Abstract
Background
We previously reported cryobiopsy (Cryo) with endobronchial ultrasonography-guide sheath (EBUS-GS) for peripheral pulmonary lesions (PPLs) provides significantly larger tissues than transbronchial biopsy (TBB) and provides high quantity and quality DNA for gene analysis by next generation sequencing. However, the tumor cell yields and programmed death ligand 1 (PD-L1) expression between each approach have not been compared. Here, we assessed the tumor cell numbers and PD-L1 expression for Cryo with EBUS-GS for PPLs and TBB in patients with lung cancer.
Methods
Sixteen patients were enrolled in this prospective study from June to November 2017 at Tokyo Women’s Medical University Hospital. The number of tumor cells from a single biopsy, total number of tumor cells, average number of tumor cells, and 22C3 PD-L1 expression (≥ 50% and ≥ 1%) were compared between Cryo and TBB.
Results
The numbers of tumor cells from a single biopsy, total numbers of tumor cells, and average numbers of tumor cells obtained by Cryo were significantly larger than those obtained by TBB (Cryo [means ± standard errors of the means]: 1321 ± 303.7, 1981 ± 411.7, and 1406 ± 310.3; TBB: 208.8 ± 38.24, 1044 ± 189.0, and 208.8 ± 37.81; P < 0.0001, P = 0.0474, P = 0.0006, respectively). PD-L1 ≥ 50% and ≥ 1% patients for Cryo were 18.8 and 56.3%, respectively, whereas those for TBB were 12.5 and 37.5%, respectively. The sensitivity, specificity, positive predictive value, negative predictive value, concordance, and κ coefficient based on Cryo for TBB were 66.7, 100, 100, 92.9, 93.8%, and 0.7647, respectively, for PD-L1 ≥ 50%; and 44.4, 71.4, 66.7, 50, 56.3%, and 0.1515, respectively, for PD-L1 ≥ 1%.
Conclusion
Cryo with EBUS-GS may be a useful diagnostic approach for lung cancer, with advantages over TBB for gene analysis and whole exon sequencing. Particularly, it could contribute to patients taking pembrolizumab as first-line therapy when PD-L1 was negative by evaluating TBB specimens. It could also provide ample tissue for PD-L1 expression analysis in addition to accurate diagnosis and gene analysis.
Keywords: Cryobiopsy, The number of tumor cells, Programmed death ligand 1 expression, Endobronchial ultrasonography-guide sheath, Peripheral pulmonary lesions
Background
Lung cancer is the most prevalent cause of cancer-related death worldwide. Peripheral pulmonary lesions (PPLs) suspicious for lung cancer have been detected at high frequency following the increased utilization of computed tomography (CT) of the chest. The 3rd edition of the American College of Chest Physicians guidelines recommends using endobronchial ultrasonography (EBUS) for PPLs [1]. Transbronchial biopsy (TBB), transbronchial needle aspiration, and brushing with EBUS-guide sheath (EBUS-GS) have been recognized as useful strategies for the diagnosis of PPLs [2–9]. In addition to diagnostic applications, it is also recommended to validate the programmed death ligand 1 (PD-L1) expression [10, 11] and maximize the volume of tissue for phenotyping and genotyping [12]. However, tissues from PPLs obtained by conventional biopsy are generally small [13]. Therefore, cryobiopsy (Cryo) with EBUS-GS may be a useful tool for overcoming this problem. Cryo with EBUS-GS has been shown to be a safe and useful tool for PPLs suspicious of lung cancer [14, 15]. We previously reported that Cryo with EBUS-GS yields significantly larger tissues than TBB and provides high quantity and quality DNA for gene analysis by next generation sequencing. Furthermore, Cryo with EBUS-GS provides a high concordance between rapid on-site evaluation and the final diagnosis [14]. However, comparisons of tumor cell numbers and PD-L1 expression in tissues obtained between Cryo and TBB have been unknown. Because Cryo with EBUS-GS yields larger tissues than TBB, we hypothesized that Cryo with EBUS-GS may be able to have more tumor cells and may therefore be more suitable for evaluation of PD-L1 expression compared with TBB. Therefore, the purpose of this study was to assess the tumor cell numbers and PD-L1 expression obtained by Cryo and TBB.
Methods
Ethical considerations
This was a prospective study approved by the Institutional Review Board of Tokyo Women’s Medical University Hospital (date of approval: April 19, 2017; approval number: 170404). Informed consent was obtained from all patients before enrollment in this study.
