Abstract
Introduction
Numerous studies have reported the risk factors of osteoporotic vertebral collapse. However, whether spino-pelvic and global spinal alignments are associated with the occurrence of osteoporotic vertebral collapse remains unclear. This study aimed to investigate the association between spino-pelvic and global spinal alignments and the occurrence of osteoporotic vertebral collapse.
Methods
A total of 46 consecutive patients who underwent a nonoperative treatment for a single-level fresh osteoporotic thoracolumbar vertebral compression fracture (T10 to L3) were retrospectively reviewed. The parameters evaluated were the pelvic incidence, anterior deviation of the C7 plumb line, distance between the C7 plumb line and the center of the fractured vertebra, and kyphotic wedge angle of the fractured vertebra in a standing whole-spine radiograph at the beginning of the nonoperative treatment. As an outcome measure, the presence or absence of osteoporotic vertebral collapse was radiographically evaluated at the final follow-up. Multiple logistic regression analysis was used to determine significant risk factors of osteoporotic vertebral collapse.
Results
The mean values for each parameter were as follows: pelvic incidence, 58.0 degrees; anterior deviation of the C7 plumb line, 3.0 cm; distance between the C7 plumb line and the center of the fractured vertebra, 5.7 cm; and kyphotic wedge angle of the fractured vertebra, 14.6 degrees. Multiple logistic regression analysis revealed that the distance between the C7 plumb line and center of the fractured vertebra was a significant risk factor of osteoporotic vertebral collapse (p = 0.012; odds ratio, 1.025). The anterior deviation of the C7 plumb line (p = 0.214), pelvic incidence (p = 0.728), and kyphotic wedge angle of the fractured vertebra (p = 0.07) did not affect the occurrence of osteoporotic vertebral collapse.
Conclusions
A large distance between the C7 plumb line and center of the fractured vertebra was a significant risk factor of osteoporotic vertebral collapse. The distance approximately represents that of between gravity center of trunk cranial to the fractured vertebra and the fractured vertebra. Accordingly, the large distance may cause larger flexion moment to the fractured site, leading to stress concentration that results in insufficient bone healing.
Keywords: spino-pelvic alignment, global spinal alignment, osteoporotic vertebral collapse, osteoporotic vertebral compression fracture, sagittal imbalance
Introduction
A major healthcare problem in aging populations is osteoporosis and its related fractures of the spine and femur bone. Osteoporotic vertebral compression fractures (OVFs) in the elderly seriously affect their quality of life, possibly leading to being bedridden for the rest of their lives1-3). Most of the time, a nonoperative treatment with braces and early physical therapy is effective4). If appropriate treatment is administered with early intervention, patients can return to ambulatory status after an injury. Nevertheless, there are some patients who develop vertebral collapse or pseudoarthrosis. Osteoporotic vertebral collapse (OVC) worsens prognosis, with prolonged pain or subsequent neurological impairment5,6).
The reported risk factors of OVC are thoracolumbar vertebral fractures5,7), aging7), middle column injuries5,8), and confined high-or diffuse low-intensity areas of the fractured vertebra on T2-weighted MR images5). Despite numerous studies regarding OVF, whether spino-pelvic and global spinal alignments are associated with the occurrence of OVC remains unknown.
This retrospective study aimed to investigate the association between spino-pelvic and global spinal alignments and the occurrence of OVC.
Materials and Methods
This study was approved by the institutional review board of our hospital. We have adhered to the 1964 Helsinki Declaration and its later amendments of comparable ethical standards.
Patient population
A total of 46 consecutive patients who underwent a nonoperative treatment for a single-level fresh thoracolumbar OVF (T10 to L3) were retrospectively reviewed. Of 46 patients, 36 were females and 10 were males, with a mean age of 80 (range, 62-94) years. The fracture levels were T11 in eight patients, T12 in 17, L1 in eight, L2 in eight, and L3 in five.
The fresh vertebral fracture was diagnosed on the basis of low-intensity areas of the vertebra on T1-weighted MR images and high-intensity areas of the vertebra on T2-weighted, short inversion time inversion-recovery MR images. We diagnosed OVF within 2-3 days after the injury and performed a nonoperative treatment for every patient. During the follow-up, we encountered some patients' status deteriorate from OVF to OVC.
Bone mineral densities were measured as a percentage of the young adult mean (YAM) using dual-energy X-ray absorptiometry. The average and range of the percentage of YAM of the lumbar vertebra were 66% and 37%-86%, respectively, and those of the femoral neck were 69% and 45%-96%, respectively.
