Abstract
Greater levels of psychological well-being are associated with reduced disease and mortality risk, and lifestyle habits may be potential mechanisms underlying these relationships. Prospective studies show that positive psychological factors enhance the likelihood of adopting specific health behaviors; yet, whether they promote the adoption of multiple healthy behaviors, which can have a multiplicative effect on disease and mortality risk compared to individual behaviors, is unknown. We investigated whether happiness and optimism were related to a healthy lifestyle (characterized by multiple health behaviors) over 10-22 years of follow-up; we also explored bidirectional associations, assessing if a healthy lifestyle at baseline was related to greater likelihood of experiencing higher happiness and optimism over time. Women reported levels of happiness in 1992 (N=52,133) and optimism in 2004 (N=36,802). Health-related behaviors (physical activity, body mass index, diet, alcohol and tobacco consumption) were self-reported and combined into a lifestyle score, every four years from baseline until 2014. Multivariable generalized estimating equations with a Poisson distribution were used. Women with moderate and higher (versus lower) happiness levels were more likely to report sustaining healthy lifestyles (RR=1.18, CI= 1.11-1.25; RR=1.39, CI=1.32-1.46, respectively). In secondary analyses, the magnitude of the inverse association was somewhat smaller (likelihood of sustaining higher happiness levels for baseline healthy versus unhealthy lifestyle, RR=1.11, CI=1.10-1.12). Results were similar when considering optimism as the exposure and in other secondary analyses (e.g., across individual habits). While bidirectional associations are apparent, these findings suggest pursuing happiness and optimism as modifiable determinants of lifestyle deserves further consideration.
Keywords: chronic disease, happiness, health, health behavior, lifestyle, optimism, psychology, prevention, resilience, well-being
INTRODUCTION
Greater levels of psychological well-being (PWB), including optimism and life purpose, are associated with reduced disease and mortality risk (1, 2), and lifestyle habits have been proposed as potential mechanisms. Behaviors like physical activity, diet, and alcohol/tobacco consumption tend to cluster (3), leading to a lifestyle that has a multiplicative effect on the likelihood of mortality compared to individual behaviors (4). To date, studies revealing associations between psychological factors and subsequent lifestyle have almost exclusively focused on the detrimental role of anxiety/depressive symptoms or medical populations (5–7). Yet, whether PWB relates to lower likelihood of adverse outcomes by promoting a healthy lifestyle, in disease-free populations is unknown. Moreover, PWB is comprised of multiple dimensions (1) and whether each are similarly linked with lifestyle has not been assessed. Filling these knowledge gaps might broaden primary prevention strategies for targeting novel determinants. In fact, existing interventions, including brief self-administered exercises, have been shown to increase PWB, including happiness (8); such interventions may in turn help alleviate chronic disease burden (3, 9) by potentially catalyzing improved lifestyle behaviors.
Numerous prospective epidemiological studies have evaluated whether PWB enhances the likelihood of adopting single health behaviors; these investigations mainly focused on optimism’s potential role in smoking cessation/abstinence or physical activity over ≤6 years of follow-up, in non-medical samples (10–18). Overall, results suggested higher optimism levels are related to greater likelihood of engaging in healthy behaviors. Findings were maintained after adjusting for not only conventional risk factors but also depressive symptoms, suggesting PWB may play a role beyond simply indicating the absence of distress. While this work is informative, it remains unclear whether i) optimism is associated with the adoption/maintenance of multiple concurrent health-related behaviors (hereafter, “lifestyle”), including physical activity, diet, alcohol/tobacco consumption, and weight, which synergistically impact morbidity and mortality (4); ii) other PWB dimensions, including happiness, may relate to future lifestyle; and iii) these relations persist over a decade and beyond. Of particular interest is whether PWB might be associated with greater ability to sustain a healthy lifestyle, rather than if it affects average lifestyle scores over time.
In the current study, we investigated whether happiness and optimism were related to subsequent healthy lifestyle over a 10-22 year follow-up period in disease-free women. We considered happiness as it is one of the most commonly assessed PWB indicators in epidemiologic and surveillance research. We hypothesized that higher baseline levels of happiness and optimism would relate to greater likelihood of sustaining a healthy lifestyle. Based on previous research (10–18), we considered relevant covariates, including depression, previously identified as key potential confounders. While prior work has shown that favorable behaviors (e.g., physical activity, healthy diet) may also enhance PWB (19, 20), to our knowledge no prospective study has evaluated potential bidirectionality between PWB dimensions and lifestyle. Thus, a secondary analysis assessed if healthy lifestyle at baseline was related to a greater likelihood of experiencing sustained higher PWB over time.
