Abstract
Introduction
Corrective surgery for adult degenerative scoliosis using lateral interbody fusion (LIF) and additional posterior fixation is an efficient procedure. However, it is unclear how this procedure affects rotational deformity correction. Therefore, the goal of the present study was to use three-dimensional (3D) images, taken during surgery, to investigate rotational deformity correction in the treatment of adult degenerative scoliosis using LIF and posterior fixation using a pedicle screw system.
Methods
The subjects were 12 females who were treated using LIF and posterior fixation for adult degenerative scoliosis. The patients had a mean age of 72 (65-76) years. 3D images were acquired before surgery, after LIF, and after additional posterior fixation. Rotational angles of the upper vertebra with respect to the lower vertebra of each fixed segment were measured in 3 planes. Correction factors for rotational deformity were investigated after LIF and additional posterior fixation.
Results
There were significant improvements in radiographical parameters for global spinal balance. The correction angles per segment were 4.7° for lateral bending, 6.9° for lordosis, and 4.5° for axial rotation. LIF was responsible for correction of four-fifths of lateral bending and axial rotation, and two-thirds of lordotic changes.
Conclusions
Lateral bending, axial rotational deformities, and lordosis were primarily corrected by LIF. Further lordosis correction was achieved using additional posterior fixation. These results indicate that corrective surgery for adult degenerative scoliosis using these procedures is effective for rotational deformity correction and leads to an ideal global spinal alignment.
Keywords: adult degenerative scoliosis, three-dimensional image analysis, lateral interbody fusion
Introduction
Adult degenerative scoliosis can be categorized into 3 major groups: type I, primary degenerative lumbar scoliosis (de novo scoliosis); type II, progressive idiopathic scoliosis; and type III, secondary degenerative scoliosis (because of neuromuscular origin, leg length discrepancy, hip pathology, or osteoporotic fracture)1). Degenerative scoliosis is diagnosed in adults with a Cobb angle >10° in the frontal plane due to slippage and rotational deformity of vertebral bodies associated with disc degeneration and facet joint arthritis, and it leads to back pain, neurological deficits, and global spinal imbalance as the main consequences of adult spinal deformity. In radiological evaluation, rotational deformities in the frontal plane can be assessed as scoliosis, typified by a large Cobb angle, and rotational deformities in the sagittal plane are evaluated as kyphosis; however, it is difficult to quantitatively evaluate rotational deformities in the axial plane using a radiograph. These deformities can be evaluated using CT axial images or the EOS® 2D/3D X-ray imaging system2-6).
The utility of three-dimensional (3D) image analysis for adolescent idiopathic scoliosis has been recently reported2,5,6). Lateral interbody fusion (LIF) such as extreme lateral interbody fusion (XLIF®) and oblique lateral interbody fusion (OLIF™) with additional posterior fixation using a percutaneous pedicle screw (PPS) system is an effective and minimally-invasive surgical procedure for treating lumbar spinal deformities caused by multiple intervertebral lesions, compared with interbody fusion via a posterior approach, such as posterior lumbar interbody fusion and transforaminal posterior lumbar interbody fusion7-9). LIF for adult degenerative scoliosis with lumbar spinal canal/foraminal stenosis is likely to result in satisfactory clinical outcome and fewer complications10-12). LIF is also useful for effective reduction and favorable alignment of lateral bending and kyphotic deformities using a large, lordotic cage through a low-invasive procedure and indirect decompression in the spinal canal and intervertebral foramen; however, it is unclear how the procedure affects rotational deformities in the axial plane. 3D analysis during surgery has become possible using O-arm® and ARCADIS Orbic 3D®, which are particularly advantageous for evaluation of rotational deformity correction in the axial plane. The purpose of the current study was to quantify correction of rotational deformity in adult degenerative scoliosis treated by LIF and additional posterior fixation, using 3D images during surgery.
