Abstract
Introduction
Sacroiliac joint pain (SIJP) after lumbar fusion surgery has recently gained attention as a source of low back pain after lumbar fusion. There are two risk factors for postoperative SIJP, i.e., fusion involving the sacrum and multiple-segment fusion. In this study, we examined whether SIJP could occur more frequently in patients with two risk factors (multiple-segment fusion to sacrum). Further, we examined SIJP after multiple-segment (≥3) lumbar fusion, focusing on the difference between floating fusion (non-fused sacrum) and fixed fusion (fused sacrum).
Methods
Ninety-one patients who underwent multiple-segment lumbar fusion were included. Patients without preoperative clinical SIJP were considered. Of these, 17 developed new-onset SIJP. We investigated postoperative SIJP development, duration from surgery to SIJP onset, and postoperative treatment outcomes of SIJP patients using Japanese Orthopaedic Association (JOA) scores. We compared the findings between floating fusion group and fixed fusion group.
Results
The incidence of SIJP was significantly higher with fixed fusion (32.1%) than with floating fusion (12.7%). The mean time of onset of sacroiliac joint pain was at 8.63 (2-13) months after surgery in the floating fusion group and 3.78 (1-10) months after surgery in the fixed fusion group, indicating that incidence occurred significantly earlier in the fixed fusion group. Our treatment outcome indicated that the mean JOA score significantly improved in the floating fusion group from 5.13 at the time of onset to 9.50 at the time of final follow-up; however, in the fixed fusion group, it improved from 5.78 at the time of onset to 7.33 at the time of final follow-up, indicating no significant improvement.
Conclusions
In multiple-segment lumbar fusion, fixed fusion (fused sacrum) has a very high risk of SIJP. In addition, the onset of SIJP in such cases may occur earlier. This aspect deserves consideration, given the difficulty of pain treatment.
Keywords: lumbar fusion, sacroiliac joint pain, low back pain
Introduction
Lumbar spinal fusion has long been the treatment of choice for various lumbar disorders1), and it has been reported to offer better clinical outcomes than conservative treatment2). However, despite careful patient selection, the failure rate of this procedure ranges from 5% to 30% according to previous studies3,4). Low back pain (LBP) often persists postoperatively or appears as a new-onset condition and may be difficult to treat. Potential causes of LBP after lumbar fusion include iliac graft harvesting5), adjacent segment disease (ASD; e.g., listhesis, instability, disc herniation, stenosis, and facet pain)6), pseudarthrosis, sacroiliac joint pain (SIJP)7), or fusion implant-related LBP8). Since the 2000s, several authors have suggested that SIJP causes LBP after lumbar fusion4,8-10). Both fusion to the sacrum4,9) and multiple-segment fusion11,12) are risk factors for SIJP following lumbar fusion. We hypothesized that the incidence of SIJP might increase when multiple-segment fusion and fusion to the sacrum were simultaneously performed.
The recent increase in the number of patients with osteoporotic kyphosis and adult spinal deformities has led to an increase in the frequency of multiple-segment lumbar fusion procedures. In this study, we investigated SIJP after multiple-segment (≥3) lumbar fusion, focusing on the difference between non-fused and fused sacrum cases.
Methods
Patients
Between June 2006 and June 2010, 95 patients underwent multiple-segment lumbar fusion, excluding cases of sacropelvic fixation. Patients without preoperative clinical SIJP were eligible for enrollment. All cases involved posterior spinal instrumentation surgery without iliac graft harvesting. Although the range of fixation for adult spinal deformity remains under debate, as a rule, we set the range of fixation for scoliosis as the principal main curve only. We performed fixation to the sacrum when lateral wedging of the intervertebral disc of L5/S or foraminal stenosis at L5/S was observed. In cases of kyphosis with poor sagittal plane balance, the fixation range was determined based on the extent of pelvic retroversion and erector spinae muscle atrophy.
Of the 95 patients, 91 were followed up for >2 years after surgery (follow-up rate: 95.8%); four could not undergo follow-up. Accordingly, 91 patients were included. We classified the patients into two groups: floating fusion (non-fused sacrum; n=63) and fixed fusion (fused sacrum; n=28). Patients' characteristics are shown in Table 1.
