Abstract
Objective:
Transfer of congenital heart disease care from the pediatric to adult setting has been identified as a priority and is associated with better outcomes. Our objective is to determine what percentage of patients with congenital heart disease transferred to adult congenital cardiac care.
Design:
A retrospective cohort study.
Setting:
Referrals to a tertiary referral center for adult congenital heart disease patients from its pediatric referral base.
Patients:
This resulted in 1,514 patients age 16–30, seen at least once in three pediatric Georgia healthcare systems during 2008–2010.
Interventions:
We analyzed for protective factors associated with age-appropriate care, including distance from referral center, age, timing of transfer, gender, severity of adult congenital heart disease and comorbidities.
Outcome Measures:
We analyzed initial care by age among patients under pediatric care from 2008–2010 and if patients under pediatric care subsequently transferred to an adult congenital cardiologist in this separate pediatric and adult health system during 2008–2015.
Results:
Among 1,514 initial patients (39% severe complexity), 24% were beyond the recommended transfer age of 21 years. Overall, only 12.1% transferred care to the referral affiliated adult hospital. 90% of these adults that successfully transferred were seen by an adult congenital cardiologist, with an average of 33.9 months between last pediatric visit and first adult visit. Distance to referral center contributed to delayed transfer to adult care. Those with severe congenital heart disease were more likely to transfer (18.7% vs. 6.2% for not severe).
Conclusion:
Patients with severe disease are more likely to transfer to adult congenital heart disease care than non-severe disease. Most congenital heart disease patients do not transfer to adult congenital cardiology care with distance to referral center being a contributing factor. Both pediatric and adult care providers need to understand and address barriers in order to improve successful transfer.
Keywords: Transfer of Care, Transition, Adult Congenital Heart Disease
Introduction
Advances in pediatric cardiology and congenital heart surgery have allowed more individuals born with congenital heart disease (CHD) to live into adulthood. Adults patients with CHD now outnumber pediatric CHD patients.1 In the last few decades, the complexity of the adult congenital heart disease (ACHD) population has continued to the increase1,2 emphasizing the urgency of providing suitable and accessible ACHD care.
Adolescents with chronic disease should start transition education at age 12 years, and finally transfer to an appropriate adult provider by age 21.3 American College of Cardiology (ACC) and American Heart Association (AHA) guidelines recommend that complex ACHD patients see an ACHD cardiologist. All other patients with CHD should be managed with consultation or in conjunction with an ACHD cardiologist.4 In Canada, ACHD referral centers improved survival for patients.5 Multiple studies have shown improved surgical outcomes with congenital heart surgeons.6,7,8 In a large single center study, ACHD cardiologists complied with guidelines more often than pediatric or adult cardiologists without congenital training.9 Now, there is a shift to formalize training of ACHD physicians and accredit ACHD centers in the United States.10, 11
Multiple studies have shown significant gaps in care after patients leave their pediatric providers. Attrition from cardiology care can start in early childhood prior to the recommended transition planning or transfer to adult congenital cardiology care.12 Much of the literature on barriers to successful transfer of care is based on unvalidated surveys of patients and providers. In the United States, successful ACHD programs have been built at both pediatric and adult institutions. Different ACHD care settings may have specific barriers to transfer of care for their ACHD population.13 The current study evaluates inter-institutional transfer between a separate pediatric and adult hospital system that, since 2004, has made a concerted effort to transfer care of all soon-to-be ACHD patients into the adult system.14 The aim of this study is to identify factors associated with transfer from pediatric cardiology to adult congenital cardiology.