Subjects and Methods
All assessments were performed after the study was approved by our institution's ethics committee, and informed consent was obtained from all subjects. The subjects were 12 females (age 65-76 years; mean age, 72 years) with primary adult degenerative scoliosis (type I) that was treated by LIF (XLIF®) and additional posterior fixation. The diagnosis of primary adult degenerative scoliosis was based on lateral bending and axial rotational deformities limited to the lumbar spine, without basic disease as a cause of secondary scoliosis. We performed LIF for lumbar vertebral disc lesions from L1 to L5 and TLIF for the L5-S1 vertebral discs, followed by posterior fixation for the lower thoracic spine, lumbar spine and sacrum as needed, using a pedicle screw system. For LIF, the cage size was selected and the cage position determined using the original XLIF® method. Facet release and bone osteotomy were not performed for lumbar vertebral lesions treated by LIF. However, facet release and grade 1 bone osteotomy were used for the inferior articular process in lower thoracic and lumbar vertebral lesions not treated by LIF and for L5-S1 within the range of posterior fixation13). In situ contouring was performed by inserting a straight rod in the frontal plane with a bend along the target alignment in the sagittal plane into extension sleeves of a pedicle screw system without a special correction maneuver in posterior fixation. The intervertebral region treated with LIF was L1/2 in 5 cases, L2/3 in 10 cases, L3/4 in 11 cases, and L4/5 in 8 cases. The upper instrumented vertebra was the lower thoracic spine in 8 cases and the lumbar spine in 4 cases, and the lower instrumented vertebra was the lumbar spine in 2 cases and the sacrum in 10 cases, with or without an iliac screw. The average follow-up period was 555 (426-716) days after surgery. Data at final follow-up were obtained for each patient for the duration of 1-2 years after surgery.
Clinical outcomes
Clinical outcomes were evaluated using the Japanese Orthopaedic Association (JOA) score, the Japanese Orthopedic Association Back Pain Evaluation Questionnaire (JOABPEQ: including pain-related disorders, lumbar spine dysfunction, gait disturbance, social life dysfunction, and psychological disorders)14), and visual analog scales (VAS) for low back pain (LBP-VAS), gluteal and lower limb pain (BLP-VAS), and gluteal and lower limb numbness (BLN-VAS). Assessments before surgery and at final follow-up were used for analysis.
Radiographical evaluation
Cobb angle, C7 plumb line-central sacral vertical line (C7PL-CSVL), sagittal vertical axis (SVA), T5-12 thoracic kyphosis (TK), L1-S1 lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI), and PI-LL were measured on radiographs taken in the standing position before surgery and at final follow-up15,16). Information on cage size in LIF was gathered, and cage position measured using the area ratio in the front-to-back direction for each intervertebral lesion, using axial CT planes at the center of the height of the vertebral lesion.
Three-dimensional image analysis
3D images of the intervertebral region treated by LIF were taken before surgery in the lateral position, after LIF in the lateral position, and after additional posterior fixation in the prone position using ARCADIS Orbic 3D (Fig. 1). The rotational angle of the upper vertebra relative to the lower vertebra of each fixed segment was measured in 3 planes using OsiriX®, and lateral bending in the frontal plane, lordosis/kyphosis in the sagittal plane, and axial rotation in the axial plane were evaluated for each segment (Fig. 2). Correction factors for rotational deformity were investigated after LIF and after additional posterior fixation.
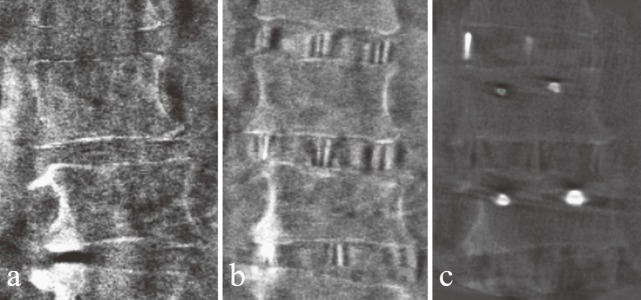
Figure 1.