Patient population and study design
The eligibility criteria and exclusion criteria were as previously described [14]. Eligible patients were over 20 years old and had PPLs suspicious of lung cancer. Patients were excluded from the study if they showed any of the following features: bleeding predisposition, platelet count < 20,000/mm3, pregnancy, active infection, respiratory insufficiency, lesions less than 2 cm from the pleura, obvious blood vessels adjacent to EBUS over 0.5 cm, and refusal to participate in the study [14]. In total, 23 patients underwent Cryo with EBUS-GS at Tokyo Women’s Medical University Hospital, and 16 patients who were given a diagnosis by biopsy were enrolled in this study.
PPLs were defined as abnormal and solid shadows in the pulmonary parenchyma, which were not identified with bronchoscopy [14, 16], and ground glass nodules were excluded. All PPLs were identified with CT or 18F-fluorodeoxy glucose-positron emission tomography prior to Cryo with EBUS-GS [14]. The lesion size was measured at the largest diameter [14]. Each patient was underwent brushing, TBB, and Cryo in this series.
Procedures
The procedures used in this study were described previously [14]. A flexible fiber bronchoscope (BF-1TQ290; Olympus, Tokyo, Japan), 20-MHz radial EBUS probe (UM-S20-20R; Olympus), guide sheath (SG-201C; Olympus), brush (BC-202D-2010; Olympus), forceps (FB-231D; Olympus), and 1.9 mm cryo probe (CRYO2; ERBE, Tuebingen, Germany) were employed [14]. Thrombin (Liquid Thrombin MOCHIDA Softbottle 10,000; Mochida Pharmaceutical, Tokyo, Japan) and balloon catheter (B5-2C; Olympus) were prepared in case of mild or severe bleeding [14]. Local anesthesia with 1% lidocaine for nebulizing, 2% lidocaine bolus to the bronchus, intravenous injection of 2–2.5 mg of midazolam, and intra-muscular injection of 35 mg pethidine hydrochloride for conscious sedation were used during the procedures [9, 14]. The blood pressure, oxygen saturation, pulse rate, and electrocardiography of all patients were monitored in this study [9, 14].
Sampling methods
Sampling methods were previously described [14]. Briefly, all patients were intubated with an endotracheal tube (7.5 mm TaperGuard; COVIDEN, MN, USA) to simplify the insertion and removal of the bronchoscope [14]. After confirmation of PPLs by EBUS and fluoroscopy, the internal EBUS was removed, leaving behind GS [3, 4, 14]. EBUS was withdrawn when PPLs were not identified, and a curette was inserted into GS to move into the appropriate bronchial segment [3, 14]. The curette was withdrawn, and EBUS was reinserted into GS to confirm PPLs under fluoroscopy [3, 14]. Brushing, TBB, and Cryo were performed in this series to obtain cytological materials and tissues [14]. Brushes for brushing were inserted into GS two times consecutively to obtain cytological materials. The forceps for TBB were inserted into GS 5 times to obtain tissues [14]. After the Cryo probe was wetted with alcohol cotton (STERI COTTOα; Kawamoto, Osaka, Japan) to facilitate smooth insertion into GS, the Cryo probe was inserted into GS and frozen with carbon dioxide for 3–5 s to about − 70 °C 1 or 2 times [14]. Subsequently, the Cryo probe was withdrawn together with GS and bronchoscope and then thawed in saline to obtain histological tissue [14]. The brush, forceps, and Cryo probe were washed with saline for cytological evaluation, cell blocks, bacterial cultures, acid-fast bacteria cultures, and polymerase chain reaction [14]. Each patient underwent chest radiography to assess potential complications 1 h after bronchoscopy [9, 14].
Sampling process and diagnosis
Sampling process and diagnosis were performed as previously described [14]. The tissues obtained by Cryo were cut in half [14]. One of the tissues obtained by Cryo and the tissue by TBB were immediately fixed with 20% formalin, stained with hematoxylin and eosin (HE) staining and immunohistochemistry (IHC) staining for histological evaluation and PD-L1 expression [14]. The other tissue obtained by Cryo was immediately frozen at − 80 °C for DNA sequencing analysis [14]. Every pathological specimen was evaluated by an experienced pathologist to reach a diagnosis [14].
Evaluation of tumor cell numbers and PD-L1 expression
After the pathologist reached a diagnosis, the number of tumor cells was counted manually by one cytoscreener and one pulmonologist in a blinded manner using HE staining slides. Then, the average number of tumor cells was calculated.
After sectioning of samples to 4–5 μm, PD-L1 staining was performed with 22C3 antibodies (rabbit monoclonal, clone 22C3; Agilent Dako, Glostrup, Denmark) using autostainer (Autostainer Link 48, Agilent Dako). PD-L1 positivity was defined as membranous staining in at least 1% of cells [10], regardless of staining intensity and proportion in the membrane. PD-L1 was evaluated by experienced pathologist, and the cut off values were classified as ≥50% and ≥ 1%. The number of tumor cells by a single biopsy, total number of tumor cells, average number of tumor cells, and PD-L1 expression for each patient were compared between Cryo and TBB.
