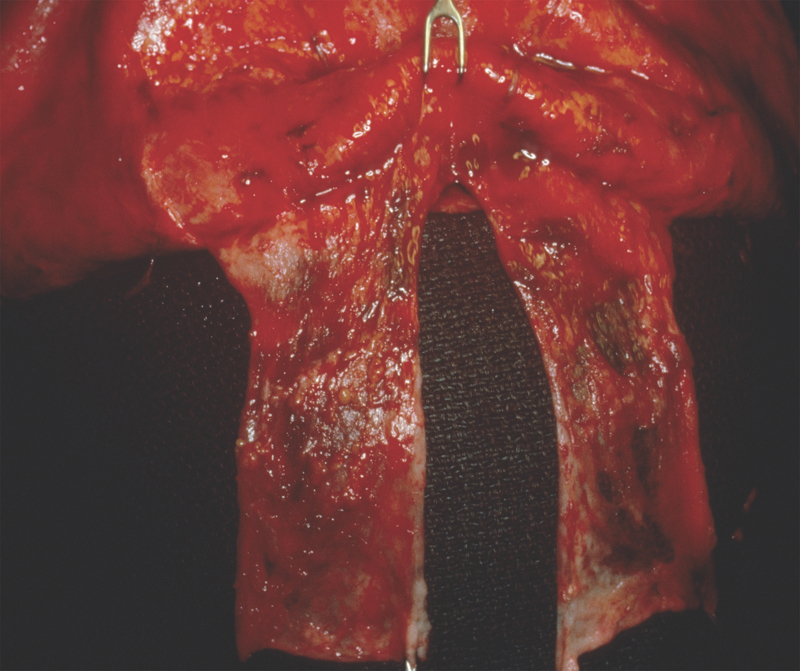
Intraoperative view of frontal sinus with pericranial flap.
Fig. 5.
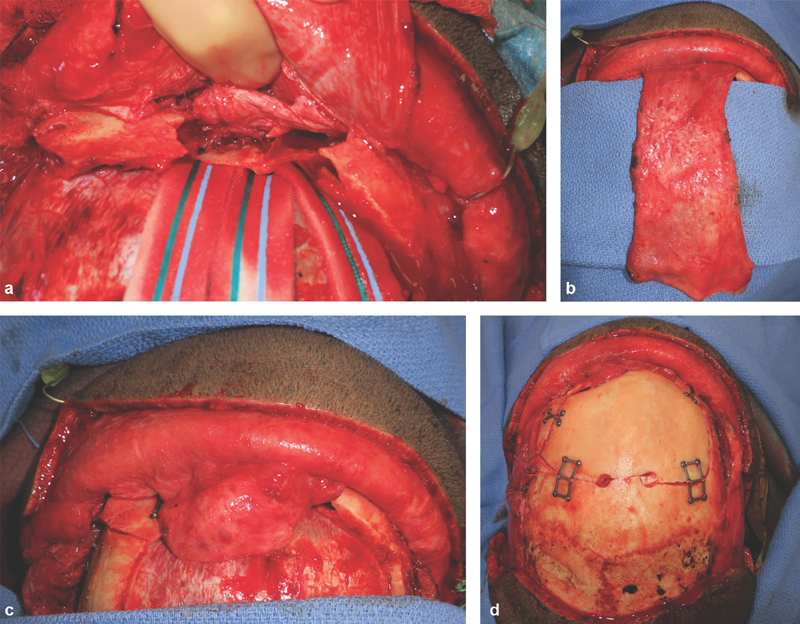
( a–d ) Cranialization of the frontal sinus using bone fragments and pericranial flap. Appearance of patient after rigid anatomic fixation.
In cases of severe comminution, bony loss, and instability, reconstruction of the anterior table can be done with autogenous bone graft. There are several sources for nonvascularized autologous bone graft including calvarium, ribs, ilium, temporal fossa, and patella. 23 24 Free rib grafts have been shown to partially resorb, thus leading to secondary deformities. Although iliac bone has been used extensively in the past, at present most surgeons prefer split calvarial bone graft 25 ( Fig. 6 ).
