Abstract
Overlooked injured structures in periorbital trauma could lead to aesthetic and functional deficits. As trauma may affect superficial, middle, and deep components, meticulous survey guided by a structured periorbital trauma classification is needed for proper management. Thus, a new classification for periorbital trauma is proposed to serve this purpose. Periorbital region was defined anatomically by anthropometric landmarks. The periorbital injuries were categorized according to anatomical and clinical basis. The new classification was used to study periorbital trauma cases received at Ain Shams University Hospitals between July 2013 and July 2016 retrospectively. The study included 260 patients: 196 (75.38%) males and 64 (24.62%) females. The type and severity of injury, time of primary intervention, type of surgery performed, and patients' visits to the outpatient clinic were evaluated. The status of the postinjury and postoperative (primary surgery) aesthetic status and functional status were evaluated. The periorbital region was identified. Anatomical categorization of periorbital injuries included periocular, frontal, temporal, and malar regions. Injuries/deficits were categorized into simple, composite, complex, and isolated bony injuries according to the depth and involved tissues. Subsequently, the classification was formulated. In the retrospective study, the incidence of extended simple injuries was the highest, while the least was the extended complex injuries. Functional deficits occurred in 24 patients (9.23%) and aesthetic deficits occurred in 55 patients (21.15%). Required secondary operations for this group included redo of fixation, correction of medial canthal ligament, repair of canalicular system, scar revisions, fat grafting, and creation of natural creases. The results of this study demonstrated that unsatisfactory aesthetic and functional results occurred when injuries of important structures were overlooked, aesthetic units were not respected, and when management was delayed. A three-dimensional, oriented, new classification of periorbital trauma based on anatomical and clinical categorization is proposed to help in identifying injured structures, stimulate the search for other injuries, structure preoperative evaluation, and recommend a surgical plan that would ultimately achieve precise primary repair with best aesthetic and functional outcome.
Keywords: periorbital trauma, classification, functional and aesthetic outcomes
The periorbital region is an important aesthetic region that is formed by complexity of tissues. Some authors used “periocular region” and “periorbital region” as interchangeable terms. Either region was described as the area including the upper eyelids, lower eyelids, and canthal regions. 1 2 3 4 5 6 7 8
The periorbital trauma could vary from simple to complicated injuries. The injury of important structures such as the medial canthus ligament and lacrimal system can be overlooked and missed in the surgical management. A survey of all structures must be done and documented. Facial injuries and deformities were usually classified according to the anatomic location, 9 fractures pattern, 10 severity, 11 12 13 14 15 16 or mechanism of injury. 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 Mokal and Desai stated that no classification system is entirely satisfactory in taking into account the mix of soft and bony tissue deficits and the resulting functional and aesthetic deformities. 33
The primary repair of bones and soft tissues requires thorough examination, imaging, and the awareness that low clinical suspicion for a fracture may not exclude significant soft tissue injury. 8 34 Multidisciplinary work may be required in severe cases due to the proximity of the vital structures in the craniofacial and skull-base region. 35 In such cases, delayed treatment may be associated with an increased risk of infection, 36 37 38 and increased soft-tissue swelling, obscuring landmarks and making it more difficult to determine definite boundaries of the lesion. 39
In our institution, we have faced a considerable number of cases presenting with complications and deformities after late or mismanagement of periorbital injuries. The authors worked on setting a three-dimensional clinical and anatomical classification for injuries of periorbital trauma emphasizing on periorbital trauma survey. The new classification is proposed to help in preoperative evaluation and surgical planning for management of periorbital region. The identification of injured structures and meticulous primary repair are emphasized to avoid late functional and aesthetic complications.
Patients and Methods
Retrospective study of patients with periorbital trauma who presented to Ain Shams University Hospitals between July 2013 and July 2016 were included in this study with institutional review board approval. The periorbital region and subunits were identified using anthropometric landmarks. A new classification of periorbital trauma was formulated. The periorbital injuries were categorized according to anatomical and clinical basis. The periorbital trauma cases were reviewed all through the patient care and the follow-up period. Data were reviewed with regard to type and severity of injury, time of primary intervention, type of surgery, and patients' visits to the outpatient clinic. The status of the postinjury and postoperative (primary surgery) aesthetic and functional status were reviewed as shown in Table 1 and Table 2 . The incidence of the functional and aesthetic deficits in each category of periorbital trauma injuries was statistically analyzed using the “Exact” test. The incidence of functional and aesthetic deficits was correlated to time of intervention, site of injury, and depth of injury of periorbital trauma injuries using the “chi-squared” test and the “Exact” test.
Table 1. Evaluation of functional status.
| Function | Status |
|---|---|
| Eye globe | Globe rupture |
| Vision | Affected vision, blindness |
| Diplopia | |
| Position | Limited globe movement |
| Disturbed globe position as enophthalmos, exophthalmos | |
| lacrimal system | Integral without epiphora |
| Interrupted with epiphora | |
| Dacryocystitis | |
| Levator palpebrae superioris muscle | Full excursion |
| Ptotic lid | |
| Medial canthus and naso-orbital valley | Restored |
| Obliterated | |
| ± Epicanthal fold | |
| Telecanthus | |
| Lateral canthus | Normal |
| Mal-insertion | |
| Facial animation | Normal |
| Facial paralysis | |
| Sensory function | Intact |
| Numbness | |
| Decreased sensation | |
| Mouth opening | None |
| Difficult/limited |
Table 2. Evaluation of aesthetic status.
| Aesthetic feature | Status |
|---|---|
| 3D topography | Preserved/restored |
| Not restored | |
| Symmetry | Normal |
| Asymmetry | |
| Dystopia | |
| Facial harmony | Normal |
| Affected facial width or depth | |
| Deformities | Irregularities |
| Depression | |
| Bulge | |
| Deviation | |
| Eyebrow | Normal |
| Disfigured | |
| Loss of hair | |
| Eye lid | Loss/deficiencies |
| Scleral show/lid retraction | |
| Nasal root | Normal |
| Depressed | |
| Scars | None |
| Well-placed fine scar | |
| Soft-tissue contracture | |
| Conspicuous | |
| Natural creases | Normal |
| Loss of crease/line between subunits |
Results
The periorbital region was defined anatomically by anthropometric landmarks. It was outlined between trichion (tr), tragion (t), zygion, alare (al), maxillofrontale (mf), and sellion (se) bilaterally as shown in Fig. 1 .