Data analysis
Data analysis was carried out using Graph Pad PRISM (GraphPad Software, La Jolla, CA, USA). T-tests were used to compare the numbers of tumor cells between Cryo and TBB. Differences with P values of less than 0.05 were considered statistically significant. The odds ratio (OR), sensitivity, specificity, positive predict value (PPV), negative predict value (NPV), concordance, and Cohen’s kappa (κ) coefficient based on Cryo for TBB were used to assess PD-L1 expression. The concordance rate was classified according to κ value as slight agreement (0–0.20), fair agreement (0.21–0.40), moderate agreement (0.41–0.60), substantial agreement (0.61–0.80), or almost perfect agreement (0.81–1.0) [17].
Results
Baseline characteristics
Patient characteristics, including the number, gender, median age, smoking history, median size of PPLs, tumor, nodes, metastasis (TNM) stage, and final diagnosis by bronchoscope, are summarized in Table 1. We diagnosed 10 adenocarcinomas, 4 squamous cell carcinomas, 1 small cell lung cancer, and 1 metastatic lung tumor.
Table 1.
Patient characteristics
| Patient characteristics | Value |
|---|---|
| Patients no. | 16 |
| Male/Female no. | 14/2 |
| Median age (range) | 69 (46–82) |
| Smoking history no. (yes/no) | 14/2 |
| Median size (cm) of PPLs (range) | 3.9 (1–8.1) |
| TNM stage no. (%) | |
| I | 3 (18.8) |
| II | 3 (18.8) |
| III | 5 (31.3) |
| IV | 5 (31.3) |
| Histological subtype no. (%) | |
| Adenocarcinoma | 10 (62.5) |
| Squamous cell carcinoma | 4 (25) |
| Small cell lung cancer | 1 (6.25) |
| Metastatic lung tumor | 1 (6.25) |
PPLs peripheral pulmonary lesions, TNM tumor, nodes, metastasis
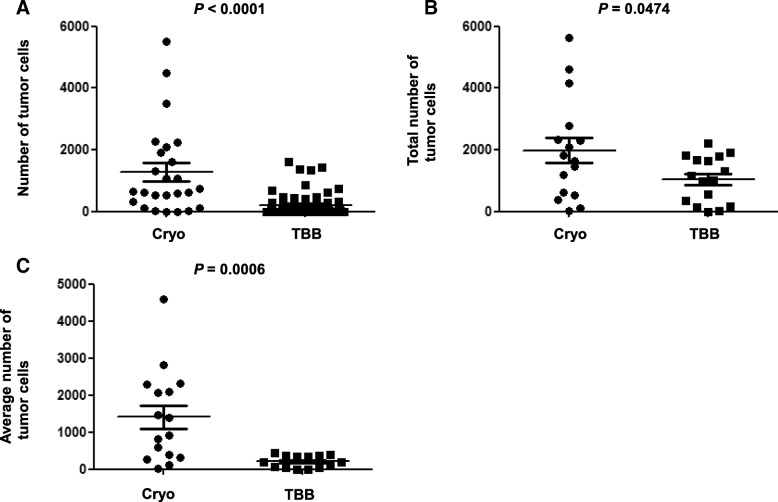
Comparison of tumor cell numbers between Cryo and TBB specimens
Comparisons of tumor cell numbers between Cryo and TBB are shown in Table 2. The number of tumor cells obtained from a single biopsy by Cryo was significantly larger than that by TBB (Cryo [mean ± standard error of the mean]: 1321 ± 303.7; TBB: 208.8 ± 38.24; 95% confidence interval [CI]: 756.8–1467, P < 0.0001, Fig. 1a). The total number of tumor cells obtained by Cryo was significantly larger than that obtained by TBB (Cryo: 1981 ± 411.7; TBB: 1044 ± 189.0; 95% CI: 11.79–1862, P = 0.0474, Fig. 1b). Furthermore, the average number of tumor cells obtained by Cryo was also significantly larger than that obtained by TBB (Cryo: 1406 ± 310.3; TBB: 208.8 ± 37.81; 95% CI: 558.6–1835, P = 0.0006, Fig. 1c).
Table 2.
