Abstract
AIM:
The study aimed to compare teeth sensitivity and shade after bleaching protocol with descending different light intensities versus bleaching protocol with the same high light intensity.
MATERIAL AND METHODS:
Sample size was twenty-four patients. Each group consisted of twelve patients. Group, I patients received bleaching protocol of descending different light intensities. Group II patients received bleaching protocol with the same high light intensity; both groups used the same home bleaching gel kit for seven days according to manufacturer instructions and protocol. Baseline records were digital photographs, teeth sensitivity and teeth shade for 12 anterior teeth. Teeth sensitivity was assessed using five points verbal rating scale and Standardized 100 mm Visual analogue scale after 1 day, after 2 days and after 1 week. Teeth shades for twelve anterior teeth were recorded by VITA Easy Shade V (VITA Zahnfabrik H. Rauter GmbH & Co. KG, Germany) after 1 week by VITA Easy Shade V. Mann-Whitney test (non-parametric test, 2 independent samples) was used to compare teeth sensitivity between both bleaching protocols at each period. A paired t-test (parametric test, 2 related samples) was performed to compare the colour change in shade guide units (SGU) and ∆E values within high light intensity bleaching protocol. While Wilcoxon Signed-Rank test (non-parametric test, 2 related samples) was used to compare colour change light intensities bleaching protocol. Comparison of bleaching effectiveness (∆SGU and ∆Ediff) between both bleaching protocols was performed by the Mann-Whitney test.
RESULTS:
Descending light intensities protocol showed a lower teeth sensitivity than high light intensity protocol after 1 and 2 days. There was no teeth sensitivity reported at 1-week post-bleaching. Regarding the teeth shade, descending light intensities protocol had a little higher effect on colour change in shade guide units (SGU) than high light intensity protocol effect. Both bleaching protocols showed there was no significant difference in ∆SGU recorded after bleaching between high and descending light intensities protocols.
CONCLUSION:
Descending different light intensities protocol showed a lower teeth sensitivity than high same light intensity protocol. Descending light intensities protocol had a little higher effect on colour change in shade guide units (SGU) than high light intensity protocol effect.
Keywords: Teeth bleaching, High light intensity protocol, Descending light intensity protocol, Teeth sensitivity, Teeth shade
Introduction
Teeth discolourations are usually various, multifaceted and have been classified as extrinsic, intrinsic, and internalised discolourations. Adult teeth get darker due to changes in enamel and dentin properties, losing their natural white shade [1]. Tooth shade is one of the most important factors determining satisfaction with dental appearance [2]. Self-satisfaction decreases with increasing severity of discolourations. White teeth look been positively correlated with high social competence, intellectual ability, psychological adjustment and relationship status [2].
Nowadays, vital tooth bleaching is one of the most requested cosmetic dental procedures asked by patients for a more pleasing smile [3]. The American Dental Association (ADA) has advised patients to ask the dentists to select the most suitable bleaching treatment, especially for those complaining of teeth sensitivity, dental restorations, extremely dark discolourations, and single dark teeth [4]. Success of teeth bleaching is affected by many factors: stains type, age, bleaching activation systems, the concentration of the bleaching agents, and duration of application as well as home bleaching application [5].
Teeth sensitivity (TS) is the most common clinical side effect of vital teeth bleaching; more than 60% of the patients undergo it. It can cause severe discomfort that is the main obstacle to patients completes the bleaching treatment [6].
Activation of the bleaching agents by heat or light may hurt pulpal tissue. It was reported that the use of intense lights elevated bleach temperature and resulted in an increased intra pulpal temperature, which may further impact patient sensitivity and pulpal health [7].
Accordingly, a randomised clinical trial (RCT) on the effect of high light intensity bleaching protocol versus descending light intensities bleaching protocol on post bleaching teeth sensitivity would be of value.
Material and Methods
Trial Approval and Registration
The trial was designed following the SPIRIT 2013 Statement (Standard Protocol Items: Recommendations for Interventional Trials). The protocol was approved by Evidence-Based Dentistry Committee (EBD) – Faculty of Dentistry, Cairo University-Egypt. This study protocol was registered on ClinicalTrial.gov website; It’s ClinicalTrials.gov identifier number: NCT02888847.
Sample size calculation
The sample size was 24 patients, based on the previous data [8], it indicated that the probability of no sensitivity among controls is 0.09. If the true probability of exposure among intervention was 0.6, then it was needed to study 12 patients in each group to be able to reject the null hypothesis, so that both groups were equal with probability (power) 0.8. The Type I error probability associated with this test of this null hypothesis was 0.05. An uncorrected chi-square statistic was used to evaluate this null hypothesis.
Participants’ recruitment
The principal investigator screened patients in Outpatient clinics of departments of Conservative Dentistry and Restorative Dentistry in Faculty of Dentistry of Cairo University and British University in Egypt respectively, who require teeth bleaching to participate in this trial. Medical and dental histories were carefully assessed. Thorough extra- and intra-oral examinations of the participants were performed and recorded in the diagnostic chart to fulfil the eligibility criteria of the trial which were recognised from previous studies [9], [10], [11]. The inclusion and exclusion criteria are listed in Table 1.
Table 1.