Fig. 6.
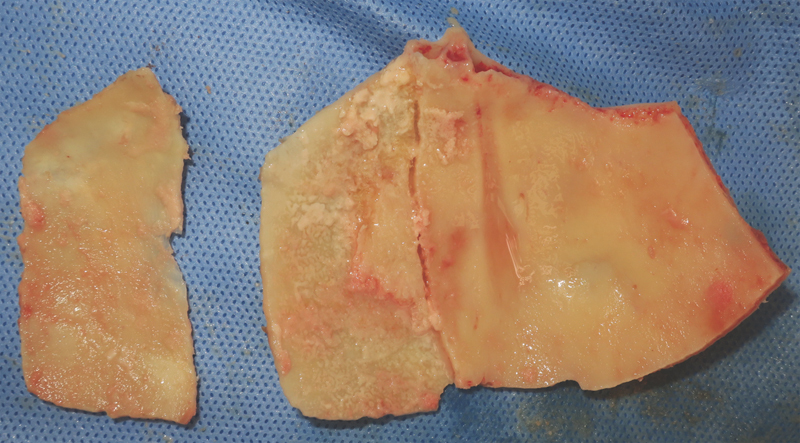
Intraoperative view of a split calvarial bone graft.
Complications
Early complications occur within the first few weeks of surgery. Intracranial hemorrhage pneumocephalus, cerebral contusion, and increased intracranial pressure are associated with frontal sinus fractures but are relatively uncommon. Contour deformities can occur, particularly when observation alone has been the mode of treatment ( Fig. 7 ). Paresthesias in the supratrochlear and supraorbital distributions are usually transient but have a long-term incidence of permanent dysesthesia of 5%. The most significant early complication is a CSF leak. CSF leaks are troublesome in the presence of intracranial injury. Postoperative CSF rhinorrhea is usually secondary to a fracture of the cribriform plate or other basilar skull fracture. Conservative management is indicated in most instances. The indications for procedures to address this scenario are beyond the scope of this discussion.
Fig. 7.

Frontal view of a patient with untreated frontal sinus fracture; note the visible deformity of the forehead.
Meningitis can occur in frontal sinus fracture patients and may not be associated with an active CSF leak. 26 As these patients may be neurologically compromised from a head injury, they are uniquely susceptible to the consequences of meningitis. Attention should be directed toward postoperative patients for signs of fever, hypotension, mental status changes, or neck rigidity. Use of broad-spectrum antibiotics with good CSF penetration is an essential first step. Antibiotics should be adjusted following the results of CSF cultures.
Mucoceles or mucopyocele are long-term complications from untreated fractures or failure to recognize frontonasal duct obstruction. Sinus malfunction proceeds through an indolent course and presents many years after initial frontal sinus injury management. 27 The natural course for a mucocele is slow, insidious expansion following the initial injury. 28 Mucoceles cause progressive bone erosion and are capable of involvement of the sinus, the orbit, and the cranium. 29 Since mucoceles are slow growing and produce few symptoms, they present late in their development only after orbital or cranial invasion has already occurred. The most frequent complaints are frontal headache, nasal purulent drainage, frontal sinus tenderness, and fluctuant swelling of the forehead. Secondary involvement of the orbit creates visual disturbances, orbital dystopia, and ocular dysfunction. Central nervous system sequelae may present with more serious clinical signs and symptoms, such as seizures, headaches, photophobia, and nuchal rigidity. Complete removal of the mucocele and reconstruction of the cranial vault or orbit and nasal cavity is the treatment method of choice. 30
Frontal bone osteomyelitis is a rare complication and occurs mostly in frontal sinus fractures when alloplastic material has been implanted that subsequently becomes secondarily infected. Osteomyelitis requires complete excision of the involved frontal bone, treatment with long-term antibiotics, and subsequent reconstruction of the frontal bone after infection has resolved.