Of 46 patients, 45 (98%) underwent pharmaceutical osteoporosis treatment. Forty-two patients were treated with bisphosphonate, two with selective estrogen receptor modulator, and one with vitamin D. Teriparatide was not used in the current series.
Patients with more than two preexisting vertebral fractures, candidates for spinal surgeries, and patients who were administered teriparatide were not included.
Radiographic assessment
The radiographic parameters assessed were the pelvic incidence (PI), anterior deviation of the C7 plumb line from the posterior corner of the sacrum (SVA), distance between the C7 plumb line and center of the fractured vertebra (DSVA) (Fig. 1), and kyphotic wedge angle of the fractured vertebra. The parameters were measured using standing whole-spine radiographs before initiating the nonoperative treatment. Therefore, the radiographic parameters in this study represent the global spinal alignment 2-3 days after the injury rather than the pre-traumatic global spinal alignment.
Figure 1.
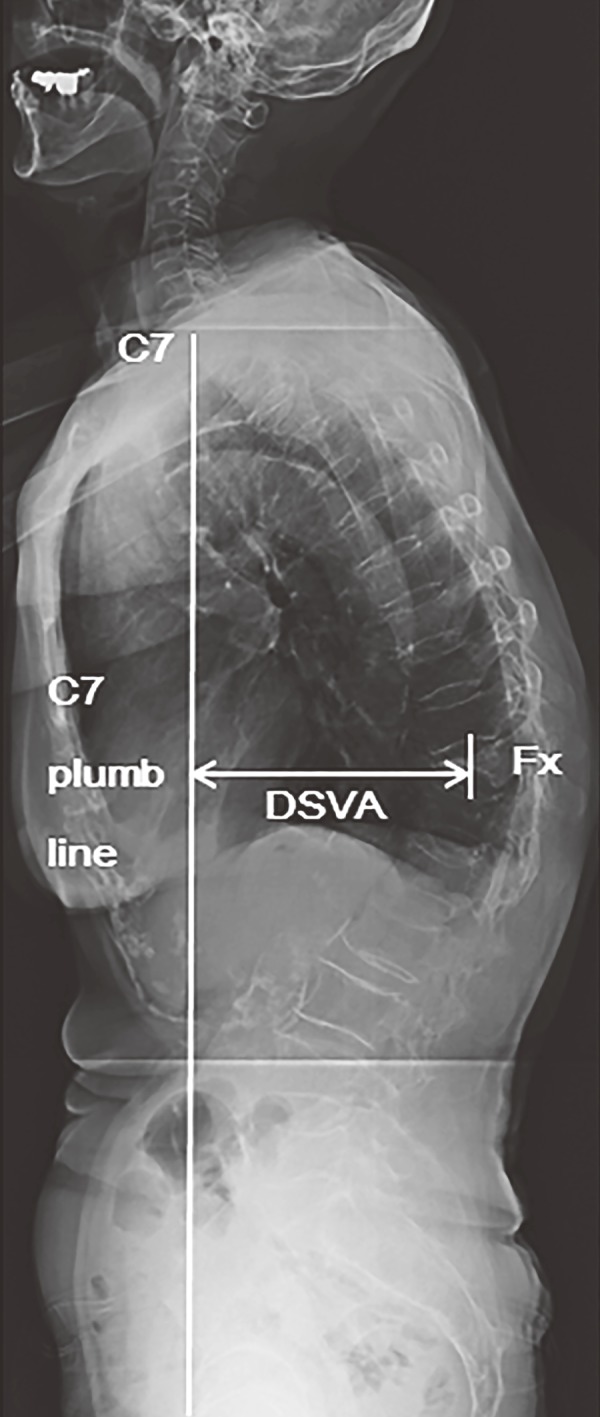
Distance of the C7 plumb line to the center of the fractured vertebra (DSVA) in the standing whole-spine radiograph before initiating the nonoperative treatment. Fx indicates the fractured vertebra.
As an outcome measure, the presence or absence of OVC was radiographically evaluated at the final follow-up. Because OVC has not been clearly defined previously and to specifically describe our outcome measure, we defined OVC as follows: the mid-vertebral body height of the non-traumatically fractured vertebra decrease to <40% with reference to the heights of adjacent vertebrae; the reference value is the average height of the upper and lower adjacent vertebrae. The mean follow-up period was 18 months.