Methods
Study Population
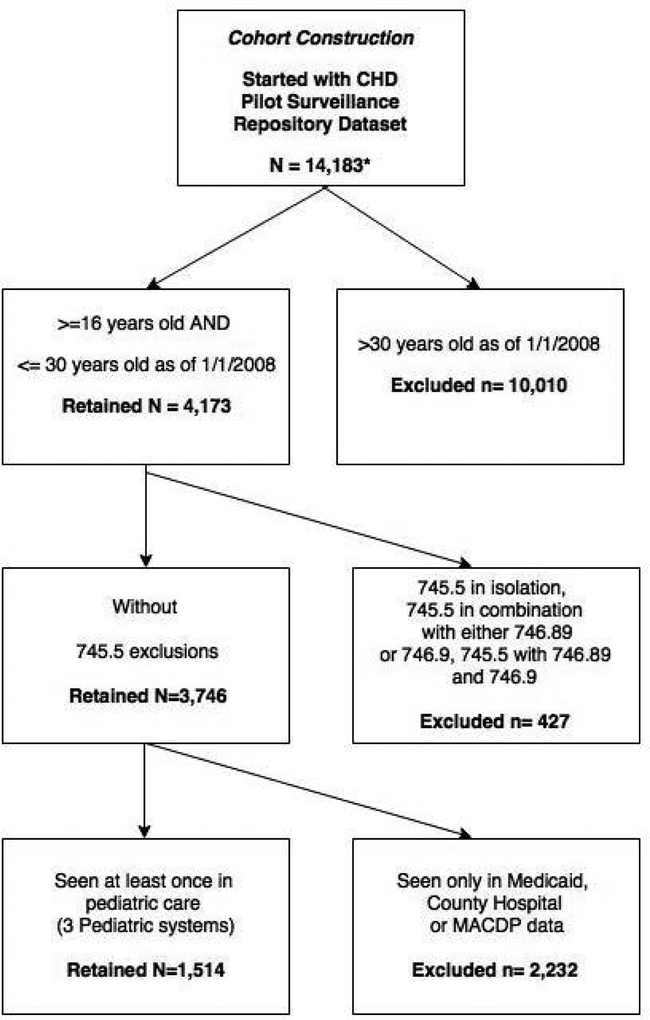
Emory University Institutional Review Board (IRB) approved this retrospective cohort study. Figure 1 illustrates the cohort construction of 1,514 adolescent and young adult CHD patients in this analysis who were between the ages of 16–30 during 2008–2010 and initially seen in a pediatric cardiology office. Data were obtained from a pilot project conducted by Emory University in collaboration with the Centers for Disease Control and Prevention (CDC) to develop a population-based surveillance system of adolescents and adults with CHD in the state of Georgia with primary focus on the five metropolitan Atlanta counties (Clayton, Cobb, DeKalb, Fulton, and Gwinnett). The pilot study included cases who had an encounter at least once from January 1, 2008-December 31, 2010 with a CHD diagnostic code. These included International Classification of Disease version 9.0 Clinical Modification (ICD-9-CM) codes 745.xx – 747.xx, excluding: congenital heart block (746.86), pulmonary arteriovenous malformations (747.32), absent/hypoplastic umbilical artery (747.5), other anomalies of peripheral vascular system (747.6×), and other specified anomalies of circulatory system (747.8×). The study excluded ICD-9-CM codes for prior heart transplant and isolated congenital hypertrophic cardiomyopathy. The pilot study identified a total of 14,183 CHD patients who met the case definition. Glidewell et al. explain the methodology of the pilot study.15 CHD codes were categorized into five groups similar to Marelli et al.16 which integrates both severity and anatomy: severe, shunts, shunts plus valve, valve, and other CHD. The modified Marelli classification accounts for ICD-9-CM codes and simplifies this classification to severe and not severe as described by Glidewell et al.15 Severe CHD was defined as a CHD usually requiring surgical or catheter intervention within the first year of life. The remaining codes were combined and classified as “not severe” for pilot study.
Figure 1:
Inclusion and exclusion criteria for study cohort.
The clinical sources for included a large multi-hospital tertiary referral pediatric system, a large academic referral healthcare system, state Medicaid data, and a county hospital system. Supplemental information came from state vital records, and a birth defect registry. Demographics, diagnostic and procedural codes, and death information were linked into a common, de-identified analytic dataset. Protected Health Information (PHI) were removed and replaced with non-identifiable IDs to maintain confidentiality and only these de-identified datasets were used for analysis.
Our study limited the initial cohort construction to 1,514 CHD patients between the ages of 16–30 initially that were seen at least once in a Georgia pediatric cardiology practice in 2008–2010. Our study included a majority of pediatric cardiologists in Georgia and The Emory Healthcare system. The initial cohort age range was chosen as the age range that, in our Georgia healthcare system, would be expected to transfer to adult care from pediatric care over the following 3–6 years of available data. Individuals with an isolated atrial septal defect or patent foramen (745.5 in isolation or in combination with 746.89 and/or 746.9) were excluded due to high false identification of cases with this code.17 Baseline 2008–2010 initial cohort demographics are shown in Table 1. These individuals were followed by record linkage from 2011 to 2016 to see if they transferred into adult care at Emory Healthcare and Emory St. Joseph’s Hospital (Figure 1). Provider specialty data was provided in the data sets used to create the linked database. The locations of the pediatric cardiology clinic and adult congenital cardiology clinics are shown in Figure 2. Follow up types of encounters captured included inpatient, outpatient, and emergency room encounters.
