Abstract
Background:
Financial strain is a prevalent form of psychosocial stress in the United States; however, information about the relationship between financial strain and cardiovascular health remains sparse, particularly in older women.
Methods:
The cross-sectional association between financial strain and ideal cardiovascular health were examined in the Women’s Health Study follow-up cohort (N=22,048; mean age= 72 + 6.0 years). Six self-reported measures of financial strain were summed together to create a financial strain index and categorized into 4 groups: No financial strain, 1 stressor, 2 stressors, and 3+ stressors. Ideal cardiovascular health was based on the American Heart Association strategic 2020 goals metric, including tobacco use, body mass index, physical activity, diet, blood pressure, total cholesterol and diabetes mellitus. Cardiovascular health was examined as continuous and a categorical outcome (ideal, intermediate, and poor). Statistical analyses adjusted for age, race/ethnicity, education and income.
Results:
At least one indicator of financial strain was reported by 16% of participants. Number of financial stressors was associated with lower ideal cardiovascular health, and this association persisted after adjustment for potential confounders (1 financial stressor (FS): B = −0.10, 95% Confidence Intervals (CI) = −0.13, −0.07; 2 FS: B = −0.20, 95% CI = −0.26, −0.15; 3+ FS: B = −0.44, 95% CI = −0.50, −0.38).
Conclusion:
Financial strain was associated with lower ideal cardiovascular health in middle aged and older female health professional women. The results of this study have implications for the potential cardiovascular health benefit of financial protections for older individuals.
Keywords: Ideal cardiovascular health, psychosocial stress, aging, women, financial strain, cardiovascular disease risk
Introduction
Psychosocial stress is a cardiovascular disease risk factor that disproportionately affects women.1 Chronic psychosocial stress triggers the fight-or-flight response that over time is maladaptive and results in increased adrenergic tone, activation of the hypothalamic-pituitary-adrenal axis, and increased systemic inflammation.2,3 Psychosocial stress, especially as a result of traumatic life events, has been associated with cardiovascular disease outcomes including acute myocardial infarction in several cohorts.4–8 Financial strain is a commonly reported psychosocial stressor in the United States9, and is a particularly noxious form of psychosocial stress that has been largely studied in relation to mental health, perceived health, and health care utilization.1 The primary objective of this study was to determine the relationship between financial strain (and its individual components) and ideal cardiovascular health in middle-aged and older women.
There are limited data regarding the relationship between financial strain and cardiovascular disease, particularly in older women. Financial strain, as defined either individually by unemployment, job insecurity, perceived family financial situation, or self-rated financial hardship, has been examined as a risk factor for ischemic heart disease with mixed results.4,10–17 In the INTERHEART study, a large case-control study of 11,119 patients and 13,648 controls, severe financial stress was associated with increased acute myocardial infarction.4 An analysis of 749 women in the Framingham Study (1965–67) found that serious financial worries were associated with an increased relative risk of incident coronary artery disease among employed women.13 However, the majority of existing studies of financial strain and cardiovascular disease did not include a large sample of older women in the US, or multiple indicators of financial stress. To the best of our knowledge, limited information exists about the potential effect of financial strain on the cardiovascular health of older women, particularly in the setting of current economic conditions, which include longer life spans with fewer financial protections for elders.
The present study uses an ideal cardiovascular health index as a measure of general cardiovascular health. Ideal cardiovascular health was developed by the American Heart Association (AHA) Goals and Metrics Committee of the Strategic Planning Task Force to track the yearly progression of population-level cardiovascular disease risk through 7 salubrious behaviors and factors (Life’s Simple 7’s).18 Since the development of the ideal cardiovascular health index, several studies have focused on the impact of a variety of psychosocial and sociodemographic (e.g., income/education) factors and have found, generally, that greater psychosocial stress and lower socioeconomic status are associated with lower cardiovascular health.19–21
As the population of the United States ages in the midst of global and national economic volatility, an understanding of the health effects of financial strain in older women is critical. The aging population of women faces unique economic pressures that likely have consequences for their overall health and well-being22. Older women in the United States are participating in the workforce in greater numbers while making less money than middle-aged women.23 We hypothesize that greater financial strain will be associated with a reduction in ideal cardiovascular health. Because past research on ideal cardiovascular health has found that lower socioeconomic status is associated with poorer cardiovascular health,20,24 we further assess whether the relationship between financial strain and ideal cardiovascular health is modified by education level or income.
Method
Study Population
This is a study of the follow-up cohort of the Women’s Health Study (WHS), a completed randomized clinical trial of the effects of low dose aspirin, Vitamin E and beta carotene in the primary prevention of cancer and CVD, consisting of female health professionals age 45 years and older with no self-reported history of apparent CVD (N=39,876).25 Randomization for WHS began in April 1993 and follow-up for the clinical trial ended in March 2004. At the conclusion of the clinical trial in 2005, the women were invited to participate in ongoing follow-up. As 4,324 declined to participate in follow-up, 33, 796 consented to annual follow-up via mailed questionnaires, with greater than 95% morbidity and mortality follow-up. Cardiovascular and other health information is ascertained on the annual mailed questionnaire. Medical record follow-up for cardiovascular disease adjudication is obtained for participants who report a cardiovascular event (e.g., myocardial infarction). A cumulative psychosocial stress questionnaire was sent to all participants without known CVD who remained in the follow-up cohort, and 25, 335 women completed the survey, of which 22,048 had complete data on financial strain, representing 87% of the women. To assess self-reported sociodemographic information and health outcomes, follow-up questionnaires were conducted by mail every 6 months during the first year, and every year thereafter. Observational follow-up is still ongoing, with a median duration of follow-up of almost 24 years.
Participants in the WHS observational cohort with no known history of apparent CVD were invited to participate in the WHS stress study (2012–2013).26 A total of 25,335 participants were willing and eligible, and provided informed consent for the stress study. Women with no prior history of cancer and complete data on cumulative psychosocial stress and ideal cardiovascular health metrics were included in this analysis (N=22,048). Missing values for total cholesterol were imputed using the value from the data collection period immediately preceding the 2011–2012 follow-up assessment. Due to the small sample size of American Indian women (N=49) and women who reported their race/ethnicity as other (N=31), we combined these data together as other. Additionally, a small subset of the sample (N =34) were missing data on the financial strain items. This study was approved by the Institutional Review Boards of Brigham and Women’s Hospital and the University of California, San Francisco. Grant support for this research was made possible by grants from the National Institute of Aging (NIA), National Heart, Lung, and Blood Institute (NHLBI) and the National Cancer Institute (NCI). The authors were responsible for design, analyses, and drafting of the current paper.
