Introduction
Purpura annularis telangiectodes of Majocchi (PATM) is a pigmented purpuric dermatosis (PPD) characterized by bluish-red annular patches with telangiectasia. Lesions often occur in young female patients and most often symmetrically involve the bilateral lower extremities.1 Here, we report a case of a PATM-like eruption presenting in a woman in her 60s after sclerotherapy for venous varicosities.
Case report
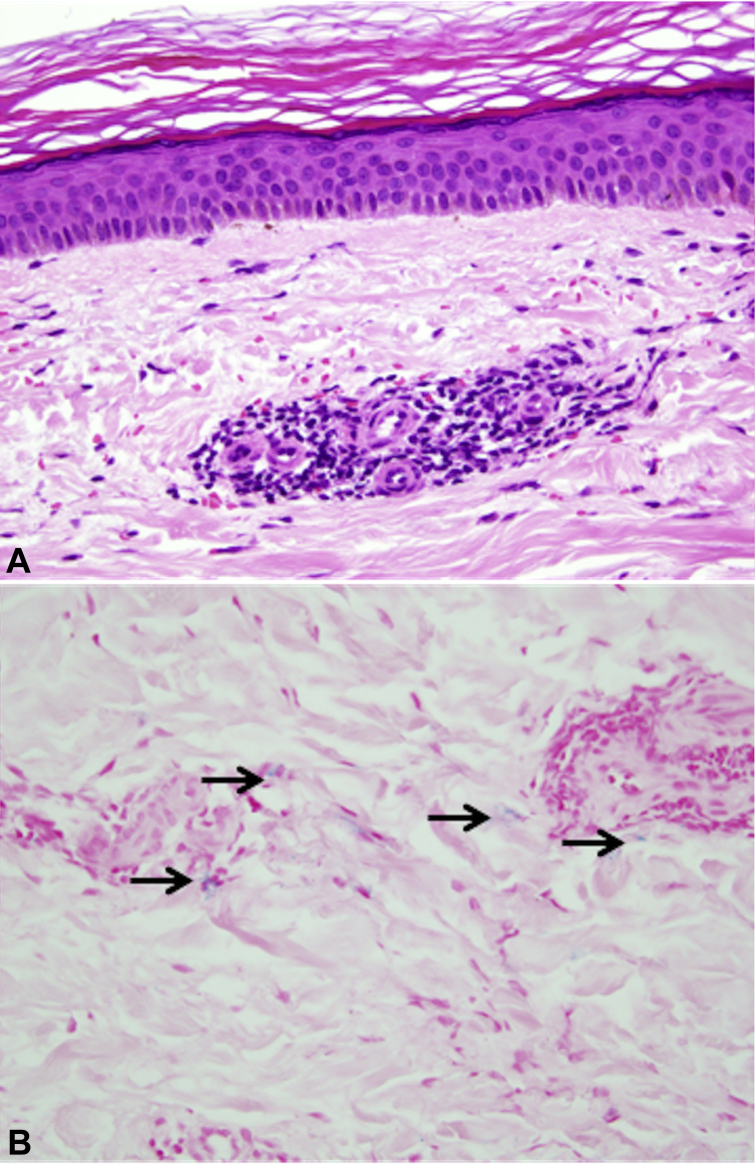
A 63-year-old white woman presented with a 1-month history of asymptomatic red-brown rings on her lower extremities (Fig 1). Six weeks before the development of lesions, she had been treated for venous reflux disease with sodium tetradecyl sulfate injections (2 sessions 2 weeks apart). The rings appeared 3 days after the injections, and she reported that they all developed at prior injection sites. Before presentation, she had been unsuccessfully treated with a course of clotrimazole/betamethasone diproprionate cream for initial concern of tinea. Examination showed numerous nonblanching annular to arcuate patches composed of confluent petechia with few telangiectasias involving the bilateral lower extremities. A punch biopsy was obtained, and the clinical differential diagnosis included PPD, postsclerotherapy hyperpigmentation, porokeratosis, granuloma annulare, and vasculitis. Histologic examination showed red blood cell extravasation with a perivascular lymphocytic infiltrate (Fig 2).
Fig 1.
Numerous nonblanching annular to arcuate petechial patches with few telangiectasias on the left lower extremity. The area of biopsy is circled.
Fig 2.
A, Punch biopsy sample (hematoxylin-eosin; original magnification, ×400). A normal epidermis overlies a perivascular lymphoid infiltrate and extravasated erythrocytes. B, Punch biopsy sample (Perl's iron stain, original magnification, ×400). Hemosiderophages in the superficial dermis (arrows).
Discussion
PATM is an uncommon form of PPD, and to our knowledge, there have been no prior reports of PPD occurring after sclerotherapy.
The etiology of the various types of PPD is unknown and likely multifactorial, with potential inciting agents/associated conditions including drugs, vascular fragility, hypertension, diabetes mellitus, and infections. PPDs have been reported to occur after administration of medications including nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, vitamins/supplements, analgesics, sedatives, chemotherapeutics, antihyperglycemics, antihypertensives, and isotretinoin.2 Although our patient was taking ibuprofen as needed in addition to a daily multivitamin, the temporal relationship and distribution of lesions at the sites of injection implicate sclerotherapy as the more likely cause of her eruption. Vascular irritation from the detergent used in the injections is a potential cause of this eruption. A possible additive role of previous topical therapy and use of an NSAID in the development of the eruption cannot be excluded.
Postsclerotherapy hyperpigmentation affects 10% to 30% of individuals after treatment and is thought to arise from direct endothelial damage with resultant red blood cell extravasation and hemosiderin deposition.3 Although postsclerotherapy hyperpigmentation was considered in this instance, the annular appearance and lack of hyperpigmentation after treatment make it less likely. Additionally, the presence of lymphocytic inflammation histologically would support a pigmented purpuric eruption as opposed to postsclerotherapy hyperpigmentation, which typically shows hemosiderosis without inflammation.
After receipt of the biopsy results, the patient was offered reassurance. Subsequent clinical evaluation showed gradual fading of lesions over the course of months, with minimal residual pigmentation. The patient has been offered pulsed dyed laser treatment for residual pigmentation but has currently deferred.
We report a case of an annular purpuric eruption showing clinical and histologic features of PATM developing after sclerotherapy for venous disease of the legs. Development of lesions directly at the site of previous injection supports injection-related trauma as the likely cause. Exacerbation of the reaction by NSAID and vitamin ingestion and topical antifungal/corticosteroid therapy cannot be excluded. We believe that recognition of this entity may prevent unnecessary treatment/workup for potential clinical mimickers, including infection and vasculitis.
Acknowledgments
We would like to thank Joseph Malters, MD, for his contribution of patient history and editorial review.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Sardana K., Sarkar R., Sehgal V.N. Pigmented purpuric dermatoses: an overview. Int J Dermatol. 2004;43:482–488. doi: 10.1111/j.1365-4632.2004.02213.x. [DOI] [PubMed] [Google Scholar]
- 2.Kaplan R., Meehan S.A., Leger M. A case of isotretinoin-induced purpura annularis telangiectodes of Majocchi and review of substance-induced pigmented purpuric dermatosis. JAMA Dermatol. 2014;150(2):182–184. doi: 10.1001/jamadermatol.2013.7371. [DOI] [PubMed] [Google Scholar]
- 3.Goldman M.P., Kaplan R.P., Duffy D.M. Postsclerotherapy hyperpigmentation: a histologic evaluation. J Dermatol Surg Oncol. 1987;13:547–550. doi: 10.1111/j.1524-4725.1987.tb00940.x. [DOI] [PubMed] [Google Scholar]