Fig. 1.
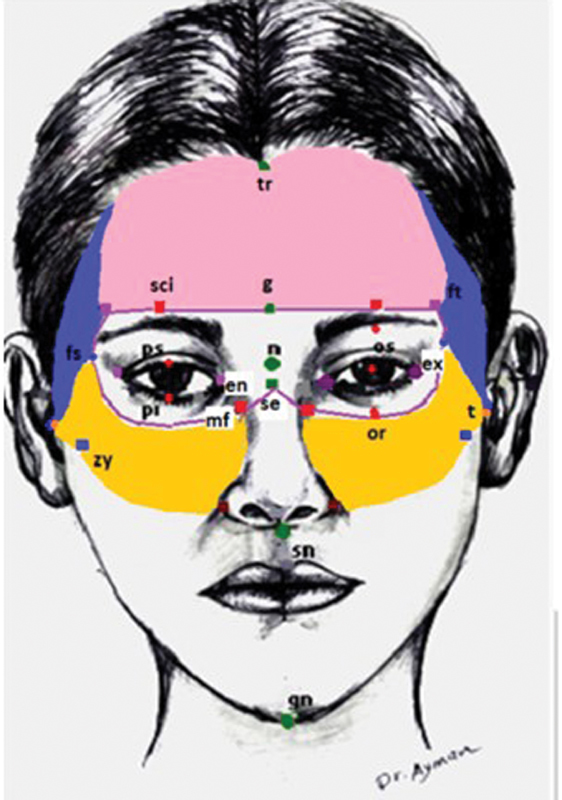
Areas of periorbital region: periocular region: (g.-sci.-ft.-fs.-or.-mf.-se.-mf.-or.-fs.-ft.-sci.-g.), frontal region (tr.-ft.-sci.-gl.-sci.-ft. tr.), temporal region: lateral to frontal and ocular regions, malar region (fs.-or.-mf.-al.-zy.-t.). Facial landmarks : trichion (tr), frontotemporale (ft), glabella (g), fronto-supraorbitale (fs), zygion (zy), tragus (t). Orbital landmarks : endocanthion (en), exocanthion (ex), palpebrale superius (ps), palpebrale inferius (pi), supraciliary (sci), orbitale inferius (or). Nasal landmarks : nasion (n), sellion (se), maxillofrontale (mf), alare (al).
The periorbital trauma classification was outlined including the clinical subcategories: superficial, middle, and deep components. Thus, trauma/deficits could be classified into simple, composite, complex, and isolated bony lesions. The simple lesion affects one soft-tissue component. The composite lesion affects more than one soft-tissue component. The complex lesion affects all layers. Isolated bony lesion affects only bone without affection of the overlying layers. Each lesion will be subclassified into localized and extended. The localized trauma affects one anatomical subunit, while the extended trauma affects more than one subunit. Thus, there are four main groups according to anatomical and clinical classifications: simple traumatic lesions, composite traumatic lesions, complex traumatic lesions, and isolated bony lesions. Each is subclassified into localized and extended. Fig. 2 shows the classification of periorbital trauma.
Fig. 2.
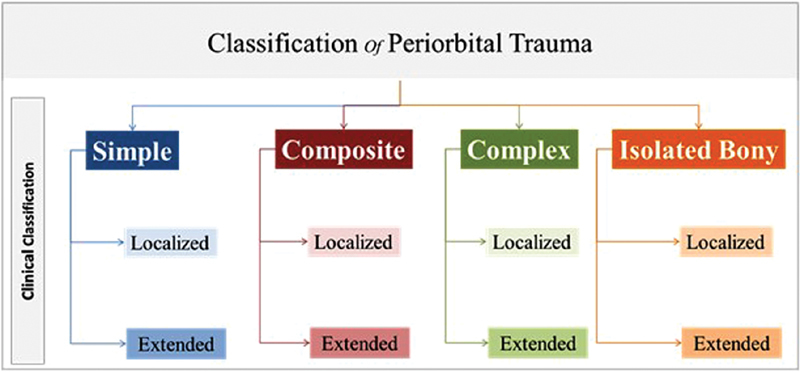
Classification of periorbital trauma.
It was noticed that patients with complications or concerns had more frequent visits to the outpatient clinic and prolonged follow-up period. Most of them came after subsidence of soft-tissue edema. Some cases came after 6 months. Few came after 1 year.
The retrospective study included 260 patients; 196 patients were males (75.38%) and 64 patients were females (24.62%). Patients' age ranged between 3 and 62 years. Mean age was 41 years. Graph 1 shows incidence of different types of periorbital injuries. The duration of postoperative edema was prolonged in the extended complex cases. It usually subsided after 3 weeks except rarities like the growing skull fractures.
Graph 1.
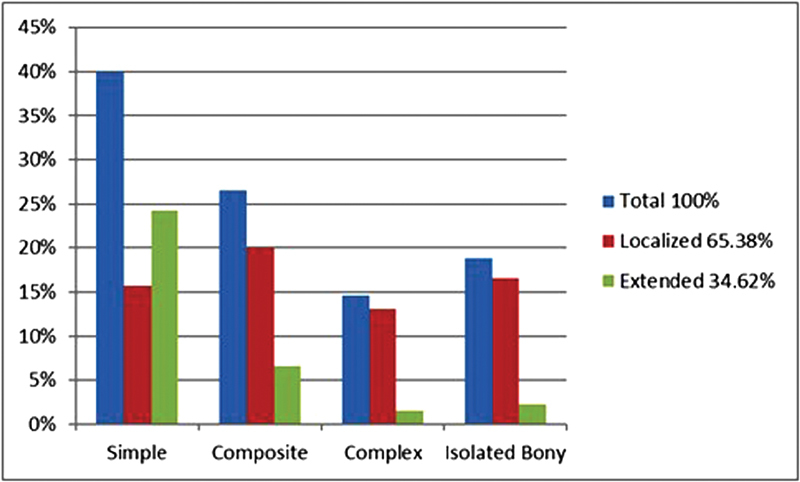
Incidence of different types of periorbital injuries.