Comparison of the number of tumor cells from a single biopsy, total number of tumor cells, average number of tumor cells, and PD-L1 expression between Cryo and TBB
| Cryo | TBB | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | No. of tumor cells | Total no. | Average no. | PD-L1 (%) | No. of tumor cells | Total no. | Average no. | PD-L1 (%) | |||||
| 1 | 4601 | 4601 | 4601 | 10 | 634 | 402 | 337 | 332 | 198 | 1903 | 380.6 | 5 | |
| 2 | 381 | 381 | 381 | 0 | 1622 | 29 | 0 | 0 | 0 | 1651 | 330.2 | 0 | |
| 3 | 25 | 25 | 25 | 0 | 871 | 302 | 140 | 0 | 0 | 1313 | 262.6 | 0 | |
| 4 | 2080 | 2080 | 2080 | 100 | 143 | 98 | 76 | 10 | 8 | 335 | 67 | 100 | |
| 5 | 115 | 115 | 115 | 10 | 3 | 0 | 0 | 0 | 0 | 3 | 0.6 | 0 | |
| 6 | 3509 | 642 | 4151 | 2075.5 | 10 | 63 | 50 | 25 | 22 | 0 | 160 | 32 | 0 |
| 7 | 1467 | 1467 | 1467 | 40 | 14 | 0 | 0 | 0 | 0 | 14 | 2.8 | 0 | |
| 8 | 532 | 0 | 532 | 266 | 0 | 1340 | 449 | 30 | 12 | 0 | 1831 | 366.2 | 0 |
| 9 | 2248 | 541 | 2789 | 1394.5 | 0 | 124 | 25 | 0 | 0 | 0 | 149 | 29.8 | 0 |
| 10 | 2321 | 2321 | 2321 | 10 | 334 | 294 | 157 | 124 | 96 | 1005 | 201 | 0 | |
| 11 | 618 | 0 | 618 | 309 | 5 | 471 | 217 | 169 | 119 | 0 | 976 | 195.2 | 0 |
| 12 | 1621 | 31 | 1652 | 826 | 0 | 331 | 222 | 0 | 0 | 0 | 553 | 110.6 | 0 |
| 13 | 5520 | 121 | 5641 | 2820.5 | 90 | 1380 | 137 | 90 | 61 | 7 | 1675 | 335 | 100 |
| 14 | 2301 | 2301 | 2301 | 70 | 1431 | 471 | 145 | 90 | 66 | 2203 | 440.6 | 10 | |
| 15 | 625 | 578 | 1203 | 601.5 | 0 | 311 | 248 | 202 | 198 | 187 | 1146 | 229.2 | 10 |
| 16 | 1075 | 740 | 1815 | 907.5 | 0 | 750 | 675 | 302 | 58 | 0 | 1785 | 357 | 10 |
Cryo cryobiopsy, TBB transbronchial biopsy, PD-L1 programmed death ligand 1
Fig. 1.
Comparison of the numbers of tumor cells between Cryo and TBB. a, The number of tumor cells obtained by a single biopsy. 1321 ± 303.7 (mean ± SEM) for Cryo, 208.8 ± 38.24 for TBB (95% CI: 756.8–1467, P < 0.0001). b, Total number of tumor cells obtained by each biopsy. 1981 ± 411.7 for Cryo, 1044 ± 189.0 for TBB (95% CI: 11.79–1862, P = 0.0474). c, Average number of tumor cells obtained by each biopsy. 1406 ± 310.3 for Cryo, 208.8 ± 37.81 for TBB (95% CI: 558.6–1835, P = 0.0006). Cryo, cryobiopsy; TBB transbronchial biopsy; SEM, standard error of the mean; CI, confidence interval
Comparison of PD-L1 expression between Cryo and TBB specimens
Comparisons of PD-L1 expression between Cryo and TBB are shown in Table 2. Representative image of HE staining for TBB and Cryo and PD-L1 ≥ 50% for Cryo with the same patient are shown in Fig. 2. PD-L1 ≥ 50% was observed in 18.8% of patients for Cryo and 12.5% of patients for TBB. PD-L1 ≥ 1% was observed in 56.3% of patients for Cryo and 37.5% of patients for TBB. The OR, sensitivity, specificity, PPV, NPV, concordance, and κ coefficient were 45 (95% CI: 1.394–1452), 66.7% (0.094–0.992), 100% (0.753–1), 100% (0.158–1), 92.9% (0.661–0.998), 93.8% (0.698–0.998), and 0.7647 (0.288–1), respectively, for PD-L1 ≥ 50% and 2 (0.244–16.37), 44.4% (0.137–0.788), 71.4% (0.290–0.963), 66.7% (0.223–0.957), 50% (0.187–0.813), 56.3% (0.299–0.803), and 0.1515 (0–0.608), respectively, for PD-L1 ≥ 1% (Table 3).
Fig. 2.
