Abstract
Introduction
Global spinal balance and its relationship to the pelvis have received much attention, and various formulae have been used to predict postoperative spinopelvic alignment for spinal surgery. However, previous studies had limitations because no consideration was given to the dynamic factor.
Methods
Fifteen healthy adults without any lumbar disorder (group A) and 9 L4-spondylolisthesis patients (Group B) volunteered to participate in the study. Sequential images were captured with the subjects in the standing position with maximal forward bending followed by backward bending using a dynamic flat panel detector system. Spinopelvic parameters (LL: lumbar lordosis, SA: sacrofemoral angle, SS: sacral slope, PI: pelvic incidence, DP: distance of the horizontal movement of the pelvis) were evaluated. We also investigated the relationship between LL and SA (lumbar/hip [L/H] ratio) as the spinopelvic rhythm.
Results
In group A, the mean change in LL was 83.2 ± 9.5°; change in SA, 45.4 ± 16.6°; SS, 42.6 ± 8.9°; PI, 43.2 ± 7.7°; DP, 15.7 ± 3.4 cm, and L/H ratio, 3.6 ± 2.7. However, spinopelvic rhythm changed over time, because the change in LL was larger than the change in SA from the middle of the rising motion to the upright position. In group B, the mean change in LL was 50.3 ± 8.0°; SA, 56.9 ± 16.0°; SS, 27.5 ± 13.5°; PI, 47.4 ± 10.4°; DP, 12.7 ± 6.8 cm; and L/H ratio, 1.0 ± 0.5.
Conclusions
When compared with the change in LL, individual differences were largely noted in the change in SA. These results demonstrated that the range of hip joint motion under physiological conditions, unlike anatomical motion, differed substantially between individuals. Therefore, spinopelvic rhythm is dependent on the change in SA.
Keywords: Spinopelvic rhythm, Global spinal balance, dynamic factor
Introduction
It is generally known that the normal coronal alignment of the human spine is straight. However, the sagittal alignment of the spine and pelvis in a standardized standing position varies considerably between individuals1,2). Sagittal plumb lines for spinal balance, which have been measured in various ways, have also shown wide cross-sectional variations among different volunteer and patient populations2-8). Global spinal balance and its relationship to the pelvis have received increased attention because recent studies have shown that sagittal plane alignment is highly correlated with disability and quality of life9-12). The analysis of sagittal balance has recently appeared to be essential in the management of lumbar degenerative pathologies, especially after spinal fusion is achieved13-19). The pelvis is characterized by an important anatomic landmark. Pelvic incidence (PI) does not change after adolescence. It directly influences pelvic alignment and such parameters as pelvic tilt (PT), sacral slope (SS), lumbar lordosis (LL), and overall sagittal spinal balance. In the occurrence of an elevated PI, the spine adapts by increasing LL. To prevent or limit sagittal imbalance, the spine may also compensate by increasing PT or pelvic retroversion in an attempt to maintain an upright posture. Abnormal spinopelvic parameters contribute to the occurrence of multiple spinal conditions, including isthmic spondylolysis, degenerative spondylolisthesis, and deformity, and impact outcome after spinal fusion.
It is no longer acceptable to perform spine surgery without considering global spinal balance and the spinopelvic junction20,21). Lafage et al. have published predictive formulae that allow the calculation of postoperative PT and sagittal vertical axis values from PI, LL, thoracic kyphosis (TK), and patient's age22). Although preoperative planning is essential for spinal deformity surgery and various formulae are used to predict the postoperative spinopelvic alignment23-27), these classifications and formulae have limitations because no consideration is given to the dynamic factor.
We, therefore, investigated the characteristics of spinopelvic rhythm in healthy male adults and elderly spondylolisthesis patients.
Materials and Methods
This study included 15 healthy adults and 9 spondylolisthesis patients. Group A comprised 15 healthy male adults, aged 30.6 ± 6.2 (range, 22-43) years old, with no lumbar disorder. Group B comprised 9 patients (7 males and 2 females), aged 73.26 ± 6.1 (range, 67-85) years old, with degenerative spondylolisthesis at L4, who had been scheduled for lumbar surgery. This study was approved by the ethics committee of our institution, and informed consent was obtained from all patients prior to their inclusion in the study.