Evaluation of the functional and the aesthetic outcomes after primary intervention revealed that functional deficits occurred in 24 patients (9.23%) and aesthetic deficits occurred in 55 patients (21.15%). Aesthetic outcome was affected by the functional deficit in (8.08%) of cases which had presented late. Table 3 shows types of injuries and results of postoperative functional and aesthetic outcomes after primary intervention. It also showed the cases which had restored good function after surgical intervention.
Table 3. Types of injuries and results of functional and aesthetic outcomes after primary intervention.
| Type | Subunit | No. | Main injury | Functional outcomes | Aesthetic outcome |
|---|---|---|---|---|---|
| Simple | Periocular | 25 | Skin wounds | – | Three cases needed revision |
| 1 | Levator palpebrae superioris injury | Ptosis | Poor a | ||
| Frontal | 10 | Skin wounds | – | Three cases needed revision | |
| Malar | 5 | Skin wounds | – | One case needs revision | |
| Extended | 63 | Skin wounds | – | Nine cases need scar revisions | |
| Composite | Periocular | 10 | Skin lacerations + cut levator injury | Two cases with ptosis (due to delayed interference) | Two cases were poor a |
| 8 | Skin lacerations + tear of medial canthus | Two cases needed re-fixation of medial canthal ligament |
Two cases were average
a
Two cases had epicanthal fold and needs revision |
||
| 16 | Skin lacerations + tarsus, conjunctiva ± lacrimal canaliculi | Two cases with disturbed lacrimal system | One case needs scar revision Two cases have minor eyelid colobomas |
||
| 6 | Skin lacerations + eyelid structures (tarsus, conjunctiva) + globe affection | RGF | One case needs scar revision | ||
| Frontal | 0 | – | – | – | |
| Temple | 4 | Lacerated skin and muscles | RGF | Good | |
| Malar | 8 | Lacerated skin and muscles | RGF | Two cases needed fat injection to achieve symmetry | |
| Extended | 5 | Periocular + frontal + temporal | One case needed re-fixation of medial canthal ligament |
Two cases were average
a
Four patients had loss of crease/line between subunits |
|
| 4 | Periocular + malar | RGF | |||
| 8 | Periocular + frontal | One case needed re-fixation of medial canthal ligament | |||
| Complex | Periocular | 16 | Eyelid injuries with orbital fractures | Five cases had enophthalmos | Five cases were average a |
| Two case had telecanthus required redo | Two cases were poor a | ||||
| 8 | Naso-orbital ethmoidal fractures + tear of medial canthal ligament | One case was not corrected | One case with depressed nasal root and shortened nose | ||
| Frontal | 10 | Frontal sinus fractures + lacerated skin | RGF | Two cases needed correction of irregularities of frontal bone | |
| Temple | 0 | – | – | – | |
| Malar | 0 | – | – | – | |
| Extended cases | 2 | Orbital fractures/nasoethmoid + frontal sinus fracture ± tear of medial canthal ligament | RGF | One case needed scar revision and correction of irregularities of frontal bone | |
| 2 | Orbital fractures + zygoma and maxilla + tear of medial canthal ligament | One case had telecanthus orbital dystopia | One case had conspicuous scar | ||
| Isolated bone lesion | Periocular | 22 | Orbital fractures Mainly blow-out inferior orbital fracture |
Four have mild enophthalmos | Four cases were average a |
| Three have entrapped muscle with limited upper gaze | Three cases were average a | ||||
| Frontal | 9 | Frontal sinus fractures | RGF | One case had forehead irregularities | |
| Temple | 0 | – | – | – | |
| Malar | 12 | Fracture zygomatic arch | Improved painful mastication in all | Two cases had prominent arch | |
| Extended | 2 | Frontal and temporal bones and orbital roof fracture | RGF | Good | |
| 4 | Orbital fractures + frontal sinus | RGF | Good |
Abbreviation: RGF, restored good function.
Aesthetic outcome was affected by the functional deficit.
We compared the eight categories of injuries described by the extension and the depth regarding the postoperative functional and aesthetic status using “Exact test.” This showed significant association between all categories for both types of deficits. The highest frequency was found in extended complex injuries, and the least in extended simple and extended isolated bony injuries. Table 4 shows incidence of functional and aesthetic outcomes in each category according to periorbital trauma classification.
Table 4. Incidence of functional and aesthetic deficits in each category of periorbital trauma injuries.
| Injury | No. | Functional deficits | Aesthetic deficits | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | p -Value a | Yes | No | p -Value a | ||||||
| No. | Row % | No. | Row % | No. | Row % | No. | Row % | ||||
| Localized simple | 41 | 1 | 2.44 | 40 | 97.56 | 0.001 | 8 | 19.51 | 33 | 80.49 | 0.022 |
| Extended simple | 63 | 0 | 0.00 | 63 | 100.00 | 9 | 14.29 | 54 | 85.71 | ||
| Localized composite | 52 | 6 | 11.54 | 46 | 88.46 | 10 | 19.23 | 42 | 80.77 | ||
| Extended composite | 17 | 2 | 11.76 | 15 | 88.24 | 4 | 23.53 | 13 | 76.47 | ||
| Localized complex | 34 | 7 | 20.59 | 27 | 79.41 | 10 | 29.41 | 24 | 70.59 | ||
| Extended complex | 4 | 1 | 25.00 | 3 | 75.00 | 4 | 100.00 | 0 | 0.00 | ||
| Localized isolated bony | 43 | 7 | 16.28 | 36 | 83.72 | 10 | 23.26 | 33 | 76.74 | ||
| Extended isolated bony | 6 | 0 | 0.00 | 6 | 100.00 | 0 | 0.00 | 6 | 100.00 | ||
| Total | 260 | 24 | 9.23 | 236 | 90.77 | 55 | 21.15 | 205 | 78.85 | ||
Exact test was used.
Time of primary surgery was delayed in 38 patients. Causes of delayed management were delayed presentation, polytrauma, and life-threatening conditions. Most of the delayed cases had suboptimal outcomes. However, other cases had complications due to misdiagnosis and overlooked injured structures. We related the effect of time of intervention, site of injury, and depth of injury to the incidence of functional and aesthetic deficits. Table 5 shows that immediate intervention was associated with significantly fewer functional and aesthetic deficits. The site and depth of injury have significantly affected functional deficits being the highest in the periocular injuries and the complex injuries, respectively. However, there were no significant differences between different depth categories regarding the aesthetic deficits. There were also no significant differences between different anatomical subunits regarding the aesthetic deficits. In certain cases, secondary operations were required, including correction of medial canthal ligament, repair of canalicular system, scar revisions, fat graft, and creation of natural creases.