Various options are available to correct contour deformities of the forehead: autogenous bone such as split calvarial bone graft or allogenic products such as demineralized bone matrix (DBM). DBM is produced after acid extraction of donor stock long diaphyses, retaining the collagen scaffold for osteoconduction and growth factors, such as bone morphogenic protein. The quantity of bone morphogenic protein in different preparations of DBM varies considerably by commercial vendors. Commercial DBM has been mixed with carriers such as hyaluronan (DBX; Synthes USA, West Chester, PA), calcium sulfate (Allomatrix; Wright Medical Technology, Inc., Arlington, TN), glycerol (Grafton; Osteotech, Eatontown, NJ), or gelatin (Regenafil; Regeneration Technologies Inc, Alachua, FL) for improved clinical handling and localization of DBM particles within the surgical recipient site. Acarturk and Hollinger 31 have demonstrated in their animal model that DBX and Grafton produce more bone formation than Allomatrix, Dynagraft, and Regenafil due to the quantity of particulate DBM within the critical size defect and perhaps because DBX and Grafton are more localized to the implant site.
Minimally Invasive and Nonoperative Management
The operative management of frontal sinus fractures implies access via a bicoronal incision, an approach not devoid of negative implications including, on occasion, an unsatisfactory scar. In some patients with receding frontal hairline, those implications become more of a concern. As a result, some interest exists in either a less invasive or a nonoperative approach, particularly perhaps in patients with isolated anterior wall fractures, patients in whom the treatment indications are primarily aesthetic.
Investigators have described an endoscopic approach, either through a brow incision, hairline, or transnasal access. 32 33 These approaches have either utilized the endoscope to enable a small skin incision for reduction without internal fixation or endoscopic confirmation by a transnasal passage to ascertain the patency of the nasofrontal duct. The liability of an endoscopic technique is the inability to perform, with any degree of facility, internal fixation of the reduced anterior wall fragments. A transnasal endoscopic procedure does enable assessment of the frontal sinus drainage system but often requires a variation of an internal ethmoidectomy as well as increased operative time and a steep learning curve. Nevertheless, with development of the technology, a minimally invasive approach to frontal sinus fractures may play a more prominent role in the future.
In the same vein, some recent interest in a selected conservative management of a band of the spectrum of frontal sinus fractures has been discussed. 34 If an acuity exists of frontal sinus fractures from least, namely, nondisplaced anterior wall to that of the most severe, open, comminuted injuries with bone loss, attended by disruption of the posterior wall, dural tears, and CSF leak, an opportunity exists perhaps for the nonoperative treatment of the lesser degree of severity. Posterior wall injury and/or outflow tract obstruction merits operative intervention primarily because of the nature of the potential complications, epidural/subdural abscess, or mucopyocele. Conceivably, as described, an anterior wall fracture even with some degree of displacement could be managed with observation alone, further treatment dictated by follow-up examination including CT scan.
Summary
The treatment of frontal sinus fractures has evolved with the advent of diagnostic tools and treatment materials. The current management of frontal sinus fracture is based on three findings: posterior table involvement or not, patency of frontonasal duct, and magnitude of anterior table displacement. Long-term follow-up of this patient population is necessary as mucocele can develop as late as several years after the initial injury.
Footnotes
Conflict of Interest None.
