Abstract
Axial neck pain can frequently be a vexing clinical problem for practitioners. Cervical spine surgery is generally regarded as less successful for axial neck pain than arm complaints. Although only few case series exist in the literature, there is evidence to suggest that upper cervical radiculopathy could be an important, treatable source of axial neck pain. Unlike patients with axial neck pain, patients with radiculopathy usually present with unilateral pain, particularly in the trapezial, parascapular, mid clavicular, or even in the form of suboccipital headaches. Similar to other regions of the cervical spine, initial imaging often consists of plain radiographs of the cervical spine, with the use of magnetic resonance imaging (MRI) or computed tomography (CT) if further evaluation of the pathology is warranted. Selective injections and electromyography can be used in conjunction with the imaging studies to aid with proper diagnosis. The surgical management of upper cervical radiculopathy is reserved for patients who fail to improve with non-operative modalities. Anterior cervical discectomy and fusion (ACDF) remain the most commonly performed and most reliable procedure for the treatment of cervical radiculopathy. Wide decompression of disc material from uncinate to uncinate is performed with or without a foraminotomy on the symptomatic side to address anterior compressive pathology. Artificial disc replacement (ADR) has been recently introduced in hopes of maintaining motion at the pathologic levels. Young patients (<40 years old) with minimal facet joint arthrosis are best indicated for this surgery. Posterior cervical foraminotomy avoids many approach related complications associated with anterior surgery and is the preferred approach when anterior surgery is contraindicated. Very few studies with small sample sizes (likely due to underdiagnosis) make it difficult to perform a comparative analysis of the different types of procedures. Ultimately, an accurate diagnosis is likely the most important predictor of a positive surgical outcome.
Keywords: Upper cervical radiculopathy, anterior cervical discectomy fusion, artificial disc replacement, posterior cervical foraminotomy
Introduction
Axial neck pain can frequently be a vexing clinical problem for practitioners. Cervical spine surgery is generally regarded as less successful for axial neck pain than arm complaints. While there are a number of reasons for this finding, one reason is the significant difficulty in determining the cause of axial neck pain. Although only few case series exist in the literature, there is evidence to suggest that upper cervical radiculopathy could be an important, treatable source of axial neck pain1-3). In current practice, however, upper cervical radiculopathy might not be commonly diagnosed due to a lack of awareness among practitioners. In this review, we present an overview of the diagnosis, management, and outcomes of upper cervical radiculopathy.
Pathoanatomy
Upper cervical radiculopathy may refer to the compression of any upper cervical nerve root (C3, C4). As with the arm pain observed in lower cervical radiculopathy, compression of the upper cervical nerve roots produces pain along the associated dermatome with the only difference being that the dermatomal distribution of the upper cervical roots tends to center on the neck and suboccipital region.
Diagnosis
History and Physical Examination
Unlike radiculopathy of the lower cervical spine, upper cervical radiculopathies commonly present with neck and trapezial pain. This aspect of upper cervical radiculopathy can make diagnosis challenging as neck pain can have several potential sources1-3). The history and physical examination must focus on differentiating radicular symptoms from other causes of neck pain including discogenic complaints, myofascial pain, and facet arthrosis among others4-6). In most cases of cervical radiculopathy, however, the diagnosis can be made based on the patient history alone.
Unlike patients with axial neck pain, patients with radiculopathy usually present with unilateral pain. Jenis and An were the first to publish a series of patients presenting with upper cervical radiculopathy1). They described 4 patients with C4 radiculopathy who all complained of unilateral neck pain. The location of C3 and C4 radicular pain is in keeping with the classically described C3 and C4 dermatomes4-6). Park et al. described a series of 23 patients undergoing surgery for upper cervical radiculopathy. In their series, the majority of patients presented with suboccipital neck pain, most commonly in the trapezial region3). Ross and Ross published a series of 18 patients undergoing surgery for C4 radiculopathy and also described pain in the paraspinous and trapezial region in all patients2). Although the C4 dermatome does extend to the anterior chest wall, in their series Ross and Ross only had one patient complain of pain in the medial aspect of the clavicle. In cases of C2-C3 disc herniation, patients may present with a suboccipital headache with radiation to the temporal region (i.e., a cervicogenic headache)7-10).
In addition to patient history, physical examination maneuvers may help confirm the diagnosis of an upper cervical radiculopathy. Unlike lower cervical radiculopathies, upper extremity strength testing frequently reveals no deficits unless there is involvement of one of the lower cervical roots. Sensory testing, however, almost always shows a unilateral deficit in the periscapular or trapezial region1). Spurling's sign can be particularly helpful; Park et al. noted that 96% of patients (22/23) had a positive Spurling's test prior to surgery3). Other “classic” tests for cervical radiculopathy including axial compression and traction may also be helpful in the diagnosis upper cervical radiculopathy if they reproduce the patients' symptoms1).