Table 5. Incidence of functional and aesthetic deficits related to the time of interference, site of injury, and depth of injury of periorbital trauma injuries.
| No. | Function deficit | p -Value | Aesthetic deficit | p -Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | |||||||||
| No. | Row no. % | No. | Row no. % | No. | Row no. % | No. | Row no. % | |||||
| Time | Immediate | 222 | 7 | 3.20% | 215 | 96.80% | <0.001 a | 32 | 14.40% | 190 | 85.60% | <0.001 a |
| Delayed | 38 | 18 | 47.40% | 20 | 52.60% | 25 | 65.80% | 13 | 34.20% | |||
| Region | Periocular | 112 | 21 | 18.75% | 91 | 81.25% | <0.001 b | 27 | 24.11% | 83 | 74.11% | 0.606 b |
| Malar | 25 | 0 | 0.00% | 25 | 100.00% | 5 | 20.00% | 20 | 80.00% | |||
| Frontal | 29 | 0 | 0.00% | 29 | 100.00% | 6 | 20.69% | 23 | 79.31% | |||
| Temple | 4 | 0 | 0.00% | 4 | 100.00% | 0 | 0.00% | 4 | 100.00% | |||
| Extended | 90 | 3 | 3.33% | 87 | 96.67% | 17 | 18.89% | 73 | 81.11% | |||
| Depth | Simple | 104 | 1 | 1.00 | 103 | 99.00 | 0.001 a | 17 | 16.30 | 87 | 83.70 | 0.069 a |
| Composite | 69 | 8 | 11.60 | 61 | 88.40 | 14 | 20.30 | 55 | 79.70 | |||
| Complex | 38 | 8 | 21.10 | 30 | 78.90 | 14 | 36.80 | 24 | 63.20 | |||
| Isolated bony | 49 | 7 | 14.30 | 42 | 85.70 | 10 | 20.40 | 39 | 79.60 | |||
| Total | 260 | 24 | 9.23% | 236 | 90.77% | 55 | 21.15% | 205 | 78.85% | |||
Notes: p -Values represent the difference between raw categories regarding the presence or absence of the functional deficits and aesthetic deficits.
Timing of intervention and type of injury in terms of depth and site all influenced the functional outcome.
The highest functional deficits were found in injuries localized to periocular region or the extended types including the periocular region.
We compared injuries described by depth as regards postoperative deficits including functional and aesthetic using “chi-squared test.” It showed significant difference between the four categories as regards the functional deficits. The category with the highest deficit frequency is complex injuries, and the least is the simple injuries. There was no significant difference between the four categories as regards the aesthetic deficits.
Chi-squared test was used.
Exact test was used.
Cases Showing Improper Management of Periorbital Injuries
Case 1
A 26-year-old male patient had a blunt trauma. Primarily, he was not diagnosed. He had a ptosis of the right upper eyelid without skin affection. The surgery explored dehiscence of the levator palpebrae superioris muscle with underlying intact conjunctiva. The edges of the proximal end was identified and advanced, then sutured and fixed to the tarsal edge. This was a case of simple localized injury of the periocular region affecting a solely intermediate structure without skin affection ( Fig. 3 ).
Fig. 3.
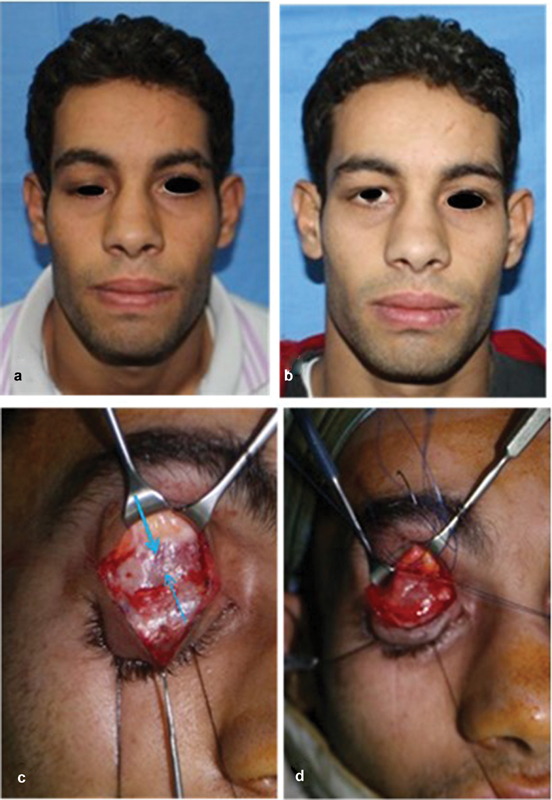
Simple localized injury of the periocular region. ( a ) Ptosis of right upper eyelid. ( b ) Postoperative correction of ptosis. ( c ) Edges of the levator dehiscence with underlying intact conjunctiva. ( d ) Edge of the proximal end identified and advanced and sutured/fixed to tarsal edge.
Case 2
A 21-year-old female patient had a blunt trauma to the left medial canthal region. No surgical repair was done. She came after 1 year with skin scarring, left canthal dystopia, and telecanthus. Only the skin has been repaired, while the medial canthal ligament has been overlooked. The patient presented 1 year later with telecanthus, canthal dystopia, and skin scarring. The ligament was re-fixed into the medial orbital wall. Undermining of soft tissue was done to facilitate skin mobilization and avoid overcorrection. This is considered as localized composite traumatic injuries. The skin and other structures of the middle layer in one subunit are affected. The injury is confined to the periocular region, so it is considered “localized.” It included more than one of soft tissues injured, the skin and medial canthal ligament; so, it is considered “composite.” The primary treatment was just skin repair ( Fig. 4 ).
Fig. 4.