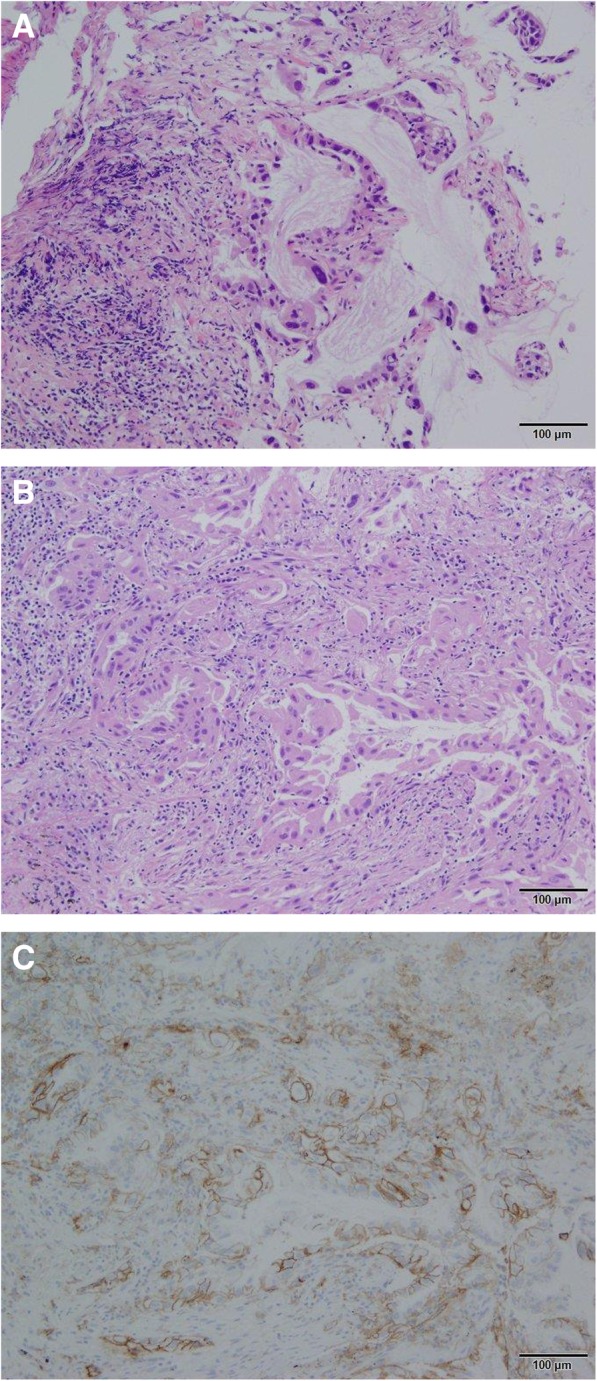
Representative image of HE staining for TBB and Cryo and PD-L1 ≥ 50% with the same patient (Adenocarcinoma 10×). a, HE staining for TBB specimens. b, HE staining for Cryo specimens. c, PD-L1 ≥ 50% for Cryo specimens. HE, hematoxylin and eosin; PD-L1, programmed death ligand 1; TBB, transbronchial biopsy; Cryo, Cryobiopsy
Table 3.
Comparison of OR, sensitivity, specificity, PPV, NPV, concordance, and κ coefficient with 95% CI between Cryo and TBB according to PD-L1 expression
| PD-L1 ≥ 50% (95% CI) | PD-L1 ≥ 1% (95% CI) | |
|---|---|---|
| OR | 45 (1.394–1452) | 2 (0.244–16.37) |
| Sensitivity | 66.7% (0.094–0.992) | 44.4% (0.137–0.788) |
| Specificity | 100% (0.753–1) | 71.4% (0.290–0.963) |
| PPV | 100% (0.158–1) | 66.7% (0.223–0.957) |
| NPV | 92.9% (0.661–0.998) | 50% (0.187–0.813) |
| Concordance | 93.8% (0.698–0.998) | 56.3% (0.299–0.803) |
| κ coefficient | 0.7647 (0.288–1) | 0.1515 (0–0.608) |
OR odds ratio, PPV positive predict value, NPV negative predict value, CI confidence interval, Cryo cryobiopsy, TBB transbronchial biopsy, PD-L1 programmed death ligand 1
Adverse events
There were no clinically serious adverse events, except mild bleeding in 4 cases; all cases required endoscopic procedures with thrombin [14].
Discussion
In this study, we described the excellent results of Cryo with EBUS-GS for PPLs. To the best of our knowledge, no other studies have reported comparisons of tumor cell numbers and PD-L1 expression between Cryo and TBB with EBUS-GS for PPLs. This report provides evidence about comparison of tumor cell numbers and 22C3 PD-L1 expression using Cryo with EBUS-GS.