Table 1.
Demographics by age group of the initial cohort seen in pediatric cardiology clinics.
| AGE GROUPING (N=1,514) | |||||
|---|---|---|---|---|---|
|
16–17 n=571 (37.7%) |
18–21 n=586 (38.7%) |
22–25 n=187 (12.4%) |
26–30 n=170 (11.2%) |
X2 | |
| GENDER | |||||
| Female | 264 (46.2%) | 315 (53.8%) | 150 (80.2%) | 160 (94.1%) | 166.2, df=3, p<.0001 |
| INSURANCE | |||||
| Private | 425 (74.4%) | 405 (69.1%) | 112 (59.9%) | 127 (74.7%) | 37.6,
df=9, p<.0001 |
| Public | 133 (23.3%) | 148 (25.3%) | 55 (29.4%) | 31 (18.2%) | |
| None | 0 (0.0%) | 7 (1.2%) | 1 (0.5%) | 1 (0.6%) | |
| Other Unknown | 13 (2.3%) | 26 (4.4%) | 19 (10.2%) | 11 (6.5% | |
| SEVERITY OF CHD | |||||
| Not Severe | 413 (72.3%) | 365 (62.3%) | 80 (42.8%) | 68 (40.0%) | 88.9,
df=3, p<.0001 |
| Severe | 158 (27.7%) | 221 (37.7%) | 107 (57.2%) | 102 (60.0%) | |
| COMORBIDITIES | |||||
| Hypertension | 18 (3.2%) | 24 (4.1%) | 7 (3.7%) | 2 (1.2%) | ns |
| Coronary artery disease | 4 (0.7%) | 18 (3.1%) | 4 (2.1%) | 2 (1.2%) | 9.5, df=3, p<.05 |
| Diabetes Mellitus | 3 (0.5%) | 7 (1.2%) | 2 (1.1%) | 1 (0.6%) | ns |
| Non CHD Birth Defects | 54 (9.5%) | 71(12.1%) | 19 (10.2%) | 13 (7.7%) | ns |
| Mental Health | 17 (3.0%) | 29 (5.0%) | 5 (2.7%) | 7 (4.1%) | ns |
| Neuro | 10 (1.8%) | 16 (2.7%) | 1 (0.5%) | 2 (1.2%) | ns |
| HOME / 5 COUNTY STATUS | |||||
| Within 5 Metro-Atlanta |
244 (42.7%) | 260 (44.4%) | 6 (33.7%) | 78 (45.9%) | 13.0,
df=6, p<.05 |
| Outside 5 Metro-Atlanta |
296 (51.8%) | 300 (51.2%) | 111 (59.4%) | 77 (45.3%) | |
| Unknown | 31 (5.4%) | 26 (4.4%) | 13 (6.9%) | 15 (8.8%) | |
| PREGNANCY | |||||
| Pregnant | 8 (1.4%) | 19 (3.2%) | 10 (5.4%) | 10 (5.9%) | 13.0, df=3, p< .01 |
| Fetal Echo
(CPT:76825, 76827, 93325) |
8 (1.4%) | 16 (2.7%) | 10 (5.4%) | 6 (3.5%) | 9.3, df=3, p<.05 |
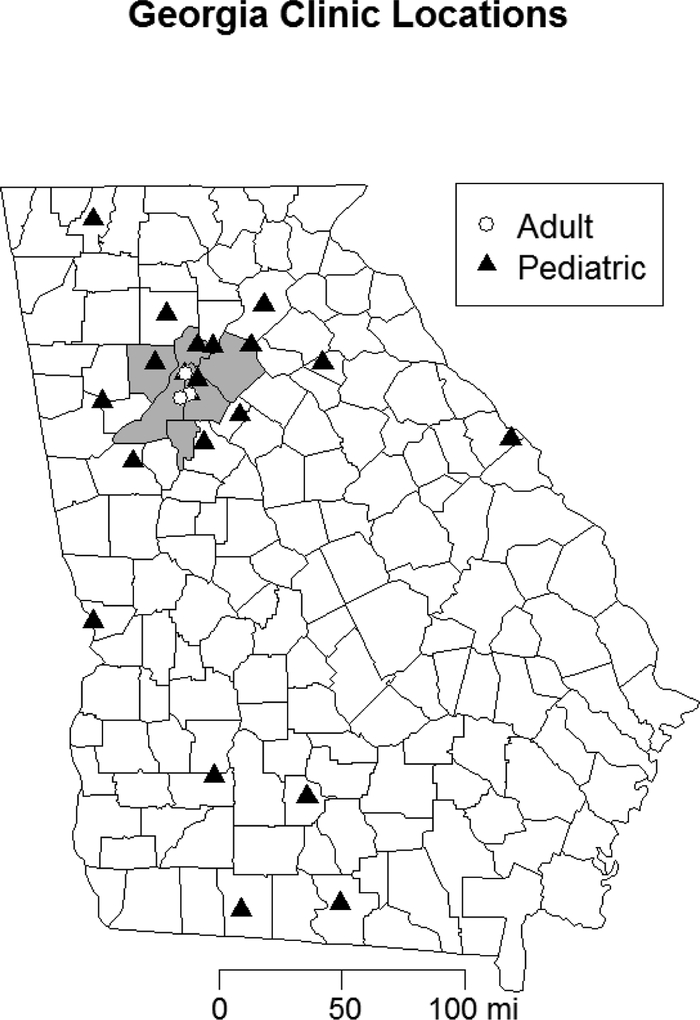
Figure 2:
Locations of the studied pediatric cardiology clinics and adult congenital cardiology clinics in Georgia.