Three-dimensional images: (a) before surgery, (b) after LIF with a myelogram, and (c) after PPS fixation. Images were taken using ARCADIS Orbic 3D®.
Figure 2.
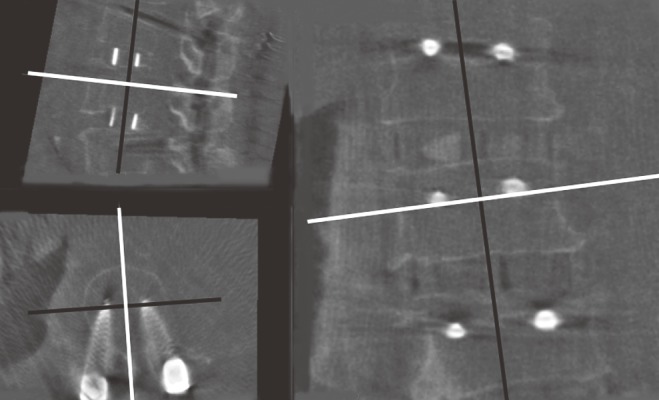
Rotational angles of lateral bending in the coronal plane, lordosis in the sagittal plane, and axial rotation in the axial plane were measured at the middle of the height of the pedicle parallel to the endplate and spinous process, using OsiriX® for each segment.
Statistical analysis
Two independent observers performed imaging classification twice, and validity was assessed using intraobserver and interobserver differences. Differences in clinical outcomes and radiographical parameters before surgery and at final follow-up were examined using the Wilcoxon signed rank test (α = 0.05). Differences in local angle changes of each segment in lateral bending, lordosis/kyphosis, and axial rotation before surgery, after LIF, and after posterior fixation were examined using the Friedman test (α = 0.05). Sample size and power were evaluated using power analysis. All calculations were performed using SPSS ver. 23.0 (IBM).
Results
Clinical outcomes
The average JOA score (out of a total of 29 points) significantly increased from 13.3 before surgery to 22.1 at final follow-up (Table 1; P = 0.002). Changes in the components of the JOABPEQ are shown in Table 1. A significant increase in pain-related disorders was observed (P = 0.025). The LBP-VAS score also decreased significantly (P = 0.041). No severe complications occurred during surgery or follow-up period. Minor complications such as temporary thigh pain and screw loosening occurred in 2 cases (sacrum screw, iliac screw), and treatable subcutaneous infection and deep vein thrombosis occurred in 1 case. In the period from one to 2 years after surgery, one patient required an additional surgical procedure for the removal of a loosened iliac screw.
Table 1.
Clinical Outcomes.
| Before surgery | Final follow-up | P value | |
|---|---|---|---|
| JOA scores | 13.3±4.4 | 22.1±4.0 | 0.002* |
| JOABPEQ | |||
| Pain-related disorders | 35.8±21.4 | 63.0±34.7 | 0.025* |
| Lumbar spine dysfunction | 49.3±32.4 | 43.0±30.1 | 0.474 |
| Gait disturbance | 25.8±19.7 | 34.6±26.5 | 0.118 |
| Social life dysfunction | 40.1±24.5 | 46.3±19.4 | 0.329 |
| Psychological disorders | 38.5±12.0 | 44.7±14.7 | 0.194 |
| VAS | |||
| LBP-VAS | 7.1±2.2 | 4.7±2.2 | 0.041* |
| BLP-VAS | 5.7±3.7 | 4.2±1.6 | 0.346 |
| BLN-VAS | 5.1±3.6 | 4.6±2.4 | 0.480 |
Clinical outcome was evaluated using the Japanese Orthopaedic Association (JOA) score, the Japanese Orthopedic Association Back Pain Evaluation Questionnaire (JOABPEQ), and visual analog scales (VAS) for low back pain (LBP-VAS), gluteal and lower limb pain (BLP-VAS), and gluteal and lower limb numbness (BLN-VAS)
Data are shown as mean±SD
*Significant difference in Wilcoxon signed rank test.
