Abstract
Introduction
The purpose of this study was to investigate the long-term incidence of lumbar disc degeneration and Modic changes in the non-fused segments of patients with adolescent idiopathic scoliosis (AIS) who previously underwent spinal fusion.
Methods
Study subjects consisted of 252 patients with AIS who underwent spinal fusion between 1968 and 1988. Of 252 patients, 35 subjects underwent lumbar spine MRI and whole spine X-ray examination. The mean patient age at the time of follow-up was 49.8 years, with an average follow-up period of 35.1 years. We classified the subjects into two groups based on the lowest fused vertebra: H group whose lowest fused vertebra was L3 or higher levels and L group whose lowest fused vertebra was L4 or lower levels.
Results
The L group had significantly advanced disc degeneration on MRI. There was no significant difference between two groups in Modic changes. The L group showed less lumbar lordosis than the H group (H group: 48.1 degrees; and L group: 32.1 degrees) and greater SVA (H group: 1.2 cm; and L group: 5.5 cm).
Conclusions
In AIS patients, 35 years after spinal fusion surgery on average, we evaluated lumbar disc degeneration and Modic changes of the non-fused segments. In patients with the lowest fusion level at L4 or lower, there were reduced lumbar lordosis, considerable SVA imbalance, and severe disc degeneration compared with those with the lowest fusion level at L3 or higher. The lowest fusion level at L3 or higher is recommended to reduce disc degeneration in midlife.
Keywords: adolescent idiopathic scoliosis, spinal fusion, long-term follow-up, lumbar disc degeneration, Modic change
Introduction
Spinal fusion is often reported to have a good course for adolescent idiopathic scoliosis (AIS)1-5). However, there are few reports on post-operative long-term changes at the adjacent levels of fusion when the patients reached their forties or fifties3). There are concerns that those who underwent spinal fusion in adolescence may develop high incidence of lumbar disc degeneration associated with low back pain in middle age.
Cochran et al. have reported that low back pain is more likely to occur in AIS patients in whom fusion was extended down to L4 or L56). Danielsson et al. examined MRIs of AIS patients fused to L4 or L5, and reported high incidence of disc degeneration associated with low back pain 25 years after surgery3). Therefore, if the fusion levels are limited to L3 or higher preserving lower motion segments, we may expect less incidence of disc degeneration in the long-term period.
On the other hand, Schwab et al. have reported positive correlations between pain and L3 or L4 vertebral body tilt in adult scoliosis7). To prevent progression of adult scoliosis, which may cause pain, Toyone et al. recommended correcting L3 vertebral tilt to less than 5 degrees8). In other words, L3 or L4 tilt should be corrected as much to get better outcomes in terms of low back pain in middle age.
For long-term prognosis, the incidence of low back pain is believed to be relatively low for those with spinal fusion down to L3 or higher. On the other hand, to correct L3 or L4 tilt sufficiently, it is advantageous to fuse down to lower levels. Therefore, there is a conflict for fusion levels: whether to preserve motion segments by limiting the fusion levels down to L3, or to secure correction of vertebral tilt by extending the fusion level down to L4 or lower.
The purpose of this study is to investigate the long-term incidence of lumbar disc degeneration and Modic changes of non-fused segments in AIS patients who underwent spinal fusion in their adolescence. Especially, we investigated whether the lowest level of fusion affected lumbar disc degeneration and whether such disc degeneration was related to low back pain and health-related quality of life (HRQOL). We hypothesized those AIS patients who were previously operated on with spinal fusion down to L4 or lower could develop low back pain in midlife due to advanced Modic changes associated with intervertebral disc degeneration of non-fused segments.
Materials and Methods
The institutional review board approved the present study. Study subjects consisted of 252 patients with AIS who underwent spinal fusion at one institution between 1968 and 1988. All patients were younger than 20 years old at the time of surgery. The average age at the time of surgery was 14.8 years. The average Cobb angle was 68.3 degrees (range, 32-130 degrees) before surgery and 39.4 degrees (range, 6-90 degrees) two years after surgery. First, we tried to contact all the 252 patients by mail. The following patients were excluded: 134 patients with unknown address, 62 patients who failed to respond to the mails, 13 patients who refused examinations and 8 patients who died. Of 252 patients, 35 (30 women, 5 men) underwent lumbar MRI and whole spine X-ray examination. These 35 subjects were included in our analysis (follow-up rate of 13.9%). The mean age of the 35 subjects was 49.8 years (range, 40-64 years), with an average follow-up period of 35.1 years (range, 27-45 years). The surgical procedures used were posterior fixation in 30 patients and anterior fixation in 5. The lowest fusion levels were: T12 in 2; L1 in 4; L2 in 12; L3 in 9; L4 in 7; and L5 in 1. Preoperative X-ray or MRIs were not available in majority of the cases.