METHODS
Participants
The Nurses’ Health Study is an ongoing cohort comprised of 121,700 U.S. female nurses, aged 30-55 years at study inception in 1976 (21), who completed biennial questionnaires on lifestyle, medical history, and newly diagnosed medical conditions, with a follow-up rate of >85% (22). As shown in Figure 1, the present study excludes participants with missing baseline data on happiness or optimism, the health-related behaviors of interest, or relevant covariates (see Supplemental Table S1 for characteristics of eligible versus ineligible women). Those reporting cancer, diabetes, or heart disease at the time PWB indicators were queried were also excluded, as chronic conditions may affect health behaviors (23), resulting in two analytic samples: nhappiness=52,133, noptimism=36,802. The study protocol was approved by the institutional review board of Brigham and Women’s Hospital.
Fig. 1.
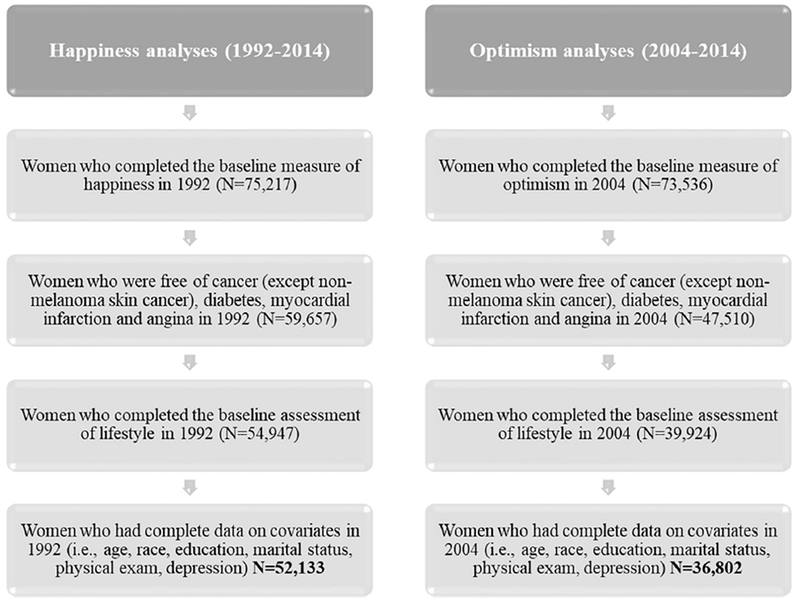
Flowchart of the two analytic samples.
Measures
Psychological well-being (PWB) dimensions.
To assess happiness, the following item from the Medical Outcomes Study SF-36 (24) was queried in 1992: “How much of the time during the last month have you been a happy person?” Women also responded to this item in 1996 and 2000; these data were used for the secondary analyses described below. Response options range from 1 “all the time” to 6 “none of the time,” and were reversed-coded so that a higher score reflected higher happiness. While single-item PWB measures are somewhat limited, they have demonstrated predictive capacity with cardiometabolic-related outcomes, including behaviors and mortality (1, 16), and often perform similarly to multiple-item measures (25). In this sample, happiness scores were modestly stable across the three assessments (intra-class correlations coefficient [ICC]=0.44). This finding is consistent with recent evidence from another study that used a similar happiness item and suggested that ~50% of the variance obtained was due to trait-like, stable processes (26).
Optimism was assessed in 2004 using the 6-item Life Orientation Test-Revised (27). It was also queried in 2008 and 2012, and these assessments were used for secondary analyses. This scale has good validity and reliability (27). Using a 5-point Likert scale, women were asked the degree to which they agreed with statements like “In uncertain times, I usually expect the best.” After reverse coding negatively worded items, all items were summed to create a composite score ranging from 6 to 30, with higher scores indicating higher optimism. Internal consistency (α=0.78) in the optimism analytic sample (2004 baseline) and overall stability across the three assessments (ICC=0.63) are moderate to high.
Happiness and optimism were first assessed at different times (1992 and 2004, respectively); therefore, the study baseline for each analytic sample was different. As both measures are available in each analytic sample, to assess the correlation between them, we considered happiness taken from 1992 in relation to optimism from 2004: rhappiness sample=0.32, roptimism sample=0.33. To assess discontinuous or threshold effects, following other studies (11, 12) we created three categories of each PWB indicator based on the score distribution in their respective analytic sample. Similar to other cohorts (28), most women in our sample reported higher happiness levels in 1992, resulting in unevenly distributed groups: low (14.62% of participants; score=1-3), moderate (18.89%; score=4), high (66.49%; score=5-6). For 2004 optimism, scores were more evenly distributed: low (32.13% of participants; score=6-23), moderate (30.96%; score=24-27), high (36.90%; score=28-30). To facilitate comparisons of effect size across indicators and studies, we also considered standardized PWB scores (M=0, SD=1).
Lifestyle score.