Table 1.
Patient Demographics.
| floating fusion group (non-fused sacrum) |
fixed fusion group (fused sacrum) |
|
|---|---|---|
| Number of patients | 63 | 28 |
| Follow-up period (months), mean (range) | 61.2±21.7 (24-105) | 58.0± 26.1 (24-110) |
| Age (years), mean (range) | 70.0±6.54 (51-81) | 69.6±8.64 (44-80) |
| Male (%): Female (%) | 17 (27.0): 46 (73.0) | 6 (21.4): 22 (78.6) |
| Number of fused segments, mean (range) | 4.29±1.31 (3-8) | 4.57±2.27 (3-13) |
| Preoperative diagnosis | ||
| Degenerative lumbar kyphosis | 19 | 12 |
| Degenerative lumbar kypho-scoliosis | 15 | 9 |
| Degenerative lumbar scoliosis | 13 | 4 |
| Osteoporotic kyphosis | 14 | 1 |
| Degenerative lumbar spondylolisthesis | 2 | 2 |
The present study was conducted in compliance with the Declaration of Helsinki after approval for the study protocol was obtained from Akita Kousei Medical Center.
Investigation
For all patients, the postoperative follow-up was performed by spinal surgeons (EA, TK, and TA). The primary author (EU) recruited patients with postoperative new-onset LBP via referral from spinal surgeons and a thorough investigation of the medical records. Causes of postoperative LBP were diagnosed from physical, neurological, and imaging findings. If required, an additional nerve root block, facet block, and lumbar discography were performed. If instruments were suspected as the cause of pain, a local anesthetic was injected into the affected site. Patients with suspected SIJP in whom lumbar-derived causes were ruled out were referred to the primary author (EU). This author re-examined the patients and administered a sacroiliac joint (SIJ) block. We used the periarticular injection technique for the SIJ block13,14). Under fluoroscopy, the patient was positioned prone-oblique with the involved side facing down to ensure clear detection of the anterior and posterior margins of SIJ. A 90 mm 23-gauege spinal needle was inserted in the posterior margin of the joint. When it provoked the same level of pain as the patient's symptoms, the periarticular injection was performed (2 ml of 2% lidocaine). In each patient, pain relief was evaluated using a visual analog scale. Scores were obtained immediately before and 15 min after the SIJ block and were then compared. The injection was identified as effective if the patient indicated more than 70% decrease in pain.
Diagnostic criteria for SIJP
In accordance with the diagnostic criteria of Murakami et al.13), patients who met the following conditions were diagnosed with SIJP.
・Unilateral pain located in the lower lumbar region and buttocks.
・Pain not caused by other diseases of the lumbar spine or hip joint.
・Positive findings on at least two provocation tests (Patrick's test, Gaenslen's test, and SIJ shear test).
・Pain relief of ≥70% achieved with the SIJ block.
Treatment of SIJP patients
All SIJP patients received conservative treatment after lumbar fusion. In addition, all patients received the following: nonsteroidal anti-inflammatory drug (NSAID) administration, pelvic belt attachment, physical therapy, and therapeutic SIJ block (periarticular injection). In our hospital, surgical treatments such as SIJ arthrodesis were not performed.
Evaluation
The following parameters were evaluated (floating fusion vs. fixed fusion)
・Incidence of SIJP following multiple-segment lumbar fusion.
・Interval from fusion surgery until the onset of SIJP.
・Treatment outcomes of SIJP patients after fusion surgery.
To evaluate the treatment, we used the following six motions of the “Restriction of ADL” in the assessment of treatment for low back pain by the Japanese Orthopaedic Association (JOA) scoring system13,15): turning over while lying down, standing up from a chair, face washing, rising halfway or continuing to stand, lifting or holding heavy objects, and walking. Restrictions of those motions were assessed as follows: 0, severe restriction; 1, moderate restriction; and 2, no restriction. No patient had a neurological deficit or osteoarthrosis of the hip joint; accordingly, all restrictions were attributed to SIJP. Pain assessment was determined from the sum of those scores, with a highest possible score of 12 points. Assessments performed before surgery and at the last follow-up after surgery were compared. The improvement rate was calculated as follows13):
 |
Statistical analysis
All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan)16), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, EZR is a modified version of R commander designed to add statistical functions frequently used in biostatistics. Dichotomous data were compared using the Fisher's exact test, Mann-Whitney U test, and Wilcoxon signed-rank test. A P value of <0.05 was considered significant.