As with all cervical radiculopathies, it is important to evaluate these patients for myelopathy. Patients with myelopathy will present with upper motor neuron signs including hyperreflexia, changes in gait and also have difficulty with fine motor tasks (changes in handwriting, buttoning shirts, etc.)11). Park et al. reported that 26% of their patients presented with myeloradiculopathy3).
Imaging
Imaging evaluation of upper cervical radiculopathy is similar to the workup of radiculopathy in other regions of the cervical spine. The imaging work up typically begins with radiographs of the cervical spine and proceeds to advanced imaging including computed tomography (CT) and magnetic resonance imaging (MRI)12) (Fig. 1).
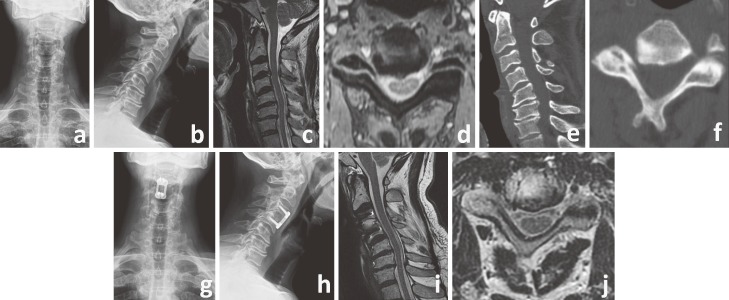
Figure 1.
A 53-year-old right hand dominant male presented with right-sided neck and trapezius pain with paresthesias that were recalcitrant to non-operative modalities. Epidural injections had provided significant but temporary relief. His neurologic exam was normal except for positive Spurling’s sign and decreased sensation in the C4 dermatome, both on the right. Radiographs (a, b) revealed multilevel spondylosis with 8 degrees of C2-7 kyhposis. MRI (c, d) and CT (e, f) showed severe right C3-4 foramenalstenosis, which correlated with his right C4 radicular symptoms. The patient underwent an uncomplicated C3-4 anterior cervical discectomy and fusion with right-sided foraminotomy (g, h). He experienced complete relief of his radicular symptoms, which was maintained at his most recent follow up visit (two years post-surgery). MRI (i, j) performed at that time for workup of neck pain revealed persistent multilevel spondylosis, particularly in the lower cervical spine, but no significant central or foraminal stenosis at C3-4.
Radiographs include anteroposterior (AP) and lateral views of the cervical spine. Oblique radiographs of the cervical spine may also be obtained to evaluate for the foraminal stenosis. Degenerative changes in the upper cervical motion segments (osteophyte formation, loss of disc height) may also be seen. Facet arthrosis is found most commonly in the upper cervical motion segments13).
CT scans with oblique foraminal reconstructions are especially helpful at detecting foraminal osteophytes causing impingement of the exiting nerve roots. MRI scans provide greater detail of any soft-tissue impingement and also allow for better evaluation of cord compression and signs of myelomalacia. MRI may be particularly useful in this patient population as upper cervical radiculopathy is most commonly due to a herniated nucleus pulposus1,3) (Fig. 2).
Figure 2.
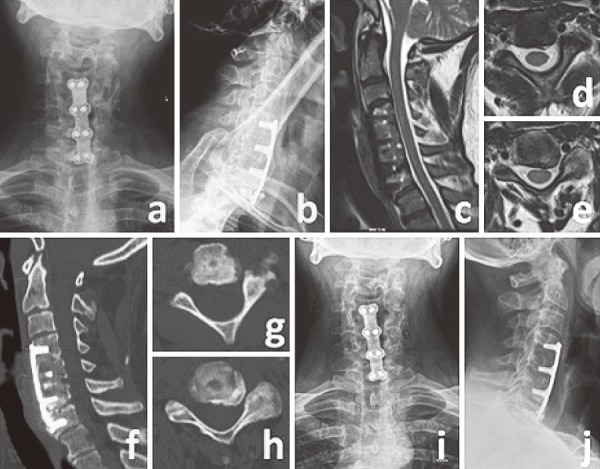
A 54-year-old right hand dominant male with a remote history of C4-7 anterior cervical discectomy and fusion presented with significant pain on the left side of his upper neck, face, and upper occiput. Prior to presentation, he was worked up for trigeminal neuralgia and found not to have it. He did, however, experience relief with high cervical epidural steroid injections, although this was temporary. On exam, he had limited cervical range of motion, tenderness to palpation in the upper cervical region, extending into the left occiput. There were no abnormalities on neurologic exam. Cervical spine radiographs showed the prior C4-7 fusion (a, b) with no instability on flexion-extension views. MRI revealed no central stenosis (c); there was left sided foraminal stenosis at C2-3 (d) and C3-4 (e). A possible C6-7 psuedarthrosis (f), which was not felt to be clinically symptomatic, as well as the C2-3 (g) and C3-4 (h) left foraminal stenosis were visualized on CT. The patient underwent left C2-3 and C3-4 posterior laminoforaminotomies. The postoperative course was uneventful, with resolution of his radicular symptoms. Subsequent radiographs show maintained alignment and disc height (i, j). Given the patient’s asymptomatic state, no postoperative axial imaging was obtained.