Financial Strain
Financial strain in past 5 years was measured using four dichotomous (yes/no) items from an acute negative life events inventory: unemployed for three months or longer, having a member of the household be unemployed for longer than three months, moving to a worse residence or neighborhood, and serious financial problems or difficulties. In addition, we incorporated information from two continuous measures of financial security, each rated on a four-point scale: difficulty paying bills (“How difficult is it for you and your family to pay your monthly bills?”) and perception of family financial situation (“Which, in general, best describes the financial situation of you and your family?”). Ability to pay bills had the following response options: (1) We have more money than we need, (2) We have just enough money for our needs (3) We sometimes do not have enough money to meet our needs, and (4) Most times we do not have money to meet our needs. The following response options were used to assess the quality of perceived family financial situation: (1) very difficult, (2) somewhat difficult, (3) only occasionally difficult, and (4) not difficult at all. We dichotomized responses on these two continuous measures in order to combine them with the four acute financial events, such that individuals who reported not having enough money sometimes or most times for perceived family situation and/or who reported difficulty paying bills (i.e., very difficult or somewhat difficult) were classified as having a financial stressor. Using the six dichotomous variables (i.e., four finance-related events, two reports on current financial situation), we constructed a score (range: 0 to 6) by awarding one point for each reported event.
For the present analyses, the financial stress score was run as a continuous score and categorized into four categories: No financial strain, one financial stressor, two financial stressors, and three or more financial stressors, with individuals who reported no financial strain as the reference group. These categories were developed based on the distribution of the summed financial strain score, as less than 2% of respondents have scores above three: No financial strain (74.0%), 1 financial stressor (16.4%), 2 financial stressors (5.3%), 3 financial stressors (2.6%), 4 financial stressors (1.4%), 5 financial stressors (0.3%), and 6 financial stressors (0.1%).
We used a two-parameter logistic Item Response Theory (IRT27) to assess the latent unidimenionality of the 6 dichotomous financial strain items. Akin to factor analysis, IRT can be used with dichotomous items. The IRT eigenvalue (3.29) was >1, denoting that the six items captured an underlying financial strain factor and could be composited as a single score. Visual inspection of the scree plot also supported the existence of a single factor.
Ideal Cardiovascular Health
Ideal cardiovascular health is an index of seven cardiovascular health-enhancing behaviors and factors, based on the AHA Strategic 2020 Impact Goals18, including: body mass index (BMI); physical activity; a healthy diet pattern including adequate servings of fruits and vegetables; no smoking history or smoking cessation >one year; total cholesterol; blood pressure; and fasting glucose.18 All Components of ideal cardiovascular health (excluding diet) were ascertained for each participant using self-reported data from the stress study questionnaire in 2011–2012, and coded as ideal, intermediate, or poor, based on the definitions provided below. Diet information was collected from a validated 131-item self-reported food frequency questionnaire administered in 2004.28 Physical activity was measured through a validated measure developed by the College Alumni Health Study.29,30 The accuracy of self-reported health conditions in WHS, including blood pressure, diabetes and weight, is greater than 90% for most outcomes.31–37
For each component of ideal cardiovascular health, participants were given a score of 1 for ideal classification, a score of 0.5 for intermediate, and a score of 0 for poor. The scores for the 7 metrics were summed to give a total ideal cardiovascular health score ranging between 0 and 7, with 7 meaning ideal risk factor category for all components. In addition to a continuous score, the ideal cardiovascular health score was categorized into 3 groups: low (scores 0 – 3), intermediate (scores 3.5 – 5.5) and high (scores 6 – 7). Please see appendix for complete explanation of the ideal cardiovascular health construct.
Covariates
The present analyses include baseline age, race/ethnicity, education, and income as model covariates. Missingness on individual covariates was accounted for by creating an individual category for missing data (e.g., missing income was a category for income).
Statistical Analyses
First, we describe the distribution of the ideal cardiovascular health metrics and covariates by categories of financial strain. Multinomial logistic regression was then used to assess the association between the number of financial strain events and the categorical ideal cardiovascular health outcome. Three models were created to assess the role of potential confounding variables: Model 1 was unadjusted; Model 2 was only adjusted for age; and, Model 3 was adjusted for age, race/ethnicity, education, and income Next, we used linear regression analyses to examine the relationship between the total number of financial strain events and ideal cardiovascular health. We assessed whether the association between financial strain and ideal cardiovascular health varied by education or income by creating interaction terms and including each interaction term in separate regression models. In sensitivity analyses, we examined the association between each indicator of financial strain and ideal cardiovascular health, in order to observe whether associations were consistent across indicators. All analyses were performed in SAS 9.4. Additionally, as per the guidelines suggested by Field et al38, we examined the Tolerance and Variance Inflation Factor (VIF) of the individual predictors in the fully-adjusted model. Overall, the examination of the diagnostics suggest that multicollinearity is not an issue for our model. Significance value for all analyses was set to p < 0.05. All results are presented as Odds Ratios (OR) or unstandardized coefficients (B), unless otherwise noted.
Result
In this analysis, 22,048 women between the ages of 68 and 78 (mean age = 72.1, SD = 6.0) who completed the WHS Stress questionnaire were included, of which 16% reported at least one indicator of financial strain (Table 1). Relative to women who did not report any indicators of financial strain, women who reported at least one indicator of financial strain were younger, had less education and lower income, were less likely to drink alcohol, and to report symptoms of depression or anxiety. These associations were greater for women with more reported financial stressors. Moreover, women with 2 or more stressors had more prevalent hypertension, diabetes and obesity than those who reported no financial strain.
Table 1.