Results
All 91 patients exhibited amelioration of preoperative symptoms. However, 59 patients developed new-onset LBP during the postoperative follow-up period. Of these patients, 17 (28.8%, 17/59) were diagnosed with SIJP (Table 2). Furthermore, symptomatic ASD, proximal junctional fracture, instrument-related LBP, and pseudarthrosis were observed in 27 (45.8%, 27/59), 9 (15.3%, 9/59), 4 (6.8%, 4/59), and 2 (3.4%, 2/59) patients, respectively.
Table 2.
Characteristics of Patients with Sacroiliac Joint Pain after Fusion Surgery (N=17).
| Age/Gender | follow up (months) | Range of fused segments (number) | Pain-free interval (months) | JOA score onset/final | Improvement rate (%) |
|---|---|---|---|---|---|
| 80M | 71 | L1-4 (3) | 12 | 5/9 | 57.1 |
| 67F | 104 | T9-L3 (6) | 10 | 7/10 | 60.0 |
| 74F | 59 | L1-5 (4) | 13 | 3/11 | 88.9 |
| 72M | 90 | L2-S1 (4) | 6 | 9/9 | 0 |
| 78F | 57 | L2-5 (3) | 3 | 8/11 | 75.0 |
| 61F | 24 | L2-5 (3) | 8 | 7/11 | 80.0 |
| 77M | 24 | L1-S1 (5) | 1 | 4/7 | 37.5 |
| 80F | 55 | T12-S1 (6) | 1 | 3/3 | 0 |
| 76F | 24 | L2-S1 (4) | 3 | 6/6 | 0 |
| 75F | 68 | L2-5 (3) | 8 | 4/7 | 37.5 |
| 73F | 35 | L1-S1 (5) | 3 | 8/11 | 75.0 |
| 74F | 91 | L1-5 (4) | 13 | 4/9 | 62.5 |
| 64F | 64 | T10-L2 (4) | 2 | 3/8 | 55.6 |
| 76F | 57 | L3-S1 (3) | 2 | 6/11 | 83.3 |
| 44F | 76 | L3-S1 (3) | 6 | 6/8 | 33.3 |
| 71F | 70 | L2-S1 (4) | 10 | 5/5 | 0 |
| 68F | 68 | T12-S1 (6) | 2 | 5/6 | 14.3 |
The postoperative incidence of SIJP was 18.7%, or 17 of 91 patients. However, after we classified the patients into two groups, floating fusion (non-fused sacrum) and fixed fusion (fused sacrum), the SIJP incidence was 12.7% (8/63 patients) in the floating fusion group and 32.1% (9/28 patients) in the fixed fusion group. The incidence was significantly higher in the fixed fusion group (Table 3).
Table 3.
Development of SIJP after Multiple-segment Lumbar Fusion: Floating Fusion vs. Fixed Fusion.
| Group | No. of patients | SIJP | ||
|---|---|---|---|---|
| Incidence | Incidence rate | Duration of onset | ||
| Floating fusion (non-fused sacrum) | 63 | 8 | 12.7% | 8.63±4.27 months |
| Fixed fusion (fused sacrum) | 28 | 9 | 32.1%a | 3.78±2.99 monthsb |
aFisher’s exact test, P=0.0409
bMann-Whitney U test, P=0.0227
SIJP: sacroiliac joint pain
The mean time of onset of SIJP was 8.63±4.27 (2-13) months after surgery in the floating fusion group and 3.78±2.99 (1-10) months in the fixed fusion group, indicating that the fixed fusion group experienced SIJP incidence significantly earlier than the floating fusion group (Table 3). In the fixed fusion group, 6 of 9 patients experienced incidence within 3 months after surgery.