Statistical analyses
The Wilcoxon test was used to compare the OVC and non-OVC groups with regard to age and the percentages of YAM bone mineral density of the lumbar vertebra and femoral neck. Unpaired t-tests were used to compare the OVC and non-OVC groups regarding PIs, SVAs, DSVAs, and kyphotic wedge angles. Multiple logistic regression analysis was performed to determine the significant risk factors of OVC with respect to PIs, SVAs, DSVAs, and kyphotic wedge angles. A p value of <0.05 was defined to be statistically significant. All statistical analyses were performed using the JMP Pro 12.0.1 software (SAS Institute Incorporation North Carolina, and America).
Results
Background data of the patients
The fracture levels were T10 in no patient, T11 in eight (OVC, three; non-OVC, five), T12 in 17 (OVC, four; non-OVC, 13), L1 in eight (OVC, two; non-OVC, six), L2 in eight (OVC, three; non-OVC, five), and L3 in five (OVC, none; non-OVC, five). The other background data are given in Table 1. Although there were no statistical differences, age was higher and the percentages of YAM bone mineral density of the lumbar vertebra and femoral neck were lower in the OVC group than in the non-OVC group. In the OVC group, there were no males, whereas in the non-OVC group, 29.4% of the patients were males.
Table 1.
Demographics of the Osteoporotic Vertebral Compression Fracture Patients.
| data | Total | OVC | Non-OVC | P-value |
|---|---|---|---|---|
| Age | 79.9±6.6 | 81.3±6.5 | 79.4±6.7 | 0.132 |
| Sex (female : male) | 36 : 10 | 12 : 0 | 24 : 10 | |
| Percentage of young adult mean | ||||
| Lumbar vertebra (%) | 66.2±11.5 | 61.9±10.6 | 67.6±11.7 | 0.076 |
| Femoral neck (%) | 69.1±12.7 | 67.6±12.6 | 69.6±13 | 0.828 |
| Fracture level | ||||
| T11 | 8 | 3 | 5 | |
| T12 | 17 | 4 | 13 | |
| L1 | 8 | 2 | 6 | |
| L2 | 8 | 3 | 5 | |
| L3 | 5 | 0 | 5 |
OVC indicates osteoporotic vertebral collapse. Comparisons between the two groups were performed using Wilcoxon test. A p-value less than 0.05 indicates statistical significance.
Radiographic assessment
The mean values for each parameter were as follows: PI, 58.0 degrees (OVC, 59.1 degrees; non-OVC, 57.6 degrees), SVA, 3.0 cm (OVC, 4.5 cm; non-OVC, 2.5 cm), DSVA, 5.7 cm (OVC, 8.3 cm; non-OVC, 4.7 cm), and kyphotic wedge angle of the fractured vertebra, 14.6 degrees (OVC, 17.7 degrees; non-OVC, 13.6 degrees) (Table 2). DSVA was significantly larger in the OVC group than in the non-OVC group. Although there were no statistical differences, SVA and kyphotic wedge angle were larger in the OVC group than in the non-OVC group; PIs in the both groups were similar.
Table 2.
Radiographic Parameters.
| Parameter | total | OVC | Non-OVC | P-value |
|---|---|---|---|---|
| PI (degrees) | 58±12.4 | 59.1±10.3 | 57.6±13.3 | 0.734 |
| SVA (cm) | 3±4.8 | 4.5±4.8 | 2.5±4.7 | 0.214 |
| DSVA (cm) | 5.7±4 | 8.3±4.9 | 4.7±3.2 | 0.006* |
| Kyphotic wedge angle (degrees) | 14.6±6.6 | 17.7±9.3 | 13.6±5 | 0.062 |
Each abbreviation indicates as follows, DSVA: distance of C7 plumb line to the center of fractured vertebra, PI: pelvic incidence, SVA: C7 plumb line to the posterior corner of the sacrum. All the parameters were compared using unpaired t-test. A p-value less than 0.05 indicates statistical significance (*).
Of 46 patients, OVC occurred in 12 (26.1%). Although no patient underwent surgery in the non-OVC group, two of 12 patients underwent surgery (both anterior spinal reconstruction) in the OVC group. In the OVC group, one patient showed a neurological deficit.
Multiple logistic regression analysis revealed that DSVA was a significant risk factor of OVC (p = 0.012; odds ratio, 1.025). When DSVA is 3 or 5 cm larger, the risk of OVC is 2.1 or 3.4 times more, respectively. PIs (p = 0.728), SVAs (p = 0.214), and kyphotic wedge angles of the fractured vertebra (p = 0.07) did not affect the occurrence of OVC (Table 3).
Table 3.