The five health-related behaviors included in the lifestyle score were: physical activity, body mass index (BMI; a behavior-related factor), diet, alcohol and tobacco consumption. They were selected based on a lifestyle index of multiple health behaviors commonly used in prior studies (6, 29), as well as cancer and cardiovascular prevention guidelines (30, 31). All individual behaviors were obtained via self-report at baseline (1992 or 2004), and every four years until 2014. We dichotomized each behavior according to whether women met recommended guidelines at each follow-up assessment (yes=1, no=0; see Text S1 for details about each cutpoint). Binary scores from each health behavior were then summed to create the lifestyle score, which ranges from 0 “least healthy” to 5 “most healthy” and was updated every four years. Because a score of 4 or 5 (healthy lifestyle) versus a score of 0-3 (unhealthy lifestyle) was associated with ~50% decreased risk of stroke in this cohort (29) and 66% decreased risk of mortality in prior research (4), we defined a healthy lifestyle using this outpoint (endorsing ≥4 healthy behaviors; yes/no). We further defined sustained healthy lifestyle as reporting a healthy lifestyle score at least twice over the study period, including the baseline assessment.
Covariates.
Selected confounders and other covariates included age (continuous), race (White, non-White), marital status (married/in a relationship, divorced/separated/widowed), education level (registered nurse, bachelor, master’s, doctorate), physical exam in the last two years (yes, no), as receiving advice from a clinician is associated with lifestyle changes (32), and depression status (i.e., antidepressant use or physician-diagnosed depression; yes, no). Age, marital status, and physical exam were self-reported at baseline for each analytic sample, whereas depression was obtained from the closest available assessment (happiness=1996; optimism=2004). Education and race were reported in 1992.
Statistical analysis
To characterize the degree of change in lifestyle over time, within-subject coefficients of variation (CVs) were computed (33). Associations of baseline happiness and optimism levels with likelihood of reporting a sustained healthy lifestyle over the follow-up period was evaluated using generalized estimating equations (GEE) which is robust to correlated observations; further a Poisson distribution was used to account for non-rare outcomes (34). In primary models we evaluated PWB dimensions as categorical variables (lower, moderate, higher levels) in relation to a sustained healthy lifestyle, with a test for linear trend. In additional models, continuous (standardized; per 1-SD) PWB variables were evaluated in relation to a sustained healthy lifestyle.
To leverage the information captured by the lifestyle scores more fully (i.e., ranging from 0-5) and assess change over time, we also considered categorical PWB indicators in relation to continuous lifestyle scores. In these models, a time x PWB interaction term was included to evaluate whether the rate of change in lifestyle scores over time differed depending on baseline PWB levels. All models controlled for age, race, marital status, education level, recent physical exam and depression.
We included secondary analyses. First, to explore the possible harmful role of extreme optimism on lifestyle, we modeled the likelihood of sustained healthy lifestyle for extremely high versus lower levels of optimism (extremely high=score of 30; 18.81% of the sample). Second, to account for women’s habits at study initiation and reduce concerns about concurrent lifestyle habits influencing both PWB levels and subsequent likelihood of sustained healthy lifestyle, we stratified models by baseline lifestyle score (healthy versus unhealthy), and used the likelihood ratio test. Third, to evaluate whether associations were consistent across habits, we investigated the likelihood of sustaining a healthy level of each behavior (i.e., for at least two assessments) separately.
Finally, we considered the inverse association, namely whether baseline lifestyle scores (categorical=healthy/unhealthy; continuous=per 1-SD) were associated with the likelihood of reporting sustained higher (versus moderate/lower) levels of happiness or optimism, at least twice over the follow-up period. For these analyses, all available PWB time points in the cohort were leveraged, including baseline lifestyle and PWB scores (happiness=1992; optimism=2004) and follow-up assessments (happiness=1996, 2000; optimism=2008, 2012). Linear mixed models were also used to assess whether PWB levels over time differed by baseline lifestyle levels (healthy/unhealthy), and whether the rate of change in PWB levels varied based by baseline lifestyle levels. Due to missing data on follow-up PWB measures, these analyses were conducted in ≥95% of the main samples (nhappiness=50,652; noptimism=35,043).
To address potential selection bias (see Table S1 for differences), person- and time-specific inverse probability weights were included in the models (35). Specifically, the probability of participating at each time point was modeled based on the exposure and covariates of interest among each analytic sample, and a weight that corresponded to the inverse of the probability of participating was created. Since results from age-adjusted models were similar to fully-adjusted models, only the latter are presented. Analyses were conducted using SAS 9.4 with a two-sided p-value of 0.05.
RESULTS
Baseline Characteristics
At the 1992 happiness baseline, women were 57.81 years old on average (SD=7.08; range=45-72), mostly White (98.00%), married/in a relationship (82.92%), registered nurses (RN=69.19%), reported a recent physical exam (87.37%) and not depressed (92.79%). The majority were non-smokers (86.45%), while nearly half had a healthy BMI (49.15%). Over one-third engaged in ≥150 minutes/week of moderate-to-vigorous physical activity (39.55%), whereas fewer drank on average 1 alcoholic drink/day (20.21%). Characteristics were comparable at the 2004 optimism baseline, with mean age=68.70 years (SD=6.83; range=57-84). Table 1 shows the distribution of covariates and health behaviors across baseline PWB levels.