Selective Injections
Given the multiple potential causes of neck pain, selective cervical nerve root injections can be a helpful tool when diagnosing upper cervical radiculopathy. Although data is limited, some authors have described the utility of transforaminal epidural steroid injections in relieving cervicogenic headaches and upper cervical radicular symptoms. Park et al. noted that transforaminal epidural steroid injections generally serve only a diagnostic purpose and do not generally change the natural history of upper cervical radiculopathy3). An excellent response to a transforaminal epidural steroid injection is suggestive of an upper cervical radiculopathy.
Other special diagnostic tests might include electromyographic (EMG) studies. Unlike lower cervical radiculopathies, these tests may show no abnormalities although it is possible to see denervation of the muscles of the periscapular region1). EMG findings in the absence of imaging, however, are a relatively poor tool for localization of pathology14).
Management
Surgical Management
The surgical management of upper cervical radiculopathy is reserved for patients who fail to improve with non-operative modalities. Surgical management is dictated by the type of pathology leading to the radiculopathy.
Anterior cervical discectomy and fusion
This operation remains the most commonly performed and most reliable procedure for the treatment of cervical radiculopathy. Wide decompression of disc material from uncinate to uncinate is performed with or without a foraminotomy on the symptomatic side to address anterior compressive pathology. Indirect decompression of the nerve roots in a cephalad-caudal direction via restoration of foraminal height is obtained by placing an interbody graft. This is often the favored approach in the setting of primarily ventral pathology (i.e., - soft-tissue disc rupture or large anterior uncovertebral osteophytes) or when a posterior approach is contraindicated.
Artificial disc replacement
Artificial disc replacement (ADR) employs the same approach as an ACDF but instead of placing a graft for fusion, a motion device is placed in the intervertebral space. The device mimics normal disc biomechanics and is thought to preserve motion and therefore diminish the risk of adjacent segment degeneration and the need for further surgery. Strict criteria apply to the use of artificial discs including the absence of deformity, advanced spondylosis, and disc space collapse, and preservation of the posterior facet joints. Young patients (<40 years old) with minimal facet joint arthrosis presenting with upper cervical radiculopathy may be candidates for ADR.
Posterior Cervical Foraminotomy
Posterior cervical foraminotomy (PCF) is an excellent alternative to fusion operations for the treatment of upper cervical radiculopathy15-17). This operation involves an interlaminar laminotomy, partial medial facetectomy, and microforaminotomy. Removal of dorsal compressive lesions provides indirect decompression of the nerve root. This technique avoids the many approach related complications associated with anterior surgery (dysphagia, dysphonia, implant-related concerns). It is also the preferred approach when anterior surgery is contraindicated (i.e., - prior anterior surgery, history of neck irradiation). PCF is also significantly more cost-effective than ACDF since there are no implant-associated costs18).
Outcomes
Due to the under diagnosis of upper cervical radiculopathy, the literature available on the surgical management of this condition remains limited19). Jenis and An offered the first report on the surgical outcomes of 12 operatively managed patients with satisfactory, good, or excellent results in all patients according to Odom's criteria; ACDF was performed in 7/12 patients in this series1). Park et al. published the largest series to date looking at 23 patients who underwent primarily ACDF (15/23 cases) for radiculopathy involving the C3 or C4 nerve roots and found 87% of patients had good or excellent results3). In another review of 13 patients undergoing one- or two-level posterior foraminotomies and five patients undergoing ACDF for the diagnosis of C4 radiculopathy the authors found statistically significant improvements in mean ODI and SF-36 scores in both groups2). Lastly, a case report from Katsumi et al. describes the successful resolution of pain following a posterior cervical foraminotomy in a 41-year-old male with ossification of the posterior longitudinal ligament presenting with C4 radiculopathy19).
In each of the available studies, the sample sizes were too small to perform a comparative analysis of the different types of procedures. It should also be noted that artificial disc replacement was not evaluated in any of the available literature. Ultimately, an accurate diagnosis is likely the most important predictor of a positive surgical outcome. Further research on larger patient cohorts is warranted.
Summary
The clinical presentation of upper cervical radiculopathy can be a diagnostic challenge. A thorough history and physical examination, including provocative nerve root irritation maneuvers, as well as the use of selective nerve root blocks can allow for the accurate identification of this clinical syndrome. Surgical management is reserved for cases refractory to non-operative modalities. Successful surgical outcomes can be achieved with either ACDF or PCF and in some cases, disc arthroplasty may be an acceptable albeit unproven option.
