Abstract
Planning of surgical treatment requires determination of whether osteoarthritis of the spine with lumbar pain should be treated as spinal canal stenosis with or without deformity or as lumbar degenerative scoliosis and clarification of whether treatment should be provided for both. When sagittal spinal alignment is not appropriate, symptoms of adult spinal deformity may be observed. To correct this deformity, appropriate pelvic tilt should be obtained similar to that in healthy adults, and, especially, the retroversion of the pelvis should be corrected.
Keywords: adult spinal deformity, surgical treatment, strategy, lumbar kyphoscoliosis, pathology
Introduction
Osteoarthritis of the spine may accompany intervertebral disk degeneration and intervertebral joint arthritis with aging as well as decreased back muscle strength, loss of lumbar lordosis, and scoliotic deformity. Takemitsu et al.1) suggested that lumbar degenerative kyphosis is caused by decreased strength and atrophy of back muscles, narrowing of intervertebral disk space, and flat deformed vertebral bodies. Glassman et al.2) and Lafage et al.3) proposed that deteriorated QOL in adults with spinal deformity is largely due to sagittal imbalance with kyphotic deformity and retroverted pelvis, rather than scoliotic deformity of the coronal plane.
Kyphoscoliotic spinal deformity, which is also referred to as lumbar degenerative scoliosis with kyphotic deformity, significantly decreases QOL in middle-aged patients. In such cases, there is a need to determine whether osteoarthritis of the spine with low back pain should be treated as spinal canal stenosis with or without deformity or as lumbar degenerative scoliosis and to clarify whether treatment should be provided for both in the planning of surgery. A patient with spinal canal stenosis and scoliotic deformity with no low back pain and mainly intermittent claudication and neurological symptoms, such as numbness, pain, and weakness in the lower extremities, should be diagnosed with lumbar spinal canal stenosis. Thus, decompression or decompression with fusion should be selected as surgery for stenosis, rather than focusing on correction of the deformity. In contrast, scoliotic deformity of ≥30° and kyphotic deformity seen in kyphoscoliosis often causes low back pain and should be diagnosed as degenerative lumbar kyphoscoliosis requiring correction of the deformity.
Classification
Lumbar degenerative kyphoscoliosis has been variously classified based on the causes, pathology, imaging findings, and therapeutic policy, but there is no standard definition. Aebi4) classified spinal deformity with a Cobb angle ≥10° after bone maturation based on causes as the following: Type 1, lumbar degenerative scoliosis in adults (de novo); Type 2, residual congenital or idiopathic scoliosis; and Type 3, deformity caused by a lumbosacral spine lesion, lower extremity lesion, and osteoporosis. Toyama et al.5) defined lumbar degenerative scoliosis as lumbar intervertebral disk degeneration accompanying scoliosis with a Cobb angle ≥10°, and classified the disease based on X-ray findings into the following: Type I, compensated scoliosis of upper lumbar vertebrae with a sphenoidal L4/5 intervertebral disk as the main lesion and Type II, scoliosis caused mainly by scoliotic deformity accompanying multiple intervertebral disk degeneration in middle level lumbar vertebrae. In 2012, the Scoliosis Research Society proposed a classification of adult spinal deformity (SRS-Schwab classification)6) based on evaluation of PI-LL (PI: pelvic incidence, LL: lumbar lordosis), SVA (sagittal vertical axis), and PT (pelvic tilt) for sagittal plane alignment, in addition to scoliotic deformity of the coronal plane with a Cobb angle ≥30°. PI-LL ≤10°, SVA <40 mm, and PT <20° are defined as the normal values to maintain QOL (Fig. 1).
Figure 1.