Table 1.
Age-Standardizeda Distribution of Covariates and Health Behaviors According to Baseline Happiness and Optimism Levels.
| Happiness (1992)b | Optimism (2004)c | |||||
|---|---|---|---|---|---|---|
| Lower (n=7,622) | Moderate (n=9,848) | Higher (n=34,663) | Lower (n=11,826) | Moderate (n=11,395) | Higher (n=13,581) | |
| Age, mean (SD) | 56.42 (7.05) | 57.29 (7.11) | 58.27 (7.04) | 69.36 (7.07) | 68.88 (6.82) | 67.97 (6.55) |
| Non-Hispanic White, % | 97.94 | 97.47 | 98.15 | 98.21 | 97.96 | 98.19 |
| RN degree, % | 70.87 | 69.47 | 68.67 | 73.37 | 67.59 | 62.59 |
| Married/in a relationship, % | 79.29 | 82.18 | 83.94 | 70.61 | 72.69 | 74.27 |
| Physical exam in the last 2 years | 87.31 | 87.61 | 87.31 | 94.87 | 95.14 | 95.60 |
| BMI in kg/m2, mean (SD) | 26.12 (5.19) | 25.76 (4.80) | 25.67 (4.71) | 26.27 (5.20) | 26.05 (4.97) | 25.86 (4.78) |
| Current smoker, % | 17.23 | 14.81 | 12.38 | 8.18 | 6.91 | 6.11 |
| Former/never smoker, % | 83.07 | 85.66 | 87.97 | 91.82 | 93.09 | 93.89 |
| Cigarettes/day among smokers, mean (SD) | 14.11 (9.84) | 12.47 (9.09) | 12.26 (9.21) | 11.05 (8.59) | 10.20 (7.73) | 9.69 (7.40) |
| Physical activity in MET-hours/week, mean (SD) | 2.06 (3.33) | 2.47 (3.40) | 3.05 (4.07) | 2.15 (3.32) | 2.56 (3.57) | 2.91 (4.01) |
| Alcohol intake of 1 drink/day, % | 16.88 | 19.51 | 21.14 | 20.09 | 22.79 | 24.38 |
| AHEI Diet scored, mean (SD) | 47.14 (10.13) | 47.88 (9.79) | 48.83 (9.75) | 53.75 (11.32) | 55.36 (11.56) | 56.95 (11.51) |
| Depressed (physician diagnosis or antidepressant use), % | 17.04 | 8.49 | 4.60 | 17.61 | 10.64 | 7.50 |
BMI=body mass index; MET=metabolic equivalent of task; RN=registered nurses; SD=standard deviation.
Values are means (SD) or percentages and are standardized to the age distribution of the study population (except age). Values of polytomous variables may not sum to 100% due to rounding.
Due to a skewed distribution of happiness measured in 1992, participants were categorized into the following different groups: low (14.62% of participants; scores ranged from 1 to 3), moderate (18.89%; 4), high (66.49%; 5 to 6).
For optimism, levels were more evenly distributed resulting in participants being categorized approximately into tertiles low (32.13% of participants; scores ranged from 6 to 23), moderate (30.96%; 24 to 27), high (36.90%; 28 to 30) in 2004.
The AHEI diet score incorporates higher intake of vegetables, fruit, whole grains, nuts and legumes, long-chain (n-3) fatty acids, polyunsaturated fats; lower intake of sugar-sweetened beverages and fruit juice, red/processed meat, saturated fats, sodium. The score for each dietary component ranges from 0 (worst) to 10 (optimal), and then scores were summed.
Relation of happiness with future lifestyle
Within individuals, lifestyle scores were stable over time, as indicated by the fairly low within-subject variance (CV=0.30, confidence intervals: CI=0.30-0.30). Almost a quarter of the sample (24.07%) reported sustaining a healthy lifestyle (≥2 healthy lifestyle scores) over the study duration and among those, most (88.28%) did so on two consecutive lifestyle assessments (e.g., maintained a healthy lifestyle score in 1996 and 2000). Compared to women with lower happiness (Figure 2), those with moderate and higher levels were 18% and 39% more likely, respectively, to report sustaining a healthy lifestyle over time, after adjusting for covariates. A dose-response relationship was observed (p-trend≤0.0001), whereby the likelihood of adopting a sustained healthy lifestyle increased monotonically as happiness levels did. A similar pattern was evident across all individual health behaviors (Table S2).
Fig. 2.
