Abstract
Goods and services provided by businesses can either promote health or represent an additional risk factor. We assessed the association between business pattern indicators and the prevalence of adult obesity, diabetes, physical inactivity, fair or poor health and frequent physical and mental distress. Data on business types were obtained from the 2013 U.S. Census Bureau County Business Patterns. County health data were obtained from the Centers for Disease Control and Prevention Diabetes Interactive Atlas, Behavior Risk Factor Surveillance System and Fatality Analysis Reporting System. We explored the relationship at county level using the global (Ordinary Least Square regression) and local (Geographically Weighted Regression (GWR)) models in 3108 U.S. counties. Density of full service restaurants and fitness centers was associated with a significant decrease in adult obesity, diabetes, fair or poor health, physical inactivity, physical and mental distress. Conversely, density of payday loan centers was associated with an increase in these adverse health outcomes. However, our GWR models revealed substantial geographical variations in these relationships across the U.S. counties. Better understanding of the association between area-level structures and important health outcomes at the local level is important for developing targeted context-specific policy interventions. Full service restaurants and fitness centers may provide places for people to access higher quality food, socialize and exercise. Conversely, payday loans provide an expensive form of short-term credit and this debt may degrade an individual or family’s ability to achieve or maintain health. Our study emphasizes the influence of local built environment characteristics on important health outcomes.
Keywords: geography, business patterns, county, chronic disease, health, quality of life, geographically weighted regression
INTRODUCTION
Background
Geography is an important determinant of health. Where we live, including the social, political, economic, and built environment impacts health and creates health inequities (1–3). County-level contextual factors (e.g., socioeconomic status, public health policy, and access to health care) have been associated with coronary heart disease (4), health related quality of life (5), and obesity (6). Disadvantaged neighborhoods may have fewer resources that support physical activity and healthy diets. Residents in poorer neighborhoods tend to have fewer recreational facilities, higher crime rates, and insufficient police protection, which constrain physical activity outdoors (7, 8). Poor and minority neighborhoods have fewer large supermarkets than wealthy and majority white neighborhoods (9). Healthy foods are more abundant and affordable at large supermarkets than at convenience stores or neighborhood grocery stores. Studies have documented increased fruit and vegetable consumption with more supermarket availability (10). Poor neighborhoods, which have been labeled “food deserts,” also tend to have more fast food restaurants, which can contribute to weight gain (11). Density of fast food restaurants has been associated with higher individual-level weight (12). Poorer dietary practices have been observed among youth and adults living in disadvantaged neighborhoods compared to those living in better off neighborhoods, even after accounting for individual socioeconomic status (SES) (13).
Several studies have documented spatial variations in the prevalence of adverse health outcomes such as obesity and diabetes across the U.S. (6, 14). Furthermore, these studies found these chronic diseases correlate with poverty and physical activity across the U.S. However, there is paucity of information on whether spatial variations in these chronic conditions are associated with spatial variations in the density of food outlets (fast food restaurants, full service restaurants) and other area-level business patterns. Understanding the influence of local business patterns on health outcomes could help customize targeted prevention and intervention programs for chronic health outcomes. The present study explored the geographical variation in the association between prevalence of health outcomes such as obesity, diabetes, physical inactivity, frequent physical and mental distress and density of area level business patterns by employing Geographically Weighted Regression (GWR). GWR, an extension of Ordinary Least Squares regression (OLS), has been used extensively in health studies (43, 44) and has also been adopted in studies on obesity and diabetes (6,14). GWR models allow exploration of spatially non-stationary relationships between each predictor and health outcomes (6,14).
Study Aims and Hypotheses
In this study, we examined geographical variation in health-related quality of life using area-level business patterns and demographic characteristics. We hypothesize that areas with more full service restaurants, fitness centers, grocery stores, and nature parks will have better health, whereas areas with more payday loan places (as an indicator of poverty and economic exploitation), alcohol outlets, and limited-service restaurants (i.e., fast food places) will have worse health-related quality of life. We use GWR to further assess the geographic heterogeneity in the relationship between business patterns and health outcomes through estimation of local, rather than global, parameter estimates.
METHODS
Business data.
Data on business types at the county level were obtained from the 2013 U.S. Census Bureau County business patterns accessed via American FactFinder (15). The following North American Industry Classification System (NAICS) codes were utilized to categorize businesses: 722410 (drinking places (alcoholic beverages); these places are also known as bars, taverns, night clubs and primarily serve alcohol and may have limited food services) and 722511 (full-service restaurants; these include for instance, diners, steakhouses). Fast food was defined by the following NAICS codes: 722513 (limited-service restaurants; these include carryout restaurants, drive-in restaurants and other fast food restaurants) and 722515 (snack and nonalcoholic beverage bars). We also tracked supermarkets and grocery stores (NAICS code: 445110), fitness and recreational sports centers (NAICS code: 713940), and nature parks (NAICS code: 712190).