Eligibility criteria of the trial
| Inclusion Criteria for participants: | Exclusion criteria for participants: |
|---|---|
| 1. Patients included in this clinical trial were at least18 years old. 2. Patients were free from any systemic disease that may affect normal healing and predictable outcome. 3. Patients agreed to the informed consent and committed to follow-up period. 4. Refrained from tobacco products and any coloured liquids or food (e.g. coffee, tea, tomato sauce, etc.) during the active study period. |
1. Patients with any systemic disease that may affect normal healing. 2. Patient with bad oral hygiene. 3. Pregnant females. 4. Patients who could not participate in the follow-up period. 5. Untreated, periodontal diseases were not allowed. 6. Active caries or defective Restorations in six anterior teeth. 7. Sensitive Teeth. 8. Bleaching history. 9. Patients are participating in more than 1 dental study. |
Participants’ grouping
All participants fulfilling the eligibility criteria were randomly assigned using computer-generated randomisation www.random.org to either intervention (descending light intensity bleaching protocol) or control (high light intensity bleaching protocol) groups.
Study setting
The study was conducted in the outpatient clinic of the Department of Restorative Dentistry - British University in Egypt.
Pre-Bleaching Teeth Sensitivity Assessment
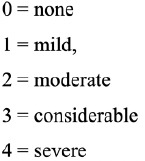
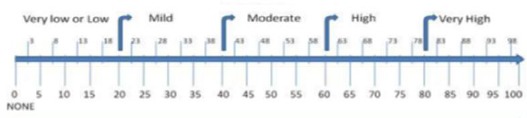
Teeth sensitivity records: through five points verbal rating scale [10], [12] and visual analogue scale (0-100 mm) [13], [14] presented in Figure 1 and Figure 2 respectively. Any patients were complaining of sensitive teeth were disregard during recruitment according to eligibility criteria.
Figure 1.
Five Verbal Points
Figure 2.
Visual Analogue Scale
Upper and lower alginate impressions were taken to fabricate customised fit bleaching trays. Two pairs of bleaching trays were fabricated for the patient. One pair was used as a positioning guide in recording teeth shade. The second pair was used with post-care gel and home bleaching gel. Teeth were scaled using ultrasonic scaler (SUPRASSON P5, ACTEON, France) followed by teeth polishing utilising white Nylon Bowl Polishing Polisher prophy Brushes and prophylaxis paste (Quartz Prophylaxis Paste, medium grit by Dharma, USA).
Pre-bleaching Base Line Shade Assessment
Pre-bleaching digital images of the patient were taken. Baseline teeth shades for 12 anterior teeth (6 maxillary anterior teeth and 6 mandibular anterior teeth) were recorded by VITA Easyshade V (VITA Zahnfabrik H. Rauter GmbH & Co. KG, Germany), through punching the middle one third of the labial surface of the 6 anterior teeth in maxillary and mandibular bleaching trays [14]. The measurement area of interest for shade matching was the middle third of the facial surface of anterior maxillary teeth, according to the American Dental Association (ADA) guidelines [15].
VITA Easyshade V shade-matched teeth with value-ordered VITA® Classical Shade Guide into the following order presented in Figure 3 [14]. The arrangement from B1 (lightest colour) to C4 (darkest colour), corresponding to a grade of whitening from 1 to 16, in which a smaller number means the tooth was lighter. Although this scale is not linear in the truest sense, the changes were treated as though they represented a continuous and approximately linear ranking for analysis.
Figure 3.
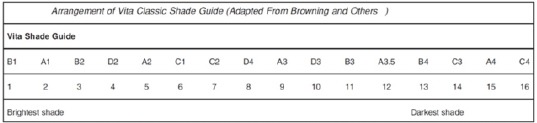
Arrangement of Vita Classic Shade Guide
Shade parameters that were recorded: shade guide units (SGU) and its relative ΔE directly through spectrophotometer measurements of VITA Easyshade V.
Δ E: The overall shade deviation closest value-ordered VITA® Classical Shade Guide in the colour space.
In-office Bleaching Phase
Three cycles were carried on according to manufacture instructions on ten anterior maxillary teeth and ten mandibular anterior teeth for two study groups.
Group I: Patients received Bleaching Protocol with same high light intensity. It represented the control group. (Philips Zoom!™ Advanced Power whitening gel and lamp, Discus Dental, Inc., Culver City, CA, USA.). It’s light source was Ultra Violet – A band. Its average wavelength of 365 nm. It had one high light intensity mode.
Group II: Patients received Bleaching Protocol with descending (high followed by moderate then low) light intensities. (Philips Zoom!™ WhiteSpeed in-office whitening gel and lamp, Discus Dental, Inc., Culver City, CA, USA.). It represented the intervention group. It’s light source was Blue Light Emitting Diode (LED). Its wavelength was 465 nm. It had three light intensities high, medium and low modes.
Only one in-office bleaching gel kit was used utilising by two different light-activated bleaching devices with different light intensities. Also, one home bleaching gel kit was utilised in this study. The materials used as well as their composition, manufacturers’ details and lot numbers were listed in Table 2.
Table 2.