Baseline characteristics of participants in the Women’s Health Study according to the number of reported financial stressors
| Number of reported acute financial strain events | ||||||
|---|---|---|---|---|---|---|
| Total Sample | No Strain |
1 Stressor |
2 Stressors |
3+ Stressors |
||
| (N = 22, 048) | (N = 16,323) | (N = 3607) | (N = 1160) | (N = 958) | P | |
| Age at baseline, mean (SD) | 72.1 (6.0) | 72.3 (6.0) | 71.8 (6.0) | 71.6 (6.0) | 70.8 (5.5) | <0.001 |
| Race/ethnicity, % | <0.001 | |||||
| White | 94.7 | 95.3 | 92.9 | 92.3 | 93.6 | |
| Hispanic | 1.1 | 0.9 | 1.3 | 2.5 | 0.9 | |
| African American/black | 1.8 | 1.5 | 2.8 | 2.6 | 2.6 | |
| Asian/Pacific Islander | 1.31 | 1.3 | 1.7 | 1.1 | 0.7 | |
| Other | 0.30 | 0.3 | 0.5 | 0.7 | 0.8 | |
| Race/ethnicity missing | 0.77 | 0.7 | 0.8 | 0.8 | 1.3 | |
| Education, % | <0.001 | |||||
| 2 Year Health Professional Ed | 10.7 | 9.0 | 13.6 | 17.1 | 22.2 | |
| 3 Year Health Professional Ed | 41.0 | 41.4 | 40.2 | 38.8 | 40.5 | |
| Bachelors | 24.9 | 25.3 | 24.8 | 22.7 | 20.3 | |
| Masters | 16.5 | 17.2 | 15.0 | 15.6 | 12.3 | |
| Doctorate | 5.2 | 5.5 | 5.5 | 4.1 | 2.8 | |
| Education missing | 1.7 | 1.7 | 1.5 | 1.8 | 1.9 | |
| Income, % | <0.001 | |||||
| < $19,999 | 3.0 | 2.4 | 3.5 | 5.4 | 7.8 | |
| $20–29,999 | 7.4 | 6.4 | 8.8 | 11.1 | 14.4 | |
| $30–39,999 | 12.1 | 11.2 | 13.9 | 14.9 | 16.2 | |
| $40–49,999 | 15.6 | 15.2 | 16.2 | 17.8 | 16.7 | |
| $50–99,999 | 42.7 | 43.8 | 41.8 | 36.6 | 34.5 | |
| ≥ $100,000 | 13.9 | 15.1 | 11.6 | 8.8 | 6.8 | |
| Income missing | 5.5 | 5.8 | 4.3 | 5.4 | 3.7 | |
| Alcohol use, % | <.0001 | |||||
| Rarely/Never | 40.7 | 38.7 | 43.9 | 49.7 | 52.1 | |
| 1–3 glasses/month | 9.8 | 9.9 | 9.2 | 10.3 | 8.6 | |
| 1–6 glasses/week | 34.6 | 35.7 | 32.9 | 29.8 | 28.4 | |
| 1 + glasses/day | 14.9 | 15.7 | 14.0 | 10.1 | 11.0 | |
| Tobacco use, % | <.0001 | |||||
| Never | 50.1 | 49.9 | 51.5 | 51.0 | 45.7 | |
| Past | 45.1 | 45.8 | 43.3 | 43.3 | 44.3 | |
| Current | 4.8 | 4.3 | 5.2 | 5.7 | 10.0 | |
| METS h/wk, mean (SD) | 17.7 (16.7) | 18.5 (16.9) | 16.2 (16.0) | 15.1 (16.0) | 13.2 (15.2) | <.0001 |
| History of hypertension, % | 69.8 | 68.5 | 71.4 | 75.5 | 77.4 | <0001 |
| History of diabetes, % | 10.0 | 8.7 | 11.9 | 15.4 | 18.7 | <.0001 |
| Hypercholesterolemia, % | 73.5 | 72.8 | 75.4 | 76.0 | 76.5 | 0.0003 |
| Body Mass Index, kg/m2, % | <.0001 | |||||
| Normal/underweight | 42.7 | 44.8 | 39.7 | 34.3 | 28.4 | |
| Overweight | 34.1 | 34.4 | 34.0 | 31.5 | 32.2 | |
| Obese | 23.3 | 20.9 | 26.2 | 34.2 | 39.5 | |
| Depression/Anxiety, mean (SD) | 9.9 (3.4) | 9.5 (3.1) | 10.3 (3.5) | 11.5 (4.2) | 12.8 (4.7) | <.0001 |
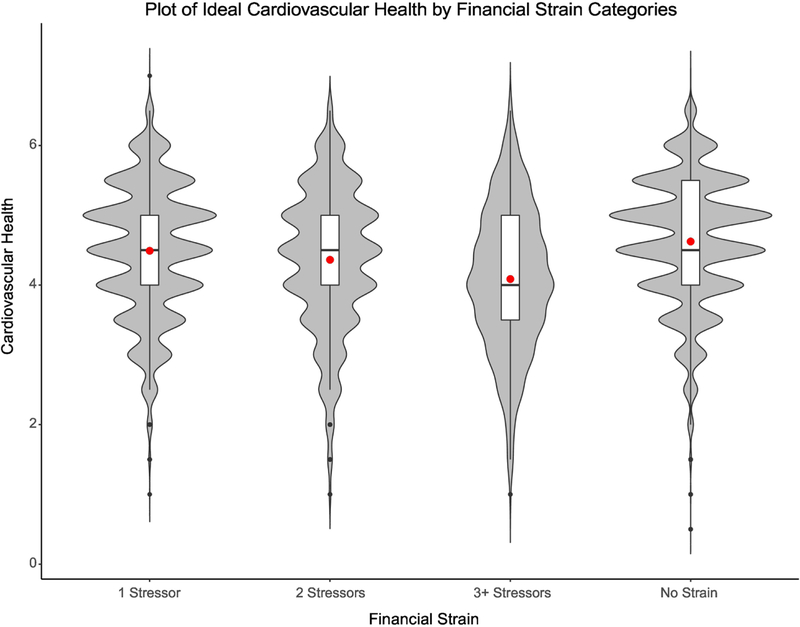
Table 2 describes the frequency of the individual measures of financial strain according to the total number of financial stressors reported. Of note, 61% of women who reported difficulty paying bills reported a total of 3 or more financial stressors. In contrast, only 20% of women with a household member of out of work for longer than 3 months reported 3 or more financial strain events. Table 2 additionally presents the difficulty (i.e., the likelihood of endorsing an item) and slope (i.e., discrimination, which can be interpreted like an item-total correlation) for each of the 6 individual items based on the IRT analyses. The range of the item difficulty ranged from 3.7 to 1.6, suggesting that endorsing a move to a worse neighborhood was a “difficult” item more likely endorsed by someone with greater financial strain. In contrast, the items reporting serious financial problems or poor perceived family financial situation were “easier” items, whereby these were more likely to be endorsed by individuals at all spectrums of financial strain. Figure 1 visually depicts the distribution of ideal cardiovascular health scores according to financial strain score. The center point in each of the boxplots depicts the mean score of each of the financial strain categories. Of note, there is a decline in mean ideal cardiovascular health score with increasing financial strain. Individuals who did not report any financial strain had a mean of 4.6 compared to 4.1 in individuals with financial strain scores of 3 or higher. Median scores were similar for all categories (4.5) except for 3 or more stressors (4.0).