County-level Health Outcomes.
All business data were then aggregated to the county-level to compare with county-level health outcomes. County health data were obtained from data from the CDC Diabetes Interactive Atlas, Behavior Risk Factor Surveillance System (BRFSS) and Fatality Analysis Reporting System (16–18). Adult obesity: is the percentage of the adult population (age 20 and older) that reported a body mass index (BMI) greater than or equal to 30 kg/m2. Diabetes: is the prevalence of diagnosed diabetes and is based on the response to the survey question, “Has a doctor ever told you that you have diabetes?” Fair or Poor Health: is the percentage of adult survey respondents who rated their health “fair” or “poor” in response to the survey question: “In general, would you say that your health is excellent, very good, good, fair, or poor? Physical inactivity: is the percentage of adults of age 20 and over reporting no leisure-time physical activity. “Poor mental health days or mental distress: This measure is based on survey responses to the question: “Thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” The value in our analytic dataset is the average number of days a county’s adult respondents reported that their mental health was not good. Poor Physical Health Days or physical distress is based on survey responses to the question: “Thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?” The value in our analytic dataset is the average number of days a county’s adult respondents reported that their physical health was not good. These measures of unhealthy days have high retest reliability (19). Additionally, a study investigating the validity of these measures found that counties with more unhealthy days were likely to have higher unemployment, poverty, percentage of adults who did not complete high school, mortality rates, and prevalence of disability than counties with fewer unhealthy days (20). Geographic information system shapefiles of U.S. counties were downloaded from the US Census Bureau Topographically Integrated Geographic Encoding and Referencing files (21).
Analytic approach.
Business pattern characteristics were categorized into quantities. In OLS regression models, we used business patterns indicators to predict health outcomes across 3108 U.S. counties. Models were run separately for each health outcome. Sample size varied due to missing outcome or predictor variables. County-level demographic characteristics were obtained from the 2010–2014 American Community Survey 5-year estimates and included the following: median age, and percentage non-Hispanic white, and an economic disadvantage factor score derived from the following characteristics: percent female-headed households, percent families living in poverty, unemployment rate, percent college graduates (reverse coded), and median family income (reverse coded) (22). In addition, models controlled for the following covariates obtained from the Robert Wood Johnson Foundation’s County Health Rankings: violent crime rate, number of primary care physicians per 100,000 population and percentage of county population not proficient in English. There was no multicollinearity between the independent variables evaluated using the variance inflation factor (45). We evaluated statistical significance at p<0.05. OLS regressions were performed using R software (23).
Geographically weighted regression (GWR) was performed to explore local association between health outcomes and the predictor variables (24). OLS models assume statistical independence of observations and spatial stationarity of the relationship between health outcome and predictor variables (24, 25). However, proximate observations often exhibit stronger relationships, which result in spatial autocorrelation and biased parameter estimates (6, 14). GWR model relaxes these assumptions and performs multiple regressions so that there is one regression for each spatial data point (e.g., county) (26). GWR assigns higher weight to observations closer in proximity to a particular data point and produces a range of coefficients for each spatial data point (26). As a measure of spatial autocorrelation, we calculated Moran’s I of the residuals estimated from the OLS regressions and GWR models across the U.S. counties. The GWR models were run separately for each health outcome and were adjusted for the same covariates described above as the OLS models. GWRs were performed using ArcGIS10.5. The study was approved by the University of Maryland Institutional Review Board.