Localized composite traumatic lesion of the periocular region. ( a ) One-year postinjury frontal view shows left telecanthus, canthal dystopia, and skin scarring. ( b ) Six months postoperative frontal view with opened eyes shows corrected telecanthus. ( c ) Postoperative frontal view with closed eyes shows corrected telecanthus.
Case 3
A 24-year-old female patient had extended composite traumatic injury of periocular and frontal regions. The skin and other structures of the middle layer in more than one subunit are affected. The immediate repair was sub-ideal. The patient presented 1 month later with epicanthal folds which needs secondary surgery ( Fig. 5 ).
Fig. 5.

Extended composite traumatic injury. ( a ) Both upper eyelids, levator palpebrae muscle, medial canthi, intercanthal regions, and left eye brow, frontal and left temporal areas. ( b, c ) Postoperative showing bilateral epicanthal folds which need revision.
Case 4
A 14-year-old male patient had left naso-orbito-ethmoidal fracture and zygoma with improper management. This is extended complex traumatic injury affecting all layers including bone in more than one subunit. The patient presented 4 months later with telecanthus and orbital dystopia. Surgical corrections of telecanthus and dystopia were done. Surgical outcome is less than ideal because of the delayed surgical intervention of such extended complex injury ( Fig. 6 ).
Fig. 6.
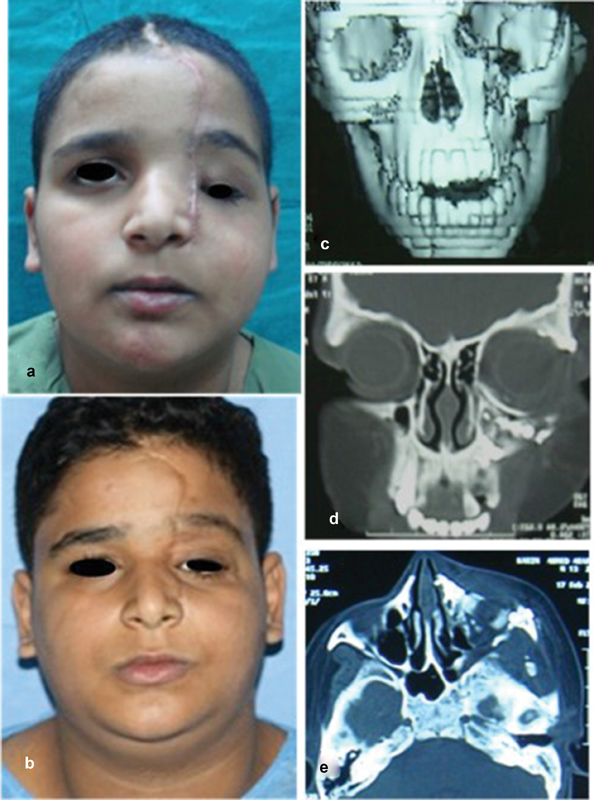
Extended complex traumatic injury affecting left naso-orbito-ethmoidal fracture and zygoma. ( a ) Postinjury frontal view with 4 months delay show telecanthus and orbital dystopia. ( b ) Postoperative frontal view after reduction and fixation. ( c, d ) Postoperative coronal and axial CTs show bone graft for the orbital floor, reconstruction of left zygoma.
Case 5
A 3-year-old child fell from a height and had fractures of right orbital roof and frontal and temporal bones. The child had a skull fracture that was unnoticed. He had growing fracture, cerebrospinal fluid leak, and expanding forehead, right orbit, eyelids, and conjunctiva. Surgical exposure revealed the growing fracture. Reduction and fixation were done. Bone grafts were used to reconstruct the orbital roof and the junction between frontal and temporal bones. Pericranial graft was used to repair the dura. Eyelids were conservatively managed ( Fig. 7 ).
Fig. 7.

Extended isolated bone traumatic injury. ( a ) Frontal view shows expanding forehead, eyelids, and conjunctiva. ( b ) 3D-CT shows fracture of frontal and temporal bones and superior orbital rim. ( c, d ) Coronal CT shows fracture of orbital roof and superior orbital rim. ( e ) Coronal approach for exposure, dural repairs, and reduction and fixation. ( f ) One-year postoperative frontal view shows normal appearance. ( g ) Postoperative PA X-ray skull shows the reduced bones and fixation.
We recommend two main steps in the assessment of periorbital trauma to enhance decision making and management plan. The first is a general approach to periorbital trauma and the second step is categorization of periorbital injuries according to anatomical and clinical classification.
-
General approach to periorbital trauma :
Primary trauma survey.
Management of life-threatening conditions.
Primary ophthalmic survey.
Assessment of concomitant injuries.
Complete history and general examination.
Thorough complete head and neck examination.
Facial CT.
Full ophthalmic assessment.
Routine investigations.
Consulting other specialties if needed.
Counseling patients and/or their relatives.
Preinjury photographs if available.
Documentation.
Categorization of periorbital injuries :
Facial examination and meticulous fully investigated workup should be done in organized manner aiming to detect all traumatic lesions without missing any of the important structures to avoid awkward complications. This would help junior surgeons to follow and avoid misdiagnosis. Table 6 shows categorization of injuries for periorbital trauma management.
Table 6. Suggested guidelines for periorbital trauma management.