Specifications of materials, composition, manufacturers and batch numbers Material
| Specifications | Composition | Manufacturer | Batch number | |
|---|---|---|---|---|
| Philips ZOOM! | In-office (chairside) light-activated bleaching gel | 25% Hydrogen Peroxide and Ferrous Gluconate photo-catalyst | Discus Dental, LLC., Ontario, CA, 91761 USA | 16243005 |
| Philips Zoom nite white | Home chemical activated the bleaching gel Professional take-home whitening system | 22% Carbamide Peroxide Formulated with ACP (amorphous calcium phosphate), potassium nitrate and fluoride. | Discus Dental, LLC., Ontario, CA, 91761 USA | 423502124491 |
| Relief® ACP Oral Care Gel | Desensitizer included into Philips ZOOM! Kit in-office (chair-side) light-activated bleaching gel | Water, Poloxamer 338, Potassium Nitrate, Mentha Piperita, Calcium Nitrate, Sodium Saccharin, Sodium Fluoride, Disodium Phosphate and Monosodium Phosphate. | Discus Dental, LLC., Ontario, CA, 91761 USA | 16243005 |
Immediate Patient Post Care
Relief® ACP Oral Care Gel included in Philips ZOOM! The kit has been shown to decrease sensitivity and remineralise teeth. It was placed into trays and seated on patient teeth. Normal wear time was 30 minutes according to manufacturer instructions. The patients were asked not to drink or eat for 30 minutes after application according to manufacturer instructions. Digital imaging and videos were taken during the whole clinical procedures.
Instructions were given to the patients after ending in-office bleaching sessions
Patients were advised not to consume coffee, tea, tobacco, alcoholic drinks, and soft drinks for 2 hours after Zoom, until pellicle reforms.
Also, they were asked to decrease their intake of any stainable food or drinks and to drink using a straw.
Home bleaching phase
They were asked to wear the tray with the gel Philips Zoom NiteWhite (Discus Dental, LLC., Ontario, CA, 91761 USA) on daily routine at night before bedtime. Starting from the next day of bleaching sessions for seven successive days. Wear time was two hours per night.
1. Post-Bleaching Teeth Sensitivity Evaluation:
Teeth sensitivity records through five points’ verbal rating scale and visual analogue scale (0-100 mm) after 1-day, after 2-days and after 1-week.
1.a. Five points verbal rating scale Evaluation:
Participants were asked to mark their sensitivity experience after in-office bleaching by 1-day, 2-days and 1-week, using the following points: 0 = none, 1 = mild, 2 = moderate, 3 = considerable, and 4 = severe.
1.b. Visual Analogue Scale (0-100 mm):
The patients were asked to mark a standardised 100 mm visual analogue scale (VAS) ranging from 0 to 100. One end was labelled ‘no discomfort’ whereas the other end was labelled ‘severe discomfort’. After the in-office bleaching treatment by 1-day, 2-days and 1-week, the patients were asked to mark the position that best indicated their current opinion.
2. Post-Bleaching Shade Evaluation:
Digital imaging of the patient was taken after one week (7 days) from the bleaching session. Also, post bleaching teeth shades for 12 anterior teeth (6 maxillary anterior teeth and 6 mandibular anterior teeth) were recorded by VITA Easy Shade V (VITA Zahnfabrik H. Rauter GmbH & Co. KG, Germany) after one week (7 days) through wearing punched bleaching trays used in baseline records by VITA Easy Shade V.
Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics Version 2.1 for Windows. Data were presented as mean and standard deviation (SD). The significance level was set at P ≤ 0.05. Kolmogorov-Smirnov and Shapiro-Wilk tests were used to assess data normality.
Kruskal-Wallis (non-parametric test, repeated comparisons) followed by Bonferroni-corrected Wilcoxon Signed-Rank test was conducted to compare post-bleaching teeth sensitivity (TS) assessed by both pain scales at different periods within each bleaching protocol. Mann-Whitney test (non-parametric test, 2 independent samples) was used to compare teeth sensitivity between both bleaching protocols at each period.
A paired t-test (parametric test, 2 related samples) was performed to compare the colour change in shade guide units (SGU) and ∆E values within high light intensity bleaching protocol. While Wilcoxon Signed-Rank test (non-parametric test, 2 related samples) was used to compare colour change light intensities bleaching protocol. Comparison of bleaching effectiveness (∆SGU and ∆Ediff) between both bleaching protocols was performed by the Mann-Whitney test.
Results
In this study, a total of twenty-four patients received teeth bleaching (3 cycles) re-evaluated after 1-day, 2-days and 1-week.
1. Post-Bleaching tooth sensitivity (TS):
1.a. Effect of different periods on post-bleaching teeth sensitivity within each bleaching protocol:
Mean, Standard deviation (SD) of VRS and VAS and P-value for the effect of different periods on post-bleaching teeth sensitivity within each bleaching protocol are presented in Table 3, Figure 4 and Figure 5.
Table 3.
Statistical analysis for mean ± St. deviation of VRS and VAS and P-value for the effect of different periods on post-bleaching teeth sensitivity within each bleaching protocol
| High light intensity | Descending light intensities | |||
|---|---|---|---|---|
| VRS | VAS | VRS | VAS | |
| Baseline | 0a | 0a | 0a | 0a |
| 1-day post-bleaching | 2.1 ± 0.7b | 42.1 ± 7.1b | 1.3 ± 0.4b | 28.3 ± 15.5b |
| 2-days post-bleaching | 0.5 ± 0.5c | 10.5 ± 12.4c | 0.3 ± 0.4c | 8.3 ± 12.3c |
| 1-week post-bleaching | 0a | 0a | 0a | 0a |
| P-value | < 0.001* | < 0.001* | < 0.001* | < 0.001* |
Different superscript letters within the same row indicates a statistically significant difference at p ≤ 0.05;
: significant (p ≤ 0.05); NS: non-significant (p > 0.05).
Figure 4.
