Abstract
Late onset non-ischemic cardiomyopathy is a rare manifestation of the presence of aberrant vessel from descending thoracic aorta to left lower lobe of lung. This congenital anomaly is associated with pulmonary sequestration. Our case was a 23-year-old male who was under observation since the age of 19 years for evaluation of shortness of breath, functional class II. He had history of professional athletic training and he denied consumption of any compound. Ejection fraction had deteriorated during three years from 45–50% to 40% and left ventricular size increased from normal size to mild enlargement. Cardiac computed tomography showed presence of aberrant artery from descending aorta to left lower pulmonary lobe with pulmonary sequestration. His cardiac function improved after successful coil embolization of aberrant vessel. In conclusion, pulmonary sequestration and aberrant pulmonary supply from aorta should be considered as a rare cause of dilated cardiomyopathy which can be reversible by proper intervention.
<Learning objective: Aberrant pulmonary supply from aorta could be considered in cases with dilated cardiomyopathy. Since this disease entity is reversible, earlier diagnosis is essential.>
Keywords: Aberrant vessel, Coil embolization, Left ventricular function, Pulmonary sequestration
Introduction
Bronchopulmonary sequestration is rare congenital anomaly. The undiagnosed aberrant systemic arterial supply to lung could lead to development of non-ischemic cardiomyopathy and congestive heart failure in adults [1]. Hereby, we report a case of reversible cardiomyopathy after coil embolization of aberrant vessel to lung.
Case report
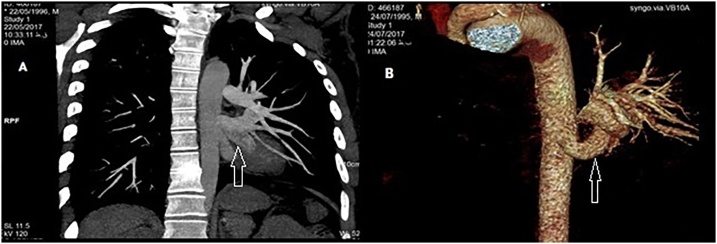
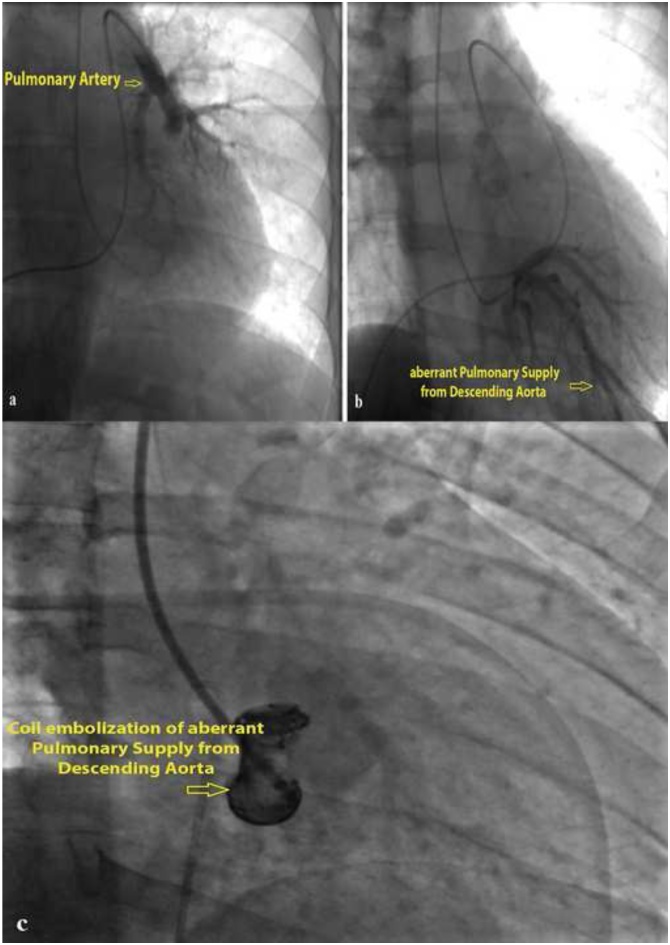
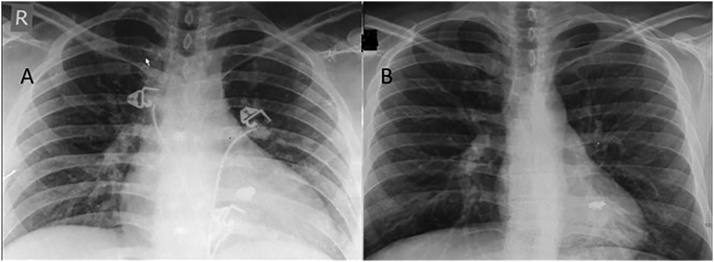
Our case was a 23-year-old male who was under observation since 4 years previously for evaluation of shortness of breath, functional class II. He had history of professional athletic training and he denied consumption of any compound. Ejection fraction had deteriorated during three years from 45–50% to 40% and left ventricular size increased from normal size to mild enlargement. Global hypokinesia, hyper trabeculated left ventricular apex and normal pulmonary artery pressure were noticeable. In echocardiography, no shunt was detected. At the end of the third year, right ventricle and left atrium showed mild enlargement and he was referred for further evaluation. Cardiac computed tomography was performed which showed aberrant artery from descending aorta to left lower pulmonary lobe with subsequent pulmonary sequestration (Fig. 1). Cardiac catheterization was done and confirmed the aberrant pulmonary artery connection to the left lower pulmonary lobe (Fig. 2a,b). He underwent successful coil embolization of the aberrant vessel (Fig. 2c) and was discharged without any complication. Left and right ventricular size decreased the following week on echocardiography to normal size and ejection fraction improved to 45%. Chest X-ray 6 months after coil embolization of aberrant pulmonary artery demonstrated reduced cardiothoracic ratio to the normal limits compared with immediately post-coil embolization (Fig. 3). On follow up, he became fully asymptomatic and is doing well.
