Abstract
Background:
The prevalence of electronic cigarette use grows amidst a dearth of published evidence of the potential health implications.
Objective:
The purpose of the study was to assess predictors of e-cigarette use among female current and former tobacco users of childbearing age—specifically to determine whether demographic factors, pregnancy status, conventional cigarette smoking, and perceived e-cigarette harm are associated with e-cigarette use. Reasons for using e-cigarettes were also measured.
Methods:
A cross-sectional, correlational design was used; 194 current and former female tobacco users, 18–45 years of age from two university-affiliated prenatal clinics and one women’s health clinic in Kentucky took part. Slightly more than half were pregnant. Age, race/ethnicity, education, pregnancy status, use history for cigarettes and e-cigarettes, and perception of health hazard from e-cigarettes were measured and associations with e-cigarette use were made with Mann-Whitney U tests or Spearman’s rank correlations. Predictors of e-cigarette use were determined using proportional odds modeling.
Results:
Most current e-cigarette users were also current cigarette smokers (88%). Nearly half of current and former e-cigarette users were pregnant. Most women perceived e-cigarettes as a minor (38%) or moderate (31%) health hazard. In the regression, younger women were at greater risk for e-cigarette use, while minority women and those who were pregnant were less likely to be e-cigarette users.
Discussion:
Pregnant women were less likely to be more recent e-cigarette users, compared with nonpregnant women. However, nearly all current e-cigarette users were dual tobacco users, including pregnant women. It is both imperative and timely to determine the impact of e-cigarette use on maternal and infant health, thus improving healthcare provider confidence to discuss the health implications of e-cigarette use with their patients.
Keywords: e-cigarettes, health risk appraisal, pregnancy, tobacco use, women
In the United States, overall use and awareness of electronic cigarettes has escalated dramatically—especially among vulnerable populations, including youth and women (Choi & Forster, 2013; King, Alam, Promoff, Arrazola, & Dube, 2013; Pearson, Richardson, Niaura, Vallone, & Abrams, 2012). Electronic nicotine delivery systems, also known as electronic cigarettes, emerged in the U.S. tobacco market in 2007 (Regan, Promoff, Dube, & Arrazola, 2013). Electronic cigarettes are plastic devices used to mimic the action of smoking a regular cigarette by having the user puff into the device, thus ingesting a nicotine-containing aerosol (Goniewicz, Kuma, Gawron, Knysak, & Kosmider, 2012). Prevalence of e-cigarette use is higher among young adults (14% of 18–24-year-olds) compared to older adults (9% of 25–44 year olds) (McMillen, Gottlieb, Shaefer, Winickoff, & Klein, 2014). Increases in e-cigarette use among all adults have been attributed to them being perceived as more convenient, advertised as less expensive, and marketed as potential smoking-cessation aids (King et al., 2013; Pearson et al., 2012). Due to the novelty of e-cigarettes and current lack of federal regulations, there has been a substantial increase in the manufacturing and marketing of these products. There are hundreds of brands of e-cigarettes, all of which contain unregulated levels of nicotine, toxic chemicals, and ultrafine particles (Grana, Benowitz, & Glantz, 2014; Schober et al., 2014). This surge in e-cigarette use poses a health risk to women of childbearing age—specifically pregnant women—due to the adverse and teratogenic effects of nicotine on reproductive and fetal health (England, Bunnell, Pechacek, Tong, & McAfee, 2015; Wickström, 2007).