Radiographical evaluation
Significant differences in radiographical parameters from before surgery to final follow-up were observed for the Cobb angle, C7PL-CSVL, SVA, TK, LL, PT, and PI-LL (Table 2, Fig. 3). The height and length of the cage in LIF averaged 8.8 mm (L1/2: 8.6 mm, L2/3: 9.1 mm, L3/4: 8.6 mm, and L4/5: 8.6 mm) and 48.7 mm (L1/2: 45.0 mm, L2/3: 48.0 mm, L3/4: 49.1 mm, and L4/5: 51.3 mm), respectively. The widths and lordotic angles of all cages were 18 mm and 10°, respectively. The position of the cage averaged 64.6% (L1/2: 84.7%, L2/3: 55.6%, L3/4 55.0%, and L4/5: 86.0%) anterior from the midline in the front-to-back direction. The average intraobserver and interobserver differences were 1.2 mm and 0.9°, and 1.4 mm and 1.1°, respectively.
Table 2.
Radiographical Parameters.
| Parameter | Before surgery | Final follow-up | P value |
|---|---|---|---|
| Cobb angle (°) | 30.0±12.2 | 9.8±4.5 | 0.002* |
| C7PL-CSVL (mm) | 36.3±35.3 | 13.6±8.8 | 0.019* |
| SVA (cm) | 12.3±4.7 | 4.3±3.8 | 0.002* |
| TK (°) | 15.7±10.4 | 25.0±17.4 | 0.029* |
| LL (°) | 8.1±27.0 | 39.8±15.8 | 0.003* |
| PT (°) | 36.0±21.0 | 17.6±12.0 | 0.010* |
| PI (°) | 55.2±20.9 | 51.1±11.1 | 0.445 |
| PI-LL (°) | 47.0±30.0 | 11.3±14.8 | 0.004* |
Cobb angle, C7 plumb line-central sacral vertical line (C7PL-CSVL), sagittal vertical axis (SVA), T5-12 thoracic kyphosis (TK), L1-S1 lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI) and PI-LL were measured on a radiograph taken in the standing position
Data are shown as mean±SD
*Significant difference in Wilcoxon signed rank test.
Figure 3.
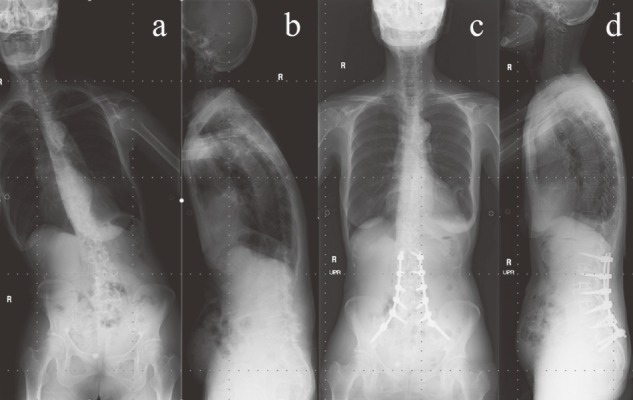
A 76-year-old female treated by LIF at L2-3, L3-4, and L4-5, followed by L2-S1 posterior fusion with an iliac screw. (a, b) Before surgery; Cobb angle: 26°, C7PL-CSVL: 135 mm, SVA: 15.5 cm, TK: 21°, LL: 18°, PT 29°, PI: 51°, PI-LL: 33°. (c, d) At final follow-up; Cobb angle: 2°, C7PL-CSVL: 0 mm, SVA: 8.7 cm, TK: 33°, LL: 44°, PT 23°, PI: 59°, PI-LL: 15°.