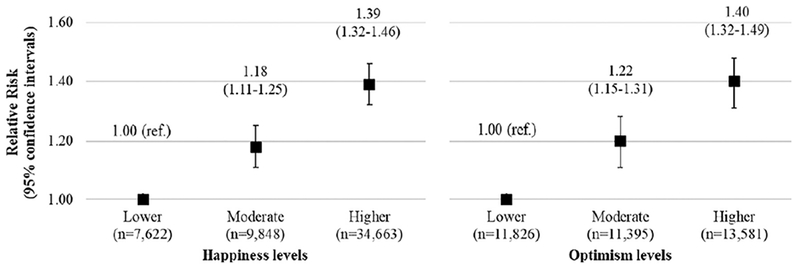
Generalized estimating equations with a Poisson distribution evaluating the associationa of baseline happiness (1992) and optimism (2004) levels with likelihood of reporting a sustained healthy lifestyleb over follow-up (until 2014).
aFully-adjusted models, controlling for baseline age, race, marital status, education level, physical exam in the last 2 years, and depression.
bDichotomized levels (healthy/unhealthy) of physical activity, diet, BMI, alcohol and tobacco consumption were summed to create the lifestyle score, ranging from 0 to 5 (most healthy) and updated at each follow-up assessment. The outcome was defined as reporting a healthy lifestyle score (i.e., ≥4 healthy behaviors) at least twice over the study period.
Findings were not altered substantially when evaluating happiness measured continuously (per 1-SD change) in relation to a sustained healthy lifestyle (relative risk: RR1-SD=1.13, CI=1.11-1.15). Results were also maintained when evaluating associations of happiness levels in relation to continuous lifestyles scores over time, with higher happiness levels associated with healthier lifestyle scores at each time point. While lifestyle scores generally decreased over time, they decreased slightly more rapidly for those with elevated happiness levels (pinteraction<0.0001; βmoderate vs. lower happiness x time=−0.001, CI=−0.002, 0.001; βhigher vs. lower happiness x time=−0.006, CI=−0.007, −0.005), perhaps because of regression to the mean. Stratified analyses by initial lifestyle levels yielded a stronger association among women with an initially unhealthy (versus healthy) lifestyle score (likelihood ratio test, phappiness x baseline lifestyle<0.0001; Table S3).
Relation of optimism with future lifestyle
In the optimism analytic subsample, women’s lifestyle scores were also stable across assessments (within-subject CV=0.25, CI=0.25-0.25); relatively few participants reported sustaining a healthy lifestyle (i.e., ≥2 healthy lifestyle scores; 15.66%), but among them, the majority (91.70%) did on two consecutive lifestyle assessments. As shown in Figure 2, moderate and higher (versus lower) optimism levels at baseline were associated with 22% and 40% greater likelihood of reporting a sustained healthy lifestyle throughout follow-up. A dose-response association was evident (p-trend≤0.0001) and similar patterns of association was observed for all individual behaviors (Table S2).
When considering optimism either as a continuous measure or at extremely high levels (versus lower optimism), the relationship with sustaining a healthy lifestyle was not substantially altered (RR1-SD=1.16, CI=1.13-1.19; RRextreme high vs. lower=1.39, CI=1.30-1.49). Findings were also comparable when considering categorical optimism with continuous lifestyle scores. As observed with the happiness results, lifestyle scores decreased somewhat more rapidly in women with elevated optimism levels (pinteraction<0.01, βmoderate vs. lower optimism x time=−0.002, CI=−0.004, 0.0002; βhigher vs. lower optimism x time=−0.004, CI=−0.006, −0.002). In stratified models, estimates were stronger among women with an initially unhealthy (versus healthy) lifestyle score (likelihood ratio test: poptimism x baseline lifestyle<0.0001; Table S3).
Relation of lifestyle with future levels of PWB
Compared to women with an unhealthy lifestyle at baseline, those with a healthy lifestyle were 11% more likely to report sustaining high happiness levels (RR=1.11, CI=1.10-1.12), and 26% more likely to report sustaining high optimism levels (RR=1.26, CI=1.22-1.31), after controlling for covariates. Continuous baseline lifestyle scores (per 1-SD) yielded similar relationships with likelihood of sustaining higher subsequent happiness and optimism levels (RRhappiness=1.06, CI=1.06-1.07; RRoptimism=1.14, CI=1.12-1.16). Further, investigating baseline lifestyle levels with continuous PWB scores at each follow-up assessments led to similar results. There was a slightly faster decline in happiness scores for women reporting healthy versus Unhealthy lifestyle at baseline (pinteraction=0.0006; βhealthy vs. unhealthy lifestyle x time=−0.005, CI=−0.007, −0.002), whereas no time x lifestyle interaction effect was noted with optimism (pinteraction>0.05).