The perception that e-cigarettes are safer than conventional cigarettes may prompt women to switch or to engage in dual use of e-cigarettes and conventional cigarettes during and after pregnancy (Baeza-Loya et al., 2014; Kahr et al., 2015; Mark, Farquhar, Chisolm, Coleman-Cowger, & Terplan, 2015). Perceptions of relative safety of e-cigarettes compared with conventional cigarettes may even promote increased use during pregnancy (Baeza-Loya et al., 2014). Increases in e-cigarette use among women have been linked to the perception that e-cigarettes may be a means to smoking cessation (Farquhar, Mark, Terplan, & Chisolm, 2015). More women try to quit smoking during pregnancy than any other time in their lives; yet, two thirds of women who quit will relapse. Although pregnant smokers using conventional cigarettes are aware of the need to quit, some believe in harm reduction as a method of quitting (Farquhar et al., 2015; Graham, Flemming, Fox, Heirs, & Sowden, 2014). E-cigarettes have been the center of recent controversy regarding novel smoking cessation or harm reduction products which putatively can reduce disease burden and possibly mortality (Etter & Bullen, 2011). There is concern that marketing strategies promoting harm reduction may increase the appeal and obfuscate the known adverse effects of nicotine on fetal development.
Demographic characteristics, including race/ethnicity and age, are associated with e-cigarette use among current and former tobacco users: e-cigarette users are more likely to be non-Hispanic White and younger (ages 18–24) (Zhu et al., 2013). There is a clear need to identify risk factors for e-cigarette use—particularly in vulnerable populations—including young women of childbearing age. The purpose of this study was to assess predictors of e-cigarette use among female current and former tobacco users of childbearing age—specifically to determine whether demographic factors, pregnancy status, conventional cigarette smoking, and perceived e-cigarette harm are associated with e-cigarette use. Reasons for using e-cigarettes were also measured among current and former users.
Methods
Design and Setting
A cross-sectional survey was administered to female current or former tobacco users of childbearing age—half of whom were pregnant. Pregnant women were recruited from two university-affiliated prenatal clinics and nonpregnant women were recruited from one women’s health clinic; clinics were located in Central and Eastern Kentucky.
Procedures
After approval from the medical Institutional Review Board, flyers describing the study were placed in the clinics. Women who indicated interest were screened by nurses at their healthcare appointments. Those who were eligible signed informed consent prior to survey completion. Recruitment was based on our previous experience with these populations (Ashford & Westneat, 2012; Ashford et al., 2010). Nearly three fourths of participants completed the survey via an iPad; the rest completed a paper form with responses entered into the database. Data were stored on a secure server, protected by a password. Participants received a $10 gift card.
Population/Sample
English-speaking women of childbearing age who reported using tobacco within the past 12 months were eligible for the study. Quota sampling was used to ensure approximately equal numbers of pregnant (n = 101) and nonpregnant (n = 99) women. This sampling was done using a recruitment schedule for each group; once 101 pregnant women were enrolled, only nonpregnant women were eligible. Recruitment continued until the sample totaled 200 women.
Measures
Demographic characteristics.
Demographics included age (in years), race/ethnicity, education, and pregnancy status. To assess race/ethnicity, women indicated their race (with six options, including multiracial) and whether their ethnicity was Hispanic/Latina (yes/no). Given the small numbers in each racial/ethnic minority, these variables were combined and categorized as “White/non-Hispanic” or “Other.” Women were asked the highest level of school completed (with seven options); a binary variable was created to indicate whether the woman was at least a college graduate. Women were asked to indicate whether they were currently pregnant (yes/no).
Reasons for using e-cigarettes.
Any participant who had ever used e-cigarettes was given a checklist of nine potential reasons for using e-cigarettes, including: “Thought it would be less expensive;” “Wanted to quit smoking;” “I became pregnant;” “Wanted to maintain weight/lose weight;” “Less harmful to others;” “Less harmful to myself;” “Like the taste of the e-cigarette;” “Can use it where smoking is not allowed;” and “Saw advertisements promoting e-cigarettes.” The participant was instructed to check all reasons that applied to her decision to use them.
Conventional cigarette use.
To assess use frequency for conventional cigarettes, participants were asked to indicate how many days within the past 30 they had smoked (“used daily,” “used often [more than 10 days this month],” “used occasionally [less than 10 days this month],” “have used, but not within the last 30 days” or “never used”). Current smokers were those who had used in the past 30 days; former users had smoked in the past, but not in the last 30 days, while “never smokers” had never used cigarettes. “Never smokers” were former or current users of some other form of tobacco (e.g., smokeless) in order to be eligible for the study.