Three-dimensional image analysis
The total number of intervertebral regions treated by LIF was 34. The average rotational angles from before surgery to after LIF and after additional posterior fixation changed from 7.0° to 3.2° to 2.3° for lateral bending (Table 3; P < 0.001), from 4.6° to 9.3° to 11.5° for lordosis (P < 0.001), and from 6.0° to 2.3° to 1.5° for axial rotation (P < 0.001). The correction angles per segment were 4.7° in lateral bending and 4.5° in axial rotation, and the LIF:posterior fixation correction ratio was 4:1. The correction angle per segment was 6.9° for lordosis and the LIF:posterior fixation correction ratio was 2:1.
Table 3.
Three-dimensional Rotational Angles Per Segment.
| Parameter | Before surgery | After LIF | After posterior fixation | P value |
|---|---|---|---|---|
| Lateral bending (°) | 7.0±6.9 | 3.2±3.2 | 2.3±2.4 | <0.001* |
| Correction (°) (%) | 3.8 (81%) | 0.9 (19%) | ||
| L1/2 (°) | 10.1±6.7 | 4.7±4.9 | 2.6±2.2 | |
| L2/3 (°) | 8.8±9.2 | 3.2±3.2 | 2.5±2.8 | |
| L3/4 (°) | 5.5±5.2 | 3.5±3.2 | 2.3±2.7 | |
| L4/5 (°) | 4.9±5.9 | 2.0±2.0 | 1.9±2.0 | |
| Lordosis (°) | 4.6±7.9 | 9.3±6.2 | 11.5±6.0 | <0.001* |
| Correction (°) (%) | 4.7 (68%) | 2.2 (32%) | ||
| L1/2 (°) | -0.9±10.2 | 5.4±7.5 | 8.6±5.7 | |
| L2/3 (°) | 5.5±5.2 | 7.9±4.9 | 8.8±4.7 | |
| L3/4 (°) | 4.6±8.5 | 10.7±6.3 | 12.1±5.1 | |
| L4/5 (°) | 7.0±8.3 | 11.4±6.2 | 15.9±6.7 | |
| Axial rotation (°) | 6.0±4.8 | 2.3±2.9 | 1.5±1.6 | <0.001* |
| Correction (°) (%) | 3.7 (82%) | 0.8 (18%) | ||
| L1/2 (°) | 8.6±7.4 | 3.4±5.3 | 1.7±1.9 | |
| L2/3 (°) | 5.4±3.8 | 1.8±2.0 | 1.3±1.5 | |
| L3/4 (°) | 6.1±5.0 | 1.8±2.0 | 1.6±1.6 | |
| L4/5 (°) | 5.2±4.1 | 2.9±3.2 | 1.3±1.7 |
Data are shown as mean±SD
*Significant difference among before surgery, after LIF and after additional posterior fixation (Friedman test).
Discussion
Decompression surgery, correction surgery, or combined surgery can be used for the treatment of adult degenerative scoliosis with lumbar spinal canal/foraminal stenosis that is unresponsive to conservative therapy. Selection of the surgical method is contingent upon the medical facility and surgeon, and correction surgery is recommended for patients with global spinal imbalance, progressive deformity, and foraminal stenosis with spinal instability1,12,17).
In the present study, we observed significant changes in global spinal alignment in adult degenerative scoliosis treated with LIF and additional posterior fixation. Clinical outcomes after short-term follow-up revealed increased JOA scores and pain-related disorders in JOABPEQ, and a decrease in LBP-VAS, with resultant improvement in activities of daily living (ADL). Therefore, corrective surgery for adult degenerative scoliosis with an average Cobb angle of 30° was achieved by correction of global spinal alignment and improvement of ADL associated with pain relief. However, long-term follow-up is required because improvement of subjective symptoms by correction surgery may be associated with other factors, such as preoperative severity, diagnosis, and muscle strength.