Conflicts of Interest: The authors report no relevant financial conflicts of interest regarding this review article.
References
- 1.Jenis LG, An HS. Neck pain secondary to radiculopathy of the fourth cervical root: an analysis of 12 surgically treated patients. J Spinal Disord. 2000;13(4):345-9. [DOI] [PubMed] [Google Scholar]
- 2.Ross DA, Ross MN. Diagnosis and Treatment of C4 Radiculopathy. Spine. 2016;41(23):1790-4. [DOI] [PubMed] [Google Scholar]
- 3.Park MS, Kelly MP, Min W-K, et al. Surgical treatment of C3 and C4 cervical radiculopathies. Spine. 2013;38(2):112-8. [DOI] [PubMed] [Google Scholar]
- 4.Nishizawa S, Yokoyama T, Yokota N, et al. High cervical disc lesions in elderly patients--presentation and surgical approach. Acta Neurochir (Wien). 1999;141(2):119-26. [DOI] [PubMed] [Google Scholar]
- 5.Slipman CW, Plastaras CT, Palmitier RA, et al. Symptom provocation of fluoroscopically guided cervical nerve root stimulation. Are dynatomal maps identical to dermatomal maps? Spine. 1998;23(20):2235-42. [DOI] [PubMed] [Google Scholar]
- 6.Schirmer CM, Shils JL, Arle JE, et al. Heuristic map of myotomal innervation in humans using direct intraoperative nerve root stimulation. J Neurosurg Spine. 2011;15(1):64-70. [DOI] [PubMed] [Google Scholar]
- 7.Palit M, Schofferman J, Goldthwaite N, et al. Anterior discectomy and fusion for the management of neck pain. Spine. 1999;24(21):2224-8. [DOI] [PubMed] [Google Scholar]
- 8.Tanaka Y, Kokubun S, Sato T, et al. Cervical roots as origin of pain in the neck or scapular regions. Spine. 2006;31(17):E568-73. [DOI] [PubMed] [Google Scholar]
- 9.Schofferman J, Garges K, Goldthwaite N, et al. Upper cervical anterior diskectomy and fusion improves discogenic cervical headaches. Spine. 2002;27(20):2240-4. [DOI] [PubMed] [Google Scholar]
- 10.Dougherty C. Occipital neuralgia. Curr Pain Headache Rep. 2014;18(5):411. [DOI] [PubMed] [Google Scholar]
- 11.Edwards CC, Riew KD, Anderson PA, et al. Cervical myelopathy. current diagnostic and treatment strategies. Spine J. 2003;3(1):68-81. [DOI] [PubMed] [Google Scholar]
- 12.Levine M, Albert T, Smith M. Cervical Radiculopathy: Diagnosis and Nonoperative Management. J Am Acad Orthop Surg. 1996;4(6):305-16. [DOI] [PubMed] [Google Scholar]
- 13.Lee MJ, Riew KD. The prevalence cervical facet arthrosis: an osseous study in a cadveric population. Spine J. 2009;9(9):711-4. [DOI] [PubMed] [Google Scholar]
- 14.Haig AJ, Geisser ME, Tong HC, et al. Electromyographic and magnetic resonance imaging to predict lumbar stenosis, low-back pain, and no back symptoms. J Bone Joint Surg Am. 2007;89(2):358-66. [DOI] [PubMed] [Google Scholar]
- 15.Skovrlj B, Gologorsky Y, Haque R, et al. Complications, outcomes, and need for fusion after minimally invasive posterior cervical foraminotomy and microdiscectomy. Spine J. 2014;14(10):2405-11. [DOI] [PubMed] [Google Scholar]
- 16.Cho TG, Kim YB, Park SW. Long term effect on adjacent segment motion after posterior cervical foraminotomy. Korean J Spine. 2014;11(1):1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Faught RW, Church EW, Halpern CH, et al. Long-term quality of life after posterior cervical foraminotomy for radiculopathy. Clin Neurol Neurosurg. 2016;142:22-5. [DOI] [PubMed] [Google Scholar]
- 18.Mansfield HE, Canar WJ, Gerard CS, et al. Single-level anterior cervical discectomy and fusion versus minimally invasive posterior cervical foraminotomy for patients with cervical radiculopathy: a cost analysis. Neurosurg Focus. 2014;37(5):E9. [DOI] [PubMed] [Google Scholar]
- 19.Katsumi K, Yamazaki A, Watanabe K, et al. The characteristic clinical symptoms of C-4 radiculopathy caused by ossification of the posterior longitudinal ligament. J Neurosurg Spine. 2014;20(5):480-4. [DOI] [PubMed] [Google Scholar]