Perceived harm from e-cigarettes.
Participants were asked to indicate the extent to which they believed, in general, that e-cigarettes are a health hazard, with four possible responses: “not a health hazard at all;” “minor health hazard;” “moderate health hazard;” and “serious health hazard.”
e-Cigarette use.
Consistent with the question that assessed frequency of conventional cigarette use, participants were asked how often they had used e-cigarettes. Their responses were used to classify them as a “current,” “former,” or “never” user of e-cigarettes with the same cutoffs as for conventional cigarettes.
Data Analysis
Bivariate group comparisons were accomplished using Spearman’s rank correlation or Mann-Whitney U test. Predictors of e-cigarette use status (current, former, never) were determined using proportional odds modeling (POM); the POM assumption was assessed using the score test. The presence of multicollinearity was evaluated using variance inflation factors. Data analysis was conducted using SAS, v. 9.4; an alpha level of .05 was used.
Results
Participant Description
In total, 379 women were screened; 164 were ineligible because they did not meet inclusion criteria. Of the 215 eligible participants, 200 enrolled and completed the survey (93% participation). Six women were omitted from this analysis since their e-cigarette status could not be determined. The average age of participants was 29.6 years; most were White/non-Hispanic and had less than a college education (Table 1). The majority were current cigarette smokers and current/former users of e-cigarettes. Most current e-cigarette users were dual users, also currently smoking cigarettes. Most women indicated that e-cigarettes were a minor or moderate health hazard. In the bivariate analysis, e-cigarette use status was only associated with race/ethnicity (White/non-Hispanic more likely to use) and education (less educated more likely to use; Table 1). The comparison of pregnant and nonpregnant participants on frequency of use was significant for both conventional cigarettes (Mann-Whitney U χ2 = 17.0; p < .001) and e-cigarettes (Mann-Whitney U χ2 = 4.7; p =03); pregnant women tended to use both products less frequently (Figure 1).
TABLE 1.
Participant Characteristics by e-Cigarette Use Status
| All (N = 194) |
Current (n = 49) |
Former (n = 77) |
Never (n = 68) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | M | (SD) | M | (SD) | M | (SD) | M | (SD) | p |
| Age | 29.6 | (6.71) | 28.4 | (6.15) | 29.5 | (6.38) | 30.5 | (7.39) | .14a |
| n | (%) | n | (%) | n | (%) | n | (%) | ||
| Race/ethnicity | |||||||||
| White/non-Hispanic | 143 | (78.1) | 40 | (87.0) | 65 | (84.4) | 38 | (63.3) | .003b |
| Other | 40 | (21.9) | 6 | (13.0) | 12 | (15.6) | 22 | (36.7) | |
| Education | |||||||||
| College graduate | 31 | (16.0) | 3 | (6.1) | 19 | (24.7) | 9 | (13.2) | .02b |
| <College graduate | 163 | (84.0) | 46 | (93.9) | 58 | (75.3) | 59 | (86.8) | |
| Pregnant | |||||||||
| Yes | 100 | (51.6) | 23 | (46.9) | 38 | (49.3) | 39 | (57.3) | .48b |
| No | 94 | (48.4) | 26 | (53.1) | 39 | (50.7) | 29 | (42.7) | |
| Conventional cigarettes | |||||||||
| Current | 163 | (84.0) | 43 | (87.8) | 64 | (83.1) | 56 | (82.4) | .45a |
| Former | 24 | (12.4) | 6 | (12.2) | 8 | (10.4) | 10 | (14.7) | |
| Never | 7 | (3.6) | 0 | (0.0) | 5 | (6.5) | 2 | (2.9) | |
| e-Cigarettes a hazard | |||||||||
| Serious | 21 | (10.9) | 4 | (8.3) | 5 | (6.5) | 12 | (17.7) | .45a |
| Moderate | 59 | (30.6) | 12 | (25.0) | 32 | (41.5) | 15 | (22.1) | |
| Minor | 74 | (38.3) | 19 | (39.6) | 30 | (39.0) | 25 | (36.7) | |
| Not at all | 39 | (20.2) | 13 | (27.1) | 10 | (13.0) | 16 | (23.5) | |
Note. SD = standard deviation. Column percentages are shown.