In our study, the number of tumor cells from a single biopsy, total number of tumor cells, and average number of tumor cells obtained by Cryo were significantly larger than those obtained by TBB. Cryo with EBUS-GS had the advantage of yielding significantly larger specimens than TBB, as we previously reported [14, 15]. The volume obtained by Cryo was about 26 times greater than that obtained by TBB [14]. Therefore, the higher volume was expected to contribute to the significant differences in the number of tumor cells. Not only did Cryo yield more tumor cells than TBB but Cryo also showed higher total and average numbers of tumor cells, suggesting that it may be appropriate to perform Cryo 1 or 2 times for PPLs suspicious of lung cancer. In addition, performing Cryo 1 or 2 times would yield more DNA for subsequent analyses of lung cancers because the numbers of tumor cells were significantly larger than that obtained by TBB, despite performing TBB 5 times. Cryo specimens may be more appropriate for analyzing gene mutations and performing whole exon sequencing compared with TBB specimens. Furthermore, despite being cut in half and the one was used for gene mutation analysis [14], even the other half of the specimen was sufficient for evaluation of HE staining and PD-L1 expression. Notably, for PD-L1 ≥ 50%, we found high specificity (100%), PPV (100%), NPV (100%), and concordance (93.8%) and substantial agreement (0.7647) for κ coefficient. In contrast, for PD-L1 ≥ 1%, we found low sensitivity (44.4%), NPV (50%), and concordance (56.3%) and slight agreement (0.1515) for κ coefficient.
Some studies have assessed the concordance rate of PD-L1 expression between resected tissues and biopsy samples [18–20] or tissue microarrays [21]. One study using a specific hybrid IHC score with 4059 antibody showed good concordance between resected samples and TBB for PD-L1 expression [18]. Another study using positive/negative IHC scores with EPR1161 (2) antibody showed moderate concordance [19]. Similarly, we demonstrated high specificity, PPV, NPV, and concordance and substantial agreement for κ coefficient between Cryo, which showed a significantly larger volume such as resected specimen than TBB, and TBB for PD-L1 ≥ 50%. In contrast, we observed low sensitivity, NPV, and concordance and slight agreement for κ coefficient for PD-L1 ≥ 1%. We hypothesized that the reasons for this discrepancy between previous reports and our results with regard to PD-L1 ≥ 1% may be related to the use of different antibody, various scoring systems, and heterogeneity of PD-L1 expression.
Some immune checkpoint inhibitors have been proved to be effective for lung cancer treatment as first-line monotherapy [11, 22], first-line combination therapy [23–25], or second-line therapy [10, 26, 27]. However, pembrolizumab is the only immune checkpoint inhibitor found to be effective as a first-line monotherapy according to the proportion of PD-L1 expression. 22C3 antibody, which are regarded as a companion diagnostics, are associated with pembrolizumab. Accordingly, in this study, we used 22C3 antibody to detect PD-L1 expression. Importantly, some studies describing PD-L1 expression have found it different with various antibodies [28, 29], and various antibodies have been shown to have different cut-off values for PD-L1 expression [22–27]. Furthermore, some studies described the intra- and inter-tumor heterogeneity of PD-L1 expression [30–32]. Indeed, heterogeneity is the one of the reasons we had 2 false-positive cases for PD-L1 ≥ 1%. Moreover, Cryo yielded larger specimens [14] and higher tumor cell numbers than TBB. These reasons support our above interpretations and may explain the differences in results for PD-L1 ≥ 1% between previous studies [18, 19] and our current findings.
Our results regarding PD-L1 expression could contribute to patients taking pembrolizumab as first-line therapy [22] when PD-L1 was negative by evaluating TBB specimens. It could be reliable for evaluating PD-L1 expression to use Cryo specimens to prevent from leading to misclassification. Moreover, we showed that Cryo specimens had the advantages of not only providing tissues for accurate diagnosis and DNA for gene analysis for personalized therapeutic strategy [14] but providing ample tissue for evaluating PD-L1 expression.
This study had several limitations. First, it was performed at a single institution with a small number of patients and did not apply a randomized control design to validate the results. Second, we compared tumor cell numbers and PD-L1 expression between Cryo and TBB. Thus, a comparison of PD-L1 expression between Cryo and resected tissues should be performed in future studies. Third, although we used a smaller Cryo probe (1.9 mm), performing Cryo with a larger probe (2.4 mm, CRYO2; ERBE) may have yielded even larger tissues and more tumor cells for evaluating gene analysis and PD-L1 expression. However, such an approach may also cause clinically significant complications. The optimal size of Cryo probe still remains unknown.
Conclusion
Cryo with EBUS-GS for PPLs is a useful diagnostic strategy. The number, total number, and average number of tumor cells obtained by Cryo were significantly larger than those obtained by TBB. Thus, this approach may be more appropriate for analyzing gene mutations and whole exon sequencing compared with TBB. These results could contribute to patients taking pembrolizumab as first-line therapy when PD-L1 was negative by evaluating TBB specimens. Cryo specimens could have an advantage of providing ample tissue for evaluating PD-L1 expression in addition to providing tissue for accurate diagnosis and DNA for gene analysis. Further studies with larger cohorts are needed to validate these results.