Outcomes:
Outcomes included whether CHD patients transferred to an ACHD cardiologist during 2008–2015 and the number of clinic visits made to the ACHD clinic between 2011 to 2016. Emory Healthcare and St. Joseph Hospital data contained provider information. The provider specialty was confirmed searching www.emoryhealthcare.org and www.doximity.com. The Medicaid and county hospital system data were excluded from this analysis since encounter data was only available for 2008–2010.
Statistical Analysis:
Data analysis was conducted using SAS software, version 9.4 for Windows. Frequencies for all categorical variables for the pediatric healthcare cohort by age group were computed and chi square analyses were conducted. Bivariate analysis by type of transition outcome used chi-square analysis to test the differences in demographic characteristics for CHD patients who appropriately transferred to an ACHD provider and those who transferred to a non-ACHD provider.
Results
Initial cohort - Patients aged 16 years and older seen in pediatric cardiology clinics
Among 1,514 patients aged 16–30 years seen in pediatric cardiology at index encounter, most (61%) had not severe complexity congenital heart disease. There was a decrease in the number of patients seen after 21 years old in the pediatric system and only 24% were beyond the recommended transfer age of 21 years (Table 1). There are significant differences in baseline characteristics by age for gender, home location, insurance type and severity of disease (Table 1). Patients who were retained in pediatric care after reaching age 21 were predominantly women (80.2% in the 22–25-year-old age range, 94.1% in the 26–30 age range) with greater disease severity (57.2%−60.0%, respectively). The 22–25-year-old group had the highest percent (59.4%) of patients residing outside the five metropolitan-Atlanta counties.
Transferred patients and ACHD patients seen in ACHD Center
Only 12.1% (183/1,514) transferred into the Emory Healthcare system and 11.0% (167/1514) to an ACHD cardiologist (Table 2). When assessed by age, the percent who transferred to the Emory Healthcare system was 6.5% (37), 18.4% (108), 13.9% (26) and 7.1% (12) for the initial age groups 16–17, 18–21, 22–25 and 26–30, respectively (X2 = 43.71, df =3, p<0.0001). Among those who transferred to the adult system, 91.3% (167/183) transferred to an ACHD cardiologist at Emory. The average transfer time between last pediatric visit and first ACHD visit was 33.9 months. 18.7% (110/588) of patients with severe CHD transferred adult congenital cardiology care compared to 6.2% (57/926) of patients with non-severe CHD patients.
Table 2.
Characteristics of transfer group.