| Subunit | Preoperative assessment findings | Type of injury | Anatomical repair |
|---|---|---|---|
| Periocular | Skin wounds/loss | Localized simple [one layer] | Anatomical repair Direct closure STSG/FTSG/local flap |
| Cut of levator palpebrae superioris muscle | Localized simple [one layer] |
Muscle repair | |
| Skin wounds | Localized composite [> one layer] |
Repair | |
| Cut of tarsus, levator palpebrae muscle | Identification of the injured middle layer structures and repair | ||
| Canthal tendons, lacrimal system | |||
| Partial or full-thickness loss of eyelids | Eyelids reconstruction | ||
| Globe injuries | Ophthalmic work | ||
| Identification of injured structures and fractured bones; skin wounds, cut of tarsus, levator palpebrae muscle, partial or full-thickness loss of eyelids, canthal tendons, lacrimal system, globe injuries + orbital wall(s) fracture ± affected sensory nerves | Localized complex [any soft tissue + bone] | Anatomical repair as in composite injuries Ophthalmic work Reduction and fixation ± primary bone graft Freeing of entrapped sensory nerves |
|
| Identification of the affected bones | Isolated bony | Reduction and internal fixation ± bone graft | |
| Frontal | Skin wounds/loss | Localized simple [one layer] | Anatomical repair Direct closure STSG/FTSG/local flap |
| Skin wounds/losses Sensory nerves Muscles |
Localized composite [> one layer] |
Anatomical repairs Direct closure, STSG FTSG Local flap/free flap |
|
| As composite + identification of the affected bones ± affected sensory nerves | Localized complex | Frontal sinus surgery ± primary bone graft Freeing of entrapped sensory nerves |
|
| Identification of the affected bones | Isolated bony | Reduction and internal fixation ± bone graft | |
| Temporal | Skin wounds/loss | Localized simple [one layer] |
Anatomical repair Direct closure STSG/FTSG/local flap |
| Skin wounds/loss Sensory nerves Facial nerve branches Muscles |
Localized composite [> one layer] |
Anatomical repair Direct closure STSG FTSG Local flap/free flap |
|
| Identification of the affected bones Skull base |
As composite + ± primary bone graft Later fat graft Reduction and internal fixation |
||
| Identification of the affected bones | Isolated Bony | Reduction and internal fixation ± bone graft | |
| Malar | Skin wounds/loss | Localized simple [one layer] |
Anatomical repair Direct closure STSG/FTSG/local flap |
| Skin wounds/losses Sensory nerves Muscles |
Localized composite [> one layer] |
Anatomical repairs Direct closure, STSG FTSG Local flap/free flap |
|
| Identification of the affected bones | As composite + reduction and internal fixation Closed reduction in isolated zygomatic arch ± bone graft Later fat graft |
||
| Identification of the affected bones | Isolated bony | Reduction and internal fixation ± bone graft | |
| More than one subunit | One layer covering more than one zone | Simple extended | Anatomical repair/reconstruction |
| Two or more layers of soft tissue covering more than one zone | Extended composite | Anatomical repair/reconstruction Ophthalmic work May need staged repairs Reconstruction Preserving creating subunits and distinguishing lines |
|
| Soft-tissue injuries including bone affection covering more than one zone | Extended complex | Anatomical repair/reconstruction + reduction and fixation May need staged repairs Reconstruction Preserving creating subunits and distinguishing lines |
Abbreviations: FTSG, full-thickness skin graft; STSG, split-thickness skin graft.
Discussion
The periorbital region is both precious and complex. Types of periorbital injuries are described in this study according to anatomical and clinical categorization. We preferred to merge the clinical classification with the anatomic classification. The clinical classification describes the injury as simple, composite, and complex and each one can be subdivided into localized and extended. The categorized injuries can be well analyzed and wisely repaired.
This study draws out the value of use of the classification in stimulating the 3D search for possible injuries through the depth of the injured region and beyond in the periorbital region trauma. All affected tissues and depth of injury should be determined with thorough examination from superficial to deep and good imaging. Simon et al 34 and Ono et al 36 emphasized that a low clinical suspicion for fracture does not rule out significant soft-tissue injury. We added that unaffected skin may not exclude affection of the underlying structures, as levator palpebrae superioris can be cut without skin laceration. Also isolated bone fractures could happen without skin wounds. Outcome deficits are more noticeable with the complex and extended lesions.
In this study, the “extended complex injuries” had the highest frequency of functional and aesthetic deficits, while the “extended simple” and “extended isolated bony injuries” had the least. The “complex injuries” had the highest frequency of functional deficits, while the “simple injuries” had the least. Important structures are involved mainly in composite and complex injuries. This is why a special survey is mandatory to assess the ocular structures, facial nerve, sensory nerves, medial canthal ligament, lacrimal system, and levator palpebrae muscle.
The extended bony injuries are expected to have functional deficits. However, in this study, the mode of trauma to some patients was blunt and the fractures were nondisplaced affecting just the outer table of the bones. Such patients were treated conservatively, while in patients who needed surgery, the surgical outcomes were accepted.
The aesthetic outcome could be affected by the functional deficit as in telecanthus. So, it is important to merge the aesthetic and reconstructive principles in the management of facial trauma patient. The restoration of a region aesthetics guided by sound anatomical repair usually restores the normal functions.
The present classification of periorbital trauma highlights the importance of the subunit concept formed of special tissues and topography with different aesthetics. The subunits of periorbital region should be repaired using reconstructive and aesthetic principles to achieve good functional and aesthetic outcomes. The special 3D topography and features of any subunit should be preserved and/or created. Issues of repair in extended injuries may become problematic when trauma encompasses more than one subunit. Restoration of contour of each subunit should be considered separately. “Fill in hole” concept is not accepted by most plastic surgeons, as it may lead to poor contour, incorrect dimension, malposition, asymmetry, and poor blending into adjacent normal tissues, and a patch-like repair often follows. 40 The incisions can be hidden within the contour lines and aesthetic unit boundaries. Kretlow et al preferred to plan for the reconstruction of each unit separately, so that incisions and the used local tissue are within or along the border of the unit being reconstructed. 41
The choice of conservative management or delayed intervention in cases requiring immediate repair is considered unwise decision. Immediate primary repair of periorbital trauma should be done with the highest possible standards. The delayed improper management may need a multistage surgical plan with resultant unaccepted outcomes. 24 41 42 This can be well seen in cases of improper management of naso-orbito-ethmoid fractures with serious secondary deformities. 43 44 45 46 47 This may make all secondary reparative trials quite difficult to restore aesthetic results and normal functions as lacrimal patency. Thus, the complexity of the injury and the time of intervention can be considered major factors in surgical outcome. Mokal and Desai added the time elapsed till secondary reconstruction. 33
Thus, surgeons should consider all factors (preinjury condition, type of injury, depth and extension of injury, time of intervention, technique limitations, postoperative healing, and comorbidities) that may hinder achieving good functional and aesthetic outcomes. They must have comprehensive understanding of structural and aesthetic details of periorbital region to be able to accurately restore structure and function as much as possible. We recommend the use of the structured for proper diagnoses and careful surgical plan and prompt intervention without delays. The study might have a limitation that surgeries were done by different surgeons. We recommend further studies to validate its significance in the proper management of periorbital trauma.