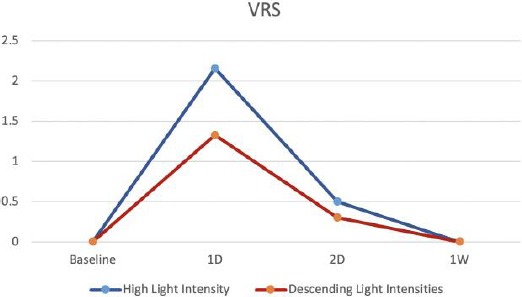
Line graph chart showing VRS at different periods within each bleaching protocol
Figure 5.
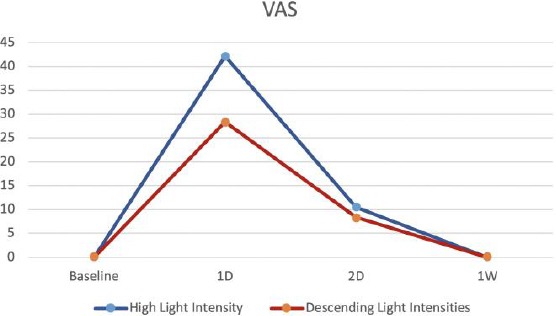
Line graph chart showing VAS at different periods within each bleaching protocol
In both high and descending light intensities protocols, the significantly highest VRS and VAS values were recorded 1-day post- bleaching, followed by those recorded 2-days post- bleaching. Then 1-week post- bleaches, there was no teeth sensitivity in both protocols.
In high light intensity protocol, values recorded 1-day post- bleaching by VRS (VRS Verbal Rating Scale), and VAS (Visual Analogue Scale) were (2.1 ± 0.7) and (42.1 ± 7.1) respectively. While descending light intensities protocol, values recorded 1-day post- bleaching by VRS and VAS were (1.3 ± 0.4) and (28.3 ± 15.5) respectively.
In high light intensity protocol, values recorded 2-days post- bleaching by VRS and VAS were (0.5 ± 0.5) and (10.5 ± 12.4) respectively. While descending light intensities protocol, values recorded 2-days post- bleaching by VRS and VAS were (0.3 ± 0.4) and (8.3 ± 12.3) respectively.
1.b. Effect of bleaching protocol on post-bleaching teeth sensitivity at each period:
Mean, Standard deviation (SD) of VRS and VAS and P-value for the effect of bleaching protocol on post-bleaching teeth sensitivity at each period are presented in Table 4, Figure 6 and Figure 7.
Table 4.
Statistical analysis for mean ± St. Deviation of VRS and VAS and P-value for the effect of bleaching protocol on post-bleaching teeth sensitivity at each period
| Baseline | 1-day post-bleaching | 2-days post-bleaching | 1-week post-bleaching | ||
|---|---|---|---|---|---|
| VRS | High light intensity | 0 | 2.1 ± 0.7 | 0.5 ± 0.5 | 0 |
| Descending light intensities | 0 | 1.3 ± 0.4 | 0.3 ± 0.4 | 0 | |
| P-value | --- | 0.006* | 0.418NS | --- | |
| VAS | High light intensity | 0 | 42.1 ± 7.1 | 10.5 ± 12.4 | 0 |
| Descending light intensities | 0 | 28.3 ± 15.5 | 8.3 ± 12.3 | 0 | |
| P-value | --- | 0.019* | 0.435NS | --- | |
: significant (p ≤ 0.05); NS: non-significant (p > 0.05).
Figure 6.
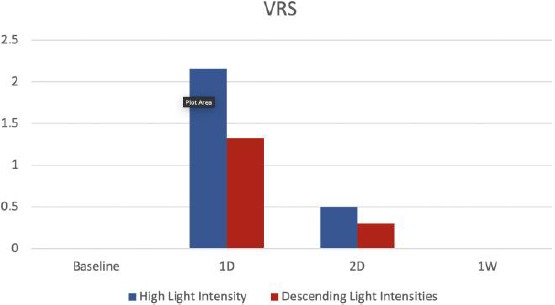
Bar chart showing VRS of both bleaching protocols at each period
Figure 7.
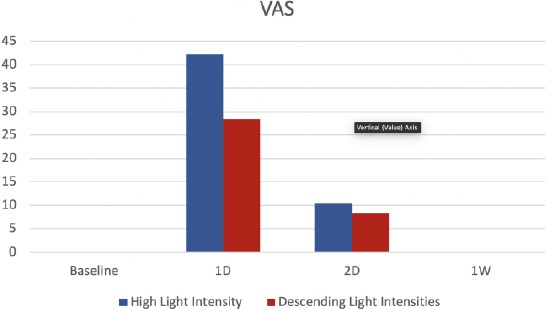
Bar chart showing VAS of both bleaching protocols at each period
At 1-day post bleaching, descending light intensities recorded lower sensitivity values than high light intensities at both scales. Mann-Whitney test showed that there was a statistically significant difference between both high and descending light intensities protocols after 1-day in VRS and VAS values (p = 0.006 and p = 0.019, respectively).
While on 2-days post bleaching, descending light intensities recorded lower sensitivity values than high light intensity at both scales. But there was no statistically significant difference between both protocols in VRS and VAS values on 2-days post bleaching (p = 0.418 and p = 0.435, respectively).
On 1-week post bleaching, descending light intensities and high light intensity protocols recorded zero sensitivity values at both scales.
Therefore, descending light intensities protocol scored lower sensitivity values than high light intensity protocol over the whole period time of investigation (1-day post, 2-days post and 1-week post).