The MRI used was Signa HDxt 1.5 T (General Electric Company, Connecticut, USA). T1-weighted and T2-weighted sagittal images and cross-sections were obtained for the lumbar spine. MRI evaluations were performed by three independent observers (O.S., F.K., and S.Y.) who were blinded to the clinical data of the patients. Pfirrmann classification was used to evaluate disc degeneration of the non-fused segments9). This classification was performed by the three observers and the most voted values were selected as the gold standard. In the case that none of the observers coincide, the median value was selected. Modic changes were evaluated in terms of signal changes at the vertebral body endplate10,11). Modic change evaluation was also performed by the three observers and the most voted types were selected as the gold standard. In the case that none of the observers coincide, the type was decided by discussion.
X-rays of the whole spine were taken from the back and the side with the subject standing. In the frontal view, we measured thoracic and lumbar Cobb angle, coronal balance (the difference between the line vertical from C7 and the sacral center line), and L3 and L4 vertebral tilt angles. The vertebral body tilt was measured as the angle formed by its superior endplate and a true horizontal line. In the lateral view, we measured thoracic kyphosis (TK: T5-T12), thoracolumbar kyphosis (TLK: T10-L2), lumbar lordosis (LL: L1-S1), pelvic incidence (PI), pelvic tilt (PT), and sagittal vertical axis (SVA: the distance between the line vertical from C7 and the S1 posterior corner). The questionnaires used were the Scoliosis Research Society Patient Questionnaire (SRS-22), Roland-Morris Disability Questionnaire (RDQ), and Oswestry Disability Index (ODI).
For statistical analyses, SPSS Statistics version 22.0 (International Business Machines Corporation, NY, USA) was used. We classified the subjects into two groups based on the lowest fused vertebra: H group whose lowest fused vertebra was L3 or higher levels; and L group L4 or lower levels. Pfirrmann grades 4 or 5 were considered lumbar disc degeneration positive (DD(+)), while those with other scores were considered negative (DD(-)). Those with Modic changes were named Modic(+), and those without Modic(-). For comparisons between two groups, we used the Mann-Whitney U test or chi-square test. The level of significance was set at less than 5%.
Results
Patient data are shown in Table 1. There were Pfirrmann grade 1 in 1 segment, grade 2 in 28, grade 3 in 51, grade 4 in 32, and grade 5 in 8. Twenty-four patients (68.6%) had disc degeneration of Pfirrmann grade 4 or higher. Modic changes were found in 20 patients (57.1%): 15 had Modic change in one segment; 2 had Modic changes in 2 segments; 3 had Modic changes in 3 segments. There were Modic type 1 changes in 10 segments, Modic type 2 in 11, and Modic type 3 in 7. There was a case of central spinal stenosis on MRI, a case of foraminal stenosis at L5-S1, and a case of L5 spondylolytic spondylolisthesis, however, there was no disc herniation noted. Average SRS-22 scores were function: 4.3; pain: 4.5; self-image: 3.0; mental: 4.1; and satisfaction: 3.6. The average RDQ was 0.9, and the average ODI was 7.3.
Table 1.
Patient Data of the Study Group.