Conclusion
This study demonstrated that unsatisfactory aesthetic and functional results occurred when injuries of important structures were overlooked, aesthetics units were disrespected, and when management was delayed. The new classification of the periorbital trauma based on anatomical and clinical categorization is proposed to stimulate three-dimensional search for possible injuries. This structured preoperative evaluation would guide wise surgical plan to ultimately achieve precise primary repair. The aesthetic and reconstructive principles should be merged in the management of periorbital trauma. A protocol for traumatic periorbital injuries formed of preoperative assessment, anatomical repair, and postoperative functional and aesthetic assessment is very much recommended.
Footnotes
Disclosure The authors have no conflict of interest.
References
- 1.Yüce S, Demir Z, Selçuk C T, Celebioğlu S. Reconstruction of periorbital region defects: a retrospective study. Ann Maxillofac Surg. 2014;4(01):45–50. doi: 10.4103/2231-0746.133077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berli J U, Merbs S L, Grant M P. Reconstruction of periorbital soft tissue defects. Facial Plast Surg. 2014;30(05):561–569. doi: 10.1055/s-0034-1395264. [DOI] [PubMed] [Google Scholar]
- 3.Mathes D W, Edwards J A, Anzai Y, Neligan P C. A functional periorbital subunit allograft: vascular, anatomic, and technical considerations for future subunit facial transplantation. J Plast Reconstr Aesthet Surg. 2014;67(10):1371–1377. doi: 10.1016/j.bjps.2014.05.046. [DOI] [PubMed] [Google Scholar]
- 4.Sosin M, Mundinger G S, Dorafshar A H et al. Optimizing reconstruction with periorbital transplantation: clinical indications and anatomic considerations. Plast Reconstr Surg Glob Open. 2016;4(02):e628. doi: 10.1097/GOX.0000000000000545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Özkaya Mutlu Ö, Egemen O, Dilber A, Üsçetin I. Aesthetic unit-based reconstruction of periorbital defects. J Craniofac Surg. 2016;27(02):429–432. doi: 10.1097/SCS.0000000000002359. [DOI] [PubMed] [Google Scholar]
- 6.Spinelli H M, Jelks G W.Periocular reconstruction: a systematic approach Plast Reconstr Surg 199391061017–1024., discussion 1025–1026 [PubMed] [Google Scholar]
- 7.Bowman P H, Fosko S W, Hartstein M E. Periocular reconstruction. Semin Cutan Med Surg. 2003;22(04):263–272. doi: 10.1016/S1085-5629(03)00076-2. [DOI] [PubMed] [Google Scholar]
- 8.Cannon P S, McCormick A, Leatherbarrow B. The use of soft tissue expanders in periocular reconstruction: a case series. Ophthal Plast Reconstr Surg. 2011;27(04):232–235. doi: 10.1097/IOP.0b013e318202e7e5. [DOI] [PubMed] [Google Scholar]
- 9.Imola M J, Ducic Y, Adelson R T. The secondary correction of post-traumatic craniofacial deformities. Otolaryngol Head Neck Surg. 2008;139(05):654–660. doi: 10.1016/j.otohns.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 10.Gruss J S, Whelan M F, Rand R P, Ellenbogen R G. Lessons learnt from the management of 1500 complex facial fractures. Ann Acad Med Singapore. 1999;28(05):677–686. [PubMed] [Google Scholar]
- 11.Cooter R D, David D J. Computer-based coding of fractures in the craniofacial region. Br J Plast Surg. 1989;42(01):17–26. doi: 10.1016/s0007-1226(89)90107-0. [DOI] [PubMed] [Google Scholar]
- 12.Osler T, Baker S P, Long W.A modification of the injury severity score that both improves accuracy and simplifies scoring J Trauma 19974306922–925., discussion 925–926 [DOI] [PubMed] [Google Scholar]
- 13.Bagheri S C, Dierks E J, Kademani D et al. Application of a facial injury severity scale in craniomaxillofacial trauma. J Oral Maxillofac Surg. 2006;64(03):408–414. doi: 10.1016/j.joms.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 14.Zhang J, Zhang Y, El-Maaytah M, Ma L, Liu L, Zhou L D. Maxillofacial Injury Severity Score: proposal of a new scoring system. Int J Oral Maxillofac Surg. 2006;35(02):109–114. doi: 10.1016/j.ijom.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad Z, Nouraei R, Holmes S. Towards a classification system for complex craniofacial fractures. Br J Oral Maxillofac Surg. 2012;50(06):490–494. doi: 10.1016/j.bjoms.2011.09.018. [DOI] [PubMed] [Google Scholar]
- 16.Sahni V. Maxillofacial trauma scoring systems: review article. Injury. 2016;47(07):1388–1392. doi: 10.1016/j.injury.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Cohen M A, Boyes-Varley G. Penetrating injuries to the maxillofacial region. J Oral Maxillofac Surg. 1986;44(03):197–202. doi: 10.1016/0278-2391(86)90108-4. [DOI] [PubMed] [Google Scholar]
- 18.Harris A MP, Wood R E, Nortjé C J, Grotepass F. Deliberately inflicted, penetrating injuries of the maxillofacial region (Jael's syndrome). Report of 4 cases. J Craniomaxillofac Surg. 1988;16(02):60–63. doi: 10.1016/s1010-5182(88)80019-2. [DOI] [PubMed] [Google Scholar]
- 19.Grobbelaar A, Knottenbelt J D. Retained knife blades in stab wounds of the face: is simple withdrawal safe? Injury. 1991;22(01):29–31. doi: 10.1016/0020-1383(91)90156-9. [DOI] [PubMed] [Google Scholar]
- 20.Thorne C H. Gunshot wounds to the face. Current concepts. Clin Plast Surg. 1992;19(01):233–244. [PubMed] [Google Scholar]
- 21.Chen A Y, Stewart M G, Raup G. Penetrating injuries of the face. Otolaryngol Head Neck Surg. 1996;115(05):464–470. doi: 10.1177/019459989611500519. [DOI] [PubMed] [Google Scholar]