RESULTS
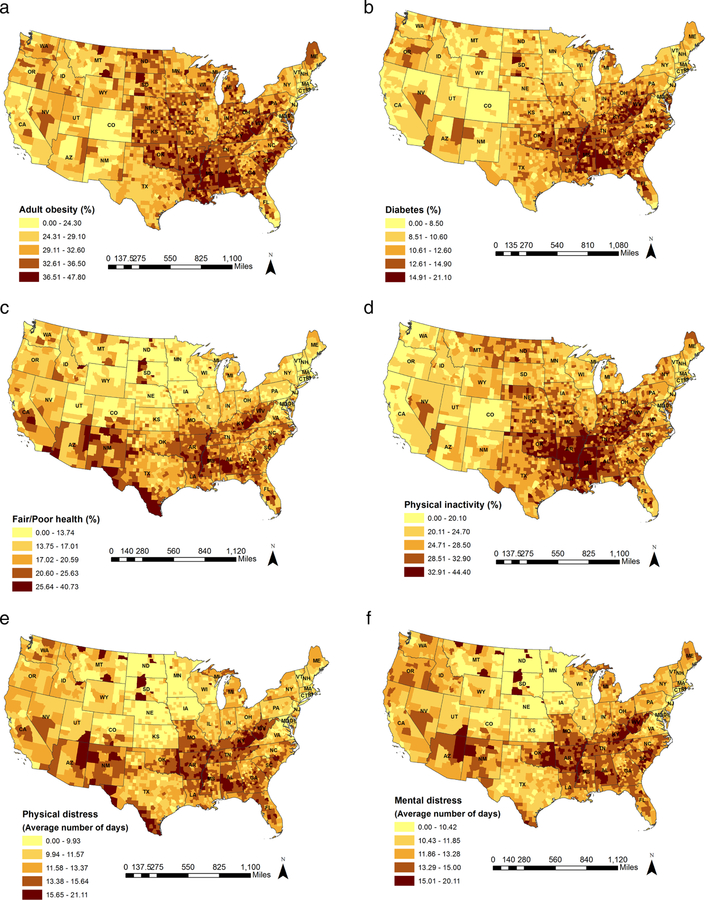
Table 1 presents the summary statistics for both the dependent and the independent variables. The mean density (per 10,000 population) of businesses were 7.60 for full service restaurants, 0.69 for fitness centers, 0.04 for nature parks, 2.51 for grocery stores, 1.79 for alcohol outlets, 0.41 for payday loan centers and 5.85 for limited service restaurants. On average, 31.48% of a county’s population was obese and 11.41% of a county’s population was diabetic. The physically inactive population and population with fair or poor health, on average, accounted for 26.87% of the county population and 17.48% of the county population. On average, a county’s population had frequent physical and mental distress for 12.00 days and 12.21 days respectively. In a county, on average, 29.92% of the motor vehicle deaths were due to alcohol involvement and on average 17.38% of a county’s population reported excessive drinking. Figure 1 shows variation in these health outcomes across the contiguous U.S. counties. Overall, the percentage of population with obesity, diabetes and physical inactivity was much higher in southeastern and Midwestern counties as compared to those in other regions. There was a higher percentage of population with frequent physical and mental distress and with fair or poor health in southeastern and southwestern counties as compared to those in other regions.
Table 1.
Descriptive statistics, county level
| Number of counties | Mean (Standard Deviation) | |
|---|---|---|
| 2013 Business patterns | ||
| (Density per 10,000 population) | ||
| Full service restaurants | 3,108 | 7.90 (6.08) |
| Fitness centers | 3,108 | 0.69 (0.73) |
| Nature parks | 3,108 | 0.04 (0.26) |
| Grocery stores | 3,108 | 2.51 (2.07) |
| Alcohol places | 3,108 | 1.79 (2.94) |
| Payday loan centers | 3,108 | 0.41 (0.58) |
| Limited service restaurants | 3,108 | 5.85 (3.20) |
| 2014–2016 County health outcomesb | ||
| Percent obesity | 3,108 | 31.48 (4.50) |
| Percent diabetes | 3,108 | 11.41 (2.50) |
| Percent fair or poor health | 3,108 | 17.48 (4.70) |
| Leisure-time physical inactivity | 3,108 | 26.87 (5.17) |
| Percent motor vehicle deaths with alcohol | 3,108 | 29.92 (15.39) |
| Percent excessive drinking | 3,108 | 17.38 (3.24) |
| Frequent physical distress (average days) | 3,108 | 12.00 (2.30) |
| Frequent mental distress (average days) | 3,108 | 12.21 (1.87) |
Data sources for health outcomes: 2014 CDC Diabetes Interactive Atlas for prevalence of obesity, diabetes, and leisure-time physical activity; 2016 Behavioral Risk Factor Surveillance System for fair or poor health, percent excessive drinking, percent of adults reporting poor mental health and physical health days; 2012–2016 Fatality Analysis Reporting System for percent motor vehicle deaths with alcohol involvement.
Business data obtained from 2013 County Business Patterns. Business categories calculated as the number of business establishments per 10,000 population.
Figure 1.
National distribution of health outcomes (unadjusted for county characteristics), county level; (a) Adult obesity; (b) Diabetes; (c) Fair/Poor health; (d) Physical inactivity; (e) Physical distress; and (f) Mental distress.
Business patterns.
Tables 2 reports the range of local coefficient estimates for business pattern indicators and other predictor variables from GWR models for obesity; eTables 1–5 report the GWR estimates for the remaining health outcomes. The estimated change in county adult obesity resulting from one standard deviation increase in the density of full service restaurants, fitness centers, payday loan centers, limited service restaurants, grocery stores, nature parks and alcohol outlets ranged from a decrease of 2.05%, 0.75%, 0.29%, 0.59%, 1.03%, 0.90%, and 1.88% to an increase of 0.20%, 0.16%, 1.31%, 0.92%, 1.37%, 0.86%, and 2.35% across U.S. counties respectively (Table 2).