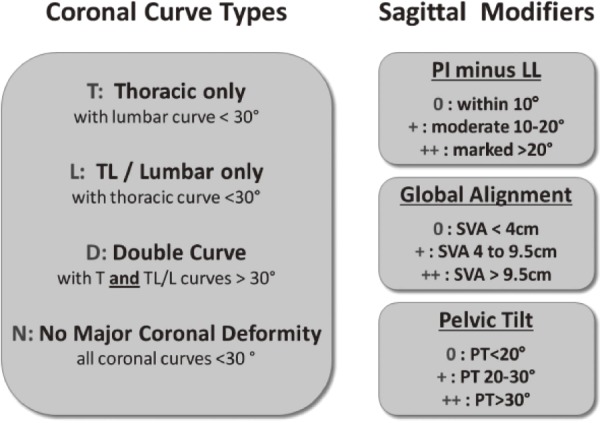
SRS-Schwab Adult Spinal Deformity Classification: A Validation Study based on evaluation of PI-LL (PI: pelvic incidence, LL: lumbar lordosis), SVA (sagittal vertical axis), and PT (pelvic tilt) for sagittal plane alignment, in addition to scoliotic deformity of the coronal plane with a Cobb angle ≥30°. PI-LL ≤10°, SVA <40 mm, and PT <20° were defined as the normal values to maintain quality of life (QOL).
Symptoms
Evaluation of symptoms caused by deformity
Symptoms of deformity generally develop with lumbar scoliosis of ≥30° or kyphoscoliosis deformity with loss of lumbar lordosis. The symptoms of spinal deformity include lumbar backache during postural maintenance, such as difficulty in standing due to severe lower back pain during work in a kitchen; intermittent claudication with low back pain, such as difficulty in walking due to severe lumbar and low back pain after 5-10 minutes of walking; and reflux esophagitis caused by abdominal compression due to kyphotic deformity.
Treatment strategy
In the planning of therapy, several groups of patients can be identified: those with kyphoscoliosis, in whom scoliotic deformity of ≥30° should be treated; those with stenosis with scoliotic deformity with main symptoms in nerve roots and cauda equine; and those with both diseases. Symptoms of adult spinal deformity are largely affected by kyphosis as deformity of the sagittal plane, rather than scoliosis as deformity of the coronal and sagittal alignment and imbalance. Thus, the surgical treatment target is selected with a focus on improvement of sagittal alignment and balance and correction of kyphosis, rather than correction of the scoliosis.
Conservative treatment should initially be performed as much as possible, including muscle exercise treatment, orthotic treatment, and drug therapy for pain control, but this may be ineffective for many patients with severe deformity, especially severe kyphotic deformity.
1. Muscle exercise treatment. This treatment is mainly for back muscle exercise. However, since many elderly patients have insufficient hip mobility, excursion training of the hip joint and muscle strengthening exercise for surrounding muscles are also important. Strengthening of muscles surrounding the pelvis will also assist the pelvis in anteversion.
2. Orthotic treatment. De novo spinal deformity mainly involves comparatively flexible kyphotic deformity in which use of a corrective brace for kyphosis may improve pain. This method is used to indicate surgical treatment in our department. Indication for surgical treatment is determined by observing improvement of pain after temporal immobilization with a cast.
3. Drug therapy. This is basically used as supportive treatment. Since osteoporosis is usually present, it is important to prepare for surgery while improving bone density.
In pain control, long-term administration of large amounts of anti-inflammatory analgesics or analgesic adjuvants and opioids should be avoided. Surgery should be considered instead and is indicated for a patient who does not want to undergo conservative treatment, who has severe stress, or who has drug-resistant reflux esophagitis accompanying kyphotic deformity. Corrective surgery for very elderly patients remains controversial, since elderly, thin, low weight patients with insufficient muscle strength and low reserve capacity cannot tolerate high level surgical invasion. We only perform corrective surgery for elderly patients with clear consciousness and lots of activity. The indication for surgical treatment should be determined by understanding the motivation of individual patients, severity of deformity, osteoporotic bone, risk of surgical invasion, cardiopulmonary function, and possibility of complications and should be discussed with an anesthetist. Low invasiveness treatment and step-by-step surgery for correction of deformity is a safer approach with less potential complications for elderly patients.
