Abstract
Dog bite–related wounds seem to have become a common problem, especially when they relate to the head and neck region. According to Overall and Love, up to 18 per 1,000 people sustain a dog bite every year, of whom 3 need medical attention. Approximately 1 to 2% of bite injuries require hospitalization of the victims. Most of the lacerations are found in the upper lip and the nose regions and they are classified according to severity and concomitant damage to other organs. Bite wounds are considered “dirty” wounds and are prone to infection. When dealing with bite wounds, there is always an indication for antibiotic treatment. Broad-spectrum antibiotics like amoxicillin-clavulanate and/or moxifloxacin cover most of the pathogenic flora and should be administered in every bite wound case at risk of infection. This article would like to present a medical record review: a retrospective analysis of all bite wounds sustained in the head and neck region, treated at the University Hospital of Leuven over the past 20 years. Furthermore, it provides an overview of the current literature and its standings on the treatment of dog bite injuries in the maxillofacial region. We assessed both surgical and medical treatment options, as well as primary management, which includes infection prevention strategies, closure management, and additional vaccination requirements. Secondary management or scar revision methods will be mentioned. After conducting a UZ Leuven database search using keywords such as “dog,” “dog bite,” “face,” “head,” “lip,” and others, 223 patients were included. Age at the time of injury, location of the injury, treatment method used, and whether secondary infection was present or not were documented. All patients have been divided in age groups. We concluded that 21.52% was 5 years old or younger. Almost half of our patients (49.33%) were 18 years old or younger. Of all patients, 79 were hospitalized (35.43%). Primary closure was the treatment of choice. In 141 patients, the wounds were closed primarily (63.23%), resulting in only 2.24% reported secondary infections. Only one fatality was reported in our center over the course of 20 years (0.45%), a 6-year-old girl who had been attacked by her father's Rottweilers. Most patients who sustained dog bite injuries in the head and neck region seem to be children, specifically toddlers. Due to their height, it is possible they are more prone to dog bite injuries in the head and neck region. It is essential to optimize management of these injuries due to the impact they have on patients. This article provides the epidemiological data and clinical outcome of the approach at our center.
Keywords: dog bite injuries, trauma, head and neck
In 2014, there were approximately 1.5 million dogs registered in Belgium. In 22.70% of all Belgian households, at least one dog was registered. 1 2 Bite injuries are a common problem mostly caused by dogs. About 80 to 90% of all bite injuries are due to dog attacks. 3 Children are the most frequent victims.
Apart from the infection risk, dog bites can be challenging from a surgical point of view. The wounds tend to appear in certain patterns, usually involving puncture wounds, lacerations, tissue defects, crushed devitalized tissue, and sometimes nerve injury. Treatment options vary from primary closure to the usage of transposition flaps or free flaps. The most common complication following a bite wound is wound infection. These infections tend to be polymicrobial and include both aerobic and anaerobic bacteria mainly of oropharyngeal origin. One deserves special attention: Capnocytophaga canimorsus , 3 an aggressive organism which causes septicemia, renal failure, necrosis of extremities, and ultimately death. Other (viral) diseases are transmissible as well, of which the most fearsome is rabies.
In this article, we review the current literature and compare it to our results and outcome over the past 20 years.
Materials and Methods
After approval of the ethics committee, a retrospective medical record review was conducted. All reported dog bite injuries in the head and neck region treated at the University Hospital of Leuven from 1997 until March of 2017 were analyzed retrospectively. In total, 222 patients had been treated, with a median age of 19 years. One patient died before any treatment could be performed.
A database search between January 1997 and March 2017 of all patient records was performed, using the following setup: We searched using these keywords: “dog,” “dog bite,” “bite,” “dogbite,” “dogs.” The reports that contained at least one of the following words were included: “face,” “head,” “nose,” “lip,” “cheek,” “neck,” “chin,” “jaw,” “eyelid.” We conducted a literature search using the following keywords: “dog bite,” “face,” “head,” and “bite wound” in the following databases: Medline database, Cochrane, and EMBASE database. The separate forensic databases of the UZ Leuven were checked for any fatalities following a dog bite injury; only one case was reported since 1997.