Table 2.
Partial results from the GWR model for adult obesity, county level
| Coefficient Range | Percentage of counties by 95% of t-statistic | ||||
|---|---|---|---|---|---|
| Min | Max | t ≤ −1.96 | −1.96 < t < 1.96 | t ≥ 1.96 | |
| Intercept | 26.52 | 33.74 | 0.00 | 0.00 | 100.00 |
| Full service restaurants | −2.05 | 0.20 | 76.45 | 23.55 | 0.00 |
| Fitness centers | −0.75 | 0.16 | 26.32 | 73.68 | 0.00 |
| Nature parks | −0.90 | 0.86 | 1.77 | 94.05 | 4.18 |
| Grocery stores | −1.03 | 1.37 | 11.65 | 80.15 | 8.20 |
| Alcohol outlets | −1.88 | 2.35 | 14.70 | 60.46 | 24.84 |
| Payday loan centers | −0.29 | 1.31 | 0.00 | 51.87 | 48.13 |
| Fast food restaurants | −0.59 | 0.92 | 8.08 | 75.45 | 16.47 |
| % less than 18 years old | −0.29 | 2.93 | 0.00 | 33.33 | 66.67 |
| % 65 years and older | −1.18 | 2.63 | 46.01 | 33.14 | 20.85 |
| % Hispanic | −6.46 | 4.03 | 59.62 | 39.06 | 1.32 |
| % non-Hispanic black | −5.35 | 0.24 | 34.65 | 65.35 | 0.00 |
| % non-Hispanic Asian | −2.30 | −0.08 | 95.82 | 4.18 | 0.00 |
| % American Indian/Alaskan | −8.73 | 4.21 | 2.16 | 50.29 | 47.55 |
| Economic Disadvantage | −1.02 | 2.50 | 1.51 | 17.60 | 80.89 |
| % not proficient in English | −2.07 | 2.26 | 4.02 | 65.51 | 30.47 |
| Violent crime rate | −0.61 | 1.34 | 5.47 | 52.80 | 41.73 |
| Primary care physicians | −1.39 | 0.29 | 47.39 | 52.61 | 0.00 |
Overall, statistically significant inverse associations between full service restaurants and adult obesity, diabetes, fair or poor health and physical inactivity occupied approximately 76%, 64%, 46% and 47% of all county-specific estimates after controlling for other county characteristics. None of the U.S. counties showed a significant positive association between full service restaurants and these health outcomes. Statistically significant inverse associations between full service restaurants and physical distress and mental distress accounted for approximately 40% and 29% of all county-specific coefficient estimates, whereas statistically significant positive associations accounted for merely 5% and 7% respectively. Statistically significant inverse associations between fitness centers and adult obesity, diabetes, fair or poor health, physical inactivity, physical distress and mental distress accounted for approximately 26%, 42%, 17%, 50%, 1.6% and 5.2% of all county-specific coefficient estimates. None of the U.S. counties showed a significant positive association between fitness centers and these health outcomes.
Statistically significant positive associations between payday loan centers and adult obesity, diabetes, fair or poor health, physical inactivity, physical distress and mental distress accounted for approximately 48%, 48.3%, 26.5%, 26% 33% and 35% of all county-specific coefficient estimates. None of the U.S. counties showed a significant inverse association between payday loan centers and prevalence of adult obesity and diabetes. A statistically significant inverse association between payday loan centers and fair/poor health, physical inactivity, physical distress and mental distress was found in approximately 14%, 5%, 23% and 33% of the U.S. counties respectively.
While a statistically significant positive association between limited service restaurants and adult obesity, diabetes, fair or poor health, physical inactivity, physical distress and mental distress was present in approximately 16%, 21%, 19%, 20%, 15% and 28% of the U.S. counties respectively, a statistically significant inverse association between limited service restaurants and these health outcomes was present in several counties. We found a statistically significant positive association between grocery stores and obesity, diabetes, fair or poor health, physical inactivity, physical distress, and mental distress in approximately 8%, 17%, 42%, 22%, 39% and 33% of the U.S. counties and a statistically significant inverse association between grocery stores and these health outcomes in several counties. A statistically significant inverse association between alcohol outlets and health outcomes was present in several U.S. counties. GWR models revealed a significant inverse association between nature parks and physical inactivity in approximately 12% of the U.S. counties.
eTables 6–8 summarize the results from OLS regression models. Decrease in the density of full service restaurants and fitness centers and increase in the density of payday loan places was associated with an increase in the county-level prevalence of adult obesity, diabetes, fair or poor health, physical inactivity, physical distress and mental distress. Decrease in the density of grocery stores was associated with an increase in county-level prevalence of diabetes, frequent physical and mental distress. Decrease in the density of nature parks was associated with an increase in the county-level prevalence of fair/poor health and physical inactivity. Counties within the highest tertile of density of alcohol outlets were associated with 2.76 percent increase in binge or heavy drinking and 5.57 percent increase in motor vehicle deaths with alcohol involvement in comparison with the lowest tertile of density of alcohol outlets. However, more alcohol outlets was also associated with lower chronic disease, physical inactivity, and mental and physical distress. Increase in the density of limited service restaurants was associated with an increase in the county-level prevalence of diabetes and frequent mental distress (eTables 6–8).