Required tests (Imaging diagnosis)
Plain X-ray
1. Lateral views in intermediate and forward/backward bending positions are most important because these enable evaluation of the slipping level and instability (slipping ≥3 mm, backward opening angle ≥15°).
2. In the frontal view, scoliosis and lateral slipping can be confirmed.
3. In an oblique view, spondylolysis can be confirmed.
4. For frontal and lateral views of the whole spine in a standing position: evaluation of alignment in this position is important, and the pelvic parameter has recently been considered to be especially important.
SVA: Sagittal vertical axis, PI: Pelvic incidence, PT: Pelvic tilt, SS: Sacral slope (Fig. 2).
Figure 2.
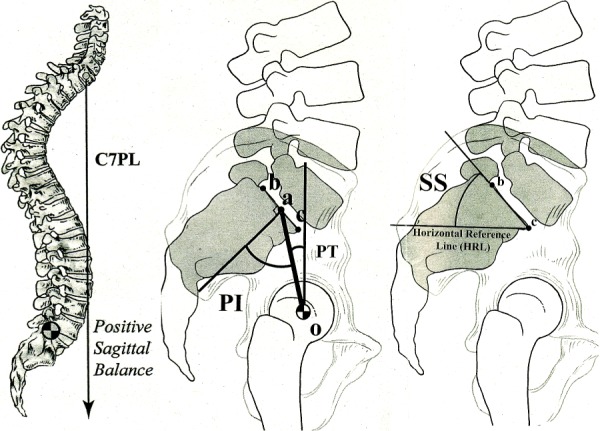
Hole spine alignment. SVA: Sagittal vertical axis, PI: Pelvic incidence, PT: Pelvic tilt, SS: Sacral slope. Spinal alignment based on frontal and lateral views of the hole spine in a standing position.
It is especially important to evaluate spinal alignment based on frontal and lateral views of the whole spine in a standing position.
Magnetic resonance imaging (MRI) is used in current treatment because it is noninvasive and provides a large amount of information, including the severity of necrosis and evaluation of intervertebral disk degeneration and aggravation of vertebral canal stenosis. In addition, oblique MRI can evaluate compression of the nerve root and angioplany in the intervertebral foramen, and MRI myelography can be used to visualize compression of the nerve root.
Computed tomography (CT) enables three-dimensional and stereoscopic evaluation using multiplanar reconstruction (MPR) of sagittal and coronal plane images, in contrast to conventional methods. An advantage over MRI includes the potential to evaluate bone conditions more correctly.
Surgical strategy
There have been many discussions of surgical policy, and various therapeutic methods are available. The outline of surgical policy for adult scoliosis in our department is as follows. Surgical algorithm for degenerative scoliosis (Table 1).
Table 1.
Surgical Algorithm for Degenerative Kyphoscoliosis.
| I | II | III | IV | V | |
|---|---|---|---|---|---|
| lower leg pain | + | + | + | + | + |
| low back pain | - | + | + | + | + |
| Instability | - | + | + | + | + |
| SVA ≥50mm | - | - | + | + | + |
| scoliosis ≥30° | - | - | + | ± | ± |
| kyphosis smooth | - | - | + | + | - |
| kyphosis sharp | - | - | - | - | + |
Level I: decompression
Level II: decompression+fusion
Level III: Ponte+(Rod rotation) or LLIF
Level IV: PSO
Level V: PVCR
Patients with deformity are classified based on their symptoms and deformity type to establish a surgical policy. Patients with neural symptoms of the lower extremity only are classified as Level I, for which only decompression is performed. Patients with low back pain and instability, in addition to neural symptoms, are classified as Level II, for which decompression with fusion is performed without correction. Patients with symptoms caused by deformity, such as abnormal posture, fatigue low back pain, intermittent claudication, scoliotic deformity ≥30°, smooth kyphosis, and sagittal imbalance with SVA ≥50 mm, are classified as Level III, for which Posterior column osteotomy (Ponte osteotomy) (usually for four intervertebral spaces: L2/L3, L3/L4, L4/L5, L5/S1) and rod rotation are performed for creating of lumbar lordosis. For patients with degenerative kyphoscoliosis, in which scoliotic deformity is accompanied by severe lumbar vertebra rotation (Level III), as suggested by Simmons et al.7), correction with rod rotation and multilevel posterior lumbar interbody fusion (PLIF) are performed. In recent years, other anterior correction and fusion methods, such as extreme lateral interbody fusion (LLIF), have also been used. In these methods, a large cage is used for correction of lumbar kyphosis and scoliotic deformity with an anterior approach. This enables correction and fusion for three intervertebral spaces (L2/L3, L3/L4, L4/L5) with low-invasive surgery with a small amount of bleeding (approx. 50 ml) and a comparatively short surgical time (approx. 90 min). Level IV includes patients with mild scoliotic deformity of ≤30° and mild and smooth kyphosis (round back), for which kyphotic correction is performed by pedicle subtraction osteotomy (PSO). Level V includes patients with mild scoliotic deformity of ≤30° and local kyphosis with severe vertebral deformity, such as compression fracture, for which correction and fusion are performed using vertebral column resection (VCR).