Inclusion criteria : All patients with dog bite wounds sustained in the head and neck region were included. Wounds in other regions like hands or legs were excluded. Bites by humans or other animals were excluded. The wound had to be fresh (<36 hours old) and untreated. Our exclusion criteria involved all patients who consulted for scar revision (unless the primary injury was treated at our hospital) or consulted for a second opinion after already having received treatment.
Of all patients included, we defined the age at the time of the injury and location of the injury. We divided the locations of the lesions into 12 regions: upper lip, lower lip, nose, cheek, chin, periorbital (eyelids included), infraorbital, forehead, scalp, neck, ear, and occipital region. We recorded whether or not the patient was hospitalized. We categorized the type of treatment and divided it into the following categories: cleansing and irrigation, approximation (using either sutures or adhesive bandage strips), primary closure, primary closure with transposition/rotation flaps, secondary closure. We recorded if the patient received antibiotic treatment, and noted the type of antibiotic therapy. All reported secondary infections were recorded as well. Secondary infection was recorded whenever a patient presented with clear symptoms (such as purulent discharge, persistent or increased swelling) or when the treating physician indicated the infection in his or her report. Information about ownership or breed of the dog was mentioned only in a few cases; therefore, this was not recorded.
Surgical procedures : All wounds were treated by medical doctors working within the University Hospitals of Leuven. Treatments varied; they included but were not limited to cleansing and irrigation, approximation, primary closure using sutures, transposition flaps, rotation flaps, and secondary closure.
Results
After performing a first database search, over 3,000 records were found. Next, all patients who consulted for an open bite or temporomandibular joint (TMJ) complaints and patients in orthodontic or orthognathic follow-up were excluded. We conducted a second search by only including the reports that contained the word “dog.” This led to 757 results. After manually selecting records, following the inclusion criteria defined earlier, a final study population of 223 patients had been reached ( Fig. 1 ).
Fig. 1.
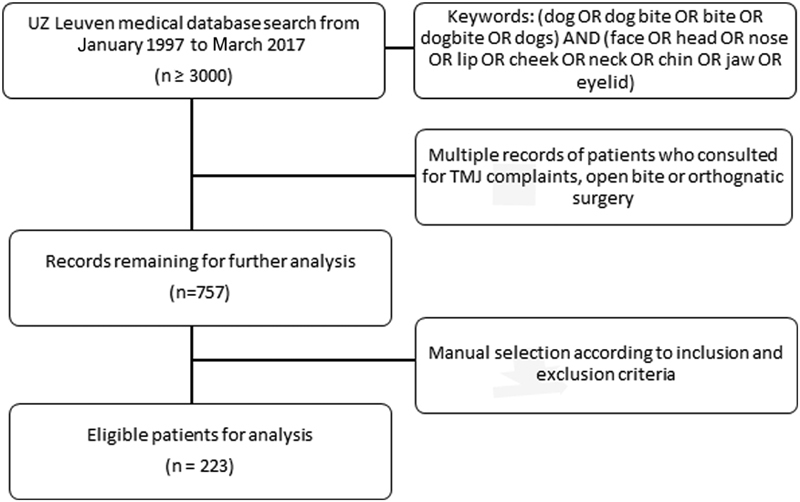
Progress of patients inclusion in the study. TMJ, temporomandibular joint.
Age Distribution
Of the 223 patients included, 48 (21.52%) were 5 years old or younger. The mean age was 19 years, average age was 24.68 years. Thirty-two patients (14.35%) were 6 to 10 years old; 23 (10.31%) were 11 to 16 years old. In total, 110 patients (49.33%) were 18 years old or younger. The remainder (113 or 50.67%) of patients were 19 years old or older.
