Abstract
Background:
Readmissions for skin disease, particularly for the same diagnosis and over time, have not been well studied.
Objective:
To characterize hospital readmissions for skin disease.
Methods:
A cross-sectional observational study was performed of the Nationwide Readmissions Database from 2010–2014, a national sample of hospital discharges in the United States.
Results:
Of 3,602,599 dermatologic hospitalizations from 2010–2014, 9.8% were readmitted for any cause and 3.3% for the same diagnosis within 30 days, and 7.8% for the same diagnosis within the calendar year (CY). The cost of all CY same-cause readmissions was $508 million per year. Mycosis fungoides had the highest 30 day all-cause readmission rate (32%), vascular hamartomas and dermatomyositis had the highest 30 day same-cause readmission rates (21%, 18%), and dermatomyositis and systemic lupus erythematosus had the highest CY same-cause readmission rates (31%, 24%). Readmission rates stayed stable from 2010–2014. Readmission for the same diagnosis was strongly associated with Medicaid and morbid obesity.
Limitations:
This study is a broad description of hospitalizations for skin disease. Conclusions for individual diseases are not intended.
Conclusion:
The rates and costs of readmissions for skin diseases have remained high from 2010–2014. This study identifies diseases that are high-risk for hospital readmissions, but disease-specific studies are needed. The diseases and risk factors presented should guide more focused studies on strategies to reduce readmissions in specific skin diseases.
Keywords: inpatient dermatology, hospital readmissions, epidemiology, cost of care, Nationwide Readmissions Database, dermatology hospitalizations, dermatology readmissions
CAPSULE SUMMARY
• Long term readmissions for skin diseases are poorly understood. We found high and stable rates and costs of readmissions, with $508 million per year spent on same cause readmissions.
• Identification of diseases at high-risk for readmissions should guide further efforts to reduce readmissions and costs.
INTRODUCTION
The burden of dermatologic disease management in the inpatient setting has been increasingly recognized in recent years. The cutaneous conditions prompting dermatologic consultation and contributing to inpatient admissions have been described1,2 and quantified,3,4 respectively. Furthermore, dermatologic consultation has been found to improve the management of these cutaneous conditions within the hospitalization.5–8 There are few studies of readmissions for skin disease, and the characteristics and costs of readmissions for the same diagnosis and over time in particular are not well understood. Identifying patterns of both short and long term readmissions can help inform efforts to reduce associated morbidity and costs. This study characterizes hospital readmissions for dermatologic disease using the largest dataset and the most years available in the United States.
METHODS
Study design and patient sample
A cross-sectional observational study was performed using the Nationwide Readmissions Database (NRD) from 2010 through 2014. The NRD is a national sample of hospital discharges from 18 participating states in 2010–2012, 21 states in 2013, and 22 states in 2014, comprising about 50% of all hospitalizations in the United States.9 The database includes uninsured patients and enrollees of all payer types, including Medicare, privately insured, and both fee for service and managed care Medicaid. Sample weights are provided for each admission, allowing for estimates of national admission numbers. Each admission contains a patient identification number, allowing linkage to all readmissions in the same state within the calendar year. Each data entry also contains principal and secondary diagnoses, patient demographics, hospital characteristics, and hospital charges. All data is de-identified and publicly available, thus the study was exempt from review by Institutional Review Board.
Disease selection
Admissions for dermatologic diseases were extracted using codes from the International Classification of Diseases, Ninth Revision (ICD-9) and diagnosis-related-groups (DRG). We first extracted all admissions from 2010–2014 with dermatology-specific DRGs 595, 596, 602, 603, 606, and 607 (major skin disorders, minor skin disorders, and cellulitis). We then compiled a list of all ICD-9 codes that were used in the principal diagnosis of these admissions. We also added ICD-9 codes for mycosis fungoides, Sézary syndrome, graft-versus-host disease, vasculitis with cutaneous involvement, systemic lupus erythematosus, systemic sclerosis, dermatomyositis, and eosinophilia myalgia syndrome; these were not under dermatology DRGs but were included in this study due to the importance of dermatologists in the management and comanagement of these diseases, including in specialty clinics and targeted fellowships such as cutaneous oncology and dermatology-rheumatology. The final set of dermatology-related hospitalizations was taken as any discharge with one of these ICD-9 codes as the principal diagnosis. ICD-9 codes for specifying different locations of the same disease were combined (i.e. “cellulitis” includes codes for head, trunk, and extremities).
Outcomes of interest
The primary outcomes were readmission rates, frequencies, and costs for each disease. Readmission rate is defined as the percentage of admissions with a repeat hospitalization within 30 days of discharge for short term evaluation or within the calendar year (CY) for long term evaluation. Only the first readmission is counted toward readmission frequencies. Only admissions prior to December were used in the calculation of 30 day readmission rates. Readmission numbers were calculated for both all cause (any diagnosis) and same cause (principal diagnosis of readmission is the same as that of the original hospitalization).