We evaluated the treatment outcome through changes in the JOA score (0-12 points). The treatment outcome for all SIJP patients indicated significant improvement to a mean of 8.35 at the time of final follow-up from a mean of 5.47 at the time of onset. The treatment outcomes of the floating fusion group indicated that the mean score significantly improved from 5.13 at the time of onset to 9.50 at the time of final follow-up. However, although the mean score in the fixed fusion group improved from 5.78 at the time of onset to 7.33 at the time of final follow-up, this was not statistically significant (Fig. 1). The mean of improvement rates for the two groups were 64.6% and 27.0%, respectively (Fig. 2). The improvement rate was significantly lower in the fixed fusion group.
Figure 1.
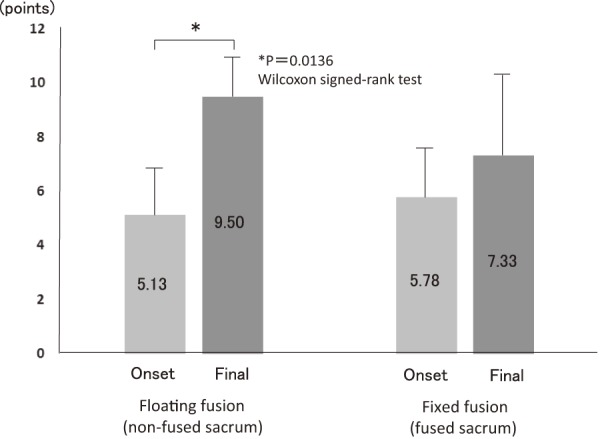
JOA scores: floating fusion vs. fixed fusion. Floating fusion group indicated that the mean score significantly improved from 5.13 at the time of onset to 9.50 at the time of final follow-up (P=0.0136, Wilcoxon signed-rank test). Whereas, in the fixed fusion group improved from 5.78 at the time of onset to 7.33 at the time of final follow-up, this was not statistically significant (P=0.0579).
Figure 2.
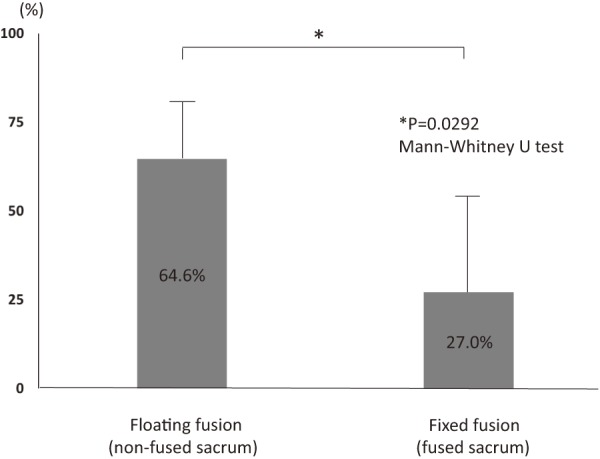
The mean of improvement rates of JOA score for the two groups. Floating fusion group was 64.6% and fixed fusion group was 27.0%. The improvement rate was significantly lower in the fixed fusion group. (P=0.0292, Mann-Whitney U test)
Discussion
The causes of LBP incidence after lumbar fusion surgery are widely known to be iliac bone graft postoperative pain and ASD, but it is not widely known that many cases are due to SIJP, and few studies have investigated SIJP4,8-10,12). It has been reported that SIJP is the cause of LBP after lumbar fusion surgery at a rate of 16.2%-43.0%4,8-10). In this study, the rate was 28.9%, which is consistent with the previous studies.
Although some studies reported the percentage of postoperative LBP cases that are caused by SIJP, only a few reported the incidence of SIJP among all fusion surgery cases. Liliang et al.10) reported SIJP in 21 of 391 fusion surgery cases, indicating an onset rate of 5.2%. However, a certain number of those cases were referred from other hospitals; thus, the accurate onset rate remains unclear. In our previous study12), we reported postoperative SIJP in 28 of 262 fusion surgery cases, including both one-segment and two-segments fusion (follow-up rate: 87.3%), indicating that the onset rate was 10.7%. In the present study, our investigation focusing on multiple-segment fusions of three or more segments revealed that the postoperative onset rate of SIJP was high at 18.7%. Furthermore, in the case of multiple-segment lumbar fusion to the sacrum, the incidence rate reached 32.1%.