Imaging with a dynamic flat panel detector system (CXDI-50RF; Canon, Tokyo, Japan) and X-ray tube (ROTANODE; DRX-1414A 1. 3/0. 6, TOSHIBA, Tokyo, Japan) was performed under the following imaging conditions: 70 kV, 4 mA, 10 ms, source-detector distance 100 cm, and 2 frames/s. Sequential images were captured with the subjects in the standing position with maximal forward bending followed by backward bending for 10 s at a constant rate. As a result, 20 lateral radiographs from L1 to the femur were obtained. The matrix size of an acquisition picture was 1110 × 1340 pixels, and the pixel size was 0.32 mm. The total radiation dose was 9.8 mGy, which was similar to that of two projections of conventional lumbar lateral imaging (10.8 mGy). For improved reproducibility of the kinetic test, the patients were given sufficient explanations regarding the procedure and how they should participate before actual imaging. Horizontal front-back movement of the pelvis was allowed, but knee joint movement was restricted.
We used ImageJ (ver. 1.47v, National Institutes of Health, USA) to analyze the images. Each point was measured three times per frame, and the average values were used for the calculation of the spinopelvic parameters. Neutral position was defined as the frame whose vertical axis was parallel to the line drawn from the posterior edge of the inferior L1 endplate to the anterior edge of the S1 endplate. Spinopelvic alignment was evaluated using the following parameters: LL, SA: sacrofemoral angle (the angle formed between the axis of the femur and the line tangent to the upper endplate of S1), SS: sacral slope, PI, DP: distance of pelvis movement (the horizontal offset between the vertical line and the posterior edge of the S1 endplate). Change in LL and SA was plotted in a chronological order with the maximum forward bending as the reference point (Fig. 1). DP was also plotted in a chronological order. For validation of the spinopelvic rhythm, we investigated the lumbar/hip ratio (L/H ratio), which was calculated by dividing the change in LL by the change in SA. We also investigated the relationship between spinopelvic parameter.
Figure 1.
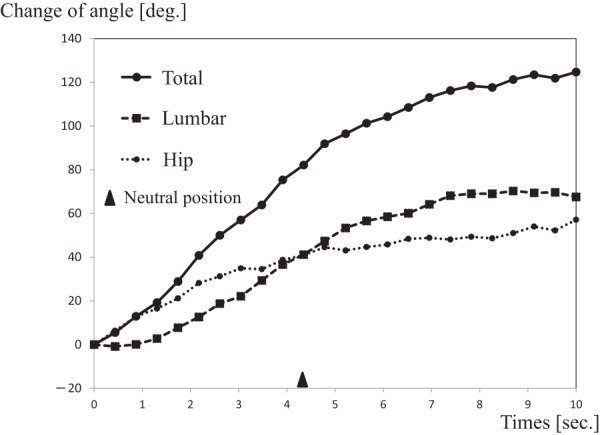
Plotted lumbar lordosis (LL) and sacrofemoral angle (SA) in chronological order.
The results are presented as mean ± standard deviation. Statistical analysis was performed using Pearson's correlation. We considered P < 0.05 to be statistically significant in all our analyses, which were performed using SPSS version 20 (IBM, Armonk, NY, USA).
Results
The mean lumbar spine motion, hip motion, L/H ratio, DP, and other spinopelvic parameters during maximal forward bending followed by backward bending are summarized in Table 1. In group A, the mean change in LL was 83.2 ± 9.5°; SA, 45.4 ± 16.6°; SS, 42.6 ± 8.9°; PI, 43.2 ± 7.7°; DP, 15.7 ± 3.4 cm; and L/H ratio, 3.6 ± 2.7. However, the spinopelvic rhythm changed over time, because the change in LL was larger than the change in SA, from the middle of the rising motion to the upright position (Fig. 2a). In group B, the mean change in LL was 50.3 ± 8.0°; SA, 56.9 ± 16.0°; SS, 27.5 ± 13.5°; PI, 47.4 ± 10.4°; DP, 12.7 ± 6.8 cm; and L/H ratio, 1.0 ± 0.5. The spinopelvic rhythm in group B, compared with group A, remained relatively constant (Fig. 2b).
Table 1.