DISCUSSION
This study investigated whether happiness and optimism levels were associated with subsequent likelihood of sustaining a healthy lifestyle over 10-22 years in middle-aged and older women. Compared to women with lower happiness and optimism levels, women with moderate levels were 18-22% more likely to report a healthy lifestyle at least twice throughout the study (with most of them being at two consecutive time assessments); the estimates were even stronger among women with higher happiness and optimism levels (i.e., 39-40%). A greater likelihood of reporting a sustained healthy lifestyle over time was also observed for every SD increase in both PWB dimensions, suggesting that even smaller improvements in happiness and optimism might potentially matter for lifestyle habits. Using prior findings from this cohort (36), we estimate that the difference in lifestyle scores evident for higher versus lower PWB levels (up to 0.33 points) would translate into up to 5.35% decreased risk of stroke (see Text S2 for calculations). Overall, our results are consistent with previous findings on single behaviors assessed over shorter periods (10–18). For instance, among women participating in the Women’s Health Initiative observational study, those with higher versus lower optimism scores at study initiation had a three-fold increase (i.e., improvement) in AHEI diet scores from baseline to one year later (11).
While happiness and optimism were assessed 12 years apart, which precludes formal comparison about within-person effects, it is notable that these modestly correlated constructs yielded comparable effect estimates for the likelihood of sustaining a healthy lifestyle. This may suggest that aspects of PWB common across the different dimensions are the critical factor driving associations of interest. In fact, an analogous phenomenon has been noted with psychological distress, whereby multiple dimensions like anger, anxiety, and depression often relate similarly with health outcomes (37, 38), and investigators have postulated that such associations could be explained by common rather than unique dimensions of psychological distress (37, 38). Or, it may be that PWB dimensions are somewhat exchangeable with regard to effects on lifestyle, perhaps in the way that different forms of physical activity may similarly affect health.
Consistent with prior studies evaluating the association of PWB with single behaviors (10–13, 16), analyses revealed associations that were independent of traditional covariates and depression. In stratified analyses, relationships of happiness and optimism with future likelihood of sustaining a healthy lifestyle were obtained among women with initially unhealthy versus healthy lifestyle scores, potentially suggesting a greater role of PWB in adopting versus maintaining a healthy lifestyle. However, approximately 65%-77% of women with an initially healthy lifestyle maintained their favorable habits subsequent to baseline, which could also have reduced our capacity to detect relations in this subgroup. Moreover, although prior research has documented negative associations between extremely high optimism levels and health-related outcomes (39), we did not find evidence for such associations. Midlife and older female nurses, due to both their maturity and knowledge about health, may be less prone to systematic cognitive distortions about their own probability of encountering negative [health] events, a characteristic of “unrealistic optimism” (39) that may be more common among younger adults or those who are not health professionals.
To our knowledge, no prospective study has specifically assessed the bidirectional associations between PWB and lifestyle. Our results revealed relationships in both directions; however, the lifestyle→PWB association was of equal or smaller magnitude than the PWB→lifestyle association, and due to data limitations, could only be evaluated over a shorter period (8 versus 10-22 years). Given efforts aimed at changing multiple behaviors have had limited success, especially in the long-term (3), our findings suggest that targeting PWB might prove to be a fruitful strategy for improving lifestyle. Accordingly, a recent conceptual model illustrates how targeting PWB as an upstream determinant may set in motion a cascade of positive changes, because subsequent concurrent healthy behaviors may in turn lead to greater PWB and, consequently, lower the risk of adverse health outcomes (9).
This study has some limitations. Since findings were from a sample of middle-aged and older health professionals free of chronic illnesses at baseline, investigating these associations among other populations is warranted. PWB levels might affect self-report of behaviors; however, participants were not aware of our study hypotheses. Self-reported habits may also be vulnerable to social desirability, which can lead to biased estimation of health behaviors (40). Yet, even if absolute levels are not reported precisely, behaviors would likely still be categorized appropriately as either healthy/unhealthy. Lastly, the l-item measure of happiness may not capture the construct comprehensively, although single items have been shown to perform similarly to multi-item measures in three large cohorts (25). To date, few epidemiologic studies have included PWB measures; while single items appear less-than-ideal, they may support further investment in multi-items measures for future research. Moreover, most women in our study reported a healthy lifestyle at two consecutive assessments; subsequent studies with more variability in lifestyle scores across assessments (e.g., alternating between healthy and unhealthy) should investigate whether PWB levels are associated with such variations. Strengths of the study include its prospective design over two decades, among a large and richly characterized sample. Additionally, repeated measures of both PWB and concurrent health behaviors allowed the investigation of bidirectionality between psychological and behavioral factors. To reduce concerns that initial lifestyle levels might affect both baseline PWB and subsequent lifestyle habits we conducted stratified analyses by baseline lifestyle levels. Lastly, the consideration of two PWB dimensions and a lifestyle composite also permitted a comprehensive perspective on how PWB indicators influence multiple habits that are synergistically involved in health.