2. Colour change:
2.a. Effect of bleaching protocol on colour change in shade guide units (SGU):
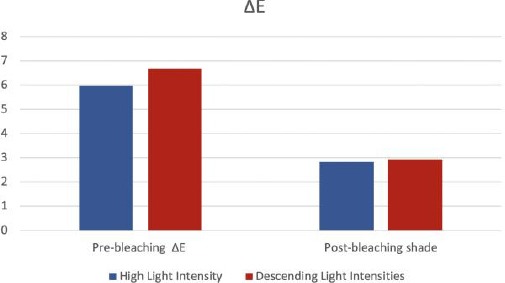
Mean, and Standard deviation (SD) for the effect of bleaching protocol on colour change in shade guide units (SGU) are presented in Table 5 and Figure 8.
Table 5.
Statistical analysis for mean ± St. deviation for the effect of bleaching protocol on colour change in shade guide units (SGU)
| Before bleaching | Post-bleaching | P-value | |
|---|---|---|---|
| High light intensity | 5.9 ± 3.1 | 2.8 ± 1.5 | 0.001* |
| Descending light intensities | 6.6 ± 1.3 | 2.9 ± 1.6 | 0.002* |
: significant (p ≤ 0.05); NS: non-significant (p > 0.05).
Figure 8.
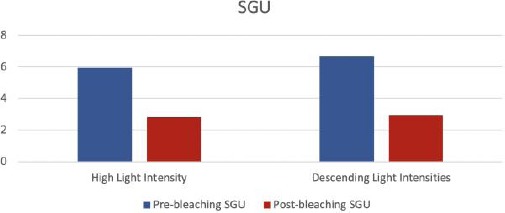
Bar chart showing a colour change in SGU within each bleaching protocol
High light intensity protocol yielded significant change in SGU [from 5.9 ± 3.1 to 2.8 ± 1.5] at (p = 0.001). Descending light intensities protocol led to significant change in SGU [from 6.6 ± 1.3 to 2.9 ± 1.6] at (p = 0.002). Thus, descending light intensities protocol had a slightly higher effect on colour change in shade guide units than high light intensity protocol effect.
2.b. Effect of each bleaching protocol on colour change in ΔE:
Mean, and Standard deviation for the effect of bleaching protocol on colour change in ΔE are presented in Table 6 and Figure 9.
Table 6.
Statistical analysis for mean ± St. Deviation for the effect of bleaching protocol on colour change in ΔE
| Before bleaching | Post-bleaching | P-value | |
|---|---|---|---|
| High intensity | 5.6 ± 2.1 | 4.3 ± 2.8 | 0.267NS |
| Descending intensities | 5.6 ± 1.7 | 5.3 ± 1.8 | 0.875NS |
*: significant (p ≤ 0.05); NS: non-significant (p > 0.05).
Figure 9.
Bar chart showing a colour change in ΔE within each bleaching protocol
High light intensity protocol yielded no significant change in ΔE (p = 0.267). Descending light intensities protocol also yielded no significant change in ΔE (p = 0.875).
2.c. Comparison of bleaching effectiveness (∆SGU) between both bleaching protocols:
Mean, and Standard deviation (SD) for the effect of bleaching effectiveness (∆SGU) between both bleaching protocols are presented in Table 7 and Figure 10.
Table 7.
Statistical analysis for mean ± St. deviation for the effect of bleaching effectiveness (∆SGU) between both bleaching protocols
| High intensity | Descending intensities | P-value | |
|---|---|---|---|
| ∆SGU | 3.1 ± 2.3 | 3.7 ± 2.7 | 0.726 NS |
*: significant (p ≤ 0.05); NS: non-significant (p > 0.05).
Figure 10.
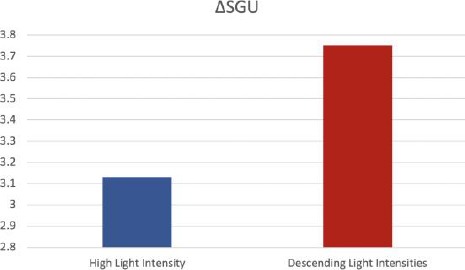
Bar chart showing ΔSGU of each bleaching protocol
There was no significant difference in ∆SGU recorded after teeth bleaching between high and descending light intensities protocols (p = 0.726).
2.d. Comparison of bleaching effectiveness (difference in ∆E) between both bleaching protocols:
Mean, and Standard deviation (SD) for the effect of bleaching effectiveness (difference in ΔE) between both bleaching protocols are presented in Table 8 and Figure 11.
Table 8.
Statistical analysis for mean ± St. deviation for the effect of bleaching effectiveness (ΔEdiff) between both bleaching protocols
| High intensity | Descending intensities | P-value | |
|---|---|---|---|
| Difference in ∆E | 1.3 ± 3.9 | 0.25 ± 2.2 | 0.165NS |
*: significant (p ≤ 0.05); NS: non-significant (p > 0.05).
Figure 11.
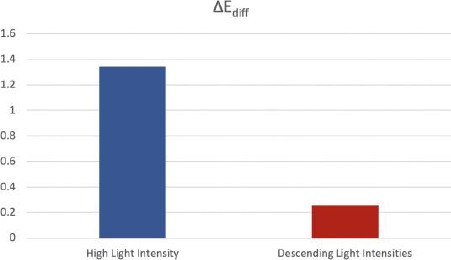
Bar chart showing the difference in ΔE of each bleaching protocol
Mann-Whitney test showed that there was no significant difference in ∆Ediff measured after teeth bleaching between high and descending light intensities protocols (p = 0.165).