Data of the Investigated Patients.
| Group A | Change of LL | Change of SA | Total | SS | PI | DP |
|---|---|---|---|---|---|---|
| 1 | 67.6 | 61.9 | 129.5 | 36.8 | 45.7 | 15.1 |
| 2 | 68.5 | 53.5 | 122.0 | 45.2 | 39.5 | 21.3 |
| 3 | 74.5 | 9.0 | 83.5 | 45.7 | 40.2 | 10.7 |
| 4 | 74.7 | 37.7 | 112.4 | 54.4 | 46.8 | 14.3 |
| 5 | 77.9 | 55.5 | 133.4 | 34.2 | 41.8 | 13.1 |
| 6 | 79.1 | 69.0 | 148.1 | 32.8 | 43.7 | 22.7 |
| 7 | 80.5 | 46.5 | 126.9 | 48.8 | 47.3 | 16.5 |
| 8 | 82.7 | 45.4 | 128.2 | 54.3 | 38.8 | 12.4 |
| 9 | 84.5 | 53.2 | 137.7 | 39.7 | 39.2 | 15.3 |
| 10 | 84.9 | 17.9 | 102.8 | 28.1 | 31.6 | 10.6 |
| 11 | 88.8 | 26.1 | 114.9 | 27.8 | 29.5 | 19.0 |
| 12 | 95.6 | 46.9 | 142.5 | 39.6 | 50.5 | 16.2 |
| 13 | 95.9 | 57.6 | 153.5 | 48.9 | 40.4 | 13.4 |
| 14 | 96.4 | 36.4 | 132.8 | 54.4 | 51.4 | 16.5 |
| 15 | 96.6 | 64.1 | 160.7 | 47.8 | 62.0 | 18.5 |
| Mean | 83.2 | 45.4 | 128.6 | 42.6 | 43.2 | 15.7 |
| STDEV | 9.5 | 16.6 | 19.2 | 8.9 | 7.7 | 3.4 |
| Group B | Change of LL | Change of SA | Total | SS | PI | DP |
| 1 | 36.6 | 68.6 | 105.2 | 36.5 | 45.7 | 10.0 |
| 2 | 42.4 | 77.5 | 119.9 | 17.7 | 36.2 | 24.2 |
| 3 | 46.6 | 45.2 | 91.8 | 25.6 | 30.1 | 8.9 |
| 4 | 48.0 | 54.9 | 102.9 | 32.7 | 47.3 | 6.9 |
| 5 | 50.4 | 66.0 | 116.4 | 50.6 | 58.6 | 21.8 |
| 6 | 52.3 | 51.5 | 103.7 | 27.6 | 60.5 | 9.9 |
| 7 | 54.7 | 75.6 | 130.3 | 25.7 | 40.3 | 14.7 |
| 8 | 60.3 | 41.8 | 102.1 | 0.9 | 53.3 | 3.4 |
| 9 | 61.1 | 31.1 | 92.3 | 29.8 | 54.6 | 15.0 |
| Mean | 50.3 | 56.9 | 107.2 | 27.5 | 47.4 | 12.7 |
Figure 2.
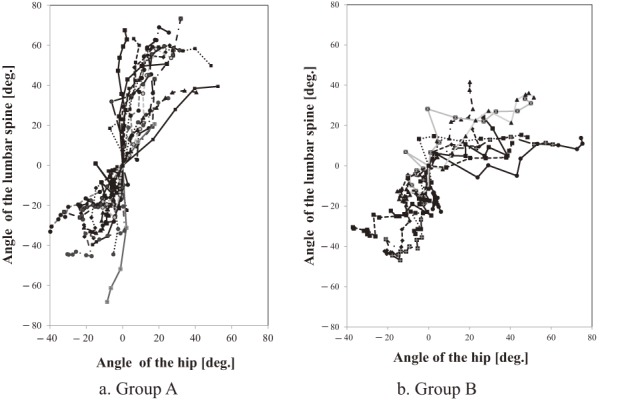
Relationship between lumbar lordosis (LL) and sacrofemoral angle (SA) (L/H ratio).
For both groups, individual differences were more marked in the change in SA than in the change in LL. Fig. 2 demonstrates the spinopelvic rhythm in each case.
Correlation between spinopelvic parameters is summarized in Table 2. No significant correlation between each parameter was observed.
Table 2.
Correlation between Spinopelvic Parameters.
| Group A | LL | SA | SS | PI |
|---|---|---|---|---|
| LL | ||||
| SA | 0.005 (0.985) | |||
| SS | 0.113 (0.688) | 0.062 (0.826) | ||
| PI | 0.289 (0.295) | 0.466 (0.080) | 0.511 (0.052) | |
| DP | −0.462 (0.083) | −0.26 (0.927) | 0.043 (0.878) | 0.103 (0.715) |
| Group B | LL | SA | SS | PI |
| LL | ||||
| SA | −0.618 (0.76) | |||
| SS | −0.345 (0.363) | 0.250 (0.516) | ||
| PI | 0.466 (0.206) | −0.319 (0.403) | 0.231 (0.549) | |
| DP | −0.207 (0.592) | 0.545 (0.129) | 0.405 (0.279) | −0.80 (0.839) |
Pearson’s correlation coefficient between each spinopelvic parameter. All satistically significant correlations are bolded.