Table 2.
Frequency of individual financial strain events reported in participants of the Women’s Health Study stratified by total number of financial stress events
| Cumulative Financial Strain | |||||||
|---|---|---|---|---|---|---|---|
| No Strain | 1 Stressor | 2 Stressors | 3+ Stressors | P | Diff | Slope | |
| Moved to worse neighborhood | <.0001 | ||||||
| No, % | 75.4 | 16.1 | 4.9 | 3.6 | 3.7 | 1.3 | |
| Yes, % | 0.0 | 33.3 | 25.1 | 41.6 | |||
| Out of work 3+ months | <.0001 | ||||||
| No, % | 79.7 | 13.7 | 4.0 | 2.6 | 3.0 | 1.0 | |
| Yes, % | 0.0 | 51.6 | 22.0 | 26.4 | |||
| Member of household out of work 3+ months | <.0001 | ||||||
| No, % | 83.6 | 10.8 | 3.2 | 2.4 | 2.6 | 0.9 | |
| Yes, % | 0.0 | 59.5 | 21.1 | 19.5 | |||
| Inability to pay bills | <.0001 | ||||||
| No, % | 77.9 | 16.4 | 4.3 | 1.4 | 1.8 | 3.8 | |
| Yes, % | 0.0 | 15.1 | 23.8 | 61.1 | |||
| Serious financial problems | <.0001 | ||||||
| No, % | 81.2 | 15.4 | 2.8 | 0.6 | 1.6 | 2.8 | |
| Yes, % | 0.0 | 26.4 | 30.7 | 42.9 | |||
| Perceived family financial situation | <.0001 | ||||||
| No, % | 80.6 | 15.3 | 3.3 | 0.9 | 1.6 | 3.4 | |
| Yes, % | 0.0 | 27.2 | 27.8 | 45.1 | |||
Note: Item difficulty and slope scores were derived from Item Response Analyses. All difficulty scores and slopes were statistically significant (P < .05). P-values between the cumulative financial strain categories and the individual items were derived from χ2 analysis
Figure 1.
Plot of ideal cardiovascular health by financial strain categories
In multinomial logistic regression analyses, financial strain was associated with a decreased likelihood of having ideal cardiovascular health status (Table 3). In the unadjusted analyses, women who reported one (odds ratio [OR] = 0.61, 95% CI = 0.51, 0.72), two (OR = 0.41, 95% CI = 0.31, 0.55), or three or more (OR = 0.17, 95% CI = 0.12, 0.24) financial stressors were less likely to be classified as having ideal cardiovascular health compared to women who did not report any financial stressors. Adjusting for potential confounding variables only modestly attenuated the relationship between financial stress and ideal cardiovascular health classification (1 stressor: OR = 0.68, 95% CI = 0.57, 0.81; 2 stressors: OR = 0.50, 95% CI = 0.38, 0.67; 3+ stressors: OR= 0.23, 95% CI = 0.16, 0.33). Similarly, increasing number of financial stressors was associated with decreased likelihood of being classified as intermediate cardiovascular health, even after adjusting for potential confounding variables (1 stressor: OR = 0.77, 95% CI = 0.68, 0.87; 2 stressors: OR = 0.62, 95% CI = 0.52, 0.75;3+ stressors: OR = 0.41, 95% CI = 0.35, 0.49).
Table 3.
Multinomial logistic regression analyses of the association of the number of financial stressors and categories of ideal cardiovascular health
| Unadjusted model | Age-adjusted model | Fully-adjusted model | |
|---|---|---|---|
| Odds ratio (95% CI) |
Odds ratio (95% CI) |
Odds ratio (95% CI) |
|
| Intermediate cardiovascular health | |||
| 1 events | 0.71 (0.62, 0.80) | 0.70 (0.62, 0.79) | 0.77 (0.68, 0.87) |
| 2 events | 0.54 (0.45, 0.65) | 0.54 (0.48, 0.64) | 0.62 (0.52, 0.75) |
| 3+ events | 0.34 (0.28, 0.40) | 0.33 (0.28, 0.39) | 0.41 (0.35, 0.49) |
| Ideal cardiovascular health | |||
| 1 events | 0.61 (0.51, 0.72) | 0.60 (0.50, 0.71) | 0.68 (0.57, 0.81) |
| 2 events | 0.41 (0.31, 0.55) | 0.40 (0.30, 0.54) | 0.50 (0.38, 0.67) |
| 3+ events | 0.17 (0.12, 0.24) | 0.16 (0.12, 0.23) | 0.23 (0.16, 0.33) |
Note: Reference: Participants classified as having poor cardiovascular health.
Statistically significant associations (P < .05) are bolded.
95% CI, 95% confidence intervals.
Fully adjusted model includes the following covariates: age, race/ethnicity, education, income
In linear regression analyses, increasing number of financial stressors was associated with a worse ideal cardiovascular health score (Table 4). Unadjusted analysis demonstrated a dose-response effect, such that women who reported one (B = −0.13, 95% confidence interval (CI) = −0.17, −0.10) two stressors (B = −0.26, 95% CI = −0.32, −0.21), or three or more stressors (B = −0.54, 95% CI −0.60, −0.48) had decreased ideal cardiovascular health, compared to women who reported no financial stressors. Adjusting for potential confounding variables, including age, education and income, only modestly attenuated the relationship between financial stress and ideal cardiovascular health (1 stressor: B = −0.10, 95% CI = −0.13, −0.07; 2 stressors: B = −0.20, 95% CI = −0.26, −0.15; 3+ stressors: B = −0.44, 95% CI = −0.50, −0.38). Financial strain as a continuous variable revealed similar results (see Table 4). There was no significant interaction between financial strain with either education or income.
Table 4.