ASD incidence after multiple-segment fusion surgery is widely known. Cheh et al.17) conducted a follow-up study for ≥5 years, during which they investigated cases after lumbar/thoracolumbar fusion. They found that the incidence of symptomatic ASD was higher in multiple-segment fusion, and that multiple-segment fusion is a risk factor for ASD incidence. In their report, three or more segment fusions were observed in 51 cases, and of these, symptomatic ASD occurred in 16 cases. It is indicated that symptomatic ASD incident rate is 31.4% (16/51) for three or more segment lumbar fusion. In the present study, symptomatic ASD was identified in 27 of 91 patients (29.7%), which is consistent with the findings reported by Cheh et al.
Regarding the mechanism of onset of SIJP after lumbar fusion, Frymoyer et al.7) hypothesized that spinal fusion involving the sacrum led to long-term compensatory hypermobility of SIJ and accelerated degeneration of these joints. Katz et al.9) reported that among patients with LBP after lumbar fusion to the sacrum, SIJ was identified as the cause of pain in 32% of patients and suspected in 29% of patients. Maigne et al.4) observed that among patients with SIJP after fusion surgery, 42% had L5-S1 fusion. Accordingly, these authors favored Frymoyer's hypothesis. Furthermore, they believed that the mechanism of onset of SIJP after lumbar fusion was similar to that of ASD after spinal fusion.
Regarding sacrum fusion, SIJ is adjacent to the fusion segment11,18), which might lead to LBP after lumbar spinal fusion. In a previous study, Ha et al.18) used computed tomography to examine the incidence of SIJ degeneration following lumbar fusion and reported an incidence of 75% in the fixed fusion group, a significantly higher rate than that in the floating fusion group (38.2%). Although Maigne et al.4) found no significant difference, they claimed that SIJP tended to occur more often in patients with fusion involving the sacrum than in those in whom lumbar fusion did not involve the sacrum.
We previously reported12) that multiple-segment fusion is a risk factor regardless of whether fusion involved the sacrum or not. Our investigation of the mechanism led us to believe that the fusion of multiple segments considerably restricts the motion of the lumbar or thoracolumbar spine depending on the number of involved spinal segments, consequently increasing the stress at SIJ.
In the present study, we compared postoperative SIJP incidence of floating fusion and fixed fusion in patients with multiple-segment fusion of ≥3 segments. We found the incidence was significantly higher in the fixed fusion group, confirming that fusion involving the sacrum is a risk factor for SIJP incidence.
Only the report by Maigne et al. mentioned the timing of SIJP onset following lumbar spinal surgery4). They indicated that SIJP onset occurred after a pain-free interval of at least 3 months following surgery. In the present study, LBP was experienced 8.63 months after surgery on average in patients in whom fusion did not involve the sacrum, which is consistent with the findings reported by Maigne et al. However, we found that in patients in whom fusion involved the sacrum, onset of SIJP occurred significantly earlier, at an average of 3.78 months after surgery and 6 of 9 patients experienced incidence within 3 months after surgery. It is conceivable, therefore, that in addition to multiple-segment fusion, fusion involving the sacrum exerts considerable stress on SIJ.
Studies have indicated that treatment of SIJP includes conservative therapy and surgery. Conservative treatment consists of rest, NSAID administration, pelvis fixation using a belt19), physical therapy20-22), and SIJ block23). However, no previous publications have described the treatment outcomes for SIJP after lumbar fusion. Liliang et al.23) described therapeutic intra-articular injections of steroids and local anesthetics. They reported that 66.7% (26/39) of patients experienced a >50% SIJP reduction for >6 weeks after SIJ block. In that study, 12 patients had a history of lumbar fusion. The SIJ block was effective in 5 of those 12 patients (42%). Conversely, the SIJ block worked in 21 of 27 patients (78%) without a history of lumbar fusion. Furthermore, the duration of SIJ block efficacy was shorter in patients with a history of lumbar fusion. In our present study, we did not make comparisons with patients in whom fusion was not performed. Murakami et al.13) investigated SIJ block (periarticular injection) on nonsurgical cases and reported that the mean pre-treatment JOA score was 5.0, the mean post-treatment JOA score was 11.7, and the recovery rate was 96%. In our floating fusion group the pre-treatment score was 5.13, the post-treatment score was 9.50, and the recovery rate was 64.6%; in our fixed fusion group the pre-treatment score was 5.78, the post-treatment score was 7.33, and the recovery rate was 27.0%, indicating that our treatment outcomes were inferior to those reported by Murakami et al. As reported by Liliang et al.23), it appears difficult to treat post-fusion SIJP.