Discussion
Given that sagittal plane alignment is determined by the interaction between spinal and pelvic parameters, understanding the spinopelvic balance is fundamental28,29). Although it is considered that proper alignment in an individual is also influenced by dynamic factors, a few reports have investigated the relationship between the spine and hip joint30-35). According to these reports, the kinetic changes in lumbar and hip motion vary between individuals. Spinopelvic rhythm is another aspect of the understanding of spinal kinematics and spinal motion with respect to dynamic sagittal alignment31,36). Esola et al. reported that lumbopelvic ratios in healthy subjects for early, middle, and late forward bending were 1.9, 0.9, and 0.4, respectively. This means that the rate of hip movement gradually exceeds lumbar movement as forward bending occurs31). Hasebe et al. also reported on lumbopelvic rhythm. In this report, lumbopelvic ratios for early, middle, and late forward bending were 4.0, 1.0, and 0.4, respectively30).
The feature of this study was that while back and forth movement of the pelvis was allowed, the knees were restricted to the extended position alone. As in previous reports, in this study, the early movement from maximum flexion started with the pelvis, and the percentage of movement of the lumbar spine was rapidly increased. The movement of the lumbar spine was 83.2 ± 9.5°, and individual differences were relatively small based on the standard deviation in group A. On the other hand, individual differences were notable regarding the movement of the hip joint and the movement distances of the pelvis back and forth. In particular, the movement of the hip joint was found to have a considerable variation with a standard deviation of 16.6° even in group A, which comprised healthy adults. Furthermore, the hip joint changed by more than 5° even after movement of the lumbar spine stopped at the end of extension movement in 5 cases in the healthy group. Even among young healthy individuals, the position of the center of gravity and movement in the anterior-posterior direction of the pelvis were found to differ individually. This greatly affected the lumbopelvic rhythm (Fig. 3). If the anterior movement of the pelvis is increased by the extension motion, the change in SS decreases and the hip joint moves even after the maximum lordotic posture has been attained. The center of the gravity line is reported to pass through the center of the pelvis and the foot in the normal standing position28). However, it can be seen that the lumbar spine is more curved in a kyphotic manner if the center of gravity is located posteriorly and the pelvis is located behind the center of the gravity line. It is also reported that the movement of the hip joint becomes smaller in the presence of a tight hamstring3). From the above, dynamic alignment is not constant even in a healthy person. We believe that these factors influence the difference in rhythm individually.
Figure 3.
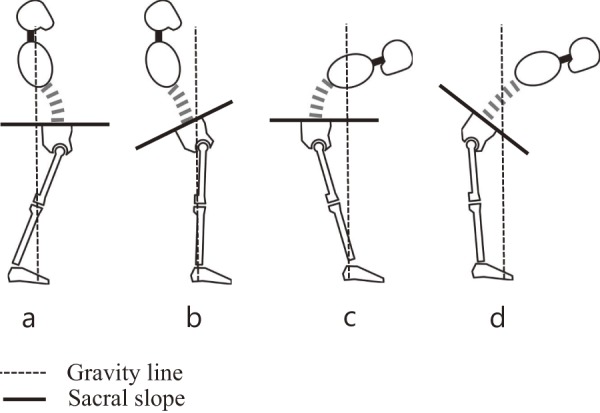
Pattern of sagittal balance.
We considered that the L/H ratio in group B was smaller because of compensatory hip movement as in previous studies. As the elderly age further, LL decreases, TK progresses, and the gravity line gradually shifts forward28). These changes make lumbar spinopelvic rhythm more complicated for elderly patients with lumbar spine disease. In current correction surgery for adult deformity, spinal fusion is indispensable. When the compensating function exceeds its limit, it is considered that spinal alignment is broken, and the group that can acquire normal alignment also acquires a higher quality of life11). We consider that individual differences in the range of hip motion and the back and forth distance of the pelvis could contribute to the magnitude of future compensatory functions. Therefore, although appropriate alignment of individuals is affected by lumbopelvic rhythm, it is difficult to generalize and standardize lumbopelvic rhythm in spinal fusion surgery.