References
- 1.Gerbino G, Roccia F, Benech A, Caldarelli C. Analysis of 158 frontal sinus fractures: current surgical management and complications. J Craniomaxillofac Surg. 2000;28(03):133–139. doi: 10.1054/jcms.2000.0134. [DOI] [PubMed] [Google Scholar]
- 2.Nahum A M. The biomechanics of maxillofacial trauma. Clin Plast Surg. 1975;2(01):59–64. [PubMed] [Google Scholar]
- 3.McLaughlin R B, Jr, Rehl R M, Jr, Lanza D C. Clinically relevant frontal sinus anatomy and physiology. Otolaryngol Clin North Am. 2001;34(01):1–22. doi: 10.1016/s0030-6665(05)70291-7. [DOI] [PubMed] [Google Scholar]
- 4.Hollinshead W H. New York: Harper and Row; 1968. Anatomy of Surgeons, Vol. 1: Head and Neck; p. 283. [Google Scholar]
- 5.Donald P J. The tenacity of the frontal sinus mucosa. Otolaryngol Head Neck Surg (1979) 1979;87(05):557–566. doi: 10.1177/019459987908700502. [DOI] [PubMed] [Google Scholar]
- 6.Levine S B, Rowe L D, Keane W M, Atkins J P., Jr Evaluation and treatment of frontal sinus fractures. Otolaryngol Head Neck Surg. 1986;95(01):19–22. doi: 10.1177/019459988609500105. [DOI] [PubMed] [Google Scholar]
- 7.Chen K T, Chen C T, Mardini S, Tsay P K, Chen Y R. Frontal sinus fractures: a treatment algorithm and assessment of outcomes based on 78 clinical cases. Plast Reconstr Surg. 2006;118(02):457–468. doi: 10.1097/01.prs.0000227738.42077.2d. [DOI] [PubMed] [Google Scholar]
- 8.Heller E M, Jacobs J B, Holliday R A. Evaluation of the frontonasal duct in frontal sinus fractures. Head Neck. 1989;11(01):46–50. doi: 10.1002/hed.2880110109. [DOI] [PubMed] [Google Scholar]
- 9.Kasper K A. Nasofrontal connections: a study based on 100 consecutive dissections. Arch Otolaryngol. 1936;23:322. [Google Scholar]
- 10.Lewin W. Cerebrospinal fluid rhinorrhoea in closed head injuries. Br J Surg. 1954;42(171):1–18. doi: 10.1002/bjs.18004217102. [DOI] [PubMed] [Google Scholar]
- 11.Eljamel M SM, Foy P M. Post-traumatic CSF fistulae, the case for surgical repair. Br J Neurosurg. 1990;4(06):479–483. doi: 10.3109/02688699008993796. [DOI] [PubMed] [Google Scholar]
- 12.Sakas D E, Beale D J, Ameen A A et al. Compound anterior cranial base fractures: classification using computerized tomography scanning as a basis for selection of patients for dural repair. J Neurosurg. 1998;88(03):471–477. doi: 10.3171/jns.1998.88.3.0471. [DOI] [PubMed] [Google Scholar]
- 13.Wolfe S A, Johnson P. Frontal sinus injuries: primary care and management of late complications. Plast Reconstr Surg. 1988;82(05):781–791. [PubMed] [Google Scholar]
- 14.Rodriguez E D, Stanwix M G, Nam A J et al. Twenty-six-year experience treating frontal sinus fractures: a novel algorithm based on anatomical fracture pattern and failure of conventional techniques. Plast Reconstr Surg. 2008;122(06):1850–1866. doi: 10.1097/PRS.0b013e31818d58ba. [DOI] [PubMed] [Google Scholar]
- 15.Thaller S R, Donald P. The use of pericranial flaps in frontal sinus fractures. Ann Plast Surg. 1994;32(03):284–287. doi: 10.1097/00000637-199403000-00010. [DOI] [PubMed] [Google Scholar]
- 16.McNeil R A. Surgical obliteration of the maxillary sinus. A clinical and experimental study. Laryngoscope. 1967;77(02):202. doi: 10.1288/00005537-196702000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Lierle D M, Huffman W C. A simplified method of obliterating frontal bone defects. Laryngoscope. 1949;59(01):61–65. doi: 10.1288/00005537-194901000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Shumrick K A, Smith C P. The use of cancellous bone for frontal sinus obliteration and reconstruction of frontal bony defects. Arch Otolaryngol Head Neck Surg. 1994;120(09):1003–1009. doi: 10.1001/archotol.1994.01880330081015. [DOI] [PubMed] [Google Scholar]