Multiple Linear Analyses of the Association of the Number of Financial Stressors and Ideal Cardiovascular Health
| Unadjusted Model | Age-Adjusted Model | Fully-Adjusted Model | |
|---|---|---|---|
| B Coefficient (95% CI) |
B Coefficient (95% CI) |
B Coefficient (95% CI) |
|
| 1 events | −0.13 | −0.14 | −0.10 |
| (−0.17, −0.10) | (−0.17, −0.10) | (−0.13, −0.07) | |
| 2 events | −0.26 | −0.26 | −0.20 |
| (−0.32, −0.21) | (−0.32, −0.21) | (−0.26, −0.15) | |
| 3+ events | −0.54 | −0.54 | −0.44 |
| (−0.60, −0.48) | (−0.60, −0.48) | (−0.50, −0.38) | |
| Continuous Score | −0.14 | −0.15 | −0.12 |
| (−0.16, −0.13) | (−0.16, −0.13) | (−0.13, −0.10) |
Note: Statistically significant associations (p <.05) are bolded.
95% CI = 95% Confidence Intervals
Note: Continuous score was computed in a separate model.
Fully-adjusted model includes the following covariates: age, race/ethnicity, education, income
Table 5 shows the relationship between each individual measure of financial strain and ideal cardiovascular health. Of note, each of the 6 measures of financial strain was significantly associated with a lower ideal cardiovascular health score and these relationships persisted after adjusting for potential confounders. Inability to pay bills and perceived family financial situation displayed the largest (inverse) associations with ideal cardiovascular health (B = −0.35, 95% CI = −0.41, −0.30; B = −0.37, 95% CI = −0.41, −0.32, respectively, in fully-adjusted models). Unemployment for 3 months or greater was the item with the smallest magnitude of association between decreased ideal cardiovascular health (B = −0.11, 95% CI = −0.15, −0.06).
Table 5.
The Association of Individual Measures of Financial Strain and Ideal Cardiovascular Health Score in Participants in the Women’s Health Study
| Unadjusted Model | Age-Adjusted Model | Fully-Adjusted Model | |
|---|---|---|---|
| B coefficient (95% CI) |
B Coefficient (95% CI) |
B Coefficient (95% CI) |
|
| Moved to Worse Neighborhood | −0.20 | −0.21 | −0.16 |
| (−0.29, −0.11) | (−0.29, −0.12) | (−0.25, −0.08) | |
| Out of Work 3+ Months | −0.16 | −0.16 | −0.11 |
| (−0.20, −0.11) | (−0.21, −0.11) | (−0.15, −0.06) | |
| Member of Household out of Work 3+ Months | −0.13 | −0.13 | −0.12 |
| (−0.17, −0.09) | (−0.17, −0.09) | (−0.15, −0.08) | |
| Inability to Pay Bills | −0.44 | −0.45 | −0.35 |
| (−0.50, −0.39) | (−0.50, −0.39) | (−0.41, −0.30) | |
| Serious Financial Problems | −0.33 | −0.34 | −0.27 |
| (−0.38, −0.29) | (−0.38, −0.29) | (−0.31, −0.23) | |
| Perceived Family Financial Situation | −0.47 | −0.47 | −0.37 |
| (−0.51, −0.42) | (−0.52, −0.43) | (−0.41, −0.32) |
Statistically significant associations (p <.05) are bolded.
95% CI = 95% Confidence Intervals
Fully-adjusted model includes the following covariates: age, race/ethnicity, education, income
The association between the financial strain items and ideal cardiovascular health were individually assessed through separate regression models
Financial Strain Sensitivity Analysis.
A sensitivity analysis was performed where acute financial strain events over the last five years (i.e., being unemployed for three months or longer, having a member of the household be unemployed for longer than three months, moving to a worse residence or neighborhood, and reporting serious financial problems or difficulties) and chronic financial strain items (i.e., ability to pay bills and overall family financial situation) were disaggregated and summed to create an acute financial strain and a chronic financial strain measure. Both measures were simultaneously inserted into a multiple linear regression analysis. While both measures were statically significant, Standardized parameter estimates (β) found a greater association between the chronic financial strain measure and ideal cardiovascular health (β = −0.12, p < .0001) than acute financial strain and ideal cardiovascular health (β = −0.05, p < .0001). Age-adjusted models had identical parameter estimates, while estimates attenuated in fully-adjusted models (Acute financial strain β = −0.10, p < .0001; Chronic financial strain β = −0.04, p < .0001). Both measures of financial strain were significantly associated (r = 0.40, p < .0001).
Discussion
In this cohort of older women health professionals, financial strain was associated with lower ideal cardiovascular health. Increasing number of financial strain events was associated with worse ideal cardiovascular health score and decreased odds of ideal cardiovascular health (ICH score 6–7). There was no interaction between number of financial strain events with either education or income. Each individual measure of financial strain was significantly associated with worse ideal cardiovascular health; perceived family financial situation and inability to pay for bills had the strongest association with ideal cardiovascular health. These relationships persisted after adjusting for potential confounding variables, including education and income.
The findings of this study align with a small number of existing studies on financial strain and cardiovascular disease in women. In the INTERHEART study4, three measures of financial strain were assessed in relation to myocardial infarction; business failure or crop loss displayed the strongest association with myocardial infarction (OR=1.6, 95% CI = 1.4, 1.8), and general financial strain (OR=1.3, 95% CI = 1.19, 1.48) and job loss (OR=1.4, 95% CI = 1.2, 1.5) were also associated with myocardial infarction. Notably, median age in this study was 58 years old and only one quarter of the participants were women, most of whom were not living in the United States. The Framingham study (1965–67) examined the relationship between baseline financial worries (“About money matters, would you say your family has been worse off, the same as, or better off than most other families you know”) and incident coronary artery disease or coronary disease-related mortality after 20 years of follow-up.13 Among employed women, those who reported a financial situation as worse off than their peers had a 90% incident risk of incident coronary disease or coronary-related mortality compared to women who reported that their financial situation was the same. The results from the Framingham study are limited by a lack of socioeconomic diversity. For instance, assessment of financial strain in the 1960’s particularly focused on blue-collar jobs in manufacturing at a time when they were more prevalent in the U.S. and women had lower participation in the workforce.