| TRANSFER GROUPING* (N=183) | |||
|---|---|---|---|
| Appropriate ACHD Transfer (n=167, 91.3%) |
Transferred, but not to ACHD (n=16, 8.7%) |
X2 | |
| GENDER | |||
| Female | 88 (52.7%) | 8 (50.0%) | ns |
| AGE | |||
| 16–17 | 31 (18.6%) | 6 (37.5%) | ns |
| 18–21 | 101 (60.5%) | 7 (43.8%) | |
| 22–25 | 25 (14.9%) | 1 (6.25%) | |
| 26–30 | 10 (5.9%) | 2 (12.5%) | |
| INSURANCE | |||
| Private | 88 (52.7%) | 8 (50.0%) | ns |
| Public | 72 (43.1%) | 7 (43.8%) | |
| None | 1 (0.6%) | 0 (0.0%) | |
| Other/Unknown | 6 (3.6%) | 1 (6.3%) | |
| SEVERITY OF CHD | |||
| Not Severe | 57 (34.1%) | 13 (81.2%) | 13.7, df=1, p<.001 |
| Severe | 110 (65.9%) | 3 (18.8%) | |
| COMORBIDITIES | |||
| Hypertension | 31 (18.6%) | 1 (6.2%) | ns |
| Coronary artery disease | 23 (13.8%) | 0 (0.0%) | ns |
| Diabetes mellitus | 6 (3.6%) | 0 (0.0%) | ns |
| Non-CHD Birth Defects |
44 (26.4%) | 1 (6.2%) | ns |
| Mental Health | 32 (19.2%) | 3 (18.8%) | ns |
| Neuro | 11 (6.6%) | 0 (0.0%) | ns |
| HOME / 5 COUNTY STATUS | |||
| Within 5 Metro-Atlanta |
74 (44.3%) | 10 (62.5%) | ns |
| Outside 5 Metro-Atlanta |
93 (55.7%) | 6 (37.5%) | |
| Unknown | -- | -- | |
| PREGNANCY | |||
| Pregnancy | 23 (13.8%) | 3 (18.8%) | ns |
| Fetal Echo (CPT: 76825, 76827, 93325) |
16 (9.6%) | 3 (18.8%) | ns |
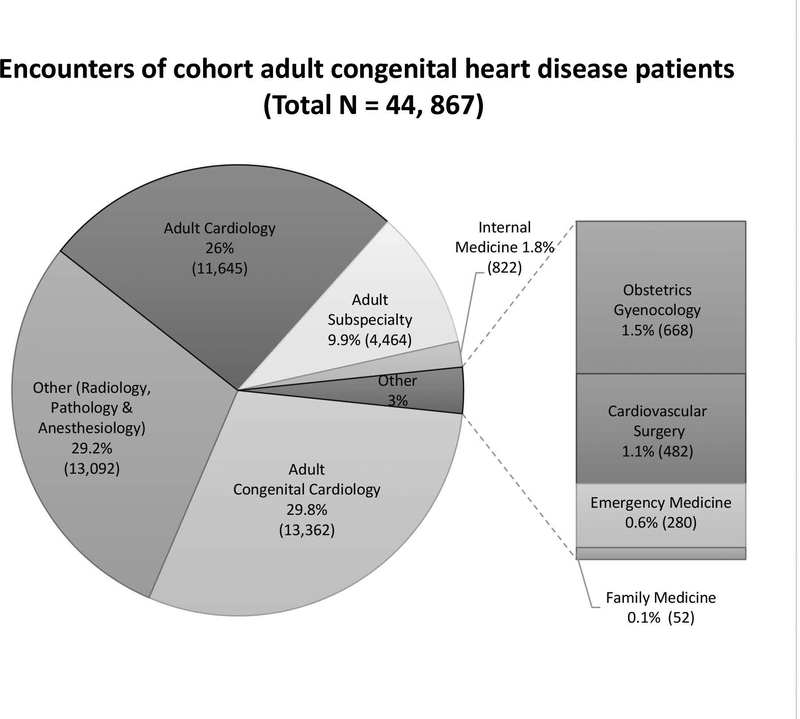
Adult subspecialty interaction with ACHD patients by 2016
The Figure 3 shows that multiple adult subspecialties interact with ACHD patients within the adult healthcare system and less than 1/3 (29.8%) of all encounters were with an ACHD physician. Most non-ACHD encounters represented other subspecialties like anesthesiology, radiology and pathology (29.2%), adult cardiology (26%), and other adult subspecialty (9.2%). Internal medicine, obstetrics and gynecology, cardiovascular surgery, emergency department and family medicine each represented less than 2% of encounters.
Figure 3:
Adult subspecialties encounters with ACHD patients within the adult healthcare system.
Discussion
Initial cohort - Patients aged 16 years and older seen in pediatric cardiology clinics
In the healthcare system studied, ACHD patients transfer from pediatric based care to an adult hospital and clinic setting began more than 10 years ago due to pediatric hospital overcrowding and lack of adult multispecialty care in the pediatric setting.14 The goal was to transfer patients to the adult healthcare system when they reached between 18 and 21 years old. Less than 25 percent of patients aged 16 or older seen in pediatric cardiology care from 2008–2010 were aged 22 years or older (Table 1). Although retention of ACHD patients in the pediatric health system is low, results suggest additional work is needed to help young adults stay in care.