Discussion
Tooth discolouration is caused by the presence of large organic compounds called chromogens, present within enamel and dentine that have conjugated double bonds in their chemical structure. Teeth bleaching works via the release of hydrogen peroxide (H2O2) either delivered directly as a concentrated bleaching agent or via the breakdown of carbamide peroxide upon contact with water [17]. H2O2 diffuses through enamel and dentine then breaks down into reactive free radicals that oxidise the chromogenic molecules into smaller molecules by breaking their double bonds [18].
This study was designed to assess teeth sensitivity using the bleaching protocol with descending different light intensities versus bleaching protocol with the same high light intensity. It was followed by one home bleaching kit in both groups.
All patients received dental prophylaxis before beginning the study, using a prophylaxis paste to remove extrinsic stains. The dental prophylaxis was performed before the teeth bleaching. It removes both saliva and polyphenols (such as tannins) on the tooth surface, which can inactivate reactive oxygen species [19].
It was evidenced that the in-office bleaching technique proved to be less efficient than home bleaching for removing stains deposited in dentin [20]. That’s why both in-office and home bleaching are recommended. Therefore, a bleaching protocol of in-office bleaching followed by home bleaching is advocated [21]. Concerning post bleaching teeth sensitivity, it is reported that teeth sensitivity is higher during the first 24 hours’ post-treatment [1]. This side effect extends for 5 days [1]. Thus, explain the duration one-week of assessing post bleaching sensitivity in this randomised clinical trial.
Different light sources have been used to activate bleaching agents, including halogen curing lights, ultraviolet and infrared lamps, plasma arcs, light-emitting diodes (LEDs), and lasers (CO2, argon, and diode lasers). Experimental studies and reviews showed controversial results regarding the effect of different forms of physical activation of in-office bleaching in colour enhancement of bleaching compared to non-activated bleaching [16], [22], [23]. The oxygen released from the hydrogen peroxide breaks down conjugated bonds in protein chains associated with stain into a single bond. This may result in more absorption of colour wavelengths and result in a reflection of colour (i.e., Lightening effect) [16], [24].
Descending light intensities protocol recorded lower sensitivity values than high light intensity protocol at both scales [13]. Due to the LED source produces the least thermal insult during the light activation process. And also, Blue LED light is optimal for photobleaching since it is not absorbed by water or hydroxyapatite. Thus, diffuse well through the tooth structure where it can remove chromophores that absorb blue/green light [19].
While UV (Ultra Violet) has very good photobleaching properties but does not diffuse well through teeth and causes pulp heating [19], thus, it confirms the high sensitivity values resulted from high light intensity bleaching protocol.
Contrarily, it was confirmed that the main success of the bleaching agents depends mainly on the nascent oxygen produced from the hydrogen peroxide, during the oxidation reaction and not on the light source, either LED lamps with the different intensities or UV lamp used [25].
It explained that descending light intensities protocol after day 1 and day 2 were lower than same high light intensity protocol. Due to lower rate production of free radicals, thus, allowing a rapid and large amount of inflammatory cells to react [26].
It was reported the increased release of substance P, a neuropeptide whose functions are linked to inflammation. It is evidenced after in-office bleaching associated with light/heat. While in the home bleaching, no increase in the release of SP and only slight histological changes were shown [9]. Therefore, sensitivity values were higher after both lights activated in-office bleaching protocols than home bleaching. Regarding the sensitivity results of this RCT, comes in agreement with El Hoshy et al., a study [27].
It embraced the high variability of the individual’s pain response among the population. Because of, positive emotional deposition which activate the central pain inhibitory system, and release endorphins that decrease painful sensations [28].
It was concluded that the LED lamp could increase the bleaching of HP by 0.4 units SGU [29]. The shade results were in agreement with previous studies [10], [27], [30], [31] and [32] that found that light application has markedly enhanced the lightening efficacy of bleaching materials.
While there was disagreement regarding shade, with other studied [33], [34] that reported no difference in efficacy between teeth bleached with or without different irradiation. They concluded that chemicals added to the bleaching gels acted as catalysts in the bleaching process and were only responsible for activation, whereas lights did not affect.
It has become obvious that blue LED light-activated teeth bleaching plays an important role in the generation of radicals and subsequent break down of stains. Contrarily, the bleaching process through UV is not advocated since it leads to thermal running through exothermic decomposition into water and oxygen.
Under the limitations of the current study, the following conclusions could be derived:
Descending different light intensities protocol showed a lower teeth sensitivity than high same light intensity protocol.
Descending light intensities protocol had a little higher effect on colour change in shade guide units (SGU) than high light intensity protocol effect.
A combination of in-office tooth bleaching with home bleaching with 22% carbamide peroxide for one week revealed a superior bleaching effect.
Further recommendations for this study:
Comparison between both investigated bleaching protocols in split-mouth study design.