| Demographics | X-ray parameters in coronal plane | X-ray parameters in sagittal plane | MRI | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Group | Sex | Age at the fullow-up (years) | Follow-up period (years) | BMI (kg/cm2) | Curve type | Surgical method | LFV | Thoracic curve (°) | Lumbar curve (°) | Coronal balance (cm) | L3 tilt (°) | L4 tilt (°) | TK (°) | TLK (°) | LL (°) | PI (°) | PT (°) | SVA (cm) | DD+/- | Modic+/- | |||
| 1 | H | F | 55 | 41 | 18.3 | D | HI | T12 | 67 | 51 | 0.9 | 2 | 14 | 55 | 9 | 53 | 35 | 15 | -2.7 | + | + | |||
| 2 | H | F | 48 | 37 | 29.3 | T | HI | T12 | 44 | 19 | 1.3 | 5 | 3 | 4 | 0 | 39 | 37 | 7 | 0.0 | - | - | |||
| 3 | H | F | 58 | 43 | 21.8 | T | HI | L1 | 51 | 40 | 4.6 | 9 | 12 | 32 | 49 | 9 | 28 | 19 | 2.7 | + | + | |||
| 4 | H | F | 54 | 38 | 20.8 | T | HI | L1 | 62 | 30 | 0.1 | 27 | 17 | 22 | 6 | 41 | 53 | 28 | 3.3 | + | + | |||
| 5 | H | F | 47 | 32 | 23.3 | T | HI wiring | L1 | 40 | 30 | 1.1 | 2 | 5 | 26 | 18 | 35 | 43 | 29 | -2.7 | + | + | |||
| 6 | H | F | 42 | 27 | 19.7 | T | HI wiring | L1 | 42 | 15 | 2.8 | 4 | 0 | 35 | 2 | 52 | 31 | 5 | 0.0 | - | - | |||
| 7 | H | F | 56 | 43 | 23.1 | T | HI | L2 | 84 | 52 | 1.8 | 20 | 6 | 37 | 8 | 47 | 63 | 23 | 9.4 | + | + | |||
| 8 | H | F | 60 | 44 | 20.6 | T | HI | L2 | 65 | 52 | 3.3 | 6 | 12 | 27 | 11 | 45 | 44 | 13 | 4.8 | + | + | |||
| 9 | H | M | 54 | 39 | 14.0 | T | HI | L2 | 69 | 24 | 4.2 | 27 | 24 | 45 | 27 | 61 | 38 | 4 | 0.0 | - | + | |||
| 10 | H | F | 49 | 37 | 20.0 | T | HI | L2 | 53 | 18 | 1.2 | 17 | 17 | 33 | 16 | 53 | 47 | 20 | 4.8 | + | + | |||
| 11 | H | F | 51 | 34 | 34.8 | T | HI | L2 | 51 | 18 | 3.7 | 12 | 9 | 33 | 4 | 35 | 87 | 50 | 16.8 | + | - | |||
| 12 | H | M | 47 | 32 | 20.8 | T | HI wiring | L2 | 44 | 13 | 1.2 | 14 | 10 | 27 | 0 | 61 | 44 | 5 | 1.3 | - | - | |||
| 13 | H | F | 45 | 30 | 27.4 | T | HI wiring | L2 | 60 | 29 | 0.8 | 16 | 9 | 46 | 7 | 55 | 35 | 8 | 0.0 | - | - | |||
| 14 | H | F | 43 | 29 | 17.9 | T | HI wiring | L2 | 31 | 21 | 0.4 | 1 | 1 | 9 | 1 | 42 | 46 | 14 | -0.6 | - | - | |||
| 15 | H | F | 47 | 28 | 18.4 | T | HI wiring | L2 | 28 | 13 | 1.1 | 6 | 5 | 31 | 9 | 51 | 47 | 17 | 2.6 | + | - | |||
| 16 | H | M | 64 | 45 | 23.0 | T | HI | L2 | 55 | 22 | 0.5 | 8 | 6 | 26 | 7 | 42 | 44 | 15 | 2.7 | + | + | |||
| 17 | H | F | 48 | 34 | 19.9 | T | Luque | L2 | 26 | 19 | 0.4 | 0 | 6 | 18 | 10 | 42 | 41 | 15 | 0.2 | + | - | |||