Spearman’s rank correlation.
Mann-Whitney U test.
FIGURE 1.
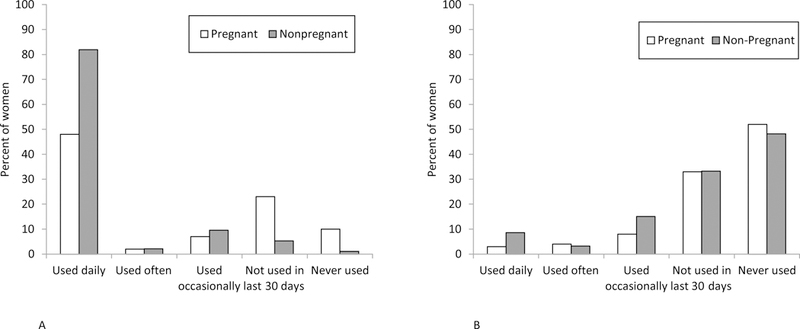
Frequency of cigarette use and e-cigarette use in pregnant and nonpregnant participants.
Reasons for Deciding to Use e-cigarettes
Figure 2 displays the percent of current and former e-cigarette users who selected each of the nine reasons for deciding to use from the checklist; totals within each group add to more than 100 since respondents indicated all that applied. More than half in each group indicated they decided to use them because they wanted to quit smoking. The next most frequent reasons among all ever users were that they thought it would be less expensive, could use e-cigarettes where smoking is prohibited, and thought they would be less harmful (to others and self).
FIGURE 2.
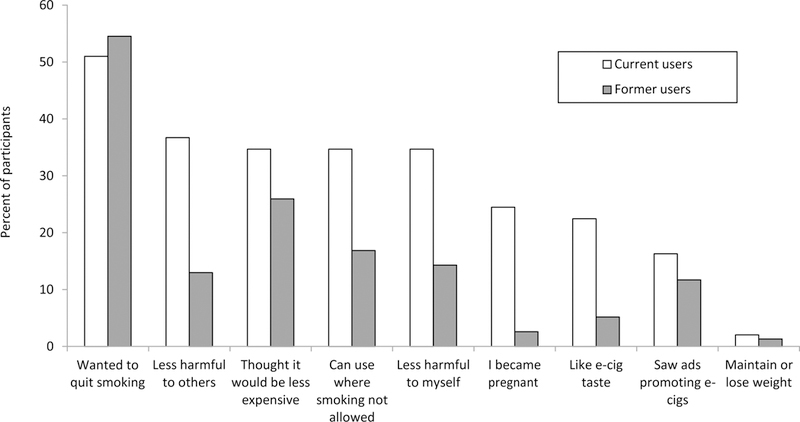
Reasons for using e-cigarettes among current (n = 49) and former (n = 77) e-cigarette users.
Predictors of e-Cigarette Use
The score test for the POM was not significant (χ2 = 14.2, p = .11), suggesting the proportional odds assumption was not violated. Variance inflation factors were all less than 1.5, suggestion no distortion in parameter estimates due to multicollinearity. In the POM, significant predictors of e-cigarette use status were age, race/ethnicity, and pregnancy status (Table 2). For every year of increase in age, the odds of being a more frequent e-cigarette user (i.e., current vs. former, former vs. never) decreased by 8%. Consistent with this relationship, for every five-year increase in age, the likelihood of being a more frequent e-cigarette user decreased by 34% (p = .001). Compared with minority participants, those who identified as White/non-Hispanic were 227% more likely to use e-cigarettes more frequently (p = .001). Pregnant women were 51% less likely to be more frequent e-cigarette users, compared with nonpregnant participants (p = .03). e-Cigarette use status was not related to education, current conventional cigarette use, or perceived harm in the multivariate model. Complete detail about the statistical model is available as Supplemental Digital Content.