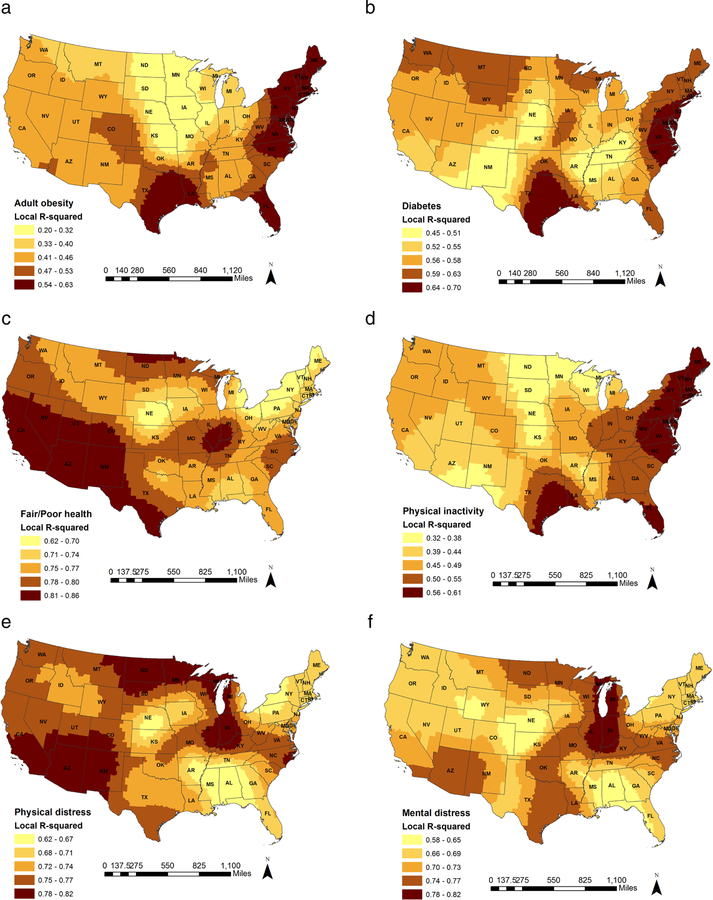
Substantial geographical variations were observed in the estimated coefficients of business pattern indicators for all the health outcomes (eFigures 2–7). The residuals from the OLS models were spatially autocorrelated indicating that the county level prevalence of health outcomes were spatially dependent across the US states (eFigure 1). The estimated values of Moran’s I of the residuals from OLS models indicated substantial geographical variation across the U.S. counties that were not explained by global OLS models (eTable 9). As suggested by Moran’s I of the residuals estimated from GWR models, the spatial autocorrelation in GWR models was reduced though not completely eliminated as compared to the OLS models (eTable 10). Compared to the OLS models, the AIC value for GWR models were greatly reduced, indicating a better fit of data using GWR for all the health outcomes. Adjusted R2 based on the OLS regression for adult obesity, diabetes, fair or poor health, physical inactivity, physical distress and mental distress was 0.46, 0.61, 0.79, 0.47, 0.74 and 0.71 respectively. Adjusted R2 based on the GWR ranged from 0.20 to 0.63, 0.45 to 0.70, 0.62 to 0.86, 0.32 to 0.61, 0.62 to 0.82 and 0.58 to 0.82 for adult obesity, diabetes, fair or poor health, physical inactivity, and frequent physical and mental distress respectively (Figure 2)
Figure 2.
Local R2 values from the GWR models; (a) Adult obesity; (b) Diabetes; (c) Fair/Poor health; (d) Physical inactivity; (e) Physical distress; and (f) Mental distress.
DISCUSSION
Unique attributes of counties such as built environment features, local policies, contexts and programs influence the burden of disabilities and chronic disease in the population (6, 14). This study assessed the association between county health outcomes and business pattern indicators (full service restaurants, limited service restaurants, grocery stores, fitness centers, nature parks, payday loan places and alcohol outlets), after adjusting for various county-level characteristics, using both global and local regression (OLS and GWR) models. GWR models revealed the existence of substantial geographical variations in the association between aforementioned health outcomes and business pattern indicators across the U.S. counties. These spatially varying relationships suggest the possible need to have geographically tailored policies and programs to address specific health outcomes in specific counties. Intervening on certain business patterns may be more effective in some counties compared to others.