| 18 | H | F | 45 | 32 | 19.5 | T | HI wiring | L2 | 28 | 14 | 0.9 | 1 | 1 | 10 | 2 | 71 | 53 | 5 | -4.7 | - | - | |||
| 19 | H | F | 54 | 42 | 17.3 | T | HI | L3 | 71 | 21 | 2.5 | 25 | 29 | 24 | 13 | 32 | 45 | 27 | 3.4 | - | - | |||
| 20 | H | F | 51 | 39 | 19.4 | T | HI | L3 | 74 | 38 | 0.6 | 8 | 6 | 61 | 20 | 66 | 42 | 10 | 0.2 | - | - | |||
| 21 | H | F | 45 | 31 | 20.6 | D | Luque | L3 | 55 | 33 | 3.3 | 2 | 4 | 21 | -2 | 75 | 47 | 4 | -5.5 | - | - | |||
| 22 | H | F | 43 | 31 | 25.1 | T | HI wiring | L3 | 38 | 19 | 0.7 | 8 | 2 | 33 | 7 | 68 | 69 | 29 | 1.2 | + | + | |||
| 23 | H | F | 40 | 29 | 18.0 | T | HI wiring | L3 | 40 | 16 | 0.0 | 8 | 4 | 20 | -5 | 62 | 36 | 3 | -4.3 | - | - | |||
| 24 | H | F | 45 | 33 | 21.0 | L | Zielke | L3 | 17 | 25 | 1.5 | 3 | 14 | 16 | 15 | 28 | 45 | 22 | 1.8 | + | + | |||
| 25 | H | M | 59 | 39 | 21.3 | T | HI | L3 | 63 | 19 | 1.0 | 23 | 18 | 62 | 15 | 42 | 24 | 6 | -0.6 | + | + | |||
| 26 | H | F | 55 | 37 | 19.0 | T | HI | L3 | 33 | 19 | 1.2 | 4 | 2 | 37 | 11 | 53 | 40 | 12 | -1.9 | + | + | |||
| 27 | H | F | 45 | 31 | 19.3 | L | Zielke | L3 | 46 | 16 | 1.4 | 13 | 8 | 12 | 9 | 38 | 44 | 17 | -1.0 | + | + | |||
| 28 | L | F | 52 | 37 | 22.7 | D | HI | L4 | 33 | 33 | 1.6 | 5 | 9 | 28 | 12 | 42 | 48 | 19 | 5.4 | + | + | |||
| 29 | L | F | 51 | 37 | 20.5 | L | Dwyer | L4 | 41 | 18 | 0.6 | 2 | 0 | 32 | 17 | 31 | 63 | 47 | 5.0 | + | - | |||
| 30 | L | F | 52 | 38 | 19.8 | L | Dwyer | L4 | 41 | 20 | 4.3 | 0 | 3 | 19 | 20 | 28 | 38 | 14 | 6.4 | + | + | |||
| 31 | L | F | 49 | 30 | 19.0 | L | Zielke | L4 | 41 | 33 | 0.6 | 0 | 4 | 21 | 6 | 37 | 34 | 9 | 1.3 | + | + | |||
| 32 | L | F | 43 | 27 | 21.7 | D | Multi hook | L4 | 65 | 47 | 0.6 | 7 | 5 | 35 | 23 | 34 | 38 | 14 | 6.0 | + | - | |||
| 33 | L | F | 56 | 42 | 20.0 | D | HI | L4 | 56 | 42 | 2.3 | 6 | 8 | 53 | 30 | 43 | 46 | 24 | 3.4 | + | + | |||
| 34 | L | M | 44 | 28 | 22.0 | D | Multi hook | L4 | 42 | 28 | 4.3 | 4 | 10 | 14 | 11 | 14 | 44 | 21 | 8.4 | + | + | |||
| 35 | L | F | 46 | 32 | 22.3 | D | HI wiring | L5 | 31 | 40 | 1.1 | 4 | 12 | 2 | 6 | 28 | 67 | 31 | 8.1 | + | + | |||
BMI: body mass index, LFV: the lowest fused vertebra, TK: thoracic kyphosis, TLK: thoracolumbar kyphosis, LL: lumbar lordosis, PI: pelvic incidence, PT: pelvic tilt, SVA: sagittal vertical axis, DD: disc degeneration with Pfirrmann grade 4 or 5, T: thoracic curve, D: double major curve, L: thoracolumbar/lumbar curve, HI: Harrington instrumentation.