Location of Lesions
The location of the lesions was subdivided into different regions ( Fig. 2 ). We noted that most patients had lesions sustained in the upper lip (32.748%) and cheek (27.35%) region. The nose (20.632%) and lower lip (14.80%) were frequently affected as well. Injuries in the periorbital or eye region were sustained in 12.11% of patients. The infraorbital region was affected in 6.73% of patients, and the frontal region and the chin were affected in 4.93% of patients. Least affected were the scalp and temporal regions; this was reported in only three (1.35%) and 4 (1.79%) cases, respectively.
Fig. 2.
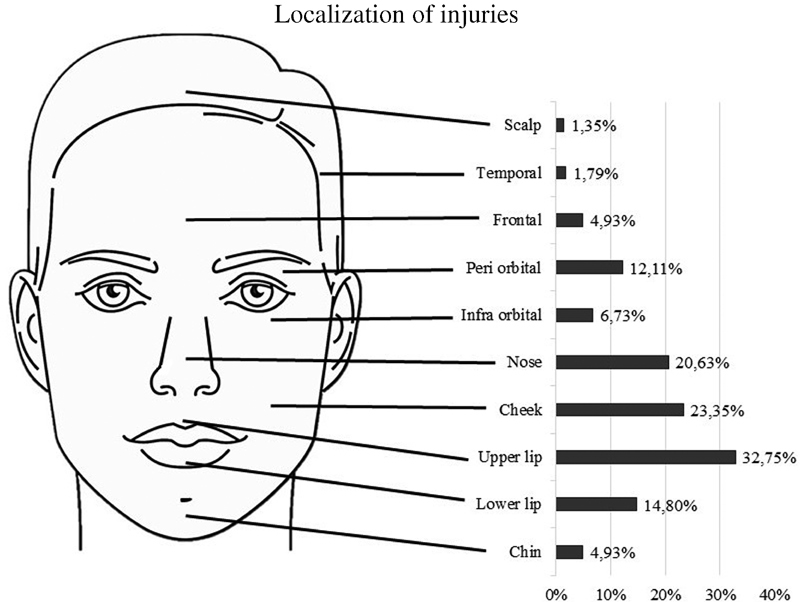
Localization of injuries.
Hospitalization and Treatment
Of all patients included, 79 were hospitalized (35.43%). All other patients (64.13%) were treated in an outpatient setting or not treated in the case of deceased patient. Some patients consulted again after a couple of days for wound evaluation in our center; however, most patients were referred to their general practitioner for follow-up. Only one fatality was reported due to a dog attack: all help came too late for this patient, and no treatment was performed. We divided the treatment of the injuries sustained in different categories ( Table 1 ). In 141 cases (63.23%), primary closure was performed, being the treatment of choice at our center. Cleansing and irrigation was performed in all cases. Forty-three (19.28%) patients were treated with just cleansing and irrigation of the wounds due to their superficial and uncomplicated nature. In 26 cases (11.66%), the wound was only approximated, using either sutures or adhesive bandage strips. A transposition flap or reconstructive surgery was necessary in only 15 cases (6.73%). Six cases needed a skin graft (2.69%). In 10 cases (4.48%), secondary closure was indicated. The usage of a drain was reported in only seven cases (3.14%). Secondary infection of the wounds was reported in five cases (2.24%). No cases of rabies or suspected rabies were recorded.
Table 1. Surgical treatment methods used.
| Method of treatment | Number of cases | Percentage |
|---|---|---|
| Approximation | 26 | 11.66% |
| Primary closure | 141 | 63.23% |
| Use of drains | 7 | 3.14% |
| Secondary closure (granulation of tissue) | 10 | 4.48% |
| Transposition flap/reconstruction required | 15 | 6.76% |
| Skin graft required | 6 | 2.69% |
Antibiotics were prescribed in almost all cases. Of 223 patients, 213 patients (95.52%) received antibiotics. Only nine patients did not receive antibiotics. Amoxicillin-clavulanate was used in 190 of 213 cases (89.20%). Other antibiotics used were clindamycin (2.82%), doxycycline (0.47%), cefadroxil (0.47%), and flucloxacillin (0.47%). In 10 cases, the type of antibiotic used was not specified.