Conclusion
Results from this study suggest that greater happiness and optimism levels might foster sustaining a healthy lifestyle over time, which could contribute to lower disease/mortality risk. It is noteworthy that elevated PWB may subsequently lead to the adoption of a healthy lifestyle even in women with initially unhealthy habits. Over the past 20 years, accumulating evidence has suggested that various interventions, from brief self-administered exercises to professionally-delivered psychotherapy, may increase diverse facets of PWB (8). As most U.S. adults exhibit suboptimal levels of physical activity and weight, and a large proportion maintain a poor diet and smoking habits (41), considering happiness and optimism as modifiable determinants of lifestyle deserves further consideration, particularly in clinical trials.
Supplementary Material
Highlights:
Higher happiness and optimism levels were related to sustaining a healthy lifestyle
These prospective relationships were evident over follow-up periods of 10-22 years
The size of effect on improved lifestyle is enough to reduce stroke risk by 2-5%
Relations were independent of age, sociodemographic factors, and depression
Healthier lifestyle also led to future greater happiness and optimism levels
Acknowledgments & Funding Sources
We would like to thank the participants and the staff of the Nurses’ Health Study for their valuable contributions. This work was supported by the National Institutes of Health [grant UM1 CA186107] to The Nurses’ Health Study, [grant K99AG055696] to the third author, and [grant R01-AG053273] to the last two authors, as well as the Fonds de Recherche du Québec-Santé [postdoctoral fellowship] to the first author. Eric S. Kim has worked as a consultant with AARP and United Health Group. The other authors do not report potential conflict of interest. No financial disclosures were reported by the authors of this paper.
Abbreviations
- BMI
body mass index
- CI
confidence interval
- CV
coefficient of variation
- GEE
generalized estimating equations
- PWB
psychological well-being
- RR
relative risk
- SD
standard deviation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Boehm JK, Kubzansky LD. The heart’s content: The association between positive psychological well-being and cardiovascular health. Psychological bulletin. 2012;138(4):655–91. [DOI] [PubMed] [Google Scholar]
- 2.Martin-Maria N, Miret M, Caballero FF, Rico-Uribe LA, Steptoe A, Chatterji S, et al. The impact of subjective well-being on mortality: A meta-analysis of longitudinal studies in the general population. Psychosomatic medicine. 2017. [DOI] [PubMed] [Google Scholar]
- 3.Spring B, King AC, Pagoto SL, Van Horn L, Fisher JD. Fostering multiple healthy lifestyle behaviors for primary prevention of cancer. The American psychologist. 2015;70(2):75–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: A systematic review and meta-analysis. Prev Med 2012;55(3):163–70. [DOI] [PubMed] [Google Scholar]
- 5.Murray J, Craigs CL, Hill KM, Honey S, House A. A systematic review of patient reported factors associated with uptake and completion of cardiovascular lifestyle behaviour change. BMC Cardiovasc Disord. 2012;12:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Trudel-Fitzgerald C, Tworoger SS, Poole EM, Zhang X, Giovannucci EL, Meyerhardt JA, et al. Psychological symptoms and subsequent healthy lifestyle after a colorectal cancer diagnosis. Health Psychol. 2018;37(3):207–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sin NL, Moskowitz JT, Whooley MA. Positive affect and health behaviors across 5 years in patients with coronary heart disease: The Heart and Soul Study. Psychosomatic medicine. 2015;77(9):1058–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health. 2013;13:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Cappellen P, Rice EL, Catalino LI, Fredrickson BL. Positive affective processes underlie positive health behaviour change. Psychology & health. 2018;33(1):77–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Progovac AM, Chang YF, Chang CH, Matthews KA, Donohue JM, Scheier MF, et al. Are optimism and cynical hostility associated with smoking cessation in older women? Ann Behav Med 2017;51(4):500–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hingle MD, Wertheim BC, Tindle HA, Tinker L, Seguin RA, Rosal MC, et al. Optimism and diet quality in the Women’s Health Initiative. J Acad Nutr Diet. 2014;114(7):1036–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim ES, Kubzansky LD, Soo J, Boehm JK. Maintaining healthy behavior: A prospective study of psychological well-being and physical activity. Ann Behav Med 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Progovac AM, Donohue JM, Matthews KA, Chang CH, Habermann EB, Kuller LH, et al. Optimism predicts sustained vigorous physical activity in postmenopausal women. Prev Med Rep 2017;8:286–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giltay EJ, Geleijnse JM, Zitman FG, Buijsse B, Kromhout D. Lifestyle and dietary correlates of dispositional optimism in men: The Zutphen Elderly Study. Journal of psychosomatic research. 2007;63(5):483–90. [DOI] [PubMed] [Google Scholar]
- 15.Haller CS. Trajectories of smoking behavior as a function of mood and satisfaction with life: What matters most? Journal of affective disorders. 2016;190:407–13. [DOI] [PubMed] [Google Scholar]