Statistical analysis
Data processing and statistical analysis were performed using MATLAB (version 76 R2017a, MathWorks, Natick, MA). Association of patient or hospital characteristics with readmission were evaluated using bivariate logistic regression with unadjusted odds ratios. The ten most common comorbidities were also evaluated for association with readmission. Costs were calculated from hospital charges using the cost-to-charge ratio files provided in the NRD and adjusted for inflation to year 2014 using the Consumer Price Index from the US Bureau of Labor Statistics.10 Readmission frequencies, rates, and costs were plotted against year to examine trends over time. Simple linear regression against time was used to determine P-values and significance of trends.
RESULTS
For all dermatologic diagnoses examined from 2010–2014, there were: 3,602,599 hospitalizations, 337,714 (9.8%) all cause readmissions within 30 days, 115,164 (3.3%) same cause readmissions within 30 days, and 282,320 (7.8%) same cause readmissions within CY. The inflation-adjusted cost of all dermatology-related hospitalizations 2010–2014 was $27.8 billion, and the cost of all CY same cause readmissions was $2.54 billion. The mean costs of each hospitalization and readmission were $7,841 (standard deviation [SD] $12,941) and $8,995 (SD $12,901), respectively.
The breakdown of patient demographics, hospital characteristics, and most common comorbidities are shown in Table 1. Unadjusted bivariate logistic regression showed highest 30 day all-cause readmission rates associated with increased age, female sex, Medicare insurance, large teaching hospitals in populous metropolitan areas, and congestive heart failure as a comorbidity. The highest same-cause readmission rates (both 30 day and CY) were associated with middle-age (18–64 years), female sex, Medicaid insurance, large teaching hospitals in populous metropolitan areas, and morbid obesity.
Table 1.
Patient demographics, hospital characteristics, and most common comorbidities in patients admitted for skin disease. Odds ratios presented are unadjusted from bivariate logistic regression.
Abbreviations: CY, calendar year; Hosp, hospitalizations; RR, readmission rate; OR, odds ratio; Ref, reference variable
| 30 day all cause readmission | 30 day same cause readmission | CY same cause readmission | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hosp, N | RR, % | OR (99% CI) | P | RR, % | OR (99% CI) | P | RR, % | OR (99% CI) | P | |
| All | 3602599 | 9.8 | 3.3 | 8.4 | ||||||
| Age | ||||||||||
| 0–17 (Ref) | 353009 | 4.8 | 1 | Ref | 2.5 | 1 | Ref | 4.4 | 1 | Ref |
| 18–44 | 960053 | 8.1 | 1.75 (1.71, 1.79) | <0.001 | 3.7 | 1.49 (1.45, 1.54) | <0.001 | 8.4 | 2.00 (1.96, 2.05) | <0.001 |
| 45–64 | 1197423 | 10.4 | 2.29 (2.24, 2.34) | <0.001 | 3.7 | 1.48 (1.44, 1.53) | <0.001 | 9.0 | 2.16 (2.11, 2.21) | <0.001 |
| 65–84 | 827838 | 12.0 | 2.70 (2.64, 2.77) | <0.001 | 2.9 | 1.14 (1.10, 1.18) | <0.001 | 7.4 | 1.74 (1.70, 1.79) | <0.001 |
| 85+ | 264276 | 13.3 | 3.03 (2.95, 3.11) | <0.001 | 2.7 | 1.05 (1.00, 1.09) | 0.0073 | 6.4 | 1.50 (1.45, 1.54) | <0.001 |
| Sex | ||||||||||
| Male (Ref) | 1852428 | 8.9 | 1 | Ref | 3.1 | 1 | Ref | 7.1 | 1 | Ref |
| Female | 1750171 | 10.8 | 1.23 (1.22, 1.24) | <0.001 | 3.6 | 1.20 (1.18, 1.22) | <0.001 | 8.6 | 1.23 (1.22, 1.25) | <0.001 |
| Insurance | ||||||||||
| Private (Ref) | 923454 | 6.8 | 1 | <Ref | 2.6 | 1 | Ref | 5.7 | 1 | Ref |
| Medicare | 1395910 | 13.0 | 2.04 (2.01, 2.07) | <0.001 | 3.4 | 1.31 (1.28, 1.34) | <0.001 | 8.7 | 1.57 (1.55, 1.59) | <0.001 |
| Medicaid | 721926 | 10.2 | 1.55 (1.52, 1.57) | <0.001 | 4.4 | 1.73 (1.69, 1.77) | <0.001 | 9.7 | 1.77 (1.74, 1.80) | <0.001 |
| Self-pay | 346045 | 5.8 | 0.85 (0.83, 0.87) | <0.001 | 2.9 | 1.11 (1.08, 1.15) | <0.001 | 6.5 | 1.14 (1.12, 1.17) | <0.001 |
| Other | 205647 | 7.4 | 1.09 (1.07, 1.12) | <0.001 | 3.2 | 1.24 (1.19, 1.29) | <0.001 | 7.2 | 1.27 (1.24, 1.30) | <0.001 |
| Zip code income quartile | ||||||||||
| 4th (Ref) | 654372 | 9.9 | 1 | Ref | 3.3 | 1 | Ref | 7.6 | 1 | Ref |