In patients in whom conservative therapy does not lead to improvement, SIJ fusion is the final option. In the past, a large number of posterior fusion24,25), lateral fusion26), and anterior fusion27,28) procedures have been attempted, but no procedure has shown a satisfactory outcome. In recent years, the posterior approach procedure, known as the distraction interference arthrodesis with neurovascular anticipation method29), and the lateral approach procedure, known as the iFuse implant system30), have been developed and are reported to have good outcomes. However, no study has reported the surgical outcomes for patients manifesting SIJP after lumbar fusion surgery31); hence, surgeons should be more careful while planning surgical treatment in such patients.
Conclusions
SIJP should not be overlooked as a cause of low back pain following lumbar spinal fusion. In particular, patients with multiple-segment fusion combined with fixation to the sacrum have an extremely high risk of SIJP incidence. In addition, the onset of SIJP in such cases may occur early, and pain treatment may be challenging. Therefore, such patients should be treated with caution.
Conflicts of Interest: The authors declare that there are no conflicts of interest.
References
- 1.Deyo RA, Nachemson A, Mirza SK. Spine-fusion surgery: the case for restraint. N Engl J Med. 2004; 350(7): 722-6. [DOI] [PubMed] [Google Scholar]
- 2.Fritzell P, Hagg O, Wessberg P, et al. Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine. 2001; 26(23): 2521-32. [DOI] [PubMed] [Google Scholar]
- 3.Bose B. Outcomes after posterolateral lumbar fusion with instrumentation in patients treated with adjunctive pulsed electromagnetic field stimulation. Adv Ther. 2001; 18(1): 12-20. [DOI] [PubMed] [Google Scholar]
- 4.Maigne JY, Planchon CA. Sacroiliac joint pain after lumbar fusion: A study with anesthetic blocks. Eur Spine J. 2005; 14(7): 654-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ebraheim NA, Elgafy H, Semaan HB. Computed tomographic findings in patients with persistent sacroiliac pain after posterior iliac graft harvesting. Spine. 2000; 25(16): 2047-51. [DOI] [PubMed] [Google Scholar]
- 6.Park P, Garton HJ, Gala VC, Hoff JT, et al. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine. 2004; 29(17): 1938-44. [DOI] [PubMed] [Google Scholar]
- 7.Frymoyer JW, Howe J, Kuhlmann D. The long-term effects of spinal fusion on the sacroiliac joints and ilium. Clin Orthop Relat Res. 1978; 134: 196-201. [PubMed] [Google Scholar]
- 8.Depalma MJ, Ketchum JM, Saullo TR. Etiology of chronic low back pain in patients having undergone lumbar fusion. Pain Med. 2011; 12(5): 732-9. [DOI] [PubMed] [Google Scholar]
- 9.Katz V, Schofferman J, Reynolds J. The sacroiliac joint: a potential cause of pain after lumbar fusion to the sacrum. J Spine Disord Tech. 2003; 16(1): 96-9. [DOI] [PubMed] [Google Scholar]
- 10.Liliang PC, Lu K, Liang CL, et al. Sacroiliac joint pain after lumbar and lumbosacral fusion: findings using dual sacroiliac joint blocks. Pain Med. 2011; 12(4): 565-70. [DOI] [PubMed] [Google Scholar]
- 11.Ivanov AA, Kiapour A, Ebraheim NA, et al. Lumbar fusion leads to increase in angular motion and stress across sacroiliac joint. Spine. 2009; 34(5): 162-9. [DOI] [PubMed] [Google Scholar]
- 12.Unoki E, Abe E, Murai H, et al. Fusion of multiple segments can increase the incidence of sacroiliac joint pain after lumbar or lumbosacral fusion. Spine. 2016; 41(12): 999-1005. [DOI] [PubMed] [Google Scholar]