TABLE 2.
Multiple Ordinal Logistic Regression: e-Cigarette Use*
| Predictor | OR | 95% CI | p |
|---|---|---|---|
| Age | 0.92 | [0.87, 0.97] | .001 |
| Race/ethnicity | |||
| White | 3.27 | [1.59, 6.70] | .001 |
| Other | 1.00 | ||
| Education | |||
| College graduate | 0.90 | [0.41, 1.98] | .79 |
| <College graduate | 1.00 | ||
| Pregnant | |||
| Yes | 0.49 | [0.25, 0.95] | .03 |
| No | 1.00 | ||
| Conventional cigarettes | |||
| Current | 1.77 | [0.39, 8.00] | .46 |
| Former | 1.28 | [0.24, 6.70] | .77 |
| Never | 1.00 | ||
| e-Cigarettes a hazard | |||
| Serious | 0.49 | [0.16, 1.49] | .21 |
| Moderate | 1.24 | [0.55, 2.82] | .61 |
| Minor | 0.90 | [0.41, 1.96] | .78 |
| Not at all | 1.00 | ||
Note. Only women with complete data on all variables in the model are included (n = 182). CI = confidence interval. OR = odds ratio.
The ordinal logistic regression estimated likelhood of being a more frequent e-cig use (i.e., current vs. former; former vs. never).
Discussion
Findings from this study reveal that over half of current and former tobacco users reported ever using e-cigarettes, and one fourth currently used e-cigarettes. It is concerning that nearly all of the current e-cigarette users were also cigarette smokers, making them dual users. Dual use of cigarettes with e-cigarettes is likely (King et al., 2013; Pearson et al., 2012), and the resulting consequences—particularly among women of childbearing age—cannot be ignored (England et al., 2015). Current e-cigarette use is significantly associated with greater nicotine dependence and concurrent dual use (Dutra & Glantz, 2014). It is unknown whether the dual users in this study initiated conventional cigarette smoking or e-cigarette use first. Assessment of dual use patterns warrants longitudinal research, particularly in this at risk population.
While perception of health hazard was not a significant predictor of e-cigarette use status in this study, more than two thirds of the participants perceived that e-cigarettes posed a minor or moderate health hazard, and an additional 20% of women did not believe e-cigarettes were a health hazard at all. Prior studies have found that e-cigarettes are generally perceived as less harmful and less addictive than conventional cigarettes (Baeza-Loya et al., 2014; Choi & Forster, 2013; Pearson et al., 2012). It is not clear whether this is due to marketing of the product as safer, or limited knowledge about the dangers of smoking cigarettes or e-cigarettes. This study confirms the misperception among smoking women of childbearing age that e-cigarettes are a “safe” alternative compared to conventional cigarettes (Choi & Forster, 2013).
White/non-Hispanic tobacco-using women of childbearing age were more likely than minorities to use e-cigarettes. Racial/ethnic minority groups tend to have less awareness of e-cigarettes (King et al., 2013) and lower e-cigarette use rates compared to nonminorities (Pearson et al., 2012). Racial/ethnic minorities also perceive e-cigarettes as more harmful than cigarettes and are less likely to believe they help with quitting (Choi & Forster, 2013). e-Cigarette marketing may be less targeted toward racial/ethnic minorities (Henningfield & Zaatari, 2010).