- 19.Gibson T, Walker F M. Large osteoma of the frontal sinus; a method of removal to minimize scarring and prevent deformity. Br J Plast Surg. 1951;4(03):210–217. doi: 10.1016/s0007-1226(51)80037-7. [DOI] [PubMed] [Google Scholar]
- 20.Rohrich R J, Mickel T J. Frontal sinus obliteration: in search of the ideal autogenous material. Plast Reconstr Surg. 1995;95(03):580–585. [PubMed] [Google Scholar]
- 21.Mickel T J, Rohrich R J, Robinson J B., Jr Frontal sinus obliteration: a comparison of fat, muscle, bone, and spontaneous osteoneogenesis in the cat model. Plast Reconstr Surg. 1995;95(03):586–592. [PubMed] [Google Scholar]
- 22.Sataloff R T, Sariego J, Myers D L, Richter H J. Surgical management of the frontal sinus. Neurosurgery. 1984;15(04):593–596. doi: 10.1227/00006123-198410000-00023. [DOI] [PubMed] [Google Scholar]
- 23.Schortinghuis J, Zeebregts C J, Bos R R. Frontal bone reconstruction using patellar bone: a case report. J Oral Maxillofac Surg. 1999;57(09):1132–1133. doi: 10.1016/s0278-2391(99)90340-3. [DOI] [PubMed] [Google Scholar]
- 24.Kohan D, Plasse H M, Zide B M.Frontal bone reconstruction with split calvarial and cancellous iliac bone Ear Nose Throat J 19896811845–846., 848–850, 853–854 [PubMed] [Google Scholar]
- 25.Luce E A. Frontal sinus fractures: guidelines to management. Plast Reconstr Surg. 1987;80(04):500–510. doi: 10.1097/00006534-198710000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Manolidis S, Hollier L H., Jr Management of frontal sinus fractures. Plast Reconstr Surg. 2007;120(07) 02:32S–48S. doi: 10.1097/01.prs.0000260732.58496.1b. [DOI] [PubMed] [Google Scholar]
- 27.Weitzel E K, Hollier L H, Calzada G, Manolidis S. Single stage management of complex fronto-orbital mucoceles. J Craniofac Surg. 2002;13(06):739–745. doi: 10.1097/00001665-200211000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Wilson B C, Davidson B, Corey J P, Haydon R C., III Comparison of complications following frontal sinus fractures managed with exploration with or without obliteration over 10 years. Laryngoscope. 1988;98(05):516–520. doi: 10.1288/00005537-198805000-00008. [DOI] [PubMed] [Google Scholar]
- 29.LaRossa D D, Noone R B, Jackson P. Facial deformity from frontal sinus mucocele: single stage surgical correction. Case report. Plast Reconstr Surg. 1977;60(06):917–919. doi: 10.1097/00006534-197712000-00019. [DOI] [PubMed] [Google Scholar]
- 30.Bordley J E, Bosley W R. Mucoceles of the frontal sinus: causes and treatment. Ann Otol Rhinol Laryngol. 1973;82(05):696–702. doi: 10.1177/000348947308200513. [DOI] [PubMed] [Google Scholar]
- 31.Acarturk T O, Hollinger J O. Commercially available demineralized bone matrix compositions to regenerate calvarial critical-sized bone defects. Plast Reconstr Surg. 2006;118(04):862–873. doi: 10.1097/01.prs.0000232385.81219.87. [DOI] [PubMed] [Google Scholar]
- 32.Kellman R, Goyal P. Managing the frontal sinus in the endoscopic age: has the endoscope changed the algorithm? Craniomaxillofac Trauma Reconstr. 2014;7(03):203–212. doi: 10.1055/s-0034-1371773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Egemen O, Özkaya Ö, Aksan T, Bingöl D, Akan M. Endoscopic repair of isolated anterior table frontal sinus fractures without fixation. J Craniofac Surg. 2013;24(04):1357–1360. doi: 10.1097/SCS.0b013e3182902518. [DOI] [PubMed] [Google Scholar]
- 34.Weathers W M, Wolfswinkel E M, Hatef D A, Lee E I, Brown R H, Hollier L H., Jr Frontal sinus fractures: a conservative shift. Craniomaxillofac Trauma Reconstr. 2013;6(03):155–160. doi: 10.1055/s-0033-1349210. [DOI] [PMC free article] [PubMed] [Google Scholar]