There were 27 subjects classified into H group and 8 classified into L group. There were no significant differences between these two groups in terms of age at the time of follow-up (H group: 50.0 years, L group: 49.2 years, p=0.749), observation period following surgery (H group: 35.4 years, L group: 33.9 years, p=0.562), body mass index (H group: 21.2, L group: 21.0, p=0.711), Cobb angle before surgery (H group: 73.5 degrees, L group: 57.3 degrees, p=0.191), or Cobb angle two years following surgery (H group: 41.8 degrees, L group: 30.2 degrees, p=0.091). Regarding curve type, among the subjects in the H group there were 23 patients with thoracic curve, 2 with thoracolumbar/lumbar curve, and 2 with double major curve. Among the subjects in the L group, there were 3 patients with thoracolumbar/lumbar curve and 5 with double major curve. As for the surgical procedure, for the H group, there were 14 cases of Harrington instrumentation, 9 of Harrington instrumentation with wiring, 2 of Luque wiring, and 2 of the Zielke method. For the L group, there were 2 cases of Harrington instrumentation, 1 of Harrington instrumentation with wiring, 2 of multiple hook, 2 of the Dwyer method, and 1 case of the Zielke method.
Sixteen of 27 patients in the H group had DD(+) (59.3%), compared with 8 of 8 in the L group (100%). The L group had significantly advanced disc degeneration on MRI (p=0.029) (Fig. 1). Fourteen of 27 patients in the H group had Modic changes (51.9%), compared with 6 of 8 in the L group (75.0%). There was no significant difference between the two groups in terms of Modic changes (p=0.245) (Table 2).
Figure 1.
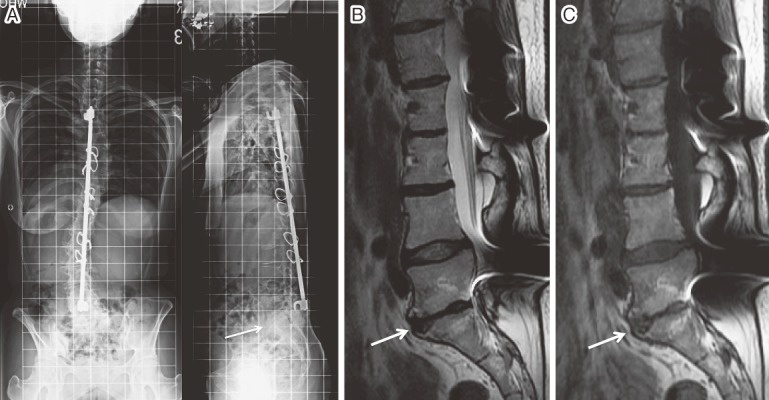
A 46-year-old female. She underwent posterior spinal fusion with Harrington rods and wires at the age of 14 years. (A) X-rays taken 32 years after spinal fusion down to L5. Lateral radiograph showed flat back and sagittal imbalance with remained L5-S1 disc narrowing. (B) T2-weighted image of MRI. Non-fused L5-S1 disc was severely degenerated and the Pfirrmann disc score was graded 5. (C) T1-weighted image of MRI showed Modic type 2 change.
Table 2.
MRI Findings of Lumbar Spine Degeneration: Comparison between H Group and L Group.
| H group | L group | P value | |
|---|---|---|---|
| DD (+) | 59.3% | 100% | 0.029* |
| Modic (+) | 51.9% | 75.0% | 0.245 |
Pfirrmann grades 4 or 5 were considered lumbar disc degeneration positive (DD(+)), while those with other scores were considered negative (DD(-)). Those with Modic changes were named Modic(+), and those without Modic(-). * indicates significant difference between groups.
There were no significant differences between the two groups in thoracic curve, lumbar curve, or coronal balance. L4 vertebral tilt was not significantly different between the two groups. However, the H group had greater L3 vertebral tilt than the L group. The L group showed less lumbar lordosis than the H group (H group: 48.1 degrees, L group: 32.1 degrees, p=0.023) and greater SVA (H group: 1.2 cm, L group: 5.5 cm, p=0.007), in addition to sagittal plane imbalance (Table 3).
Table 3.