Ideal LL with correction of lateral bending deformity was achieved using a large lordotic cage via the lateral approach in LIF, with 4.7° correction of lateral bending and 6.9° of lordosis obtained per segment. The position of the cage at L1/2 and L4/5 was more anterior from the midline in the front-to-back direction, compared with that at L2/3 and L3/4. The cage placement could have been affected by anatomical features such as the ribs and iliac and lumbar plexuses. Also, there were characteristic differences in correction at different vertebral levels, with larger correction of lateral bending deformity at upper vertebral levels, and a larger lordotic angle at lower vertebral levels. These data are useful for preoperative planning of correction surgery including global spinal balance. Our results, showing an average correction of 4.5° in axial rotation, suggest that this procedure can also correct axial rotational deformity in adult degenerative scoliosis. The axial rotational angle is smaller near the apical region and larger near the junctional region in adolescent idiopathic scoliosis. Effective correction of axial rotation was obtained at all vertebral levels, regardless of differences in cage positions. Using LIF, correction in the axial plane could be obtained by the effect of ligamentotaxis by increasing the disc height with lateral release of the annulus fibrous of the disc and stretching of the ligaments18). Further studies are required for assessment of factors that affect correction in the axial plane.
The results for local segmental correction indicated that LIF has advantages in correction of rotational deformities in all 3 planes. Our evaluation of rotational deformity correction using 3D images for quantitative evaluation in stages after LIF and after additional posterior fixation showed that LIF produced 80% of lateral bending and axial rotational correction and about 67% of lordotic changes out of the total effects of LIF and posterior fixation. That is, most correction was because of LIF, with an additional effect on lordosis by posterior fixation. In this series, we used in situ contouring without special correction techniques for posterior fixation. Steib et al. reported that a reliable detorsion in the axial plane was obtained by in situ contouring in surgical correction of scoliosis19). It was suspected that a straight rod in the frontal plane with bending along the target alignment in the sagittal plane worked for correction in the axial plane, despite motion of the polyaxial screw head. This suggests that posterior fixation using a pedicle screw system provides mechanical stabilization and an additional correction effect.
This study has some limitations, including the cost and radiation exposure associated with the use of ARCARDIS Orbic 3D® and the limited number of subjects. Sample size and power were appropriate in the power analysis, but the subjects had some inherent variability. Differences between the lateral and prone positions might have also affected the results. Therefore, large-scale prospective and long-term studies are necessary to verify these results. Considering these limitations, we conclude that the effect of rotational deformity correction in adult degenerative scoliosis treated with LIF and additional posterior fixation can be quantified using 3D image analysis during surgery. Lateral bending and axial rotational deformities were primarily corrected by LIF, whereas lordosis was improved by additional posterior fixation. Thus, corrective surgery for adult degenerative scoliosis using this approach is effective for rotational deformity correction in 3 planes and obtaining an ideal global spinal alignment.
Conflicts of Interest: The authors declare that there are no conflicts of interest.
Sources of funding: Funding was from JSPS KAKENHI; Grant Number 16K01439.