| 3rd | 795949 | 9.9 | 1.01 (0.99, 1.02) | 0.21 | 3.4 | 1.03 (1.01, 1.06) | <0.0019 | 7.8 | 1.03 (1.02, 1.05) | <0.001 |
| 2nd | 902011 | 9.8 | 0.99 (0.98, 1.01) | 0.12 | 3.3 | 1.00 (0.97, 1.02) | 0.63 | 7.8 | 1.04 (1.02, 1.06) | <0.001 |
| 1st | 1187259 | 9.7 | 0.98 (0.97, 1.00) | 0.0042 | 3.3 | 1.01 (0.99, 1.04) | 0.13 | 8.0 | 1.07 (1.05, 1.08) | <0.001 |
| Hospital bed size | ||||||||||
| Small (Ref) | 526826 | 8.7 | 1 | Ref | 3.3 | 1 | Ref | 7.8 | 1 | Ref |
| Medium | 893008 | 9.5 | 1.10 (1.09, 1.12) | <0.001 | 3.2 | 1.00 (0.97, 1.02) | 0.63 | 7.7 | 0.99 (0.97, 1.00) | 0.045 |
| Large | 2182765 | 10.2 | 1.20 (1.18, 1.22) | <0.001 | 3.4 | 1.05 (1.02, 1.07) | <0.001 | <0.001 | 1.02 (1.01, 1.04) | <0.001 |
| Hospital location | ||||||||||
| Non-urban (Ref) | 161905 | 7.5 | 1 | Ref | 2.7 | 1 | Ref | 7.0 | 1 | Ref |
| Micropolitan | 336703 | 8.7 | 1.17 (1.14, 1.21) | <0.001 | 2.8 | 1.05 (1.00, 1.10) | 0.015 | 7.1 | 1.00 (0.97, 1.03) | 0.93 |
| Small metropolitan | 1106347 | 9.7 | 1.33 (1.30, 1.37) | <0.001 | 3.1 | 1.18 (1.13, 1.23) | <0.001 | 7.3 | 1.04 (1.01, 1.07) | <0.001 |
| Large metropolitan | 1997645 | 10.3 | 1.42 (1.38, 1.45) | <0.001 | 3.6 | 1.36 (1.31, 1.42) | <0.001 | 8.3 | 1.20 (1.17, 1.23) | <0.001 |
| Hospital teaching status | ||||||||||
| Non-metropolitan (Ref) | 498608 | 8.3 | 1 | Ref | 2.8 | 1 | Ref | 7.1 | 1 | Ref |
| Metropolitan non-teaching | 1337382 | 9.7 | 1.19 (1.17, 1.21) | <0.001 | 3.2 | 1.17 (1.14, 1.21) | <0.001 | 7.8 | 1.12 (1.10, 1.14) | <0.001 |
| Metropolitan teaching | 1766609 | 10.4 | 1.28 (1.26, 1.30) | <0.001 | 3.6 | 1.32 (1.28, 1.35) | <0.001 | 8.1 | 1.16 (1.14, 1.18) | <0.001 |
| Comorbidities | ||||||||||
| Hypertension | 1271067 | 10.5 | 1.12 (1.11, 1.13) | <0.001 | 3.5 | 1.09 (1.07, 1.10) | <0.001 | 8.6 | 1.18 (1.17, 1.19) | <0.001 |
| Hyperlipidemia | 682989 | 11.3 | 1.21 (1.20, 1.22) | <0.001 | 3.2 | 0.94 (0.92, 0.96) | <0.001 | 7.9 | 1.00 (0.99, 1.02) | 0.61 |
| Smoking | 676758 | 8.9 | 0.88 (0.87, 0.89) | <0.001 | 3.8 | 1.17 (1.14, 1.19) | <0.001 | 8.7 | 1.15 (1.13, 1.16) | <0.001 |
| Type 2 diabetes | 605064 | 11.8 | 1.29 (1.27, 1.30) | <0.001 | 3.5 | 1.08 (1.06, 1.10) | <0.001 | 9.2 | 1.23 (1.21, 1.24) | <0.001 |
| Methicillin resistant Staph aureus | 454470 | 6.5 | 0.60 (0.59, 0.61) | <0.001 | 2.1 | 0.57 (0.56, 0.59) | <0.001 | 6.0 | 0.72 (0.71, 0.73) | <0.001 |
| Reflux | 422415 | 12.3 | 1.34 (1.32, 1.36) | <0.001 | 3.8 | 1.15 (1.12, 1.17) | <0.001 | 9.1 | 1.20 (1.19, 1.22) | <0.001 |
| Morbid obesity | 364720 | 12.5 | 1.37 (1.35, 1.39) | <0.001 | 4.9 | 1.59 (1.56, 1.63) | <0.001 | 13.8 | 2.07 (2.04, 2.10) | <0.001 |
| Hypothyroidism | 342772 | 12.9 | 1.41 (1.39, 1.43) | <0.001 | 3.8 | 1.15 (1.12, 1.18) | <0.001 | 9.4 | 1.24 (1.22, 1.26) | <0.001 |
| Depression | 323816 | 12.5 | 1.35 (1.33, 1.37) | <0.001 | 4.1 | 1.27 (1.24, 1.31) | <0.001 | 10.3 | 1.39 (1.37, 1.41) | <0.001 |
| Congestive heart failure | 318282 | 17.5 | 2.13 (2.10, 2.16) | <0.001 | 3.8 | 1.17 (1.14, 1.20) | <0.001 | 10.3 | 1.39 (1.37, 1.41) | <0.001 |
Table 2 shows readmission rates each year for the 10 most common dermatologic causes for hospitalization. Cellulitis was the most common diagnosis, comprising 83.6% of all admissions for dermatologic conditions. Table 3 lists the diseases with highest readmission rates and highest total CY same cause readmission costs, excluding those with less than 100 total hospitalizations from 2010–2014. Mycosis fungoides, Sezary syndrome, and graft-versus-host disease had the highest 30 day all cause readmission rates (32%, 29%, and 28% respectively). Vascular hamartomas, dermatomyositis, and thrombotic microangiopathy had the highest 30 day same cause readmission rates (21%, 18%, and 14% respectively). Dermatomyositis, systemic lupus erythematosus, and vascular hamartomas had the highest CY same cause readmission rates (31%, 24%, and 23% respectively). Cellulitis and systemic lupus erythematosus had the highest CY same cause readmission costs—$1.94 billion and $221 million, respectively, over years 2010–2014.