X-ray Parameters of H Group and L Group.
| H group | L group | P value | |
|---|---|---|---|
| Thoracic curve (°) | 49.5±16.8 | 43.8±11.4 | 0.536 |
| Lumbar curve (°) | 25.4±11.8 | 32.6±10.3 | 0.196 |
| Coronal balance (cm) | 1.6±1.3 | 1.9±1.6 | 0.831 |
| L3 tilt (°) | 10.0±8.4 | 3.5±2.6 | 0.033* |
| L4 tilt (°) | 9.0±7.2 | 6.4±4.0 | 0.454 |
| TK (T5-T12) (°) | 29.7±14.9 | 25.5±15.3 | 0.712 |
| TLK (T10-L2) (°) | 10.8±10.6 | 15.6±8.5 | 0.216 |
| LL (L1-S1) (°) | 48.1±14.6 | 32.1±10.3 | 0.023* |
| PI (°) | 44.7±12.7 | 47.2±11.9 | 0.724 |
| PT (°) | 15.6±10.7 | 22.3±12.0 | 0.332 |
| SVA (cm) | 1.2±4.5 | 5.5±2.3 | 0.007* |
Values are mean (±: standard division). * indicates significant difference between groups. TK: thoracic kyphosis, TLK: thoracolumbar kyphosis, LL: lumbar lordosis, PI: pelvic incidence, PT: pelvic tilt, SVA: sagittal vertical axis.
There were no significant differences between the groups in all domains of the SRS-22, the RDQ, or the ODI (Table 4).
Table 4.
Questionnaire Scores of H Group and L Group.
| H group | L group | P value | ||
|---|---|---|---|---|
| SRS-22 | ||||
| Function | 4.3±0.6 | 4.4±0.3 | 0.511 | |
| Pain | 4.5±0.5 | 4.3±0.7 | 0.371 | |
| Self image | 3.0±0.8 | 2.9±0.7 | 0.696 | |
| Mental health | 4.2±0.8 | 4.0±0.6 | 0.337 | |
| Satisfaction | 3.7±0.7 | 3.3±0.9 | 0.167 | |
| RDQ | 0.5±1.2 | 2.3±5.2 | 0.131 | |
| ODI (%) | 6.8±8.4 | 8.9±8.3 | 0.661 | |
Values are mean (±: standard division). RDQ: Roland-Morris Disability Questionnaire, ODI: Oswestry Disability Index.
Intra-observer reliability of MRI evaluations
Intra-observer reliability was calculated using intra-class correlation coefficients (ICC). ICC of Pfirrmann classification was 0.775, indicating good agreement, and ICC of Modic change was 0.800, indicating excellent agreement.
Comparison between participants and non-participants
Participants and non-participants were compared. There were no significant differences between these groups in terms of their age at surgery (participants: 14.7±2.0 years vs. non-participants: 14.8±2.0 years, p=0.580), preoperative scoliosis curve (68.7±21.0 degrees vs. 68.2±20.0 degrees, p=0.968), and postoperative scoliosis curve 2 years after surgery (36.9±15.3 degrees vs. 39.7±16.3 degrees, p=0.469). When the percentages of participants and non-participants were compared by sex, there was no significant difference between these groups in terms of the percentage of women (participants: 85.7% vs. non-participants: 91.7%, p=0.253).
Discussion
Compared with those in the H group, subjects in the L group who underwent spinal fusion down to L4 or lower, disc degeneration progressed, lumbar lordosis was decreased, and sagittal imbalance was developed. Whether disc degeneration led to less lumbar lordosis and sagittal plane imbalance or whether disc generation was present from the time of surgery reducing lumbar lordosis was not verified, since there were no X-ray films remaining from the time before surgery or of progress since surgery. Hansen et al. reported that reductions in lumbar lordosis were due to increases in age-related disc degeneration12). Harding et al. pointed out that sagittal imbalance and/or malalignment of the spine following fusion were factors that contribute to adjacent segment degeneration13). In the L group, because less motion segments were preserved, progress of age-related disc degeneration may lead to decreased lumbar lordosis.
In terms of most of the parameters for back pain and HRQOL score, the L group was generally inferior to H group, but no score reached statistically significance. Although SRS-22 pain, RDQ, and ODI score were worse in the L group, there were no statistically significant differences. It may be due to the small sample size of the L group of 8 patients. Since the present study was considerably long-term follow-up period, it was extremely difficult for us to include all the patients. In the future, we hope to attempt again to contact the patients who did not reply or refused doctor's visits.