Patients were more likely to be retained in a pediatric setting if they were women or if they were seen outside of the five-county metropolitan-Atlanta area. The pediatric practices consisted of 21 practices across the state of Georgia (Figure 2), whereas there is only one ACHD center in Georgia in the Atlanta area, which may contribute to those outside the metro area being more likely to remain in pediatric care. The counties outside the five metropolitan-Atlanta counties had a significantly higher percentage of 22–25 year-olds (Table 1). In previous population studies, women have been shown to stay longer in health care.12 One theory for the higher retention among woman in health care is insurance coverage around a pregnancy. However, most of the women who remained in pediatric care did not have a corresponding billing code for a pregnancy or a fetal echocardiogram. Among adults who successfully transferred to the ACHD clinic, 52% of them were women (Table 2).
Transferred patients and ACHD patients seen in ACHD Center by 2016
Although high retention within the pediatric health system was not seen after 21 years old (24%), there was a low percent (12%) of patients who transferred to our adult healthcare system by 2016 (Table 2). Once patients reached the adult Emory Healthcare System, over 90% of those patients transferred to ACHD care (Table 2). The patients who transferred from pediatrics to ACHD care did so by age 21 years, but the average time revealed an average gap in care of almost three years. In the current study, those with severe CHD severity were more likely to stay in CHD care (Table 1–2), and this finding is consistent with current literature.13 Although severity of disease was a protective factor, most patients with severe disease (81%) still did not transfer to ACHD care during the study time frame.
One possible reason for the low transfer rate may be some patients may have relocated to another state. Many others have remained in Georgia, but may be seen in another local adult health care systems or by adult cardiology without ACHD training outside of the Emory Healthcare System. Another reason for failure of successful transfer to the ACHD center may be related to insurance access. Georgia has one of the highest uninsured rates in the United Studies (13–19%).18 Although less than 1% of those who successfully transferred to the ACHD center were uninsured, the percent of uninsured individuals in Georgia was high during the study period; 18.8%, 15.8%, 13.9% and 12.9% in 2013, 2014, 2015, and 2016, respectively. Georgia is one of the states that did not expand Medicaid18 and many pediatric patients who were covered by Medicaid and the Children’s Health Insurance Program (CHIP) lose access to this insurance at 18 years of age. Oregon Health and Science University’s ACHD program, which also has an inter-institutional transfer of care model, reported a transfer rate of 34%, but also reported a high retention rate in pediatric cardiology care of 31%.19 Unlike Georgia, Oregon has a lower uninsured population.18 Even though the Emory center has a charity care program and a social worker to help with the process, new referrals may not be aware of all available resources, and these resources can be challenging to access.
Structural barriers include lack of insurance, lack of reimbursement for transition visits and inter-institutional transfer.20, 21 Institutional barriers may include lack of a formal transition program, lack of ACHD providers, or unavailability of primary care physicians comfortable caring for ACHD patients. Other institutional barriers are related to the complexity of health care navigation or institutional age limits.21 Patients graduating from the pediatric system and their families may find it difficult to navigate the healthcare system with these barriers. Transferring from one healthcare system to another can lead to an increase in structural and institutional barriers for successful transfer of care.13
Similar to other studies,12 many patients are lost to care prior to the time of transfer into the adult system and do not participate in the formal transition program. Although a formal transition program is in place, it targets patients and families already engaged in this process. The goal of Emory’s quality improvement (QI) projects over the last three years was to keep pediatric and adult patients in care, and facilitate transfer of care for the adult patients. Projects included a student-led public health initiative to ensure continued care for established ACHD patients, an electronic medical record (EMR) improvement to identify pediatric patients with gaps in care, and hiring of an ACHD nurse navigator to facilitate new patient visits. Although the quality improvement projects were not the goal of this study, these projects may reduce gaps in care and improve transfer rates to lifelong adult congenital heart disease care by reducing structural and intuitional barriers of a two-hospital system.
The pediatric cardiology practice that refers to Emory adult congenital heart center (ACHC) provides care to the majority of children with CHD in Georgia and has a wide geographic coverage; the Emory ACHC is located within the Atlanta metropolitan area and is the only adult congenital heart program in Georgia. (Figure 2). The center has a limited outreach outside the five-county metro-Atlanta area which may explain why there is an older population within the pediatric outreach centers. Services such as telemedicine and expansion of outreach may improve access to ACHD care for remote locations.