Acknowledgements
We are grateful to Ms. Yoshimi Sugimura and Mr. Masayuki Shino for technical assistance.
Abbreviations
- Cryo with EBUS-GS
Cryobiopsy with endobronchial ultrasonography using a guide sheath
- PD-L1
Programmed death ligand 1
- PPLs
Peripheral pulmonary lesions
- TBB
Transbronchial biopsy
Authors’ contributions
Conception and design: KA, TJ; Acquisition of data: KA, FK; Analysis of data: KA, MK; Diagnosis: YN; Manuscript the article: KA, MK, ET; Revision and Edition the article: KA, MK, YN, KT, ET; All authors read and approved the manuscript.
Funding
This study was supported in part by the Japanese Foundation for Research and Promotion of Endoscopy grant.
Availability of data and materials
The dataset supporting the conclusions of this study is presented in this manuscript. The clinical detail dataset is available from the author and corresponding author, but has not been made publicly available.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Tokyo Women’s Medical University Hospital (date of approval: April 19, 2017; approval number: 170404). Informed consent was obtained from all patients before enrollment in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rivera MP, Mehta AC, Wahidi MM. Establishing the diagnosis of lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e142S–e165S. doi: 10.1378/chest.12-2353. [DOI] [PubMed] [Google Scholar]
- 2.Shirakawa T, et al. Usefulness of endobronchial ultrasonography for transbronchial lung biopsies of peripheral lung lesions. Respiration. 2004;71(3):260–268. doi: 10.1159/000077424. [DOI] [PubMed] [Google Scholar]
- 3.Kikuchi E, et al. Endobronchial ultrasonography with guide-sheath for peripheral pulmonary lesions. Eur Respir J. 2004;24(4):533–537. doi: 10.1183/09031936.04.00138603. [DOI] [PubMed] [Google Scholar]
- 4.Kurimoto N, et al. Endobronchial ultrasonography using a guide sheath increases the ability to diagnose peripheral pulmonary lesions endoscopically. Chest. 2004;126(3):959–965. doi: 10.1378/chest.126.3.959. [DOI] [PubMed] [Google Scholar]
- 5.Herth FJ, Eberhardt R, Becker HD, Ernst A. Endobronchial ultrasound-guided transbronchial lung biopsy in fluoroscopically invisible solitary pulmonary nodules: a prospective trial. Chest. 2006;129(1):147–150. doi: 10.1378/chest.129.1.147. [DOI] [PubMed] [Google Scholar]
- 6.Yoshikawa M, et al. Diagnostic value of endobronchial ultrasonography with a guide sheath for peripheral pulmonary lesions without X-ray fluoroscopy. Chest. 2007;131(6):1788–1793. doi: 10.1378/chest.06-2506. [DOI] [PubMed] [Google Scholar]
- 7.Eberhardt R, Ernst A, Herth FJ. Ultrasound-guided transbronchial biopsy of solitary pulmonary nodules less than 20 mm. Eur Respir J. 2009;34(6):1284–1287. doi: 10.1183/09031936.00166708. [DOI] [PubMed] [Google Scholar]
- 8.Asahina H, et al. Transbronchial biopsy using endobronchial ultrasonography with a guide sheath and virtual bronchoscopic navigation. Chest. 2005;128(3):1761–1765. doi: 10.1378/chest.128.3.1761. [DOI] [PubMed] [Google Scholar]
- 9.Arimura K, et al. The efficacy of transbronchial needle aspiration with endobronchial ultrasonography using a guide sheath for peripheral pulmonary lesions suspected to be lung cancer. Respir Investig. 2017;55(6):365–371. doi: 10.1016/j.resinv.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 10.Borghaei H, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373(17):1627–1639. doi: 10.1056/NEJMoa1507643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reck M, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med. 2016;375(19):1823–1833. doi: 10.1056/NEJMoa1606774. [DOI] [PubMed] [Google Scholar]
- 12.Dietel M, et al. Diagnostic procedures for non-small-cell lung cancer (NSCLC): recommendations of the European expert group. Thorax. 2016;71(2):177–184. doi: 10.1136/thoraxjnl-2014-206677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Travis WD, et al. Diagnosis of lung cancer in small biopsies and cytology: implications of the 2011 International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification. Arch Pathol Lab Med. 2013;137(5):668–684. doi: 10.5858/arpa.2012-0263-RA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arimura Ken, Tagaya Etsuko, Akagawa Hiroyuki, Nagashima Yoji, Shimizu Satoru, Atsumi Yoshihide, Sato Akitoshi, Kanzaki Masato, Kondo Mitsuko, Takeyama Kiyoshi, Massion Pierre P., Tamaoki Jun. Cryobiopsy with endobronchial ultrasonography using a guide sheath for peripheral pulmonary lesions and DNA analysis by next generation sequencing and rapid on-site evaluation. Respiratory Investigation. 2019;57(2):150–156. doi: 10.1016/j.resinv.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 15.Schuhmann M, et al. Endobronchial ultrasound-guided cryobiopsies in peripheral pulmonary lesions: a feasibility study. Eur Respir J. 2014;43(1):233–239. doi: 10.1183/09031936.00011313. [DOI] [PubMed] [Google Scholar]