There are several existing reports on non-fused intervertebral disc degeneration in patients who underwent spinal fusion for AIS. Green et al. compared AIS patients' preoperative MRIs with those from an average of 11 postoperative years later. They recognized progression of disc degeneration in 85% of the subjects, but it showed no association with low back pain14). Nohara et al. examined MRIs from AIS patients with an average of 12.8 years post hybrid method operation. They found that 48% of the patients had Pfirrmann grade 3 or higher intervertebral disc degeneration, but there was also no low back pain observed in their series15). On the other hand, Danielsson et al. with an average of 25 years following Harrington rod placement reported a relationship between the intensity of back pain and disc degeneration, in comparison to healthy controls3. In the present study, an average of 35 years after surgery, 68.6% of the patients had intervertebral disc degeneration of Pfirrmann grade 4 or higher. However, a previous study reported that MRI findings might not always be related to patient reported questionnaires16). Based on SRS-22, RDQ, and/or ODI, the findings did not relate to low back pain.
As far we know, there was no previous report on Modic changes between non-fused segments in AIS patients who underwent spinal fusion. In the current study, we detected Modic changes in 57.1% of the subjects. There are controversial reports about the relationship of low back pain and Modic changes. Toyone et al. reported MRI signal changes in vertebral endplates associated with back pain17). In a longitudinal cohort study, Määttä et al. characterized Modic changes as a risk factor for severe back pain18). Additionally, in an immunohistochemical study, Ohtori et al. detected the presence of tumor necrosis factor in a vertebral body endplate with Modic changes and reported this as a cause of low back pain19). On the other hand, Kovacs et al. reported no association of chronic low back pain with Modic changes20). In the present study, the presence of Modic changes was not associated with low back pain.
There are several limitations to our study. As our study had a very long follow-up period, there was a low follow-up rate. Half of our patients have relocated. In Japan, there is no national patient registry, so these patients could not be followed up. Additionally, in 25.8% of patients, there was unfortunately no reply to our attempts at contact. This study had a considerably long follow-up period, and this time it was not possible to include any more patients. In the future, we are considering contacting again the patients who did not reply and those who declined to participate. Since X-ray films from the time of the original operations have been discarded, it was not possible to verify the preoperative condition of patients for comparison purposes. According to previous decision making of fusion level, the lowest fused vertebra was almost 2 levels below the lower end vertebra. But it was not possible to confirm the selection of the fusion level because of loss of the original films. In the present day, because imaging data are stored digitally rather than as physical films, data are easier to store and fears of losing them are reduced; for long-term follow-up studies, it will be necessary for a new generation of researchers to take over.
AIS patients with an average of 35 years after spinal fusion surgery showed lumbar disc degeneration in the non-fused intervertebral discs as well as Modic changes, though we could not observe related back pain or HRQOL changes. In patients with the lowest fusion level at L4 or lower, although L3 vertebral tilt in the coronal plane was small, there was reduced lumbar lordosis in the sagittal plane and considerable SVA imbalance, and disc degeneration had significantly progressed. There was no significant difference in RDQ or ODI related to low back pain. Although fusion levels depend on the curve types in most cases, the lowest fusion level at L3 or higher is recommended in order to reduce the risk of disc degeneration in midlife.
Conflicts of Interest: The authors declare that there are no conflicts of interest.
Acknowledgments
The authors thank Mr. Hideo Ishikawa, Mr. Mitoshi Ishino, Ms. Mika Fujiwara, and Ms. Mayumi Ishii for assistance on data collection.