Only 1 out of 223 patients died due to dog bite injuries (0.45%).
Discussion
Age Distribution
We defined age groups of 5-year intervals ( Fig. 3 ). Children were most frequently affected. More than a fifth of all patients were 5 years old or younger (21.52%). Children seem to be more prone to dog bite injuries in the head and neck region, possibly due to their height. They are probably more likely to provoke an attack, unknowingly, as they are not familiar with the signs indicating an impeding attack. 4 5 Our findings are in line with findings of the literature. 4 6 7 8
Fig. 3.
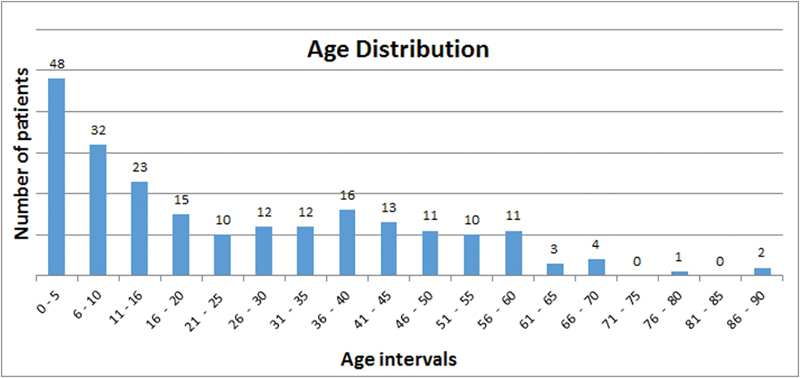
Age distribution.
Location and Presentation
We found that most lesions occur in the upper lip region and the cheeks; this is in line with findings in the literature. 6 9 10 11 The natural playful behavior of children could be a causative factor in facial injuries of lips and cheeks. The presentation of dog bites follows a certain pattern. Lacerations and puncture wounds are common. Lacerations can fairly easily be treated using primary closure techniques. Puncture wounds pose an added risk of secondary infection. Closure of these types of wounds is usually easy; however, this should never be performed carelessly. Cleansing and adequate irrigation is pervious for infection control, as is antibiotic treatment. Tissue defects and nerve injury are possible as well and should be documented. Often, crushed devitalized tissue is present due to the bite force of the animal. This can serve as a nidus for infection, as blood supply is insufficient in necrotic tissue to get rid of present pathogens. Therefore, adequate debridement is required. 12
Assessment and Treatment Options
All dog bite injuries should be assessed according to the primary and advanced trauma care. Stabilization of the patient in the emergency room should be performed whenever necessary. 13 Primary closure is the treatment of choice at our institution, as we found that this provided the best aesthetical results even in case of severe or multiform lacerations ( Figs. 4 5 6 7 ).
Fig. 4.

Extensive injuries with multiform lacerations.
Fig. 5.

The boy in Fig. 4 after primary closure.
Fig. 6.

The boy in Fig. 4 , five months later.
Fig. 7.

The boy in Fig. 4 , 18 months later.
Approximation of wounds was chosen as a treatment method whenever wounds appeared to be at risk for infection. Whenever the wound was deeper than the width, approximation using either sutures or adhesive bandage strips was performed to allow drainage of pus if necessary. Most wounds tended to be simple lacerations without severe tissue defects. In case of large tissue defects, either transposition or rotation flaps were used. Rarely, secondary closure was used—only in cases in which primary closure was either insufficient due to wound traction or when it provided an unpleasing aesthetical result. This is the most popular treatment method mentioned in the literature. 8 9 11 14
The successful management practices of dog bite wounds are meticulous cleansing of the wound, adequate debridement, primary repair, appropriate antibiotic therapy, and rabies immunization where indicated. 4 15 This is the method of treatment used at our center.