The associations of age and education with e-cigarette use in this study (either in the bivariate or multivariable analysis) are consistent with how these are related to cigarette smoking. As is the case with conventional cigarettes, younger tobacco-using women were more likely to be current or former e-cigarette users, controlling for other demographic factors. Previous research has demonstrated that young adults are more likely to have heard of e-cigarettes (King et al., 2013; Regan et al., 2013) and have used them (Pearson et al., 2012). Women in this study who reported current use of e-cigarettes tended to have less education compared to former/never users; however, educational attainment was not a significant predictor of e-cigarette use status in the multivariable model. The findings of the bivariate and regression analyses related to e-cigarette use are consistent with reports that current tobacco users are generally more likely to be younger and have less education than nonusers (Tong et al., 2013).
In the bivariate comparison with nonpregnant participants, pregnant women tended to use both e-cigarettes and cigarettes less frequently. Pregnant women had a lower likelihood of more frequent e-cigarette use—controlling for other demographic characteristics and perceived harm of e-cigarettes—in the multivariable model. This may be in part due to the observation that pregnant women smoke about 70% less than nonpregnant women (Williamson, Serdula, Kendrick, & Binkin, 1989). Further, lower e-cigarette use during pregnancy may be linked to consistent messaging that any tobacco use is unsafe while pregnant. There is also evidence that nicotine has detrimental effects on the fetus (Baeza-Loya et al., 2014), yet, future research is needed to evaluate reproductive and perinatal health risks associated with e-cigarette use.
Although results of this study indicate pregnant women were less likely to use e-cigarettes, it is concerning that among current e-cigarette users, nearly half were pregnant. Unfortunately, few healthcare providers consistently screen pregnant women for use of noncombustible tobacco products such as e-cigarettes (England et al., 2014; England et al., 2015). However, in a recent survey of 252 OBGYN providers, the vast majority wanted to know more about the health effects of novel tobacco products on maternal and neonatal outcomes. There is a critical need to train women’s and primary healthcare providers to improve their ability to screen for and discuss the health implications of e-cigarette use with their patients (England et al., 2014). This has implications for nurses in clinic settings in particular.
In a related qualitative study, we conducted focus groups of 12 participants to gain a deeper understanding of factors contributing to e-cigarette usage among pregnant and postpartum women. Pregnant women are initially attracted to e-cigarettes as a harm reduction strategy, yet, often to return to conventional cigarettes in the postpartum period. Most women using e-cigarettes were simultaneously using conventional cigarettes. Further, there was uncertainty regarding the health effects of e-cigarettes due to mixed messages about safety from healthcare providers and family members. Women valued choice in determining the dosage of nicotine and flavors, but they disliked having to purchase the “equipment” associated with e-cigarettes (Fallin, Miller, Assef, & Ashford, 2016).
One limitation is that tobacco use other than cigarettes and e-cigarettes was not assessed. In addition, tobacco use was not verified using biochemical validation, since there is not a test that can distinguish between cigarette smoking and e-cigarette use. Related to this, we did not measure daily e-cigarette consumption, so we were not able test for an association between daily use frequency and either pregnancy status or perception of risk. Future studies will benefit from a specific measure of daily consumption, such as average cartridges per day. The purposive sampling design, while providing detailed information about female current and former tobacco users of childbearing age, is not generalizable to the wider population. Longitudinal research is needed to assess trends in e-cigarette use and perceived harm among other population subgroups.
Conclusion
e-Cigarette use is growing despite concerns about safety and dual use. Prior to this study, there was limited information about risk factors for e-cigarette use among female current and former tobacco users of childbearing age, including pregnant women. The next step would be to develop and test interventions specific to this highly vulnerable population and their healthcare providers. Nurses are a key component of this goal, given regular interactions with at-risk women in clinic settings.
Supplementary Material
Acknowledgments
The authors acknowledge this work was supported in part by a Research Support Grant from the University of Kentucky Office of the Vice President for Research, as well as support by the University of Kentucky Clinical and Translational Research Center KL2RR033171 CTSA grant number NIH CTSA UL1TR000117, through use of the REDCap research project database.