Regarding the range of correction and fusion for spinal kyphoscoliosis in cases of Level III or higher, the upper instrumented vertebra (UIV) will be the thoracic vertebra (usually the tenth thoracic vertebra or higher) reaching the rib cage beyond the apical vertebra of the kyphosis, and the lower instrumented vertebra (LIV) will be the pelvis, for which fusion is performed using iliac screws. Since some patients have hard deformity and a need for improvement of sagittal plane balance, osteotomy for vertebral body and intervertebral joint, such as Smith-Peterson osteotomy (SPO), PSO, and vertebral column resection (VCR), are required in many cases. For patients with wedge deformity of the vertebral body and severe kyphotic deformity, correction and fusion are performed concomitantly with vertebral body osteotomy, such as PSO and VCR. The Schwab osteotomy classification is used in selection of the osteotomy method. In this classification, osteotomy is anatomically classified into six levels based on the level of vertebral excision (Fig. 3).
Figure 3.
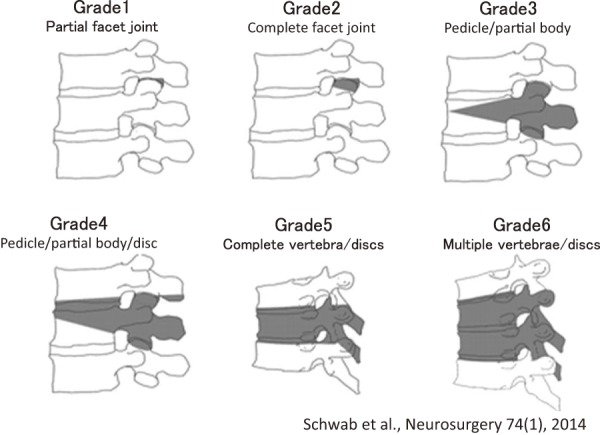
The Schwab osteotomy classification. Selection of the osteotomy method. In this classification, osteotomy is anatomically classified into six levels based on the level of vertebral excision.