Conclusion
Static alignment using sagittal spinopelvic parameters in the upright position is an important index in spinal fusion surgery. However, an individual's proper alignment settings should be determined with reference not only to standardized static alignment but also to dynamic alignment. Even among young healthy individuals, there are large individual differences in the range of hip joint motion compared with lumbar spine motion. The position of the center of gravity and movement in the anterior-posterior direction of the pelvis differed individually, and this greatly affected the lumbopelvic rhythm. We believe that the allowable range of proper spinal alignment varies depending on individual spinopelvic rhythm. In recent years, the total sagittal alignment from the cervical vertebra to the ankle has gradually become an important topic, and three-dimensional alignment analysis is also progressing37). Hence, it is necessary to study the relationship between spinal sagittal alignment and quality of life with consideration for dynamic factors.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Author Contributions: Katsuhito Yoshioka wrote and prepared the manuscript, and all of the authors participated in the study design. All authors have read, reviewed, and approved the article.
References
- 1.Stagnara P, De Mauroy JC, Dran G, et al. Reciprocal angulation of vertebral bodies in a sagittal plane: approach to references for the evaluation of kyphosis and lordosis. Spine. 1982;7(4):335-42. [DOI] [PubMed] [Google Scholar]
- 2.Roussouly P, Gollogly S, Berthonnaud E, et al. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30(3):346-53. [DOI] [PubMed] [Google Scholar]
- 3.Sairyo K, Kawamura T, Mase Y, et al. Jack-knife stretching promotes flexibility of tight hamstrings after 4 weeks: a pilot study. Eur J Orthop Surg Traumatol. 2013;23(6):657-63. [DOI] [PubMed] [Google Scholar]
- 4.Gelb DE, Lenke LG, Bridwell KH, et al. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20(12):1351-8. [PubMed] [Google Scholar]
- 5.Jackson RP, Kanemura T, Kawakami N, et al. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine. 2000;25(5):575-86. [DOI] [PubMed] [Google Scholar]
- 6.During J, Goudfrooij H, Keessen W, et al. Toward standards for posture. Postural characteristics of the lower back system in normal and pathologic conditions. Spine. 1985;10(1):83-7. [PubMed] [Google Scholar]
- 7.Legaye J, Duval-Beaupere G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boulay C, Tardieu C, Hecquet J, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15(4):415-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lafage V, Schwab F, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine. 2009;34(17):E599-606. [DOI] [PubMed] [Google Scholar]
- 10.Hikata T, Watanabe K, Fujita N, et al. Impact of sagittal spinopelvic alignment on clinical outcomes after decompression surgery for lumbar spinal canal stenosis without coronal imbalance. J Neurosurg Spine. 2015;23(4):451-8. [DOI] [PubMed] [Google Scholar]
- 11.Terran J, Schwab F, Shaffrey CI, et al. The SRS-Schwab adult spinal deformity classification: assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery. 2013;73(4):559-68. [DOI] [PubMed] [Google Scholar]
- 12.Funao H, Tsuji T, Hosogane N, et al. Comparative study of spinopelvic sagittal alignment between patients with and without degenerative spondylolisthesis. Eur Spine J. 2012;21(11):2181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lazennec JY, Ramare S, Arafati N, et al. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9(1):47-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berthonnaud E, Dimnet J, Roussouly P, et al. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18(1):40-7. [DOI] [PubMed] [Google Scholar]
- 15.Korovessis P, Dimas A, Iliopoulos P, et al. Correlative analysis of lateral vertebral radiographic variables and medical outcomes study short-form health survey: a comparative study in asymptomatic volunteers versus patients with low back pain. J Spinal Disord Tech. 2002;15(5):384-90. [DOI] [PubMed] [Google Scholar]