Mortality
Only one fatality was reported at our center (0.45%). The case involved a 6-year-old girl who got attacked by the two Rottweilers of her father in their backyard. Unfortunately, all help came too late, as the patient was already dead when the emergency medical teams arrived. 16
Infection
The low number of secondary infections (2.24%) is perhaps due to the fact that many patients were treated in an outpatient setting and follow-up was provided by the general practitioner in many cases. If there was any evidence for secondary infection in these cases, it might not have been reported or recorded in our hospital. On the other hand, Javaid et al reported about the same percentage of infections in 1998 after dog bite injury. 9 Foster and Hudson also reported no infections at all in their 2014 article. 4
Another possible complication of dog bite injuries is the infectious disease rabies. Rabies is usually sustained following a transdermal bite or scratch by an infected animal. It is among the most fearsome of complications, as it is almost always fatal once symptoms of central nervous system involvement develop. A progressive fatal encephalomyelitis causes hyperactivity, fluctuating consciousness, and hydrophobia or aerophobia. Postexposure prophylaxis following exposure with a high risk of transmission should always be administered. Low-risk exposure consists of touching or feeding animals and licks on intact skin. After exposure, whenever skin penetrating wounds in the exposed region are present, immediate vaccination is required. 14 17 In most industrialized countries, however, rabies is almost eradicated due to wildlife control and domestic animal vaccination programs. Western Europe was declared free of rabies in 2015, in nonflying mammals. 18 The risk of developing rabies after sustaining a dog bite injury is therefore rather low. In Western Europe, rabies postexposure prophylaxis is rarely administered after a dog bite injury. A 10-day observation period of the dog in question is recommended. 19 If the dog is not showing symptoms of rabies infection within this time window, it is not carrying the disease. If, in the rare cases, it does show symptoms of rabies, euthanasia of the animal and laboratory studies should be performed. 20
Conclusion
Dog bite injuries to the head and neck region are frequently encountered and can be life threatening. Children are most frequently affected and in many cases they leave aesthetically unpleasing scars or cause severe disfigurement. This potentially has an enormous social impact on the child; therefore, it is essential to optimize management of these injuries. The infectious risk is rather low when treated properly—for example, administration of broad-spectrum antibiotics in association with adequate debridement, cleansing, and irrigation. Primary closure of the wound remains the best treatment option today. The dangers of allowing domestic animals and small children to play together are often underestimated. Trauma care protocols for dog bite injuries should be present in every emergency room department and can provide better outcomes.
Data
Data are presented using frequencies and percentages. Some data might have been lost as a lot of investigations conducted before the year 2000 were not recorded digitally. Therefore, some may not have been recorded in the current digital database of the University Hospitals of Leuven.
Acknowledgments
All authors contributed to the design and conduct of the study; data collection and management; analysis and interpretation of the data; and preparation, review, or approval of the manuscript. We would like to thank Professor Vranckx, Professor Verelst, and Professor Nys for approval of this study.
Funding Statement
Funding None.
Conflict of Interest The authors report no conflict of interest in this work. This article has not been presented nor published elsewhere, and no financial support has been obtained in its preparation.
Informed Consent
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for design or implementation of the study. All clinical images of patients were anonymized.