Adult subspecialty interaction with ACHD patients
Many adult care providers do not realize that ACHD patients need to return to adult congenital cardiology care. Outreach to outside adult healthcare systems is needed to encourage patients to return to ACHD care since specialty care has been shown to improve survival especially in patients with severe CHD.5 That this could be an effective intervention is reflected in a survey of ACHD patients returning to referral centers. Many reported that they returned to care on the recommendation from a health care provider.22 The current study shows that ACHD patients interacted with many non-ACHD adult subspecialties within the Emory Healthcare system (Figure 3). This is in line with other studies.9,12 Many patients were seen by both an ACHD cardiologist and another cardiology subspecialist including heart failure, electrophysiology or interventional. The study did not estimate the number of patients seen by adult cardiologists without congenital expertise outside of the adult Emory Healthcare system. Very few patients were seen by general internal medicine and family medicine within the Emory Healthcare system. The study was unable to determine the role of primary care access as a factor in transfer of care. Outreach to internal medicine physicians and trainees to encourage them to refer complex patients may also ease their increasing discomfort treating young adults with chronic disease due to a self-perception of lack of training and lack of exposure to these diseases.22,23,24
Limitations
This was a single center retrospective study. Our congenital heart program has separate pediatric and adult systems; the obstacles in transition and transfer of care may be different than other centers where the ACHD program is housed in the pediatric center. Only access to the database for one large multi-center and multi-specialty adult healthcare system for the full period of the study was achieved. This study cannot account for patients that moved to a different state during the study. The number of patients being cared for in adult healthcare systems in the community is unknown, as is the number of patients lost to all health care.
Medicaid claims data and data from county health system acquired from the original pilot data set were excluded since provider information was absent and data after 2010 were not available. Thus, an analysis of other non-ACHD center sites where ACHD patients are receiving non-ACHD specialty care in the community was not possible. In the future, evaluating other adult healthcare systems including the county healthcare system may answer the question if these patients are seeking care elsewhere or are lost to all healthcare.
Conclusions
Most ACHD patients do not remain in pediatric cardiology care after 21 years old, but a large majority also do not transfer to ACHD care. Gender, CHD severity, insurance and distance to the referral center all affect the rate of transfer. However, intensive outreach efforts to primary care, pediatric, and adult cardiology in order to keep patients in healthcare may reduce the structural and institutional barriers that can occur during transfer from pediatric healthcare to ACHD healthcare. The benefit of interventions including improved access to outreach clinics, EMR identification of patients with gaps in care and nurse navigators to simplify the transfer process merit further investigation.
Funding:
Dr. Book receives Funding/Support: Centers for Disease Control and Prevention, Grant/Award Number: CDC‐RFA‐DD15-1506
National Institutes of Health, National Heart Lung and Blood Institute, 35860
Footnotes
Conflict of Interest: None of the authors have any conflict of interest.
References:
- 1.Marelli AJ, Ionescu-Ittu R, Mackie AS, Guo L, Dendukuri N and Kaouache M. Lifetime prevalence of congenital heart disease in the general population from 2000 to 2010. Circulation. 2014; 130 (9):749–56. [DOI] [PubMed] [Google Scholar]
- 2.Tutarel O, Kempny A, Alonso-Gonzalez R et al. Congenital heart disease beyond the age of 60: emergence of a new population with high resource utilization, high morbidity, and high mortality. Eur Heart J. 2014; 35(11): 725–32. [DOI] [PubMed] [Google Scholar]
- 3.Sable C, Foster E, Uzark K et al. Best practices in managing transition to adulthood for adolescents with congenital heart disease: the transition process and medical and psychosocial issues: a scientific statement from the American Heart Association. Circulation. 2011; 123(13): 1454–85. [DOI] [PubMed] [Google Scholar]
- 4.Stout KK, Daniels CJ, Aboulhosn JA et al. 2018 AHA/ACC Guideline for the management of adults with congenital heart disease: Executive summary. Circulation. 2018. August 16 (Epub). [DOI] [PubMed] [Google Scholar]
- 5.Mylotte D, Pilote L, Ionescu-Ittu R et al. Specialized adult congenital heart disease care: the impact of policy on mortality. Circulation. 2014; 129(18): 1804–12. [DOI] [PubMed] [Google Scholar]
- 6.Karamlou T, Diggs BS, Person T, Ungerleider RM and Welke KF. National practice patterns for management of adult congenital heart disease: operation by pediatric heart surgeons decreases in-hospital death. Circulation. 2008; 118 (23): 2345–52. [DOI] [PubMed] [Google Scholar]
- 7.Mori M, Vega D, Book W and Kogon BE. Heart transplantation with congenital heart disease: 100% survival with operations performed by a surgeon specializing in congenital heart disease in an adult hospital. Ann Thorac Surg. 2015; 99(6): 2173–8. [DOI] [PubMed] [Google Scholar]
- 8.Kogon BE, Plattner C, Leong T et al. Adult congenital heart surgery: adult or pediatric facility? Adult or pediatric surgeon? Ann Thorac Surg. 2009; 87(3): 833–40. [DOI] [PubMed] [Google Scholar]
- 9.Gerardin JF, Menk JS, Pyles LA, Martin CM and Lohr JL. Compliance with adult congenital heart disease guidelines: Are we following the recommendations? Congenit Heart Dis. 2016; 11(3): 245–53. [DOI] [PubMed] [Google Scholar]
- 10.http://www.abim.org/~/media/ABIM%20Public/Files/pdf/publications/certification-guides/policies-and-procedures.pdf Accessed October 11 2017.