- 16.Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001;10(4):314-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morel E, Ilharreborde B, Lenoir T, et al. Sagittal balance of the spine and degenerative spondylolisthesis. Rev Chir Orthop Reparatrice Appar Mot. 2005;91(7):615-26. [DOI] [PubMed] [Google Scholar]
- 18.Barrey C, Jund J, Perrin G, et al. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery. 2007;61(5):981-6. [DOI] [PubMed] [Google Scholar]
- 19.Ferrero E, Ould-Slimane M, Gille O, et al. Sagittal spinopelvic alignment in 654 degenerative spondylolisthesis. Eur Spine J. 2015;24(6):1219-27. [DOI] [PubMed] [Google Scholar]
- 20.Mehta VA, Amin A, Omeis I, et al. Implications of spinopelvic alignment for the spine surgeon. Neurosurgery 2012;70(3):707-21. [DOI] [PubMed] [Google Scholar]
- 21.Lamartina C, Berjano P. Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms. Eur Spine J. 2014;23(6):1177-89. [DOI] [PubMed] [Google Scholar]
- 22.Lafage V, Schwab F, Vira S, et al. Spino-pelvic parameters after surgery can be predicted: a preliminary formula and validation of standing alignment. Spine. 2011;36(13):1037-45. [DOI] [PubMed] [Google Scholar]
- 23.Schwab F, Lafage V, Farcy JP, et al. Surgical rates and operative outcome analysis in thoracolumbar and lumbar major adult scoliosis: application of the new adult deformity classification. Spine. 2007;32(24):2723-30. [DOI] [PubMed] [Google Scholar]
- 24.Lafage V, Bharucha NJ, Schwab F, et al. Multicenter validation of a formula predicting postoperative spinopelvic alignment. J Neurosurg Spine. 2012;16(1):15-21. [DOI] [PubMed] [Google Scholar]
- 25.Vialle R, Levassor N, Rillardon L, et al. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87(2):260-7. [DOI] [PubMed] [Google Scholar]
- 26.Yamato Y, Hasegawa T, Kobayashi S, et al. Calculation of the target lumbar lordosis angle for restoring an optimal pelvic tilt in elderly patients with adult spinal deformity. Spine. 2016;41(4):E211-7. [DOI] [PubMed] [Google Scholar]
- 27.Inami S, Moridaira H, Takeuchi D, et al. Optimum pelvic incidence minus lumbar lordosis value can be determined by individual pelvic incidence. Eur Spine J. 2016;25(11):3638-43. [DOI] [PubMed] [Google Scholar]
- 28.Garbossa D, Pejrona M, Damilano M, et al. Pelvic parameters and global spine balance for spine degenerative disease: the importance of containing for the well being of content. Eur Spine J. 2014;23(Suppl 6):616-27. [DOI] [PubMed] [Google Scholar]
- 29.Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine. 2012;37(12):1077-82. [DOI] [PubMed] [Google Scholar]
- 30.Hasebe K, Sairyo K, Hada Y, et al. Spino-pelvic-rhythm with forward trunk bending in normal subjects without low back pain. Eur J Orthop Surg Traumatol. 2014;24(Suppl 1):193-9. [DOI] [PubMed] [Google Scholar]
- 31.Esola MA, McClure PW, Fitzgerald GK, et al. Analysis of lumbar spine and hip motion during forward bending in subjects with and without a history of low back pain. Spine. 1996;21(1):71-8. [DOI] [PubMed] [Google Scholar]
- 32.Dolan P, Adams MA. Influence of lumbar and hip mobility on the bending stresses acting on the lumbar spine. Clin Biomech. 1993;8(4):185-92. [DOI] [PubMed] [Google Scholar]
- 33.Paquet N, Malouin F, Richards CL. Hip-spine movement interaction and muscle activation patterns during sagittal trunk movements in low back pain patients. Spine. 1994;19(5):596-603. [DOI] [PubMed] [Google Scholar]
- 34.Porter JL, Wilkinson A. Lumbar-hip flexion motion. A comparative study between asymptomatic and chronic low back pain in 18- to 36-year-old men. Spine. 1997;22(13):1508-13. [DOI] [PubMed] [Google Scholar]
- 35.Wong TK, Lee RY. Effects of low back pain on the relationship between the movements of the lumbar spine and hip. Hum Mov Sci. 2004;23(1):21-34. [DOI] [PubMed] [Google Scholar]
- 36.McClure PW, Esola M, Schreier R, et al. Kinematic analysis of lumbar and hip motion while rising from a forward, flexed position in patients with and without a history of low back pain. Spine. 1997;22(5):552-8. [DOI] [PubMed] [Google Scholar]
- 37.Hasegawa K, Okamoto M, Hatsushikano S, et al. Standing sagittal alignment of the whole axial skeleton with reference to the gravity line in humans. J Anat. 2017;230(5):619-30. [DOI] [PMC free article] [PubMed] [Google Scholar]