Footnotes
The authors have no conflicts of interest to report.
Contributor Information
Kristin Ashford, College of Nursing, University of Kentucky, Lexington, KY..
Amanda Wiggins, College of Nursing, University of Kentucky, Lexington, KY..
Karen Butler, College of Nursing, University of Kentucky, Lexington, KY..
Melinda Ickes, Department of Kinesiology and Health Promotion, University of Kentucky, Lexington, KY..
Mary Kay Rayens, College of Nursing, University of Kentucky, Lexington, KY..
Ellen Hahn, Marcia A. Dake Professorship, BREATHE College of Nursing, University of Kentucky, Lexington,KY..
References
- Ashford K, & Westneat S (2012). Prenatal hair nicotine analysis in homes with multiple smokers. Nursing Clinics of North America, 47, 13–20. doi: 10.1016/j.cnur.2011.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashford KB, Hahn E, Hall L, Rayens MK, Noland M, & Ferguson JE (2010). The effects of prenatal secondhand smoke exposure on preterm birth and neonatal outcomes. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 39, 525–535. doi: 10.1111/j.1552-6909.2010.01169.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baeza-Loya S, Viswanath H, Carter A, Molfese DL, Velasquez KM, Baldwin PR, … Salas R (2014). Perceptions about e-cigarette safety may lead to e-smoking during pregnancy. Bulletin of the Menninger Clinic, 78, 243–252. doi: 10.1521/bumc.2014.78.3.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi K, & Forster J (2013). Characteristics associated with awareness, perceptions, and use of electronic nicotine delivery systems among young US Midwestern adults. American Journal of Public Health, 103, 556–561. doi: 10.2105/AJPH.2012.300947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutra LM, & Glantz SA (2014). Electronic cigarettes and conventional cigarette use among US adolescents: A cross-sectional study. JAMA Pediatrics, 168, 610–617. doi: 10.1001/jamapediatrics.2013.5488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- England LJ, Anderson BL, Mahoney J, Coleman-Cowger VH, Melstrom P, & Schulkin J (2014). Screening practices and attitudes of obstetricians-gynecologists toward new and emerging tobacco products. American Journal of Obstetrics and Gynecology, 211, 695.e1–695.e7. doi: 10.1016/j.ajog.2014.05.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- England LJ, Bunnell RE, Pechacek TF, Tong VT, & McAfee TA (2015). Nicotine and the developing human: A neglected element in the electronic cigarette debate. American Journal of Preventive Medicine, 49, 286–293. doi: 10.1016/j.amepre.2015.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etter J-F, & Bullen C (2011). Electronic cigarette: Users profile, utilization, satisfaction and perceived efficacy. Addiction, 106, 2017–2028. doi: 10.1111/j.1360-0443.2011.03505.x [DOI] [PubMed] [Google Scholar]
- Fallin A, Miller A, Assef S, & Ashford K (2016). Perceptions of electronic cigarettes among Medicaid-eligible pregnant and postpartum women. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 45, 320–325. doi:10.1016.jogn.2016.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farquhar B, Mark K, Terplan M, & Chisolm MS (2015). Demystifying electronic cigarette use in pregnancy. Journal of Addiction Medicine, 9, 157–158. doi: 10.1097/adm.0000000000000100 [DOI] [PubMed] [Google Scholar]
- Goniewicz ML, Kuma T, Gawron M, Knysak J, & Kosmider L (2012). Nicotine levels in electronic cigarettes. Nicotine & Tobacco Research. doi: 10.1093/ntr/nts103 [DOI] [PubMed] [Google Scholar]