Traditional measures of socioeconomic status, such as education and income, have been well-studied in association with cardiovascular disease.7 However, in our study the relationship between financial strain and ideal cardiovascular health was independent of education and income. Not only did the relationship between financial strain and ideal cardiovascular health persist after adjusting for income and education, but furthermore, there was no interaction between these measures of SES and financial strain. Income and education may not adequately reflect debt or disposable income of an individual and the resulting stress from not having the resources to meet her immediate needs, and thus do not comprehensively reflect the true financial situation of an individual. Additionally, income and education do not capture wealth, which arguably more consistently reflects financial stability.
There are several potential mechanisms by which financial strain might lead to worse ideal cardiovascular health. Chronic psychosocial stress, such as financial strain, results in physiological dysregulation of the stress response systems.2,3,39 Acute and chronic psychosocial stress has been associated with elevated levels of serum biomarkers of systemic inflammation including C-reactive protein, interleukin-6 and interleukin-1β.40–43 Financial strain in particular has a robust association with inflammatory biomarkers and allostatic load, an observation that persists across age groups, race/ethnicity, and nationality.44–52 Another potential mechanism by which financial strain might lead to worse ideal cardiovascular health is through maladaptive coping strategies that can lead to poorer cardiovascular health, including dietary changes, sedentarism and substance use.1 For example, unemployment has been associated with increased obesity in large study of working-age adults in the United Kingdom.53 However, the maladaptive coping strategies that result in poor cardiovascular health are likely to be a pathway that is independent of the increased inflammation associated with psychosocial stress response.39,54 While obesity can lead to increased systemic inflammation, the relationship between financial strain and inflammation might be independent of BMI.50
The study has some potential limitations. First, this is a cross-sectional study, and thus we are unable to make causal inference. Moreover, there is potential for reverse causality as poor health can lead to financial strain. However, in this cohort of female health professionals, we excluded women with major cancer or cardiovascular diagnoses. Second, similar analyses should be performed in men, other professional and non-professional women as well as in various racial/ethnic minority populations. In terms of generalizability, as our cohort consists of older female health professionals, the fact that 26% reported some amount of financial strain is still concerning. Arguably, because these findings emerged in our unique sample of older, predominately white female health professionals, we contend that the associations found would be heightened in the general population. Our results are of importance because the associations documented in the present study may be greater in magnitude among younger and racially- and ethnically-diverse populations. All measures of ideal cardiovascular health were assessed by self-report. However, reporting of medical conditions in WHS previously has been demonstrated to have over 95% accuracy.31–35 Diet was collected in 2004 and we cannot correct for this limitation due to the follow-up data collection in WHS. Fourth, because retirement status was unavailable, we were unable to account for retirement in our models.
The necessity of working past the age of retirement among women is occurring more frequently due to their increased life expectancy compared to men55, increased financial dependency of adult children, increased debt burden, and decreased retirement benefits overall.22,56 This economic reality for older women in the United States is likely to persist for the foreseeable future,57 and the consequences are likely to extend to their ability to access healthcare. Improving the quality of life for older women in the United States while controlling healthcare expenditures is of high public health priority. However, little attention is paid to economic policies and programs that affect the financial welfare of older women. Thus, this study may have implications for the potential cardiovascular health benefit of financial protections for older individuals.58
In conclusion, financial strain was associated with worse ideal cardiovascular health in the Women’s Health Study, even after adjusting for income and education. Clinical and population-wide interventions to reduce financial strain, particularly in older women, should be further investigated in relation to cardiovascular health.
Highlights.
Little is known on the impact of financial strain on CV health in older women.
An indicator of general CV health, was created based on AHA 2020 guidelines
Greater financial strain was associated with poorer ideal CV health
Acknowledgments
We are grateful to the WHS participants. The Women’s Health Study is supported by grants HL080467, HL099355, HL043851, CA047988, and UM1-CA182913 from the National Heart, Lung, and Blood Institute and the National Cancer Institute. This study is funded by NIH R01 grant AG038492 (Dr. MA Albert).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Psychological Association. Stress in America: Our Health at Risk. Washington, DC: American Psychological Association [Google Scholar]
- 2.Friedman EM, Williams DR, Singer BH, Ryff CD. Chronic discrimination predicts higher circulating levels of E-selectin in a national sample: The MIDUS study. Brain Behav Immun. 2009;23(5):684–692. doi: 10.1016/j.bbi.2009.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McEwen BS. Protective and Damaging Effects of Stress Mediators. Flier JS, Underhill LH, eds. N Engl J Med. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307 [DOI] [PubMed] [Google Scholar]
- 4.Rosengren A, Hawken S, Ôunpuu S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11 119 cases and 13 648 controls from 52 countries (the INTERHEART study): case-control study. The Lancet. 2004;364(9438):953–962. doi: 10.1016/S0140-6736(04)17019-0 [DOI] [PubMed] [Google Scholar]