Local food environments comprising of food stores and food serving places have been shown to be associated with people’s dietary choices (10, 27). Results from our GWR models showed that there existed a significant inverse association between full service restaurants and the prevalence of health outcomes such as adult obesity, diabetes, fair or poor health and physical inactivity in a proportion of the U.S. counties. None of the U.S. counties showed a significant positive association between full service restaurants and these health outcomes. Our findings are consistent with the findings from previous county-level studies, which documented an inverse relationship between full service restaurants and prevalence of obesity and diabetes (27, 41).
However, we observed spatial variation in the association between full service restaurants and the prevalence of physical distress and mental distress across the U.S. counties. For instance, we found a statistically significant inverse association between full service restaurants and frequent physical distress in counties in the western, northeastern, southeastern region and in Nebraska and Kansas and a statistically significant positive association between full service restaurants and frequent physical distress in the counties in Mississippi, Louisiana, Arkansas and Texas.
Consumption of fast food and density of fast food outlets has been shown to be positively associated with the county-level prevalence of obesity and diabetes (28, 27, 41). We found a spatial variation in the association between limited service/fast food restaurants and prevalence of obesity and diabetes. While a statistically significant positive association between limited service restaurants and obesity was observed in the counties in Northeastern region and in Colorado, New Mexico, Illinois, Indiana, Kentucky, Missouri, Arkansas, Mississippi, Tennessee, a statistically significant inverse association was observed in counties in Texas and Oklahoma. Several studies have suggested the influence of distance and availability on the prevalence of adverse health outcomes. Residing further away from healthier food outlets and closer to fast food restaurants is likely to result in reduced access to healthier foods and unhealthy dietary habits (10, 28, 29–31). Similar geographical variation was observed in the relationship between limited service restaurants and other health outcomes such as diabetes, fair or poor health, physical inactivity, physical and mental distress across the U.S. counties. In our study, spatially varying patterns were also observed in the association between the density of grocery stores and adverse health outcomes. Other studies have reported mixed findings regarding association between density of grocery stores and county-level prevalence of obesity and diabetes (27, 32, 41).
The GWR models also revealed a significant inverse association between density of fitness centers and the prevalence of adult obesity, diabetes, fair or poor health and physical inactivity in a proportion of the U.S. counties. Our findings are consistent with the findings from studies conducted by Pitts and colleagues and Salois, which documented an inverse association between county-level prevalence of obesity and diabetes and density of recreational and fitness facilities (28, 42). Several other studies have documented favorable effects of availability of fitness centers and recreational facilities on physical activity, blood pressure and body weight (33–35).
Previous studies have suggested a positive association between payday loan or similar short-term loans and a range of worse health outcomes such as obesity, high blood pressure, and poor psychological health (36–39). Payday loans provide an expensive form of short-term credit and this debt may degrade an individual’s ability to achieve or maintain health. In our study, the results from GWR models showed that there was a statistically significant positive association between payday loan places and obesity and diabetes in counties in the Midwestern, southeastern and western region. None of the U.S. counties showed a significant inverse association between payday loan centers and adult obesity and diabetes. However, spatial variation was observed in the association between density of payday loan places and prevalence of other health outcomes such as fair or poor health, physical inactivity, physical distress and mental distress.
Study strengths and limitations.
This study used GWR to examine spatial heterogeneities in the relationship between business pattern indicators and adverse health outcomes. The advantage of using GWR over the OLS model is that GWR models allow examining the impact of predictors and geographical location on important health outcomes and produces location-specific estimates. The examination of spatial variation in the association between business pattern indicators and important health outcomes can help to identify high-risk regions for targeted prevention strategies. Our regression models accounted for important potential confounders such as county compositional characteristics and health care resources.
There are some limitations in this study. The GWR models (with all the predictor variables included) explained less than half of the variance in the county-level prevalence of adult obesity, diabetes and physical inactivity in large geographic areas in the Western and Midwestern U.S. This suggests that several factors associated with the county-level prevalence of these health outcomes in these geographic areas were missing from our models. Another limitation of this study is that the data was aggregated at the county level and therefore we cannot make generalizations about individuals or other levels of aggregation. Since the present study was cross-sectional, we cannot make conclusions about causality.
CONCLUSIONS
In this study, we examined the potential impact of type commercial entities in an area on the health outcomes of that area. Results revealed full service restaurants and fitness centers as being associated with reductions in chronic disease burden. On the other hand, density of payday loan centers was found to be associated with an increase in chronic disease burden. Relationships between outcomes and business patterns varied substantially across the U.S. Better understanding of the association between area-level structures and important health outcomes at the local level is important for developing targeted context-specific policy interventions.