Table 2.
Readmission rates for the most common principal diagnoses in dermatology-related hospitalizations by year.
Abbreviations: Hosp, hospitalizations; 30-AC, 30 day all cause readmission rate; 30-SC, 30 day same cause readmission rate; CY-SC, calendar year same cause readmission rate; SLE, systemic lupus erythematosus
| 2010 | 2011 | 2012 | 2013 | 2014 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hosp, N | 30-AC, % | 30-SC, % | CY-SC, % | Hosp, N | 30-AC, % | 30-SC, % | CY-SC, % | Hosp, N | 30-AC, % | 30-SC, % | CY-SC, % | Hosp, N | 30-AC, % | 30-SC, % | CY-SC, % | Hosp, N | 30-AC, % | 30-SC, % | CY-SC, % | |
| All | 744617 | 9.8 | 3.3 | 7.7 | 736241 | 9.8 | 3.3 | 7.8 | 729310 | 9.9 | 3.3 | 7.9 | 699159 | 9.7 | 3.4 | 7.9 | 693272 | 9.8 | 3.4 | 7.9 |
| Cellulitis | 618571 | 9.2 | 3.1 | 7.7 | 613230 | 9.2 | 3.2 | 7.9 | 611208 | 9.3 | 3.2 | 8.1 | 587030 | 9.1 | 3.3 | 8.1 | 582711 | 9.2 | 3.3 | 8.0 |
| SLE | 14900 | 24.9 | 13.0 | 26.0 | 14700 | 24.4 | 13.1 | 24.5 | 14358 | 25.5 | 13.8 | 25.3 | 13453 | 23.9 | 12.9 | 23.1 | 12933 | 23.1 | 11.2 | 22.4 |
| Drug rash | 7672 | 11.7 | 1.1 | 1.3 | 7634 | 11.3 | 0.9 | 1.0 | 7638 | 10.7 | 0.7 | 0.8 | 6929 | 11.9 | 1.1 | 1.3 | 7098 | 11.3 | 0.9 | 1.1 |
| Herpes zoster | 7784 | 12.2 | 0.5 | 0.6 | 7707 | 12.0 | 0.6 | 0.8 | 7458 | 11.8 | 0.9 | 1.2 | 6200 | 12.4 | 0.7 | 1.0 | 6164 | 11.5 | 0.7 | 0.9 |
| Hidradenitis | 3740 | 12.6 | 6.1 | 18.2 | 3992 | 11.1 | 5.5 | 17.5 | 4242 | 14.7 | 7.4 | 20.5 | 4077 | 12.7 | 6.4 | 17.1 | 4398 | 13.6 | 6.8 | 19.9 |
| Kawasaki | 4804 | 12.8 | 9.1 | 8.8 | 3857 | 6.7 | 5.3 | 5.3 | 3008 | 5.3 | 4.3 | 4.8 | 3560 | 7.7 | 5.7 | 5.5 | 4198 | 8.2 | 5.3 | 5.6 |
| Pilonidal cyst | 4259 | 3.2 | 0.6 | 1.8 | 3904 | 3.8 | 0.7 | 1.9 | 3928 | 3.4 | 0.7 | 2.1 | 3722 | 3.9 | 1.3 | 3.5 | 3502 | 4.7 | 0.8 | 3.4 |
| Melanoma | 3573 | 9.2 | 1.5 | 3.9 | 3458 | 11.4 | 3.0 | 4.5 | 3157 | 8.2 | 1.7 | 4.0 | 2976 | 8.8 | 1.6 | 3.8 | 2751 | 9.1 | 1.6 | 3.8 |
| Urticaria | 3392 | 6.5 | 0.8 | 1.1 | 3418 | 6.3 | 1.2 | 1.5 | 2918 | 5.1 | 0.4 | 0.6 | 2612 | 6.2 | 0.5 | 1.1 | 2397 | 7.0 | 0.3 | 0.7 |
| Swelling in head and neck | 3156 | 9.8 | 0.1 | 0.5 | 2892 | 12.4 | 0.5 | 1.0 | 2869 | 11.3 | 0.4 | 0.6 | 2641 | 12.0 | 0.3 | 0.6 | 2422 | 12.2 | 0.6 | 0.6 |
Table 3.