- 5.Sumner JA, Kubzansky LD, Elkind MSV, et al. Trauma Exposure and Posttraumatic Stress Disorder Symptoms Predict Onset of Cardiovascular Events in Women CLINICAL PERSPECTIVE. Circulation. 2015;132(4):251–259. doi: 10.1161/CIRCULATIONAHA.114.014492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Slopen N, Glynn RJ, Buring JE, Lewis TT, Williams DR, Albert MA. Job strain, job insecurity, and incident cardiovascular disease in the Women’s Health Study: Results from a 10-year prospective study. Behrens T, ed. PLoS ONE. 2012;7(7):e40512. doi: 10.1371/journal.pone.0040512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Havranek EP, Mujahid MS, Barr DA, et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132(9):873–898. doi: 10.1161/CIR.0000000000000228 [DOI] [PubMed] [Google Scholar]
- 8.Richardson S, Shaffer JA, Falzon L, Krupka D, Davidson KW, Edmondson D. Meta-Analysis of Perceived Stress and Its Association With Incident Coronary Heart Disease. Am J Cardiol. 2012;110(12):1711–1716. doi: 10.1016/j.amjcard.2012.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khandelwal N, Hough CL, Downey L, et al. Prevalence, Risk Factors, and Outcomes of Financial Stress in Survivors of Critical Illness: Crit Care Med. 2018;46(6):e530–e539. doi: 10.1097/CCM.0000000000003076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlsson AC, Starrin B, Gigante B, Leander K, Hellenius M-L, de Faire U. Financial stress in late adulthood and diverse risks of incident cardiovascular disease and all-cause mortality in women and men. BMC Public Health. 2014;14(1). doi: 10.1186/1471-2458-14-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrie JE, Martikainen P, Shipley MJ, Marmot MG. Self-reported economic difficulties and coronary events in men: evidence from the Whitehall II study. Int J Epidemiol. 2005;34(3):640–648. doi: 10.1093/ije/dyi063 [DOI] [PubMed] [Google Scholar]
- 12.Georgiades A, Janszky I, Blom M, László KD, Ahnve S. Financial strain predicts recurrent events among women with coronary artery disease. Int J Cardiol. 2009;135(2):175–183. doi: 10.1016/j.ijcard.2008.03.093 [DOI] [PubMed] [Google Scholar]
- 13.Eaker ED, Pinsky J, Castelli WP. Myocardial Infarction and Coronary Death among Women: Psychosocial Predictors from a 20-Year Follow-up of Women in the Framingham Study. Am J Epidemiol. 1992;135(8):854–864. doi: 10.1093/oxfordjournals.aje.a116381 [DOI] [PubMed] [Google Scholar]
- 14.Backé E-M, Seidler A, Latza U, Rossnagel K, Schumann B. The role of psychosocial stress at work for the development of cardiovascular diseases: a systematic review. Int Arch Occup Environ Health. 2012;85(1):67–79. doi: 10.1007/s00420-011-0643-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuper H, Marmot M. Job strain, job demands, decision latitude, and risk of coronary heart disease within the Whitehall II study. J Epidemiol Community Health. 2003;57(2):147–153. doi: 10.1136/jech.57.2.147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Virtanen M, Nyberg ST, Batty GD, et al. Perceived job insecurity as a risk factor for incident coronary heart disease: systematic review and meta-analysis. BMJ. 2013;347. doi: 10.1136/bmj.f4746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferrie JE, Kivimäki M, Shipley MJ, Davey Smith G, Virtanen M. Job insecurity and incident coronary heart disease: The Whitehall II prospective cohort study. Atherosclerosis. 2013;227(1):178–181. doi: 10.1016/j.atherosclerosis.2012.12.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 19.Cabeza de Baca T, Durazo EM, Rodriguez F. Achieving Optimal Cardiovascular Health: a Social Epidemiological Approach. Curr Epidemiol Rep. June 2018. doi: 10.1007/s40471-018-0154-z [DOI] [Google Scholar]
- 20.Caleyachetty R, Echouffo-Tcheugui JB, Muennig P, Zhu W, Muntner P, Shimbo D. Association between cumulative social risk and ideal cardiovascular health in US adults: NHANES 1999–2006. Int J Cardiol. 2015;191:296–300. doi: 10.1016/j.ijcard.2015.05.007 [DOI] [PubMed] [Google Scholar]
- 21.Mathews L, Ogunmoroti O, Nasir K, et al. Psychological Factors and Their Association with Ideal Cardiovascular Health Among Women and Men. J Womens Health. January 2018. doi: 10.1089/jwh.2017.6563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Campbell A, Lopez-Fernandini A, Gorin D, Lipman B, Tabir B. Insights into the Financial Experiences of Older Adults: A Forum Briefing Paper. Board of Governors of the Federal Reserve System; 2013. [Google Scholar]
- 23.Hess C, Mili J, Hayes J, Hegewisch A. The status of women in the states 2015. 2015. www.iwpr.org.
- 24.Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics—2018 Update: A Report From the American Heart Association. Circulation. 2018;137(12):e67–e492. doi: 10.1161/CIR.0000000000000558 [DOI] [PubMed] [Google Scholar]
- 25.Rexrode KM, Lee I-M, Cook NR, Hennekens CH, Buring JE. Baseline Characteristics of Participants in the Women’s Health Study. J Womens Health Gend Based Med. 2000;9(1):19–27. doi: 10.1089/152460900318911 [DOI] [PubMed] [Google Scholar]
- 26.Albert MA, Durazo EM, Slopen N, et al. Cumulative psychological stress and cardiovascular disease risk in middle aged and older women: Rationale, design, and baseline characteristics. Am Heart J. 2017;192:1–12. doi: 10.1016/j.ahj.2017.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hays RD, Morales LS, Reise SP. Item Response Theory and Health Outcomes Measurement in the 21st Century. Med Care. 2000;38:II-28–II-42. doi: 10.1097/00005650-200009002-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Willett WC, Sampson L, Stampfer MJ, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122(1):51–65. doi: 10.1093/oxfordjournals.aje.a114086 [DOI] [PubMed] [Google Scholar]
- 29.Lee I-M, Paffenbarger RS Jr. Design of present-day epidemiologic studies of physical activity and health In: Epidemiologic Methods in Physical Activity Studies. New York, NY: Oxford University Press; 2009:100–123. [Google Scholar]
- 30.Wolf AM, Hunter DJ, Colditz GA, et al. Reproducibility and Validity of a Self-Administered Physical Activity Questionnaire. Int J Epidemiol. 1994;23(5):991–999. doi: 10.1093/ije/23.5.991 [DOI] [PubMed] [Google Scholar]
- 31.Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM. C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA. 2001;286(3):327–334. doi: 10.1001/jama.286.3.327 [DOI] [PubMed] [Google Scholar]