References
- 1.Akazawa T, Minami S, Kotani T, Nemoto T, Koshi T, Takahashi K. Long-term clinical outcomes of surgery for adolescent idiopathic scoliosis 21 to 41 years later. Spine 2012; 37(5): 402-405. [DOI] [PubMed] [Google Scholar]
- 2.Bartie BJ, Lonstein JE, Winter RB. Long-term follow-up of adolescent idiopathic scoliosis patients who had Harrington instrumentation and fusion to the lower lumbar vertebrae: Is low back pain a problem? Spine 2009; 34(24): E873-E878. [DOI] [PubMed] [Google Scholar]
- 3.Danielsson AJ, Cederlund CG, Ekholm S, Nachemson AL. The prevalence of disc aging and back pain after fusion extending into the lower lumbar spine: a matched MR study twenty-five years after surgery for adolescent idiopathic scoliosis. Acta Radiol 2001; 42(2): 187-197. [DOI] [PubMed] [Google Scholar]
- 4.Danielsson AJ, Nachemson AL. Back pain and function 23 years after fusion for adolescent idiopathic scoliosis: a case-control study—part II. Spine 2003; 28(18): E373-E383. [DOI] [PubMed] [Google Scholar]
- 5.Mariconda M, Galasso O, Barca P, Milano C. Minimum 20-year follow-up results of Harrington rod fusion for idiopathic scoliosis. Eur Spine J 2005; 14(9): 854-861. [DOI] [PubMed] [Google Scholar]
- 6.Cochran T, Irstam L, Nachemson A. Long-term anatomic and functional changes in patients with adolescent idiopathic scoliosis treated by Harrington rod fusion. Spine 1983; 8(6): 576-584. [DOI] [PubMed] [Google Scholar]
- 7.Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M. Adult scoliosis: a quantitative radiographic analysis. Spine 2002; 27(4): 387-392. [DOI] [PubMed] [Google Scholar]
- 8.Toyone T, Ozawa T, Inada K, Orita S, Ohtori S, Takahashi K. Horizontal fixation the L3 vertebra with a tilt of less than 5° can prevent the long-term curve progression of unfused adult scoliosis: ten-year follow-up study of concave PLIF at the wedged disc below the caudal end vertebra. Spine 2015; 40(5): 312-315. [DOI] [PubMed] [Google Scholar]
- 9.Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 2001; 26(17): 1873-1878. [DOI] [PubMed] [Google Scholar]
- 10.Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 1988; 166: 193-199. [DOI] [PubMed] [Google Scholar]
- 11.Zhang YH, Zhao CQ, Jiang LS, Chen XD, Dai LY. Modic changes: a systematic review of the literature. Eur Spine J 2008; 17(10): 1289-1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hansen BB, Bendix T, Grindsted J, et al. Effect of lumbar disc degeneration and low-back pain on the lumbar lordosis in supine and standing: a cross-sectional MRI study. Spine 2015; 40(21): 1690-1696. [DOI] [PubMed] [Google Scholar]
- 13.Harding IJ, Charosky S, Vialle R, Chopin DH. Lumbar disc degeneration below a long arthrodesis (performed for scoliosis in adults) to L4 or L5. Eur Spine J 2008; 17(2): 250-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Green DW, Lawhorne TW 3rd, Widmann RF, et al. Long-term magnetic resonance imaging follow-up demonstrates minimal transitional level lumbar disc degeneration after posterior spine fusion for adolescent idiopathic scoliosis. Spine 2011; 36(23): 1948-1954. [DOI] [PubMed] [Google Scholar]
- 15.Nohara A, Kawakami N, Seki K, et al. The effects of spinal fusion on lumbar disc degeneration in patients with adolescent idiopathic scoliosis: a minimum 10-year follow-Up. Spine Deform 2015; 3: 462-468. [DOI] [PubMed] [Google Scholar]
- 16.Kelly DM, McCarthy RE, McCullough FL, Kelly HR. Long-term outcomes of anterior spinal fusion with instrumentation for thoracolumbar and lumbar curves in adolescent idiopathic scoliosis. Spine 2010; 35(2): 194-198. [DOI] [PubMed] [Google Scholar]
- 17.Toyone T, Takahashi K, Kitahara H, Yamagata M, Murakami M, Moriya H. Vertebral bone-marrow changes in degenerative lumbar disc desease. J Bone Join Surg [Br] 1994; 76-B(5): 757-764. [PubMed] [Google Scholar]
- 18.Määttä JH, Wadge S, MacGregor A, Karppinen J, Williams FMK. Vertebral endplate (Modic) change is an independent risk factor for episodes of severe and disabling low back pain. Spine 2015; 40(15): 1187-1193. [DOI] [PubMed] [Google Scholar]
- 19.Ohtori S, Inoue G, Ito T, Koshi T, Ozawa T. Tumor necrosis factor-immunoreactive cells and PGP 9.5-immunoreactive nerve fibers in vertebral endplates of patients with discogenic low back pain and Modic type 1 or type 2 changes on MRI. Spine 2006; 31(9): 1026-1031. [DOI] [PubMed] [Google Scholar]
- 20.Kovacs FM, Arana E, Royuela A, et al. Vertebral endplate changes are not associated with chronic low back pain among Southern European subjects: a case control study. AJNR Am J Neuroradiol 2012; 33(8): 1519-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]