Principal diagnoses with the highest readmission rates (30 day all-cause, 30 day same cause, and calendar year same cause) and total calendar year same cause readmission costs (calendar year same cause). Readmission frequencies are totaled over 2010–2014. Diagnoses with less than 100 total hospitalizations from 2010–2014 are excluded.
Abbreviations: CY, calendar year; NOS, not otherwise specified
| 30 day all-cause readmissions, N (readmission rate, %) | 30 day same-cause readmissions, N (readmission rate, %) | CY same-cause readmissions, N (readmission rate, %) | Total CY same-cause readmission cost, million $ | ||||
|---|---|---|---|---|---|---|---|
| Mycosis fungoides | 2728 (32.3) | Vascular hamartomas | 35 (21.1) | Dermatomyositis | 2016 (30.8) | Cellulitis | 1942 |
| Sezary syndrome | 77 (29.2) | Dermatomyositis | 1115 (18.3) | Systemic lupus erythematosus | 17108 (24.3) | Systemic lupus erythematosus | 221 |
| Graft-versus-host disease | 44 (28.2) | Thrombotic microangiopathy | 1233 (13.7) | Vascular hamartomas | 40 (22.7) | Thrombotic microangiopathy | 50.4 |
| Dermatomyositis | 1626 (26.6) | Systemic lupus erythematosus | 8541 (12.8) | Alopecia NOS | 37 (22.6) | Hidradenitis | 47.5 |
| Pityriasis rubra pilaris | 40 (26.2) | Pityriasis rubra pilaris | 15 (10.6) | Morphea | 95 (18.8) | Mycosis fungoides | 42.9 |
| Kaposi sarcoma | 47 (25) | Pemphigus | 199 (9.2) | Hidradenitis | 3822 (18.7) | Dermatomyositis | 29.3 |
| Calcinosis cutis, necrobiosis lipoidica, and other degenerative / depositional skin disease | 369 (24.8) | Henoch-Schonlein purpura | 708 (8.1) | Thrombotic microangiopathy | 1614 (16.9) | Systemic sclerosis | 21.4 |
| Systemic lupus erythematosus | 16323 (24.4) | Sezary syndrome | 20 (7.9) | Pityriasis rubra pilaris | 23 (16.3) | Granulomatosis with polyangiitis | 21.4 |
| Vascular hamartomas | 40 (24) | Granulomatosis with polyangiitis | 582 (7) | Pemphigus | 369 (16.2) | Pyoderma | 12.0 |
| Thrombotic microangiopathy | 1990 (22.2) | Pyoderma gangrenosum | 331 (6.6) | Pyoderma gangrenosum | 830 (15.3) | Squamous cell carcinoma | 10.7 |
| Cutaneous small vessel vasculitis NOS | 1297 (21.6) | Alopecia NOS | 9 (6.6) | Systemic sclerosis | 1249 (14.4) | Scar and fibrosis of skin | 10.3 |
| Human herpes virus 6 | 27 (21.3) | Hidradenitis | 1258 (6.5) | Mycosis fungoides | 1224 (13.9) | Skin cancer NOS | 10.2 |
| Morphea | 94 (19.9) | Mycosis fungoides | 536 (6.3) | Congenital skin disorders NOS | 135 (12.3) | Cutaneous small vessel vasculitis | 10.1 |
| Polyarteritis nodosa | 657 (19.6) | Systemic sclerosis | 512 (6.2) | Psoriasis | 671 (12.3) | Kawasaki disease | 8.17 |
| Systemic sclerosis | 1581 (19.3) | Morphea | 29 (6.2) | Granulomatosis with polyangiitis | 1067 (12) | Melanoma | 7.48 |
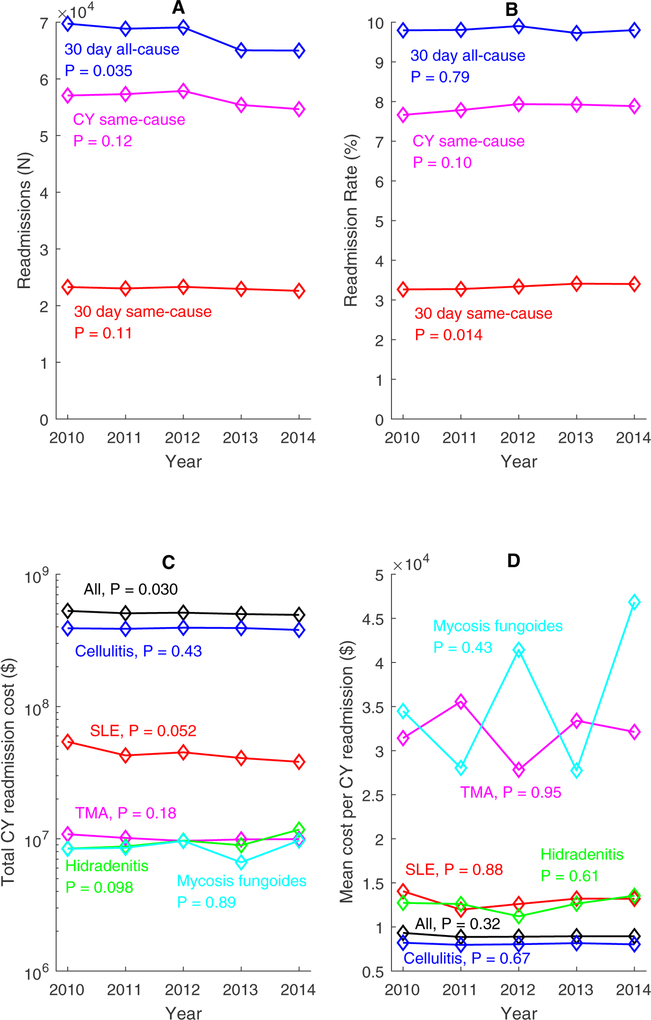
The trends in readmissions for all diseases from year to year are shown in Figure 1. Readmission frequencies for all three measures exhibited a general decrease over time (range of 3–7% decreases from 2010 to 2014), but the rates of readmission stayed stable (range of 0–0.2% increases from 2010 to 2014). Trends in total and mean CY readmission costs for the five most costly diseases are also shown in Figure 1. All-disease total costs showed a decreasing trend (7% decrease from 2010 to 2014). Systemic lupus erythematosus was the only disease to show a decreasing trend in total cost (29% decrease from 2010 to 2014). The total cost of hidradenitis showed an increasing trend (39% increase from 2010 to 2014). There were no clear trends in total costs of cellulitis, thrombotic microangiopathy, or mycosis fungoides. Mean cost per CY readmission for all diseases decreased 5% from 2010 to 2011 but remained stable from 2011–2014 (< 1.2% variation). Mean costs of single diseases fluctuated from year to year with no clear trend.