- 32.Song Y, Manson JE, Buring JE, Liu S. A Prospective Study of Red Meat Consumption and Type 2 Diabetes in Middle-Aged and Elderly Women: The Women’s Health Study. Diabetes Care. 2004;27(9):2108–2115. doi: 10.2337/diacare.27.9.2108 [DOI] [PubMed] [Google Scholar]
- 33.Ding EL, Song Y, Manson JE, Pradhan AD, Buring JE, Liu S. Accuracy of Administrative Coding for Type 2 Diabetes in Children, Adolescents, and Young Adults: Response to Rhodes et al. Diabetes Care. 2007;30(9):e98–e98. doi: 10.2337/dc07-0903 [DOI] [PubMed] [Google Scholar]
- 34.Liu S, Lee I-M, Song Y, et al. Vitamin E and Risk of Type 2 Diabetes in the Women’s Health Study Randomized Controlled Trial. Diabetes. 2006;55(10):2856–2862. doi: 10.2337/db06-0456 [DOI] [PubMed] [Google Scholar]
- 35.Sesso HD, Cook NR, Buring JE, Manson JE, Gaziano JM. Alcohol Consumption and the Risk of Hypertension in Women and Men. Hypertension. 2008;51(4):1080–1087. doi: 10.1161/HYPERTENSIONAHA.107.104968 [DOI] [PubMed] [Google Scholar]
- 36.Wang L, Manson JE, Buring JE, Sesso HD. Meat intake and the risk of hypertension in middle-aged and older women: J Hypertens. 2008;26(2):215–222. doi: 10.1097/HJH.0b013e3282f283dc [DOI] [PubMed] [Google Scholar]
- 37.Willett W, Stampfer MJ, Bain C, et al. Cigarette smoking, relative weight, and menopause. Am J Epidemiol. 1983;117(6):651–658. doi: 10.1093/oxfordjournals.aje.a113598 [DOI] [PubMed] [Google Scholar]
- 38.Field AP, Miles J, Field Z. Discovering Statistics Using R. London ; Thousand Oaks, Calif: Sage; 2012. [Google Scholar]
- 39.Nusslock R, Miller GE. Early-Life Adversity and Physical and Emotional Health Across the Lifespan: A Neuroimmune Network Hypothesis. Biol Psychiatry. 2016;80(1):23–32. doi: 10.1016/j.biopsych.2015.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barbosa-Leiker C, Roper V, McPherson S, et al. Cross-sectional and Longitudinal Relationships between Perceived Stress and C-reactive Protein in Men and Women: Perceived Stress and C-reactive Protein. Stress Health. 2014;30(2):158–165. doi: 10.1002/smi.2507 [DOI] [PubMed] [Google Scholar]
- 41.McDade TW, Hawkley LC, Cacioppo JT. Psychosocial and Behavioral Predictors of Inflammation in Middle-Aged and Older Adults: The Chicago Health, Aging, and Social Relations Study. Psychosom Med. 2006;68(3). https://journals.lww.com/psychosomaticmedicine/Fulltext/2006/05000/Psychosocial_and_Behavioral_Predictors_of.4.aspx. [DOI] [PubMed] [Google Scholar]
- 42.Paul K, Boutain D, Agnew K, Thomas J, Hitti J. The Relationship between Racial Identity, Income, Stress and C-Reactive Protein among Parous Women: Implications for Preterm Birth Disparity Research. J Natl Med Assoc. 2008;100(5):540–546. doi: 10.1016/S0027-9684(15)31300-6 [DOI] [PubMed] [Google Scholar]
- 43.Steptoe A, Hamer M, Chida Y. The effects of acute psychological stress on circulating inflammatory factors in humans: A review and meta-analysis. Brain Behav Immun. 2007;21(7):901–912. doi: 10.1016/j.bbi.2007.03.011 [DOI] [PubMed] [Google Scholar]
- 44.Hughes A, Kumari M, McMunn A, Bartley M. Unemployment and inflammatory markers in England, Wales and Scotland, 1998–2012: Meta-analysis of results from 12 studies. Brain Behav Immun. 2017;64:91–102. doi: 10.1016/j.bbi.2017.03.012 [DOI] [PubMed] [Google Scholar]
- 45.Chen E, Miller GE, Yu T, Brody GH. The Great Recession and health risks in African American youth. Brain Behav Immun. 2016;53:234–241. doi: 10.1016/j.bbi.2015.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cutrona CE, Abraham WT, Russell DW, et al. Financial strain, inflammatory factors, and haemoglobin A1c levels in African American women. Br J Health Psychol. 2015;20(3):662–679. doi: 10.1111/bjhp.12120 [DOI] [PubMed] [Google Scholar]
- 47.Gallo LC, Jiménez JA, Shivpuri S, Espinosa de los Monteros K, Mills PJ. Domains of Chronic Stress, Lifestyle Factors, and Allostatic Load in Middle-Aged Mexican-American Women. Ann Behav Med. 2011;41(1):21–31. doi: 10.1007/s12160-010-9233-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gémes K, Ahnve S, Janszky I. Inflammation a possible link between economical stress and coronary heart disease. Eur J Epidemiol. 2008;23(2):95–103. doi: 10.1007/s10654-007-9201-7 [DOI] [PubMed] [Google Scholar]
- 49.Lipowicz A, Szklarska A, Mitas AW. Biological costs of economic transition: Stress levels during the transition from communism to capitalism in Poland. Econ Hum Biol. 2016;21:90–99. doi: 10.1016/j.ehb.2015.12.005 [DOI] [PubMed] [Google Scholar]
- 50.Steffen PR, Walker J, Meredith R, Anderson C. The Effects of Job Instability and Financial Strain on C-Reactive Protein in a Sample of Mexican Immigrants. Ethn Dis. 2016;26(1):37. doi: 10.18865/ed.26.1.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sturgeon JA, Arewasikporn A, Okun MA, Davis MC, Ong AD, Zautra AJ. The Psychosocial Context of Financial Stress: Implications for Inflammation and Psychological Health. Psychosom Med. 2016;78(2):134–143. doi: 10.1097/PSY.0000000000000276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hintikka J, Lehto SM, Niskanen L, et al. Unemployment and ill health: a connection through inflammation? BMC Public Health. 2009;9(1):410. doi: 10.1186/1471-2458-9-410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hughes A, Kumari M. Unemployment, underweight, and obesity: Findings from Understanding Society (UKHLS). Prev Med. 2017;97:19–25. doi: 10.1016/j.ypmed.2016.12.045 [DOI] [PubMed] [Google Scholar]
- 54.Penninx BWJH. Depression and cardiovascular disease: Epidemiological evidence on their linking mechanisms. Neurosci Biobehav Rev. 2017;74:277–286. doi: 10.1016/j.neubiorev.2016.07.003 [DOI] [PubMed] [Google Scholar]
- 55.Munnell A The average retirement age: an update. 2015. http://crr.bc.edu/wp-content/uploads/2015/03/IB_15-4_508_rev.pdf.
- 56.Morgan PS, Cumberworth E, Wimer C. The Great Recession and the American Family. Stanford, CA: Stanford Center on Poverty and Inequality; 2012. [Google Scholar]
- 57.Elson D Gender relations and economic issues. Gend Dev. 1993;1(3):6–12. doi: 10.1080/09682869308519974 [DOI] [PubMed] [Google Scholar]
- 58.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: The emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45(5):637–651. doi: 10.1016/j.jacc.2004.12.005 [DOI] [PubMed] [Google Scholar]