- 11.https://www.achaheart.org/provider-support/accreditation-program/ Accessed October 11, 2017.
- 12.Mackie AS, Ionescu-Ittu R, Therrien J, Pilote L, Abrahamowicz M and Marelli A. Children and adults with congenital heart disease lost to follow up: Who and when? Circulation. 2009; 120 (4): 302–9. [DOI] [PubMed] [Google Scholar]
- 13.Everitt IK, Gerardin JF, Rodriguez FH and Book WM. Improving the quality of transition and transfer of care in young adults with congenital heart disease. Congenit Heart Dis. 2017; 12: 242–50. [DOI] [PubMed] [Google Scholar]
- 14.Kogon B, Rosenblum J, Alsoufi B, Shashidharan S and Book W. The evolution of an adult congenital heart surgery program: The Emory System. Semin Thorac Cardiovasc Surg Pediatr Card Surg Ann. 2017. January; 20: 28–32. [DOI] [PubMed] [Google Scholar]
- 15.Glidewell J, Book W, Raskind-Hood C et al. Population-based surveillance of congenital heart defects among adolescents and adults: surveillance methodology. Birth Defects Research. 2018. November 15; 110(19):1395–1403. Epub 2018 Nov 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marelli AJ, Mackie AS, Ionescu-Ittu R, Rahme E and Pilote L. Congenital Heart disease in the general population: changing prevalence and age distribution. Circulation. 2007. January 16; 115(2): 163–72. [DOI] [PubMed] [Google Scholar]
- 17.Glidewell J, Book W, Raskind-Hood C et al. Population-based surveillance of congenital heart defects among adolescents and adults: surveillance methodology. Birth Defects Research. 2018. November 15; 110(19):1395–1403. Epub 2018 Nov 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rodriguez FH, Ephrem G, Gerardin JF, Raskind-Hood C, Hogue C and Book W. The 745.5 issue in code-based, adult congenital heart disease population studies: Relevance to current and future ICD-9-CM and ICD-10-CM studies. Congenit Heart Dis. 2018. January; 13(1): 59–64. [DOI] [PubMed] [Google Scholar]
- 19.https://www.census.gov/content/dam/Census/library/publications/2017/demo/p60-260.pdf Accessed October 11 2017.
- 20.Bohun CM, Woods P, Winter C et al. Challenges of intra-intuitional transfer of care from paediatric to adult congenital cardiology: the need for retention as well as transition. Cardiol Young. 2016. February; 26(2): 327–33. [DOI] [PubMed] [Google Scholar]
- 21.Fortuna RJ, Halterman JS, Pulcino T, Robbins BW. Delayed transition of care: a national study of visits to pediatricians by young adults. Acad Pediatr. 2012;12(5):405–11. [DOI] [PubMed] [Google Scholar]
- 22.Okumura MJ, Kerr EA, Cabana MD, Davis MM, Demonner S, Heisler M. Physician views on barriers to primary care for young adults with childhood-onset chronic disease. Pediatrics. 2010;125(4): e748–e754. [DOI] [PubMed] [Google Scholar]
- 23.Gurvitz M, Valente AM, Broberg C et al. Prevalence and predictors of gaps in care among adult congenital heart disease patients: HEART-ACHD (the Health, Education and Access Research Trial). J Am Coll Cardiol. 2013; 61(21): 2180–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peter NG, Forke CM, Ginsburg KR and Schwarz DF. Transition from pediatric to adult care: internists’ perspectives. Pediatrics. 2009; 123(2): 417–23. [DOI] [PubMed] [Google Scholar]
- 25.Patel MS and O’Hare K. Residency training in transition of youth with childhood-onset chronic disease. Pediatrics. 2010; 126: S190–3. [DOI] [PubMed] [Google Scholar]