References
- 1.Aebi M. The adult scoliosis. Eur Spine J. 2005;14(10):925-48. [DOI] [PubMed] [Google Scholar]
- 2.Hattori T, Sakaura H, Iwasaki M, et al. In vivo three-dimensional segmental analysis of adolescent idiopathic scoliosis. Eur Spine J. 2011;20(10):1745-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pasha S, Cahill PJ, Dormans JP, et al. Characterizing the differences between the 2D and 3D measurements of spine in adolescent idiopathic scoliosis. Eur Spine J. 2016;25(10):3137-45. [DOI] [PubMed] [Google Scholar]
- 4.Somoskeoy S, Tunyogi-Csapo M, Bogyo C, et al. Accuracy and reliability of coronal and sagittal spinal curvature data based on patient-specific three-dimensional models created by the EOS 2D/3D imaging system. Spine J. 2012;12(11):1052-9. [DOI] [PubMed] [Google Scholar]
- 5.Thong W, Parent S, Wu J, et al. Three-dimensional morphology study of surgical adolescent idiopathic scoliosis patient from encoded geometric models. Eur Spine J. 2016;25(10):3104-13. [DOI] [PubMed] [Google Scholar]
- 6.Schlosser TP, van Stralen M, Brink RC, et al. Three-dimensional characterization of torsion and asymmetry of the intervertebral discs versus vertebral bodies in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2014;39(19):E1159-66. [DOI] [PubMed] [Google Scholar]
- 7.Ozgur BM, Aryan HE, Pimenta L, et al. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006;6(4):435-43. [DOI] [PubMed] [Google Scholar]
- 8.Ohtori S, Orita S, Yamauchi K, et al. Mini-Open Anterior Retroperitoneal Lumbar Interbody Fusion: Oblique Lateral Interbody Fusion for Lumbar Spinal Degeneration Disease. Yonsei Med J. 2015;56(4):1051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Narita W, Takatori R, Arai Y, et al. Prevention of neurological complications using a neural monitoring system with a finger electrode in the extreme lateral interbody fusion approach. J Neurosurg Spine. 2016;25(4):456-63. [DOI] [PubMed] [Google Scholar]
- 10.Berjano P, Lamartina C. Far lateral approaches (XLIF) in adult scoliosis. Eur Spine J. 2013;22 Suppl 2:S242-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phillips FM, Isaacs RE, Rodgers WB, et al. Adult degenerative scoliosis treated with XLIF: clinical and radiographical results of a prospective multicenter study with 24-month follow-up. Spine (Phila Pa 1976). 2013;38(21):1853-61. [DOI] [PubMed] [Google Scholar]
- 12.Alimi M, Hofstetter CP, Tsiouris AJ, et al. Extreme lateral interbody fusion for unilateral symptomatic vertical foraminal stenosis. Eur Spine J. 2015;24 Suppl 3:346-52. [DOI] [PubMed] [Google Scholar]
- 13.Schwab F, Blondel B, Chay E, et al. The comprehensive anatomical spinal osteotomy classification. Neurosurgery. 2015;76 Suppl 1:S33-41;discussion S. eng. [DOI] [PubMed] [Google Scholar]
- 14.Fukui M, Chiba K, Kawakami M, et al. JOA Back Pain Evaluation Questionnaire (JOABPEQ)/JOA Cervical Myelopathy Evaluation Questionnaire (JOACMEQ). The report on the development of revised versions. April 16, 2007. The Subcommittee of the Clinical Outcome Committee of the Japanese Orthopaedic Association on Low Back Pain and Cervical Myelopathy Evaluation. J Orthop Sci. 2009;14(3):348-65. [DOI] [PubMed] [Google Scholar]
- 15.Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976). 2012;37(12):1077-82. [DOI] [PubMed] [Google Scholar]
- 16.Ames CP, Smith JS, Scheer JK, et al. Impact of spinopelvic alignment on decision making in deformity surgery in adults: A review. J Neurosurg Spine. 2012;16(6):547-64. [DOI] [PubMed] [Google Scholar]
- 17.Wang G, Hu J, Liu X, et al. Surgical treatments for degenerative lumbar scoliosis: a meta analysis. Eur Spine J. 2015;24(8):1792-9. [DOI] [PubMed] [Google Scholar]
- 18.Elowitz EH, Yanni DS, Chwajol M, et al. Evaluation of indirect decompression of the lumbar spinal canal following minimally invasive lateral transpsoas interbody fusion: radiographic and outcome analysis. Minimally invasive neurosurgery: MIN. 2011;54(5-6):201-6. eng. [DOI] [PubMed] [Google Scholar]
- 19.Steib JP, Dumas R, Mitton D, et al. Surgical correction of scoliosis by in situ contouring: a detorsion analysis. Spine (Phila Pa 1976). 2004;29(2):193-9. [DOI] [PubMed] [Google Scholar]