Figure 1.
Readmission frequencies, rates, and costs over time from 2010 through 2014. (A) Yearly readmission frequencies from 2010–2014. (B) Readmission rates from 2010–2014. (C) Total cost of calendar year same cause readmissions from 2010–2014, plotted on log-linear scale. (D) Mean cost per calendar year same cause readmission from 2010–2014.
Abbreviations: CY, calendar year; SLE, systemic lupus erythematosus; TMA, thrombotic microangiopathy
DISCUSSION
Of 721,000 mean hospitalizations per year for dermatologic diagnoses from 2010–2014, 9.8% were readmitted within 30 days for any cause and 3.3% for the same diagnosis as the initial admission. 7.8% were readmitted for the same diagnosis within the CY, costing $508 million per year.
There are very few prior studies of readmissions for skin disease. A recent study by Arnold et al. examined readmissions in the context of all-cause readmissions within 30 days in 2014.11 Their finding of cutaneous lymphoma having the highest 30 day all-cause readmission rate is consistent with ours. We also found that graft-versus-host disease, which was not examined by Arnold et al., had the next highest 30-day all-cause readmissions rate after cutaneous lymphoma. To our knowledge, dermatologic readmissions for the same cause and over a longer term and disease-specific readmission costs have not been previously studied. The disease profile for highest same-cause readmission rates was different, with connective tissue diseases, vasculitides/vasculopathies, hidradenitis, and pemphigus having higher readmission rates than mycosis fungoides. Demographics associated with same-cause and all-cause readmissions were also different.
All-cause readmissions were associated with increased age and Medicare insurance, which may reflect increased comorbidities and fragility and potential loss of social support in elderly patients. On the other hand, readmission for the same skin disease was associated with middle age (18–64 years), which may suggest increased prevalence of chronic and autoimmune skin diseases in this age group. Same-cause readmission was also associated with Medicaid insurance. This may be due to barriers to outpatient access and post-hospitalization follow up. Studies have found only 1.4% of Medicaid enrollees see a dermatologist annually vs. 5.5% of patients with private insurance.12 Medicaid patients were also shown to have lower acceptance rate (30% vs. 91% for privately insured) and longer wait time (66 days vs. 31 days for privately insured) to a dermatologist.13 The single characteristic associated with highest same-cause readmission rate was morbid obesity. This may relate to the incidence of cellulitis in this dataset, for which obesity is a known risk factor as well as coexisting secondary lymphedema, venous insufficiency, and delayed healing.14–16 The high rates of misdiagnosis of cellulitis may also contribute; studies have found 31% of cellulitis diagnoses are misdiagnosed and 74% of dermatology consultations for cellulitis were actually pseudocellulitis.7,17 Pseudocellulitis—mimickers of cellulitis, such as stasis dermatitis and lymphedema—is often associated with obesity and does not require admission but will persist and result in unnecessary readmissions if treated incorrectly as cellulitis.18 Higher all-cause and same-cause readmission rates for females may be attributed to the high readmission frequencies of systemic lupus erythematosus and dermatomyositis, which are more common in females.19,20 Increased rate of all readmission types at large metropolitan teaching hospitals is likely due to increased complexity of patients at these hospitals.