Supplementary Material
Research Highlights.
Assessed association between business pattern indicators and chronic health outcomes.
Full service restaurants were associated with reduced chronic disease burden.
Fitness centers were associated with decrease in chronic health outcomes.
Payday loan centers were associated with increase in adverse health outcomes.
ACKNOWLEDGEMENTS
This study was supported the National Institutes of Health’s Big Data to Knowledge Initiative (BD2K) grants 5K01ES025433; R01 LM012849 and the NIH Commons Credit Pilot Program (grant number: CCREQ-2016-03-00003).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Bostic RW, Thornton RL, Rudd EC, Sternthal MJ. Health in all policies: The role of the US Department of Housing and Urban Development and present and future challenges. Health Affairs 2012. August 22;31(9):2130–7. [DOI] [PubMed] [Google Scholar]
- 2.Marmot M, Friel S, Bell R, Houweling TA, Taylor S, Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. The lancet 2008. November 8;372(9650):1661–9. [DOI] [PubMed] [Google Scholar]
- 3.Blas E, Gilson L, Kelly MP, Labonté R, Lapitan J, Muntaner C, Östlin P, Popay J, Sadana R, Sen G, Schrecker T. Addressing social determinants of health inequities: what can the state and civil society do?. The Lancet 2008. November 8;372(9650):1684–9. [DOI] [PubMed] [Google Scholar]
- 4.Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Sorlie P, Szklo M, Tyroler HA, Watson RL. Neighborhood of residence and incidence of coronary heart disease. New England Journal of Medicine 2001. July 12;345(2):99–106. [DOI] [PubMed] [Google Scholar]
- 5.Jia H, Moriarty DG, Kanarek N. County-level social environment determinants of health-related quality of life among US adults: a multilevel analysis. Journal of community health 2009. October 1;34(5):430–9. [DOI] [PubMed] [Google Scholar]
- 6.Black NC. An ecological approach to understanding adult obesity prevalence in the United States: a county-level analysis using geographically weighted regression. Applied Spatial Analysis and Policy 2014. September 1;7(3):283–99. [Google Scholar]
- 7.Yen IH, Kaplan GA. Poverty area residence and changes in physical activity level: evidence from the Alameda County Study. American Journal of Public Health 1998. November;88(11):1709–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross CE. Walking, exercising, and smoking: does neighborhood matter?. Social science & medicine 2000. July 16;51(2):265–74. [DOI] [PubMed] [Google Scholar]
- 9.Morland K, Wing S, Roux AD, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. American journal of preventive medicine 2002. January 1;22(1):23–9. [DOI] [PubMed] [Google Scholar]
- 10.Morland K, Wing S, Roux AD. The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study. American journal of public health 2002. November;92(11):1761–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee RE, Cubbin C. Neighborhood context and youth cardiovascular health behaviors. American Journal of Public Health 2002. March;92(3):428–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehta NK, Chang VW. Weight status and restaurant availability: a multilevel analysis. American journal of preventive medicine 2008. February 1;34(2):127–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diez-Roux AV, Nieto FJ, Caulfield L, Tyroler HA, Watson RL, Szklo M. Neighbourhood differences in diet: the Atherosclerosis Risk in Communities (ARIC) Study. Journal of Epidemiology & Community Health 1999. January 1;53(1):55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hipp JA, Chalise N. Peer reviewed: spatial analysis and correlates of county-level diabetes prevalence, 2009–2010. Preventing chronic disease 2015;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.U.S. Census Bureau County business patterns. 2013. Available from: https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t#none
- 16.Centers for Disease Control and Prevention (CDC). Centers for disease control and prevention diabetes interactive atlas 2014. Available from: http://www.cdc.gov/diabetes/atlas/
- 17.Centers for Disease Control and Prevention (CDC). Behavioral risk factor surveillance system (BRFSS) 2016. Available from: https://www.cdc.gov/brfss/
- 18.Fatality Analaysis Reporting System. 2012. –2016. Available from: https://www.nhtsa.gov/research-data/fatality-analysis-reporting-system-fars
- 19.Andresen EM, Catlin TK, Wyrwich KW, Jackson-Thompson J. Retest reliability of surveillance questions on health related quality of life. Journal of Epidemiology & Community Health 2003. May 1;57(5):339–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jia H, Muennig P, Lubetkin EI, Gold MR. Predicting geographical variations in behavioural risk factors: an analysis of physical and mental healthy days. Journal of Epidemiology & Community Health 2004. February 1;58(2):150–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.U.S. Census Bureau. TIGER/LINE Shapefile 2018. Available from: https://www.census.gov/geo/maps-data/data/tiger-line.html
- 22.American Community Survey 5-year estimates. 2010. –2014. Available from: https://www.census.gov/programs-surveys/acs/data.html