- Graham H, Flemming K, Fox D, Heirs M, & Sowden A (2014). Cutting down: Insights from qualitative studies of smoking in pregnancy. Health & Social Care in the Community, 22, 259–267. doi: 10.1111/hsc.12080 [DOI] [PubMed] [Google Scholar]
- Grana R, Benowitz N, & Glantz SA (2014). E-cigarettes: A scientific review. Circulation, 129, 1972–1986. doi: 10.1161/circulationaha.114.007667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henningfield JE, & Zaatari GS (2010). Electronic nicotine delivery systems: Emerging science foundation for policy. Tobacco Control, 19, 89–90. doi: 10.1136/tc.2009.035279 [DOI] [PubMed] [Google Scholar]
- Kahr MK, Padgett S, Shope CD, Griffin EN, Xie SS, Gonzalez PJ, … Suter MA (2015). A qualitative assessment of the perceived risks of electronic cigarette and hookah use in pregnancy. BMC Public Health, 15, 1273. doi: 10.1186/s12889-015-2586-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King BA, Alam S, Promoff G, Arrazola R, & Dube SR (2013). Awareness and ever-use of electronic cigarettes among U.S. adults, 2010–2011. Nicotine & Tobacco Research, 15, 1623–1627. doi: 10.1093/ntr/ntt013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark KS, Farquhar B, Chisolm MS, Coleman-Cowger VH, & Terplan M (2015). Knowledge, attitudes, and practice of electronic cigarette use among pregnant women. Journal of Addiction Medicine, 9, 266–272. doi: 10.1097/ADM.0000000000000128 [DOI] [PubMed] [Google Scholar]
- McMillen RC, Gottlieb MA, Shaefer RMW, Winickoff JP, & Klein JD (2014). Trends in electronic cigarette use among U.S. adults: Use is increasing in both smokers and nonsmokers. Nicotine & Tobacco Research. doi: 10.1093/ntr/ntu213 [DOI] [PubMed] [Google Scholar]
- Pearson JL, Richardson A, Niaura RS, Vallone DM, & Abrams DB (2012). E-cigarette awareness, use, and harm perceptions in US adults. American Journal of Public Health, 102, 1758–1766. doi: 10.2105/ajph.2011.300526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regan AK, Promoff G, Dube SR, & Arrazola R (2013). Electronic nicotine delivery systems: Adult use and awareness of the ‘e-cigarette’ in the USA. Tobacco Control, 22, 19–23. doi: 10.1136/tobaccocontrol-2011-050044 [DOI] [PubMed] [Google Scholar]
- Schober W, Szendrei K, Matzen W, Osiander-Fuchs H, Heitmann D, Schettgen T, … Fromme H (2014). Use of electronic cigarettes (e-cigarettes) impairs indoor air quality and increases FeNO levels of e-cigarette consumers. International Journal of Hygiene and Environmental Health, 217, 628–637. doi: 10.1016/j.ijheh.2013.11.003 [DOI] [PubMed] [Google Scholar]
- Tong VT, Dietz PM, Morrow B, D’Angelo DV, Farr SL, Rockhill KM, & England LJ (2013). Trends in smoking before, during, and after pregnancy—Pregnancy Risk Assessment Monitoring System, United States, 40 sites, 2000–2010. Morbidity and Mortaility Weekly Report Surveillance Summaries, 62(6), 1–19. Retrieved from www.cdc.gov/mmwr/preview/mmwrhtml/ss6206a1.htm?utm_source=rss&utm_me [PubMed] [Google Scholar]
- Wickström R (2007). Effects of nicotine during pregnancy: Human and experimental evidence. Current Neuropharmacology, 5, 213–222. doi: 10.2174/157015907781695955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson DF, Serdula MK, Kendrick JS, & Binkin NJ (1989). Comparing the prevalence of smoking in pregnant and nonpregnant women, 1985 to 1986. JAMA, 261, 70–74. doi: 10.1001/jama.1989.03420010080037 [DOI] [PubMed] [Google Scholar]
- Zhu S-H, Gamst A, Lee M, Cummins S, Yin L, & Zoref L (2013). The use and perception of electronic cigarettes and snus among the U.S. population. PLOS ONE, 8, e79332-e79332. doi: 10.1371/journal.pone.0079332 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