- 16.Baruth M, Lee DC, Sui X, Church TS, Marcus BH, Wilcox S, et al. Emotional outlook on life predicts increases in physical activity among initially inactive men. Health Educ Behav 2011;38(2):150–8. [DOI] [PubMed] [Google Scholar]
- 17.Boehm JK, Chen Y, Koga H, Mathur MB, Vie LL, Kubzansky LD. Is optimism associated with healthier cardiovascular-related behavior? Meta-analyses of 3 health behaviors. Circulation research. 2018;122(8):1119–34. [DOI] [PubMed] [Google Scholar]
- 18.Boehm JK, Soo J, Zevon ES, Chen Y, Kim ES, Kubzansky LD. Longitudinal associations between psychological well-being and the consumption of fruits and vegetables. Health Psychol. 2018;37(10):959–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.White RL, Babic MJ, Parker PD, Lubans DR, Astell-Burt T, Lonsdale C. Domain-specific physical activity and mental health: A meta-analysis. American journal of preventive medicine. 2017;52(5):653–66. [DOI] [PubMed] [Google Scholar]
- 20.Stevenson RJ. Psychological correlates of habitual diet in healthy adults. Psychological bulletin. 2017;143(1):53–90. [DOI] [PubMed] [Google Scholar]
- 21.Willett WC, Green A, Stampfer MJ, Speizer FE, Colditz GA, Rosner B, et al. Relative and absolute excess risks of coronary heart disease among women who smoke cigarettes. N Engl J Med 1987;317(21):1303–9. [DOI] [PubMed] [Google Scholar]
- 22.Bao Y, Bertoia ML, Lenart EB, Stampfer MJ, Willett WC, Speizer FE, et al. Origin, methods, and evolution of the three Nurses’ Health Studies. American journal of public health. 2016;106(9):1573–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Newsom JT, Huguet N, McCarthy MJ, Ramage-Morin P, Kaplan MS, Bernier J, et al. Health behavior change following chronic illness in middle and later life. The journals of gerontology. 2012;67(3):279–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 25.Cheung F, Lucas RE. Assessing the validity of single-item life satisfaction measures: results from three large samples. Qual Life Res 2014;23(10):2809–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hudson NW, Lucas RE, Donnellan MB. Day-to-day affect is surprisingly stable: A two-year longitudinal study of well-being. Soc Psychol Personal Sci 2017;8(1):45–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. Journal of personality and social psychology. 1994;67(6):1063–78. [DOI] [PubMed] [Google Scholar]
- 28.Boehm JK, Chen Y, Williams DR, Ryff C, Kubzansky LD. Unequally distributed psychological assets: Are there social disparities in optimism, life satisfaction, and positive affect? PloS one. 2015;10(2):e0118066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chiuve SE, Rexrode KM, Spiegelman D, Logroscino G, Manson JE, Rimm EB. Primary prevention of stroke by healthy lifestyle. Circulation. 2008;118(9):947–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, et al. American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: Reducing the risk of cancer with healthy food choices and physical activity. CA: a cancer journal for clinicians. 2012;62(1):30–67. [DOI] [PubMed] [Google Scholar]
- 31.Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. Journal of the American College of Cardiology. 2011;57(12):1404–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rose SA, Poynter PS, Anderson JW, Noar SM, Conigliaro J. Physician weight loss advice and patient weight loss behavior change: a literature review and meta-analysis of survey data. Int J Obes (Lond). 2013;37(1):118–28. [DOI] [PubMed] [Google Scholar]
- 33.Hankinson SE, Manson JE, Spiegelman D, Willett WC, Longcope C, Speizer FE. Reproducibility of plasma hormone levels in postmenopausal women over a 2–3-year period. Cancer Epidemiol Biomarkers Prev 1995;4(6):649–54. [PubMed] [Google Scholar]
- 34.Zou G A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159(7):702–6. [DOI] [PubMed] [Google Scholar]
- 35.Hernan MA, Hernandez-Diaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15(5):615–25. [DOI] [PubMed] [Google Scholar]
- 36.Trudel-Fitzgerald C, Tworoger SS, Poole EM, Williams DR, Kubzansky LD. Prospective changes in healthy lifestyle among midlife women: When psychological symptoms get in the way. American journal of preventive medicine. 2016;51(3):327–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suls J Toxic affect: Are anger, anxiety, and depression independent risk factors for cardiovascular disease? Emotion Review. 2018;10(1):6–17. [Google Scholar]
- 38.Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: the problems and implications of overlapping affective dispositions. Psychological bulletin. 2005;131(2):260–300. [DOI] [PubMed] [Google Scholar]
- 39.Shepperd JA, Waters E, Weinstein ND, Klein WM. A primer on unrealistic optimism. Curr Dir Psychol Sci 2015;24(3):232–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hebert JR, Ebbeling CB, Matthews CE, Hurley TG, Ma Y, Druker S, et al. Systematic errors in middle-aged women’s estimates of energy intake: comparing three self-report measures to total energy expenditure from doubly labeled water. Ann Epidemiol 2002;12(8):577–86. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization. Global status report on noncommunicable diseases. Geneva: World Health Organization; 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