Mycosis fungoides, SLE, and dermatomyositis had high short and long term same-cause and all-cause readmission rates. Vascular hamartomas had the highest 30 day same cause readmission rate. The corresponding ICD-9 code (757.32) is a subcategory of congenital skin anomalies. Prior studies have shown this code used for port wine stains and hemangiomas in the pediatric inpatient setting,21 as well as cutis marmorata telangiectatica congenita.22 A recent study showed delayed presentation to specialists for infantile hemangiomas in patients with Medicaid or assisted insurance programs, which again highlights the need to address barriers to access.23 Along with many other diseases with high readmission rates in Table 3, these conditions with frequent readmissions should lower the threshold for obtaining dermatology consultation, which has been shown to decrease readmission8 and alter diagnosis and management, for example changing diagnosis in 45% of cases and stopping unnecessary antibiotics.3,6,7 Knowledge of the high readmission rates for these diseases can also inform efforts to keep these patients out of the hospital. Many of the skin diseases with the highest rates of CY readmissions—such as morphea, hidradenitis suppurativa, pityriasis rubra pilaris, pemphigus, pyoderma gangrenosum, and psoriasis—are generally managed in the outpatient setting, again highlighting the importance of addressing barriers to access. Urgent care dermatology clinics have been shown to circumvent referral to the emergency department and result in decreased visit times and healthcare and patient costs compared to emergency department visits.24–26 Providing same day appointments for patients with flares in cutaneous lymphoma or connective tissue disease, dermatology involvement in multidisciplinary clinics, or utilizing teledermatology to improve access to medically underserved populations27 may reduce readmissions and costs.
While total readmissions showed a general decreasing trend from 2010–2014, the rates of readmission have remained constant. This implies that total admissions are decreasing but not readmission rates, suggesting potential improvements in outpatient management of skin diseases but room for improvement in inpatient care. The cost of readmissions for cellulitis alone was $389 million per year and shows no sign of decreasing. While some diseases such as systemic lupus erythematosus show a decreasing trend in yearly costs, those of other diseases like hidradenitis show increases. These high costs highlight the importance of investment in inpatient dermatology services and coordination between inpatient and outpatient dermatology care in an effort to reduce readmissions and save health care dollars.
Limitations of this study include the use of ICD-9 codes to identify diseases, potentially entered by non-dermatologists. However, this is a descriptive study of many diseases as a whole and is not intended to present or test hypotheses for individual skin diseases. Furthermore, ICD 9 codes are examined only in the context of principal discharge diagnoses, which are generally entered with greater attention than secondary diagnoses. Given analysis of only principal diagnoses, the readmission rates for skin disease may be underestimated due to the omission of events where the skin disease was coded as a secondary diagnosis. Sampling error is another limitation that comes with using the NRD. While the NRD provides weights to estimate national frequencies, it is collected from about half of all hospitalizations and states and may not be nationally representative, particularly for rare diseases. In addition, the use of calendar year readmissions underestimates the total number of year-long readmissions, since patients are re-identified after January 1st of every year. Thus a patient with an index hospitalization in September would only include 4 months of tracking compared to 12 months for a patient admitted in January. We used an unadjusted bivariate model to evaluate associations of patient and hospital characteristics with readmission. We did not use a multivariable model due to the broad nature of this study and large number of diseases being examined. Thus, conclusions cannot be made about causation or independent predictors of readmission. Targeted research on individual diseases is needed to examine predictors of readmission more closely.
CONCLUSION
We describe skin conditions requiring hospitalization accounting for a large number of both short and long term readmissions and associated healthcare costs. Diseases, characteristics, and comorbidities associated with high readmission rates should trigger hospitals to consider dermatology consultation, coordinate outpatient follow-up, and support underinsured outpatient access. These measures have been shown to reduce readmissions or hospital visits in general dermatologic settings, but outcomes in individual diseases are not well-studied. This characterization of readmissions should guide future studies on disease specific risk factors and mitigation strategies to reduce readmissions.
Funding sources:
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748.
ABBREVIATIONS
- CY
calendar year
- NRD
Nationwide Readmissions Database
- ICD-9
International Classification of Diseases, Ninth Revision
- DRG
diagnosis-related-groups
- SD
standard deviation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None declared
IRB approval: Exempt
REFERENCES
- 1.Phillips GS, Freites-Martinez A, Hsu M, et al. Inflammatory dermatoses, infections, and drug eruptions are the most common skin conditions in hospitalized cancer patients. J Am Acad Dermatol. December 19 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Storan ER, McEvoy MT, Wetter DA, et al. Experience of a year of adult hospital dermatology consultations. Int J Dermatol. October 2015;54(10):1150–1156. [DOI] [PubMed] [Google Scholar]
- 3.Hu L, Haynes H, Ferrazza D, Kupper T, Qureshi A. Impact of specialist consultations on inpatient admissions for dermatology-specific and related DRGs. J Gen Intern Med. November 2013;28(11):1477–1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kirsner RS, Yang DG, Kerdel FA. Dermatologic disease accounts for a large number of hospital admissions annually. J Am Acad Dermatol. December 1999;41(6):970–973. [DOI] [PubMed] [Google Scholar]
- 5.Bauer J, Maroon M. Dermatology inpatient consultations: a retrospective study. J Am Acad Dermatol. March 2010;62(3):518–519. [DOI] [PubMed] [Google Scholar]
- 6.Falanga V, Schachner LA, Rae V, et al. Dermatologic consultations in the hospital setting. Arch Dermatol. August 1994;130(8):1022–1025. [PubMed] [Google Scholar]
- 7.Ko LN, Garza-Mayers AC, St John J, et al. Effect of Dermatology Consultation on Outcomes for Patients With Presumed Cellulitis: A Randomized Clinical Trial. JAMA Dermatol. February 16 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Milani-Nejad N, Zhang M, Kaffenberger BH. Association of Dermatology Consultations With Patient Care Outcomes in Hospitalized Patients With Inflammatory Skin Diseases. JAMA Dermatol. June 1 2017;153(6):523–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agency for Healthcare Research and Quality, Rockville, MD. HCUP Nationwide Readmissions Database (NRD). Healthcare Cost and Utilization Project (HCUP). 2010–2014; https://www.hcup-us.ahrq.gov/db/nation/nrd/nrddbdocumentation.jsp.