Unify the baseline teeth shade into one shade.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Sulieman M. An Overview of Tooth Discoloration: Extrinsic, Intrinsic and Internalized Stains. J Restor Dent. 2005;32(8):463–8. doi: 10.12968/denu.2005.32.8.463. https://doi.org/10.12968/denu.2005.32.8.463 PMid:16262034. [DOI] [PubMed] [Google Scholar]
- 2.Tin-O MM, Saddki N, Hassan N. Factors influencing patient satisfaction with dental appearance and treatments they desire to improve aesthetics. J BMC Oral Health. 2011;11(6):1–8. doi: 10.1186/1472-6831-11-6. https://doi.org/10.1186/1472-6831-11-6 PMid:21342536 PMCid:PMC3059271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meireles SS, Goettems ML, Dantas RV, Bona ÁD, Santos IS, Demarco FF. Changes in oral health related quality of life after dental bleaching in a double-blind randomized clinical trial. J Dent. 2014;42(2):114–21. doi: 10.1016/j.jdent.2013.11.022. https://doi.org/10.1016/j.jdent.2013.11.022 PMid:24316342. [DOI] [PubMed] [Google Scholar]
- 4.American Dental Association Council on Scientific Affairs. Statement on the effectiveness of tooth whitening products. 2008 [Google Scholar]
- 5.Yu H, Zhang Chang CY, Cheng SL, Cheng H. Effects of bleaching agents on dental restorative materials:A review of the literature and recommendation to dental practitioners and researchers. J Esthet Restor Dent. 2018;30(2):52–60. [Google Scholar]
- 6.Pintado-Palomino K, Peitl Filho O, Zanotto ED, Tirapelli C. A clinical, randomized, controlled study on the use of desensitizing agents during tooth bleaching. J Dent. 2015;43(9):1099–105. doi: 10.1016/j.jdent.2015.07.002. https://doi.org/10.1016/j.jdent.2015.07.002 PMid:26159384. [DOI] [PubMed] [Google Scholar]
- 7.Kelleher M. Dental Bleaching (Quintessentials of Dental Practice: Operative Dentistry 6), 30 Sep. 2007 [Google Scholar]
- 8.Kugel G, Ferreira S, Sharma S, Barker ML, Gerlach RW. Clinical trial assessing light enhancement of in-office tooth whitening. J Esthet Restor Dent. 2009;21(5):336–47. doi: 10.1111/j.1708-8240.2009.00287.x. https://doi.org/10.1111/j.1708-8240.2009.00287.x PMid:19796303. [DOI] [PubMed] [Google Scholar]
- 9.De Almeida LC, Costa CA, Riehl H, Dos Santos PH, Sundfeld RH, Briso AL. Occurrence of sensitivity during at-home and in-office tooth bleaching therapies with or without use of light sources. J Acta Odontol Latinoam. 2012;25(1):3–8. [PubMed] [Google Scholar]
- 10.Reis A, Tay LY, Herrera DR, Kossatz S, Loguercio AD. Clinical effects of prolonged application time of an in-office bleaching gel. J Oper Dent. 2011;36(6):590–6. doi: 10.2341/10-173-C. https://doi.org/10.2341/10-173-C PMid:21913864. [DOI] [PubMed] [Google Scholar]
- 11.Moncada G, Sepúlveda D, Elphick K, Contente M, Estay J, Bahamondes V, Fernandez E, Oliveira OB, Martin J. Effects of light activation, agent concentration, and tooth thickness on dental sensitivity after bleaching. J Oper Dent. 2013;38(5):467–76. doi: 10.2341/12-335-C. https://doi.org/10.2341/12-335-C PMid:23391030. [DOI] [PubMed] [Google Scholar]
- 12.Mokhlis GR, Matis BA, Cochran MA, Eckert GJ. A clinical evaluation of carbamide peroxide and hydrogen peroxide whitening agents during daytime use. JADA. 2000;131(9):1269–77. doi: 10.14219/jada.archive.2000.0380. https://doi.org/10.14219/jada.archive.2000.0380 PMid:10986827. [DOI] [PubMed] [Google Scholar]
- 13.Kossatz S, Dalanhol AP, Cunha T, Loguercio A, Reis A. Effect of light activation on tooth sensitivity after in-office bleaching. J Oper Dent. 2011;36(3):251–7. doi: 10.2341/10-289-C. https://doi.org/10.2341/10-289-C PMid:21740236. [DOI] [PubMed] [Google Scholar]
- 14.Browning WD. Use of shade guides for color measurement in tooth-bleaching studies. J Esthet Restor Dent. 2003;15(Suppl 1):S13–20. doi: 10.1111/j.1708-8240.2003.tb00314.x. https://doi.org/10.1111/j.1708-8240.2003.tb00314.x. [DOI] [PubMed] [Google Scholar]
- 15.Dental Association. Acceptance program guidelines:dentist-dispensed home use tooth bleaching products. ADA Council of Scientific Affairs, Chicago. 2006 [Google Scholar]
- 16.Joiner A. The bleaching of teeth:a review of the literature. J Dent. 2006;34(7):412–9. doi: 10.1016/j.jdent.2006.02.002. https://doi.org/10.1016/j.jdent.2006.02.002 PMid:16569473. [DOI] [PubMed] [Google Scholar]
- 17.Carey CM. Tooth whitening:What we now know. J Evidence-Based Dental Practice. 2014;14(Suppl):70–76. doi: 10.1016/j.jebdp.2014.02.006. https://doi.org/10.1016/j.jebdp.2014.02.006 PMid:24929591 PMCid:PMC4058574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Floriani L, Freitas T, De Maria H, Rêgo C, Borges AB, Pucci CR, Torres G. Efficacy of Bleaching Treatment on Demineralized Enamel Treated with Resin Infiltration Technique. World Journal of Dentistry. 2012;3(4):279–283. https://doi.org/10.5005/jp-journals-10015-1173. [Google Scholar]