Fig. 1.
A,B: Multi-slice computed tomography angiography shows large aortopulmonary collateral artery arising from descending aorta in to the lower lobe of left lung (white arrow).
Fig. 2.
(a) Pulmonary artery injection showed absent left lower lobe pulmonary artery. (b) Pulmonary artery injection showed aberrant pulmonary artery from descending aorta. (c) Coil embolization in aberrant pulmonary branch from descending aorta.
Fig. 3.
Chest X-ray 6 months after coil embolization of aberrant pulmonary artery demonstrated reduced cardiothoracic ratio to the normal limits compared with immediately post-coil embolization and also notes to the presence of metallic coil in left lower pulmonary lobe in both images.
Discussion
Congenital malformation of pulmonary lobe or segment due to aberrant blood supply directly from aorta is a rare anomaly [2]. Pulmonary symptoms such as recurrent infection and cough are the leading clues toward diagnosis [3]. Other symptoms of shortness of breath, chest pain, and hemoptysis are other pulmonary manifestations [4]. In the case of absence of pulmonary symptoms, cardiovascular symptoms due to congestive heart failure would manifest most commonly during the neonatal period or in childhood [5]. Thus, early diagnosis and treatment is essential before development of irreversible cardiac damage. Although this is rare, but in any case with deteriorated cardiac function in follow-up echocardiography, pulmonary sequestration and aberrant pulmonary supply from aorta may be considered as differential diagnosis. Currently, percutaneous arterial embolization of aberrant vessel has become a promising non-invasive approach as an alternative to surgery in symptomatic pulmonary sequestration cases [6]. This option brings hope for earlier treatment in cases with early diagnosis. As seen in our case, even earlier diagnosis and early trans-catheter coil embolization of aberrant vessel would cause improvement in symptoms and cardiac function.
Conclusions
Pulmonary sequestration and aberrant pulmonary supply from aorta should be considered as a rare cause of dilated cardiomyopathy which can be reversible by proper intervention.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Kim B.R., Jo J.H., Park B.H. Transarterial embolization treatment for aberrant systemic arterial supply to the normal lung: a case report and literature review. J Korean Soc Radiol. 2017;76:395–402. [Google Scholar]
- 2.Pescarus R., Rakovich G., Ouellette D., Beauchamp G. A patient with an aberrant pulmonary blood supply and recurrent infection. Can Respir J. 2010;17:e94–e95. doi: 10.1155/2010/813106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gompelmann D., Eberhardt R., Heussel C.P., Hoffmann H., Dienemann H., Schuhmann M. Lung sequestration: a rare cause for pulmonary symptoms in adulthood. Respiration. 2011;82:445–450. doi: 10.1159/000323562. [DOI] [PubMed] [Google Scholar]
- 4.Petty L., Joseph A., Sanchez J. Case report: pulmonary sequestration in an adult. Radiol Case Rep. 2017;13:21–23. doi: 10.1016/j.radcr.2017.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martí V., Pujadas S., Casan P., García J., Guiteras P., Augé J.M. Reversible dilated cardiomyopathy after lobectomy for pulmonary sequestration. J Thorac Cardiovasc Surg. 2001;121:1001–1002. doi: 10.1067/mtc.2001.112320. [DOI] [PubMed] [Google Scholar]
- 6.Zener R., Bottoni D., Zaleski A., Fortin D., Malthaner R.A., Inculet R. Transarterial embolization of intralobar pulmonary sequestration in a young adult with hemoptysis. J Thorac Dis. 2017;9:E188–E193. doi: 10.21037/jtd.2017.02.82. [DOI] [PMC free article] [PubMed] [Google Scholar]