- 22.Demetriades D, Chahwan S, Gomez H, Falabella A, Velmahos G, Yamashita D. Initial evaluation and management of gunshot wounds to the face. J Trauma. 1998;45(01):39–41. doi: 10.1097/00005373-199807000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Hollier L, Grantcharova E P, Kattash M. Facial gunshot wounds: a 4-year experience. J Oral Maxillofac Surg. 2001;59(03):277–282. doi: 10.1053/joms.2001.20989. [DOI] [PubMed] [Google Scholar]
- 24.Motamedi M H. Primary management of maxillofacial hard and soft tissue gunshot and shrapnel injuries. J Oral Maxillofac Surg. 2003;61(12):1390–1398. doi: 10.1016/j.joms.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 25.Daya N P, Liversage H L. Penetrating stab wound injuries to the face. SADJ. 2004;59(02):55–59. [PubMed] [Google Scholar]
- 26.McLean J N, Moore C E, Yellin S A. Gunshot wounds to the face--acute management. Facial Plast Surg. 2005;21(03):191–198. doi: 10.1055/s-2005-922859. [DOI] [PubMed] [Google Scholar]
- 27.Agrillo A, Sassano P, Mustazza M C, Filiaci F. Complex-type penetrating injuries of craniomaxillofacial region. J Craniofac Surg. 2006;17(03):442–446. doi: 10.1097/00001665-200605000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Kesting M R, Hölzle F, Pox C, Thurmüller P, Wolff K D. Animal bite injuries to the head: 132 cases. Br J Oral Maxillofac Surg. 2006;44(03):235–239. doi: 10.1016/j.bjoms.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 29.Kaufman Y, Cole P, Hollier L. Contemporary issues in facial gunshot wound management. J Craniofac Surg. 2008;19(02):421–427. doi: 10.1097/SCS.0b013e31816ae4a8. [DOI] [PubMed] [Google Scholar]
- 30.Stefanopoulos P K.Management of facial bite wounds Oral Maxillofac Surg Clin North Am 20092102247–257., vii [DOI] [PubMed] [Google Scholar]
- 31.Meer M, Siddiqi A, Morkel J A, Janse van Rensburg P, Zafar S. Knife inflicted penetrating injuries of the maxillofacial region: a descriptive, record-based study. Injury. 2010;41(01):77–81. doi: 10.1016/j.injury.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 32.Yardley A M, Hoskin A K, Hanman K, Wan S L, Mackey D A. Animal-inflicted ocular and adnexal injuries in children: a systematic review. Surv Ophthalmol. 2015;60(06):536–546. doi: 10.1016/j.survophthal.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 33.Mokal N J, Desai M F. Secondary correction of post-traumatic craniofacial deformities. J Craniofac Surg. 2014;25(05):1658–1664. doi: 10.1097/SCS.0000000000001138. [DOI] [PubMed] [Google Scholar]
- 34.Simon B, Letourneau P, Vitorino E, McCall J.Pediatric minor head trauma: indications for computed tomographic scanning revisited J Trauma 20015102231–237., discussion 237–238 [DOI] [PubMed] [Google Scholar]
- 35.Katzen J T, Jarrahy R, Eby J B, Mathiasen R A, Margulies D R, Shahinian H K. Craniofacial and skull base trauma. J Trauma. 2003;54(05):1026–1034. doi: 10.1097/01.TA.0000066180.14666.8B. [DOI] [PubMed] [Google Scholar]
- 36.Ono K, Wada K, Takahara T, Shirotani T.Indications for computed tomography in patients with mild head injury Neurol Med Chir (Tokyo) 20074707291–297., discussion 297–298 [DOI] [PubMed] [Google Scholar]
- 37.Denny A D, Bonawitz S C. Clostridial infection following severe facial trauma. Ann Plast Surg. 1994;33(03):313–316. doi: 10.1097/00000637-199409000-00013. [DOI] [PubMed] [Google Scholar]
- 38.Jayamanne D G, Bell R W, Allen E D. Orbital cellulitis--an unusual presentation and late complication of severe facial trauma. Br J Oral Maxillofac Surg. 1994;32(03):187–189. doi: 10.1016/0266-4356(94)90108-2. [DOI] [PubMed] [Google Scholar]
- 39.Thomas J R, Frost T W. Immediate versus delayed repair of skin defects following resection of carcinoma. Otolaryngol Clin North Am. 1993;26(02):203–213. [PubMed] [Google Scholar]
- 40.Menick F J. Defects of the nose, lip, and cheek: rebuilding the composite defect. Plast Reconstr Surg. 2007;120(04):887–898. doi: 10.1097/01.prs.0000277662.51022.1d. [DOI] [PubMed] [Google Scholar]
- 41.Kretlow J D, McKnight A J, Izaddoost S A. Facial soft tissue trauma. Semin Plast Surg. 2010;24(04):348–356. doi: 10.1055/s-0030-1269764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Berthe J V, Pelc P, Jortay A, Coessens B C. Do multiple consecutive head and neck reconstructions improve the patients functional outcome? Acta Otorhinolaryngol Belg. 2002;56(04):391–397. [PubMed] [Google Scholar]
- 43.Elbarbary A S, Ali A. Medial canthopexy of old unrepaired naso-orbito-ethmoidal (noe) traumatic telecanthus. J Craniomaxillofac Surg. 2014;42(02):106–112. doi: 10.1016/j.jcms.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 44.Becelli R, Renzi G, Mannino G, Cerulli G, Iannetti G. Posttraumatic obstruction of lacrimal pathways: a retrospective analysis of 58 consecutive naso-orbitoethmoid fractures. J Craniofac Surg. 2004;15(01):29–33. doi: 10.1097/00001665-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 45.Kelly C P, Cohen A J, Yavuzer R, Moreira-Gonzalez A, Jackson I T. Medial canthopexy: a proven technique. Ophthal Plast Reconstr Surg. 2004;20(05):337–341. doi: 10.1097/01.iop.0000139519.40976.28. [DOI] [PubMed] [Google Scholar]
- 46.Reifler D M. Management of canalicular laceration. Surv Ophthalmol. 1991;36(02):113–132. doi: 10.1016/0039-6257(91)90125-y. [DOI] [PubMed] [Google Scholar]
- 47.Evans G R, Daniels M, Hewell L. An evidence-based approach to zygomatic fractures. Plast Reconstr Surg. 2011;127(02):891–897. doi: 10.1097/PRS.0b013e31820456e5. [DOI] [PubMed] [Google Scholar]