- 13.Murakami E, Tanaka Y, Aizawa T, et al. Effect of periarticular and intraarticular lidocaine injections for sacroiliac joint pain: prospective comparative study. J Orthop Sci. 2007; 12(3): 274-80. [DOI] [PubMed] [Google Scholar]
- 14.Kurosawa D, Murakami E, Ozawa H, et al. A diagnostic scoring system for sacroiliac joint pain originating from the posterior ligament. Pain Med. 2016; 0: 1-11. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 15.Japanese Orthopaedic Association. Assessment of treatment of low back pain. J Jpn Orthop Assoc. 1986; 60(3): 393-394. [Google Scholar]
- 16.Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013; 48(3): 452-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheh G, Bridwell KH, Lenke LG, et al. Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation. Spine. 2007; 32(20): 2253-7. [DOI] [PubMed] [Google Scholar]
- 18.Ha KY, Lee JS, Kim KW. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: a prospective cohort study over five-year follow-up. Spine. 2008; 33(11): 1192-8. [DOI] [PubMed] [Google Scholar]
- 19.Vleeming A, Buyruk HM, Stoeckart R, et al. An integrated therapy for peripartum pelvic instability: a study of the biomechanical effects of pelvic belts. Am J Obset Gynecol. 1992; 166(4): 1243-7. [DOI] [PubMed] [Google Scholar]
- 20.DonTigney RL. Function and pathomechanics of the sacroiliac joint, A review. Phys Ther. 1985; 65(1): 35-44. [DOI] [PubMed] [Google Scholar]
- 21.Greenman PE. Clinical aspects of sacroiliac function in walking. J Man Med. 1990; 5: 125-9. [Google Scholar]
- 22.Slipman CW, Whyte WS 2nd, Chow DW, et al. Sacroiliac joint syndrome. Pain Physician. 2001; 4(2): 143-52. [PubMed] [Google Scholar]
- 23.Liliang PC, Lu K, Weng HC, et al. The therapeutic efficacy of sacroiliac joint blocks with triamcinolone acetonide in the treatment of sacroiliac joint dysfunction without spondyloarthropathy. Spine. 2009; 34(9): 896-900. [DOI] [PubMed] [Google Scholar]
- 24.Waisbrod H, Krainick JU, Gerbershagen HU. Sacroiliac joint arthrodesis for chronic lower back pain. Arch Orthop Trauma Surg. 1987; 106(4): 238-40. [DOI] [PubMed] [Google Scholar]
- 25.Belanger TA, Dall BE. Sacroiliac arthrodesis using a posterior midline fascial splitting approach and pedicle screw instrumentation: a new technique. J Spinal Disord. 2001; 14(2): 118-24. [DOI] [PubMed] [Google Scholar]
- 26.Giannikas KA, Khan AM, Karski MT, et al. Sacroiliac joint fusion for chronic pain: a simple technique avoiding the use of metal work. Eur Spine J. 2004; 13(3): 253-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pennal GF, Massiah KA. Nonunion and delayed union of fractures of the pelvis. Clin Orthop Relat Res. 1980; 151: 124-9. [PubMed] [Google Scholar]
- 28.Rand JA. Anterior sacro-iliac arthrodesis for post-traumatic sacro-iliac arthritis. J Bone Joint Surg Am. 1985; 67(1): 157-9. [PubMed] [Google Scholar]
- 29.Endres S, Ludwig E. Outcome of distraction interference arthrodesis of the sacroiliac joint for sacroiliac arthritis. Indian J Orthop. 2013; 47(5): 437-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rudolf L, Capobianco R. Five-year clinical and radiographic outcomes after minimally invasive sacroiliac joint fusion using triangular implants. Open Orthop J. 2014; 8: 375-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yoshihara H. Sacroiliac joint pain after lumbar / lumbosacral fusion: current knowledge. Eur Spine J. 2012; 21(9): 1786-96. [DOI] [PMC free article] [PubMed] [Google Scholar]