- 19.DeMoor RJG, Verheyen J, Diachuk A, Verheyen P, Meire MA, De Coster PJ, Keulemans F, Bruyne MD, Walsh LJ. Review Article:Insight in the Chemistry of Laser-Activated Dental Bleaching. Scientific World Journal 2015. 2015:650492. doi: 10.1155/2015/650492. https://doi.org/10.1155/2015/650492 PMid:25874251 PMCid:PMC4385672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.D'Arce MBF, Lima DANL, Aguiar FHB, Bertoldo CES, Ambrosano GMB, Lovadino JR. Effectiveness of dental bleaching in depth after using different bleaching agents. J Clin Exp Dent. 2013;5(2):e100–7. doi: 10.4317/jced.51063. https://doi.org/10.4317/jced.51063 PMid:24455056 PMCid:PMC3892220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dietschi D, Rossier S, Krejci I. In vitro colorimetric evaluation of the efficacy of various bleaching methods and products. J Quintessence Int. 2010;41(6):505–16. [PubMed] [Google Scholar]
- 22.Buchalla W, Attin T. External bleaching therapy with activation by heat, light or laser- Asystematic review. J Dent Mater. 2007;23(5):586–96. doi: 10.1016/j.dental.2006.03.018. https://doi.org/10.1016/j.dental.2006.03.018 PMid:16820199. [DOI] [PubMed] [Google Scholar]
- 23.He LB, Shao MY, Tan K, Xu X, Li JY. The effects of light on bleaching and tooth sensitivity during in-office vital bleaching:A systematic review and meta-analysis. J Dent. 2012;40(8):644–53. doi: 10.1016/j.jdent.2012.04.010. https://doi.org/10.1016/j.jdent.2012.04.010 PMid:22525016. [DOI] [PubMed] [Google Scholar]
- 24.Watts A, Addy M. Tooth discoloration and staining: a review of the literature. Br Dent J. 2001 Mar;190(6):309–16. doi: 10.1038/sj.bdj.4800959. Br Dent J. 2001; 190(6):309-16. https://doi.org/10.1038/sj.bdj.4800959 PMid:11325156. [DOI] [PubMed] [Google Scholar]
- 25.Joiner A, Philpotts CJ, Alonso C, Ashcroft AT, Sygrove NJ. A novel optical approach to achieving tooth whitening. J Dent. 2008;36(Suppl 1):S8–14. doi: 10.1016/j.jdent.2008.02.005. https://doi.org/10.1016/j.jdent.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 26.Amengual J, Forner L. Dentine hypersensitivity in dental bleaching:case report. J Minerva Stomatol. 2009;58(4):181–5. [PubMed] [Google Scholar]
- 27.El Hoshy AZ, Abouelenein K, El Baz M. In vivo comparative study between different light activated bleaching systems in terms of color and sensitivity. J Future Dent. 2018;4(2):262–267. https://doi.org/10.1016/j.fdj.2018.06.001. [Google Scholar]
- 28.Martin J, Fernandez E, Bahamondes V, Werner A, Elphick K, Oliveira OB, Jr, Moncada G. Dentin hypersensitivity after teeth bleaching with in-office systems. Randomized clinical trial. Am J Dent. 2013;26(1):10–4. [PubMed] [Google Scholar]
- 29.Ajaj RA, Chiappelli F, Phi L, Giroux A, Maida C, Garrett N, Polinovsky O. Systematic Review Evidence-based assessment of the efficacy and effectiveness of light/laser activation in in-office dental bleaching. J Dental Hypotheses. 2012;3(2):55–66. https://doi.org/10.4103/2155-8213.100388. [Google Scholar]
- 30.Matis BA, Cochran MA, Wang G, Eckert GJ. A Clinical Evaluation of Two In-office Bleaching Regimens with and without Tray Bleaching. J Oper Dent. 2009;34(2):142–9. doi: 10.2341/08-64. https://doi.org/10.2341/08-64 PMid:19363969. [DOI] [PubMed] [Google Scholar]
- 31.Torres CR, Barcellos DC, Batista GR, Borges AB, Cassiano KV, Pucci CR. Assessment of the effectiveness of light-emitting diode and diode laser hybrid light sources to intensify dental bleaching treatment. J Acta Odontol Scand. 2011;69(3):176–81. doi: 10.3109/00016357.2010.549503. https://doi.org/10.3109/00016357.2010.549503 PMid:21250920. [DOI] [PubMed] [Google Scholar]
- 32.Domínguez A, García JA, Costela A, Gómez C. Influence of the light source and bleaching gel on the efficacy of the tooth whitening process. J Photomed Laser Surg. 2011;29(1):53–9. doi: 10.1089/pho.2009.2751. https://doi.org/10.1089/pho.2009.2751 PMid:20969438. [DOI] [PubMed] [Google Scholar]
- 33.Hein DK, Ploeger BJ, Hartup JK, Wagstaff RS, Palmer TM, Hansen LD. In-office vital tooth bleaching-what do lights add? J Compend Contin Educ Dent. 2003;24(4A):340–52. [PubMed] [Google Scholar]
- 34.Bruzell EM, Johnsen B, Aalerud TN, Dahl JE, Christensen T. In vitro efficacy and risk for adverse effects of light-assisted tooth bleaching. J Photochem Photobiol Sci. 2009;8(3):377–85. doi: 10.1039/b813132e. https://doi.org/10.1039/b813132e PMid:19255679. [DOI] [PubMed] [Google Scholar]