- 23.Team RC. R: A language and environment for statistical computing [Google Scholar]
- 24.Brunsdon C, Fotheringham AS, Charlton ME. Geographically weighted regression: a method for exploring spatial nonstationarity. Geographical analysis 1996. October;28(4):281–98. [Google Scholar]
- 25.O’SULLIVAN DA. Geographically Weighted Regression: The Analysis of Spatially Varying Relationships, by AS Fotheringham, C. Brunsdon, and M. Charlton. Geographical Analysis 2003. July;35(3):272–5. [Google Scholar]
- 26.An R, Li X, Jiang N. Geographical variations in the environmental determinants of physical inactivity among US adults. International journal of environmental research and public health 2017. October 31;14(11):1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haynes-Maslow L, Leone LA. Examining the relationship between the food environment and adult diabetes prevalence by county economic and racial composition: An ecological study. BMC public health 2017. December;17(1):648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salois MJ. Obesity and diabetes, the built environment, and the ‘local’food economy in the United States, 2007. Economics & Human Biology 2012. January 1;10(1):35–42. [DOI] [PubMed] [Google Scholar]
- 29.Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: a geographic analysis. American journal of preventive medicine 2004. October 1;27(3):211–7. [DOI] [PubMed] [Google Scholar]
- 30.Moore LV, Diez Roux AV. Associations of neighborhood characteristics with the location and type of food stores. American journal of public health 2006. February;96(2):325–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Preventive medicine 2007. March 1;44(3):189–95. [DOI] [PubMed] [Google Scholar]
- 32.AlHasan DM, Eberth JM. An ecological analysis of food outlet density and prevalence of type II diabetes in South Carolina counties. BMC public health 2015. December;16(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shah SN, Digenis-Bury E, Russo ET, O’Malley S, Blanding N, McHugh A, Wada R. Nocost gym visits are associated with lower weight and blood pressure among non-Latino black and Latino participants with a diagnosis of hypertension in a multi-site demonstration project. Preventive Medicine Reports 2018. June 1;10:66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roux AV, Evenson KR, McGinn AP, Brown DG, Moore L, Brines S, Jacobs DR Jr. Availability of recreational resources and physical activity in adults. American journal of public health 2007. March;97(3):493–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sallis JF, Hovell MF, Hofstetter CR, Elder JP, Hackley M, Caspersen CJ, Powell KE. Distance between homes and exercise facilities related to frequency of exercise among San Diego residents. Public health reports 1990. March;105(2):179. [PMC free article] [PubMed] [Google Scholar]
- 36.Sweet E, Kuzawa CW, McDade TW. Short-term Lending: Payday Loans as Risk Factors for Anxiety, Inflammation and Poor Health. SSM-Population Health 2018. June 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Münster E, Rüger H, Ochsmann E, Letzel S, Toschke AM. Over-indebtedness as a marker of socioeconomic status and its association with obesity: a cross-sectional study. BMC Public Health 2009. December;9(1):286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pollack CE, Lynch J. Health status of people undergoing foreclosure in the Philadelphia region. American journal of public health 2009. October;99(10):1833–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sweet E, Nandi A, Adam EK, McDade TW. The high price of debt: Household financial debt and its impact on mental and physical health. Social Science & Medicine 2013. August 31;91:94–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Babey SH, Diamant AL, Hastert TA, Harvey S. Designed for disease: the link between local food environments and obesity and diabetes [Google Scholar]
- 41.Ahern M, Brown C, Dukas S. A national study of the association between food environments and countylevel health outcomes. The Journal of Rural Health 2011. September;27(4):367–79. [DOI] [PubMed] [Google Scholar]
- 42.Pitts SB, Edwards MB, Moore JB, Shores KA, DuBose KD, McGranahan D. Obesity is inversely associated with natural amenities and recreation facilities per capita. Journal of physical activity and health 2013. September;10(7):1032–8. [DOI] [PubMed] [Google Scholar]
- 43.Acharya BK, Cao C, Lakes T, Chen W, Naeem S, Pandit S. Modeling the spatially varying risk factors of dengue fever in Jhapa district, Nepal, using the semi-parametric geographically weighted regression model. International journal of biometeorology 2018. November 1;62(11):1973–86. [DOI] [PubMed] [Google Scholar]
- 44.Corner RJ, Dewan AM, Hashizume M. Modelling typhoid risk in Dhaka Metropolitan Area of Bangladesh: the role of socio-economic and environmental factors. International journal of health geographics 2013. December;12(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.O’brien RM. A caution regarding rules of thumb for variance inflation factors. Quality & quantity 2007. October 1;41(5):673–90. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.