- 10.Bureau of Labor Statistics, US Department of Labor. Consumer Price Index Detailed Reports. 2010–2014; https://www.bls.gov/cpi/tables/detailed-reports/home.htm.
- 11.Arnold JD, Crockett RM, Kirkorian AY. Hospital readmissions among patients with skin disease: A retrospective cohort study. J Am Acad Dermatol. October 2018;79(4):696–701. [DOI] [PubMed] [Google Scholar]
- 12.Mulcahy A, Mehrotra A, Edison K, Uscher-Pines L. Variation in dermatologist visits by sociodemographic characteristics. J Am Acad Dermatol. May 2017;76(5):918–924. [DOI] [PubMed] [Google Scholar]
- 13.Alghothani L, Jacks SK, Vander Horst A, Zirwas MJ. Disparities in access to dermatologic care according to insurance type. Arch Dermatol. August 2012;148(8):956–957. [DOI] [PubMed] [Google Scholar]
- 14.Bjornsdottir S, Gottfredsson M, Thorisdottir AS, et al. Risk factors for acute cellulitis of the lower limb: a prospective case-control study. Clin Infect Dis. November 15 2005;41(10):1416–1422. [DOI] [PubMed] [Google Scholar]
- 15.Hirschmann JV, Raugi GJ. Lower limb cellulitis and its mimics: part I. Lower limb cellulitis. J Am Acad Dermatol. August 2012;67(2):163.e161–112; quiz 175–166. [DOI] [PubMed] [Google Scholar]
- 16.Quirke M, Ayoub F, McCabe A, et al. Risk factors for nonpurulent leg cellulitis: a systematic review and meta-analysis. Br J Dermatol. August 2017;177(2):382–394. [DOI] [PubMed] [Google Scholar]
- 17.Strazzula L, Cotliar J, Fox LP, et al. Inpatient dermatology consultation aids diagnosis of cellulitis among hospitalized patients: A multi-institutional analysis. J Am Acad Dermatol. July 2015;73(1):70–75. [DOI] [PubMed] [Google Scholar]
- 18.Levell NJ, Wingfield CG, Garioch JJ. Severe lower limb cellulitis is best diagnosed by dermatologists and managed with shared care between primary and secondary care. Br J Dermatol. June 2011;164(6):1326–1328. [DOI] [PubMed] [Google Scholar]
- 19.Gaubitz M Epidemiology of connective tissue disorders. Rheumatology (Oxford). October 2006;45 Suppl 3:iii3–4. [DOI] [PubMed] [Google Scholar]
- 20.Petri M Epidemiology of systemic lupus erythematosus. Best Pract Res Clin Rheumatol. December 2002;16(5):847–858. [DOI] [PubMed] [Google Scholar]
- 21.Penate Y, Borrego L, Hernandez N, Islas D. Pediatric dermatology consultations: a retrospective analysis of inpatient consultations referred to the dermatology service. Pediatr Dermatol. Jan-Feb 2012;29(1):115–118. [DOI] [PubMed] [Google Scholar]
- 22.Wright DR, Frieden IJ, Orlow SJ, et al. The misnomer “macrocephaly-cutis marmorata telangiectatica congenita syndrome”: report of 12 new cases and support for revising the name to macrocephaly-capillary malformations. Arch Dermatol. March 2009;145(3):287–293. [DOI] [PubMed] [Google Scholar]
- 23.Lie E, Psoter KJ, Püttgen KB. Lower Socioeconomic Status is Associated with Delayed Access to Care for Infantile Hemangioma, a Cohort Study. J Am Acad Dermatol. 2018/10/01/ 2018. [DOI] [PubMed] [Google Scholar]
- 24.Jayakumar KL, Samimi SS, Vittorio CC, et al. Expediting patient appointments with dermatology rapid access clinics. Dermatol Online J. June 15 2018;24(6). [PubMed] [Google Scholar]
- 25.Rosenbach M, Kagan S, Leventhal S. Dermatology urgent care clinic: a survey of referring physician satisfaction. J Am Acad Dermatol. December 2013;69(6):1067–1069.e1061. [DOI] [PubMed] [Google Scholar]
- 26.Sempler J, Thomas F, Pettit J, Klein SZ. The value of urgent care dermatology. Int J Dermatol. August 28 2018. [DOI] [PubMed] [Google Scholar]
- 27.Uscher-Pines L, Malsberger R, Burgette L, Mulcahy A, Mehrotra A. Effect of Teledermatology on Access to Dermatology Care Among Medicaid Enrollees. JAMA Dermatol. August 1 2016;152(8):905–912. [DOI] [PubMed] [Google Scholar]