Multiple Logistic Regression Analysis to Identify Radiographic Risk Factor of Osteoporotic Vertebral Collapse.
| parameter | P-value | Odds ratio |
|---|---|---|
| PI (degrees) | 0.728 | 1.01 |
| SVA (mm) | 0.214 | 1.009 |
| DSVA (mm) | 0.012* | 1.025 |
| Kyphotic wedge angle (degrees) | 0.070 | 1.101 |
Each abbreviation indicates as follows, DSVA: distance of C7 plumb line to the center of fractured vertebra, PI: pelvic incidence, SVA: C7 plumb line to the posterior corner of the sacrum. A p-value less than 0.05 indicates statistical significance (*).
Discussion
The majority of patients with OVF are successfully treated by a nonoperative management using braces and physical therapy4). However, in patients with a vertebral collapse or pseudoarthrosis, pain is prolonged and their physical state is impaired5,6). As Tsujio et al.5) reported, intractable pain because of pseudoarthrosis and after a collapse markedly impair the activities of daily living of patients.
According to previous studies, the risk factors of osteonecrosis are thoracolumbar vertebra fractures5,7), aging7), middle column injuries5,8), and confined high-intensity or diffuse low-intensity areas of the fractured vertebra on T2-weighted MR images5).
Tsujio et al.5) conducted a prospective multicenter clinical study (350 patients with OVF from 25 institutes were enrolled) and revealed that the significant risk factors of vertebral pseudoarthrosis were thoracolumbar level of fractures, presence of middle column injuries, and confined high-intensity or diffuse low-intensity areas of the fractured vertebra on T2-weighted MR images. Mirovsky7) also reported that elderly patients with deformed thoracolumbar fractures were at a high risk of developing vertebral clefts, particularly when the adjacent disc was degenerated.
Furthermore, in their cadaver study (the load-carrying capacities of 10 human cadaver spines were evaluated), Haher et al.8) showed that a risk factor of collapse could be middle column injuries, which have the greatest impact on the loss of load-carrying capacity of the spine.
Spino-pelvic parameters were reported to be correlated to back pain. Diebo et al.9) performed a retrospective review of 143 patients with degenerative lumbar scoliosis, progressive idiopathic scoliosis, or kyphoscoliosis who underwent full-body radiographs and completed health-related quality of life questionnaires. Correlation analysis revealed that SVA had a coefficient of 0.399 with a visual analog scale for scoring back pain, implying that SVA had a good correlation with back pain. Moreover, Weng et al.10) prospectively assessed the influence of global spine and spino-pelvic-leg alignments on low back pain in 69 patients with hip osteoarthritis and found that total hip arthroplasty reduced the fixed flexion of the hip joints, thereby improving global spinal imbalance and reducing low back pain at 1 year after surgery.
This study revealed that DSVA was a risk factor of OVC after OVF. Interestingly, in case of OVC secondary to OVF, SVA was not a significant risk factor. Moment of rotation possibly occurs to the fractured vertebra. The magnitude of moment can be obtained by multiplying the body weight of the cranial trunk relative to the fractured vertebra with the distance between gravity center of trunk cranial to the fractured vertebra and the fractured vertebra. SVA does not represent the distance, but DSVA can be an approximate value of it. Hence, a large DSVA can be an explanation of a high stress concentration in the fractured vertebra. In addition, DSVA and the other radiographic parameters were measured using a standing whole-spine radiograph before initiating the nonoperative treatment. Accordingly, our finding is applicable to the global spinal alignment 2-3 days after injury rather than to the pre-traumatic global spinal alignment. This indicates that the standing posture of a patient with pain owing to a vertebral fracture influences the outcome of OVF, i.e., how a patient copes with pain and stands determines the occurrence of OVC.
Several biomechanical studies have assessed the relevance of stress concentration and fracture nonunion11-13). As Roberts et al.11) reported, sustained excess motion at a fracture site prevents bone healing. Regarding the mechanism of nonunion, in the mathematical study by Geris et al.12), overload-induced nonunion formation could predict by both angiogenesis and osteogenesis. The study by Carlier et al.,13) who used computational models, provided a further understanding regarding pathogenesis; although effective angiogenic factors are present in the fracture callus, an adverse mechanical environment prevents new vasculature formation. DSVA and not SVA had a significant influence on bone healing was consistent with the result of the aforementioned biomechanical study.