Compliance with Ethical Statements
The protocol was approved by the Ethics Committee of our institution (University Hospitals of Leuven; file number S60452) and was conducted according to the principles expressed in the Declaration of Helsinki. 21
References
- 1.Overall K L, Love M. Dog bites to humans--demography, epidemiology, injury, and risk. J Am Vet Med Assoc. 2001;218(12):1923–1934. doi: 10.2460/javma.2001.218.1923. [DOI] [PubMed] [Google Scholar]
- 2.Statbel.Belgische gezinnen spenderen 1,3 miljard euro aan huisdieren in 2014Statistics Belgium. Available at:http://statbel.fgov.be/nl/statistieken/organisatie/statbel/informatie/statbel/in_de_kijker_archief/In_de_kijker_2016/20160825_honden_en_katten_in_2014.jsp. Published 2016. Accessed April 29, 2017
- 3.Szczypa K, Hryniewicz W. Epidemiology, microbiology and diagnostics of dog and cat bites related infections [in Polish] Pol Merkuriusz Lek. 2015;39(232):199–204. [PubMed] [Google Scholar]
- 4.Foster M D, Hudson J W. Contemporary update on the treatment of dog bite: injuries to the oral and maxillofacial region. J Oral Maxillofac Surg. 2015;73(05):935–942. doi: 10.1016/j.joms.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Mannion C JJ, Graham A, Shepherd K, Greenberg D. Dog bites and maxillofacial surgery: what can we do? Br J Oral Maxillofac Surg. 2015;53(06):522–525. doi: 10.1016/j.bjoms.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 6.Schultz R C, McMaster W C. The treatment of dog bite injuries, especially those of the face. Plast Reconstr Surg. 1972;49(05):494–500. doi: 10.1097/00006534-197205000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Chen H H, Neumeier A T, Davies B W, Durairaj V D. Analysis of pediatric facial dog bites. Craniomaxillofac Trauma Reconstr. 2013;6(04):225–232. doi: 10.1055/s-0033-1349211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palmer J, Rees M. Dog bites of the face: a 15 year review. Br J Plast Surg. 1983;36(03):315–318. doi: 10.1016/s0007-1226(83)90051-6. [DOI] [PubMed] [Google Scholar]
- 9.Javaid M, Feldberg L, Gipson M. Primary repair of dog bites to the face: 40 cases. J R Soc Med. 1998;91(08):414–416. doi: 10.1177/014107689809100804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kizer K W. Epidemiologic and clinical aspects of animal bite injuries. JACEP. 1979;8(04):134–141. doi: 10.1016/s0361-1124(79)80339-1. [DOI] [PubMed] [Google Scholar]
- 11.Lackmann G M, Draf W, Isselstein G, Töllner U. Surgical treatment of facial dog bite injuries in children. J Craniomaxillofac Surg. 1992;20(02):81–86. doi: 10.1016/s1010-5182(05)80472-x. [DOI] [PubMed] [Google Scholar]
- 12.Andersson L, Kahnberg K-E, Pogrel M A. Hoboken, NJ: Wiley-Blackwell; 2012. Oral and Maxillofacial Surgery. [Google Scholar]
- 13.Gwinnutt C L, Driscoll P A. Advanced trauma life support. Eur J Anaesthesiol. 1996;13(02):95–101. doi: 10.1046/j.1365-2346.1996.00939.x. [DOI] [PubMed] [Google Scholar]
- 14.Reyes V RV, Ávila M GF, Balandrano A GP. Treatment of craniofacial region wounds. Rev Odontol Mex. 2013;17(04):243–250. [Google Scholar]
- 15.Lin W, Patil P M. Facial dog attack injuries. Indian J Surg. 2015;77(01):55–58. doi: 10.1007/s12262-013-0964-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Munnynck K, Van de Voorde W. Forensic approach of fatal dog attacks: a case report and literature review. Int J Legal Med. 2002;116(05):295–300. doi: 10.1007/s00414-002-0332-9. [DOI] [PubMed] [Google Scholar]
- 17.Looke D DC.Bites (mammalian). Systematic review 914. BMJ Clin Evid 2015Available at:http://clinicalevidence.bmj.com/x/systematic-review/0914/overview.html. Accessed May 10, 2018
- 18.Ribadeau-Dumas F, Cliquet F, Gautret P, Robardet E, Le Pen C, Bourhy H. Travel-associated rabies in pets and residual rabies risk, Western Europe. Emerg Infect Dis. 2016;22(07):1268–1271. doi: 10.3201/eid2207.151733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization.WHO expert consultation on rabies. Second report World Health Organ Tech Rep Ser 20139829821–139. [PubMed] [Google Scholar]
- 20.World Health Organization.Weekly epidemiological record - Relevé épidémiologique hebdomadaire World Health Organ Tech Rep Ser 20108532309–320. [Google Scholar]
- 21.World Medical Association.World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects JAMA 2013310202191–2194. [DOI] [PubMed] [Google Scholar]