- 16.Izumo T, et al. Utility of rapid on-site cytologic evaluation during endobronchial ultrasound with a guide sheath for peripheral pulmonary lesions. Jpn J Clin Oncol. 2017;47(3):221–225. doi: 10.1093/jjco/hyw180. [DOI] [PubMed] [Google Scholar]
- 17.Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33(2):363–374. doi: 10.2307/2529786. [DOI] [PubMed] [Google Scholar]
- 18.Kitazono S, et al. Reliability of small biopsy samples compared with resected specimens for the determination of programmed death-ligand 1 expression in non--small-cell lung cancer. Clin Lung Cancer. 2015;16(5):385–390. doi: 10.1016/j.cllc.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 19.Sakakibara R, et al. EBUS-TBNA as a promising method for the evaluation of tumor PD-L1 expression in lung cancer. Clin Lung Cancer. 2017;18(5):527–534. doi: 10.1016/j.cllc.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Sakata KK, et al. Comparison of programmed death Ligand-1 Immunohistochemical staining between endobronchial ultrasound Transbronchial needle aspiration and resected lung cancer specimens. Chest. 2018;154(4):827–837. doi: 10.1016/j.chest.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 21.Li C, et al. Comparison of 22C3 PD-L1 expression between surgically resected specimens and paired tissue microarrays in non-small cell lung cancer. J Thorac Oncol. 2017;12(10):1536–1543. doi: 10.1016/j.jtho.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 22.Mok TSK, et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393(10183):1819–1830. doi: 10.1016/S0140-6736(18)32409-7. [DOI] [PubMed] [Google Scholar]
- 23.Gandhi L, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378(22):2078–2092. doi: 10.1056/NEJMoa1801005. [DOI] [PubMed] [Google Scholar]
- 24.Socinski MA, et al. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288–2301. doi: 10.1056/NEJMoa1716948. [DOI] [PubMed] [Google Scholar]
- 25.Horn L, et al. First-line Atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379(23):2220–2229. doi: 10.1056/NEJMoa1809064. [DOI] [PubMed] [Google Scholar]
- 26.Herbst RS, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387(10027):1540–1550. doi: 10.1016/S0140-6736(15)01281-7. [DOI] [PubMed] [Google Scholar]
- 27.Fehrenbacher L, et al. Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): a multicentre, open-label, phase 2 randomised controlled trial. Lancet. 2016;387(10030):1837–1846. doi: 10.1016/S0140-6736(16)00587-0. [DOI] [PubMed] [Google Scholar]
- 28.Hirsch FR, et al. PD-L1 immunohistochemistry assays for lung cancer: results from phase 1 of the blueprint PD-L1 IHC assay comparison project. J Thorac Oncol. 2017;12(2):208–222. doi: 10.1016/j.jtho.2016.11.2228. [DOI] [PubMed] [Google Scholar]
- 29.Tsao MS, et al. PD-L1 immunohistochemistry comparability study in real-life clinical samples: results of blueprint phase 2 project. J Thorac Oncol. 2018;13(9):1302–1311. doi: 10.1016/j.jtho.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mansfield AS, et al. Heterogeneity of programmed cell death ligand 1 expression in multifocal lung cancer. Clin Cancer Res. 2016;22(9):2177–2182. doi: 10.1158/1078-0432.CCR-15-2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Casadevall D, et al. Heterogeneity of tumor and immune cell PD-L1 expression and lymphocyte counts in surgical NSCLC samples. Clin Lung Cancer. 2017;18(6):682–691. doi: 10.1016/j.cllc.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 32.Dill EA, et al. PD-L1 expression and Intratumoral heterogeneity across breast Cancer subtypes and stages: an assessment of 245 primary and 40 metastatic tumors. Am J Surg Pathol. 2017;41(3):334–342. doi: 10.1097/PAS.0000000000000780. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this study is presented in this manuscript. The clinical detail dataset is available from the author and corresponding author, but has not been made publicly available.