This study has some limitations that should be addressed. First, this study was a retrospective one, which is relatively weak compared with a prospective study. Thus, a future prospective study is necessary for validation. However, our study assessed whether a radiographic parameter would be a risk factor of radiographic outcomes. Because of this protocol, the difference between retrospective and prospective studies may be small. Second, there was a variation in medication for osteoporosis. Patients who were administered teriparatide were excluded. The osteogenic effect of teriparatide may greatly affect the outcome of OVF. Hence, further investigations with the inclusion of patients administered teriparatide may provide important data regarding the outcome of patients with OVF. Third, this study only focused on radiographic parameters and the outcome of OVC. This study was based on previous studies5,6) that reported that the prognosis of OVC worsened with prolonged pain or subsequent neurological impairment. However, confirming the clinical impact of OVC using a pain numeric rating scale, Oswestry Disability Index, and the Short Form Health Survey questionnaire may also be an aim of future studies. Nonetheless, this study provided a novel parameter for predicting the hazardous outcome of patients with OVF, and the current results will help in treating patients with OVF using a better strategy.
In this study, DSVA was the risk factor of OVC after OVF. The study results may be useful for orthopedic surgeons to predict the outcome of patients with OVF and to plan a strategy for OVF treatment.
Conflicts of Interest: The authors declare that there are no conflicts of interest concerning the materials or methods used in this study or the findings specified in this paper. Takashi Ohnishi and Akira Iwata have multiple affiliations. Masahiro Kanayama has relevant financial activities outside the submitted work.
References
- 1.Gold DT. The clinical impact of vertebral fractures: quality of life in women with osteoporosis. Bone. 1996;18(3):185S-9S. [DOI] [PubMed] [Google Scholar]
- 2.Crans GG, Silverman SL, Genant HK, et al. Association of severe vertebral fractures with reduced quality of life: reduction in the incidence of severe vertebral fractures by teriparatide. Arthritis Rheum. 2004;50(12):4028-34. [DOI] [PubMed] [Google Scholar]
- 3.Lyles KW, Gold DT, Shipp KM, et al. Association of osteoporotic vertebral compression fractures with impaired functional status. Am J Med. 1993;94(6):595-601. [DOI] [PubMed] [Google Scholar]
- 4.Magdalena R. The efficacy of conservative treatment of osteoporotic compression fractures on acute pain relief: a systematic review with meta-analysis. Eur Spine J. 2015;24(4):702-14. [DOI] [PubMed] [Google Scholar]
- 5.Tsujio T, Nakamura H, Terai H, et al. Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: a prospective multicenter study. Spine. 2011;36(15):1229-35. [DOI] [PubMed] [Google Scholar]
- 6.Picazo DR, Villaescusa JR, Martinez EP, et al. Late collapse osteoporotic vertebral fracture in an elderly patient with neurological compromise. Eur Spine J. 2014;23(12):2696-702. [DOI] [PubMed] [Google Scholar]
- 7.Mirovsky Y, Anekstein Y, Shalmon E, et al. Vacuum clefts of the vertebral bodies. AJNR. AJNR Am J Neuroradiol. 2005;26(7):1634-40. [PMC free article] [PubMed] [Google Scholar]
- 8.Haher TR, Tozzi JM, Lospinuso MF, et al. The contribution of the three columns of the spine to spinal stability: a biomechanical model. Paraplegia. 1989;27(6):432-9. [DOI] [PubMed] [Google Scholar]
- 9.Diebo BG, Oren JH, Challier V, et al. Global sagittal axis: a step toward full-body assessment of sagittal plane deformity in the human body. Journal of neurosurgery. Spine. 2016;25(4):494-9. [DOI] [PubMed] [Google Scholar]
- 10.Weng W, Wu H, Wu M, et al. The effect of total hip arthroplasty on sagittal spinal-pelvic-leg alignment and low back pain in patients with severe hip osteoarthritis. Eur Spine J. 2016;25(11):3608-14. [DOI] [PubMed] [Google Scholar]
- 11.Roberts TT, Rosenbaum AJ. Bone grafts, bone substitutes and orthobiologics: the bridge between basic science and clinical advancements in fracture healing. Organogenesis. 2012;8(4):114-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geris L, Sloten JV, Van Oosterwyck H. Connecting biology and mechanics in fracture healing: an integrated mathematical modeling framework for the study of nonunions. Biomech Model Mechanobiol. 2010;9(6):713-24. [DOI] [PubMed] [Google Scholar]
- 13.Carlier A, Lammens J, Van Oosterwyck H, et al. Computational modeling of bone fracture non-unions: four clinically relevant case studies. In Silico Cell Tissue Sci. 2015;2(1):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]