Correction of target values
Criteria have been proposed of PI-LL ≤10° by Schwab et al.6) LL + PI + TK ≤45° by Rose et al.8) and the full balance integrated (FBI) technique and correction angle = angle of C7 translation (C7TA) + Femur obliquity angle (FOA) + Angle of pelvic tilt compensation (PTCA) by Le Huec et al.9) However, these are based on standard values for Caucasian patients, and it is unclear if they are appropriate for Japanese patients. In addition, when different surgical methods or ranges of fusion are used, adaptive criteria will be different. Thus, we suggest that postoperative alignment should be estimated based on the surgical method and policy of fusion range, using standard values for Japanese people. PI-LL ≤10° was initially targeted, but this criteria was not suitable in some Japanese cases. Thus, at present, PT and SVA are changed to meet target values in Japanese people, with LL corrected to 0.45×PI+31.8. The objectives of correction and fusion are an appropriate backward-leaning position of the pelvis and lumbar lordosis, which are defined by PI. A detailed explanation is omitted here, but we use values obtained using the Hamamatsu formula10), which was established based on data in volunteers. ideal PT=0.47×PI-7.5 ideal LL=0.45×PI+31.8
Range of fusion
Regarding the range of fusion, it is sufficient to perform correction and fusion only for the area of kyphotic deformity in a young patient showing compensation of the spine. Fusion reaching to the pelvis can often be avoided. However, for a patient with lumbar degenerative kyphosis with compensation in the pelvis and lower extremities, the UIV will be the thoracic vertebra (usually the tenth thoracic vertebra) reaching the rib cage beyond the apical vertebra of the kyphosis, and the LIV will be the pelvis (iliac bone). However, in a patient with severe kyphosis of thoracic vertebrae, compensation cannot be achieved when fusion is performed at the lower thoracic vertebra, and kyphosis occurs easily at the adjacent UIV. Thus, fusion is performed at upper thoracic vertebrae, T3-4. In many cases with severe kyphotic deformity of lumbar vertebrae, a thoracic vertebra may straighten or become lordotic due to a compensation function of the thoracic vertebra. The upper thoracic vertebra physiologically becomes kyphotic by performing fusion to T9 and T10.
For fusion at upper vertebrae, only a vertebral pedicle screw is used for lower thoracic vertebrae, while a hook and lamina wiring with high molecular weight polyethylene tape are added for fusion at UIV. When excessive corrective force is added to UIV, loosening of the screw and fracture of the costotransverse process of the vertebra caused by the hook may develop in osteoporotic patients. Therefore, we carefully perform rod contour and placement with mild kyphosis appropriate for the spinal alignment to avoid such excessive correction force at the edge.
Conflicts of Interest: The authors declare that there are no conflicts of interest.
References
- 1.Takemitsu Y, Harada Y, Iwahara T, et al. Lumbar degenerative kyphosis: Clinical, radiological and epidemiological studies. Spine. 1988; 13(11): 1317-26. [PubMed] [Google Scholar]
- 2.Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005; 30(6): 682-8. [DOI] [PubMed] [Google Scholar]
- 3.Schwab F, Lafage V, Shaffrey CI, et al. The Schwab-SRS adult spinal deformity classification: assessment and clinical correlations based on a prospective operative and non-operative cohort. Neurosurgery. 2012; 71(2): E556. [DOI] [PubMed] [Google Scholar]
- 4.Aebi M. The adult scoliosis. Eur Spine. 2005; J14(10): 925-48. [DOI] [PubMed] [Google Scholar]
- 5.Toyama Y. Spinal deformity and degenerative scoliosis. In: Toyama Y (ed): Lumbar Vertebra in Clinical Practice, Medical View Co., 210-5, 2001. [Google Scholar]
- 6.Schwab F, Ungar B, Blondel B, et al. Scoliosis research society―Schwab adult spinal deformity classification. Spine. 2012; 37(12): 1077-82. [DOI] [PubMed] [Google Scholar]
- 7.Simmons ED. Surgical treatment of patients with lumbar spinal stenosis with associated scoliosis. Clin Orthop Relat Res. 2001; 382: 153-61. [DOI] [PubMed] [Google Scholar]
- 8.Rose PS, Bridwell K, Lenke LG, et al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine. 2009; 34(8): 785-91. [DOI] [PubMed] [Google Scholar]
- 9.Le Huec JC, Leijssen P, Duarte M, et al. Thoracolumbar imbalance analysis for osteotomy planification using a new method: FBI technique. Eur Spine J. 2011; 20(5): 669-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yamato Y, Hasegawa T, Kobayashi S, et al. Calculation of the target lumbar lordosis angle for restoring an optimal pelvic tilt in elderly patients with adult spinal deformity. Spine. 2016; 41(4): E211-7. [DOI] [PubMed] [Google Scholar]


