ABSTRACT
Background
Recent research suggests that sugar-sweetened beverage (SSB) consumption has been declining among US children aged 2–18 y. However, most studies focused on changes in mean intake, ignore high SSB consumers and do not examine intake among vulnerable groups and, including adolescents, low-income households, and several racial/ethnic minorities.
Objective
The aim was to estimate usual SSB intake from NHANES surveys from 2003–2004 to 2013–2014 to examine shifts at both the median and 90th percentile among US children, evaluating the extent to which intake disparities in total SSBs and subtypes have persisted.
Design
Children 2–18 y from NHANES 2003, 2005, 2007, 2009, 2011 and 2013. SSBs were all non-diet beverages sweetened with sugars including revising all beverages to as consumed status and excluding soy and dairy based beverages. The NCI usual intake method was used to estimate usual intake from two 24-hour recalls. A 2-part correlated model accounted for nonconsumers. Quantile regression was then used to examine differences in SSB usual intakes at the 50th and 90th percentiles by race-ethnicity, and examine interactions indicating whether racial-ethnic disparities in intake were modified by income.
Results
Despite considerable declines, children's SSB intake remains high, particularly among heavy consumers. Among adolescents, median SSB intake in 2013–2014 was on the order of 150–200 kcal/d, and heavy intake at the 90th percentile was on the order of 250–300 kcal/d. There were important disparities in intake that persisted over time. Although high household income was associated with lower SSB intake in non-Hispanic white (NHW) children, intakes of non-Hispanic black (NHB) and Mexican-American (MA) children from these households were similar to or higher than those from poor households. There were also large racial/ethnic differences in the types of SSBs consumed. The consumption of regular sodas by NHB children was somewhat lower than among MA and NHW children, whereas fruit drink intake was markedly higher.
Conclusions
Overall, these findings suggest that, despite recent declines, strategies are needed to further reduce SSB consumption, and particularly heavy intake, especially among NHB children where fruit drinks also are key source of SSBs.
Keywords: sugar-sweetened beverages, fruit drinks, racial/ethnic disparities, children, adolescents
Introduction
Sugar-sweetened beverages (SSBs) are a major contributor to energy intake in both adults and children in the United States (1–8). Numerous reviews suggest that SSB consumption—particularly when the amount of intake is high—contributes to weight gain and obesity as well as related cardiometabolic problems, the prevalence of which has increased in recent years, especially in disadvantaged population groups (9–18). Indeed, a number of studies have shown meaningful racial/ethnic and socioeconomic disparities in SSB intake (19, 20). Given evidence of adverse health effects, there is growing attention to strategies that aim to decrease SSB consumption in children (21–24).
Current studies have shown that, after an earlier increase, US children's mean energy intake from SSBs began to decline steeply in the early 2000s (1, 3, 4, 25–28). Similar trends have been shown for total added sugars, of which SSBs comprise approximately half (29). Despite this decline, however, at a mean of 14% of energy in 2011–2012, US children's added-sugars intake exceeded current guidelines, which recommend a limit of <10% of energy/d (30). Moreover, the understanding of these recent shifts in SSB consumption and their impact on the distribution of intake among vulnerable population groups is incomplete. First, because most studies have focused on mean intake, less is known about changes in heavy SSB intake (28, 29). The magnitude of decline among heavy consumers—those with the highest intakes most likely to contribute to weight gain and diabetes risk—has not been described to our knowledge. Second, disparities in intake shifts are poorly understood. Previous studies have documented disparities in children's SSB intake at varied cross-sections in time, with higher consumption among low socioeconomic status (SES) groups (1, 28). Nonetheless, studies have yet to examine to what extent declines in intake—particularly in heavy consumption—have occurred in racial/ethnic minorities and low-SES groups with a persistently high burden of childhood obesity (1, 28, 31). Studies on US obesity trends suggest that socioeconomic disparities in obesity have recently increased (32–34). Moreover, socioeconomic disparities in US obesity have been shown to vary by race/ethnicity and sex, with particularly marked racial/ethnic differences often apparent with higher SES (32). Studies on SSBs have yet to evaluate disparities in intake trends, particularly for heavy intake, in order to evaluate the extent to which declining trends in SSB consumption are reaching vulnerable groups.
The current study examines disparities in recent shifts in both heavy (90th percentile) and median usual SSB intakes among US children using NHANES dietary surveillance data collected between 2003–2004 and 2013–2014. Analyses improve on earlier research by utilizing techniques developed by the National Cancer Institute (NCI) to estimate the distribution of usual intake, incorporating up to 2 d rather than a single dietary recall (35–37). We examine the extent to which there may be SES disparities in intakes and trends across racial/ethnic groups. In addition, to inform future efforts to promote further changes in SSB consumption in vulnerable groups, trends in intake were examined for the major SSB subtypes, regular nondiet sodas and fruit drinks.
Methods
This analysis used dietary intake data from children aged 2 to 18 y from 6 cycles (2003–2004, 2005–2006, 2007–2008, 2009–2010, 2011–2012, and 2013–2014) of What We Eat in America, the dietary component of the NHANES surveys. Data from these waves utilized the USDA food-composition tables applying the same dietary intake assessment methods (38–48). The 2003–2004 survey was selected as the earliest wave for analysis because dietary assessment methods and food-composition tables differed in earlier waves of NHANES, and previous analyses of US children's SSB consumption incorporating earlier waves suggested that declines in intake began in 2003–2004 (1, 3). Dietary intakes were assessed by using ≤2 nonconsecutive days of 24-h dietary recalls administered with the use of the USDA's Automated Multiple-Pass Method (49). After the first recall, collected in-person by trained interviewers in the Mobile Examination Centers, the second recall was collected for most participants 3–10 d later by telephone. Recalls were completed by adult caregivers for preschoolers aged 2–5 y (“preschoolers”), by children assisted by caregivers for the 6- to 11-y school-age group (“school-aged children”), and on their own for the oldest age group, adolescents aged 12–18 y (“adolescents”). The terms “children” or “youth” are used interchangeably to refer to all participants aged 2–18 y rather than to specific age groups. Each wave of NHANES data was linked to the USDA's Food and Nutrient Database for Dietary Studies corresponding to that wave, reflecting foods available at the time of each survey. Protocols were approved by the National Center for Health Statistic's Institutional Review Board, and written informed consent was obtained from all participants.
Participants were excluded from analyses if data were missing for parental education (n = 648) or household income as a percentage of the federal poverty level (FPL; n = 1193). Diet recall reports were excluded if self-reported intake amount (more, same, or less than usual) was not reported (n = 52), energy intake was 0 kcal (n = 5), or energy intake was >4 SDs beyond individual estimated energy requirements (n = 179) and thus physiologically implausible as an estimate of habitual intake. Estimated energy requirement was calculated by sex and age according to equations provided by the Institute of Medicine's 2005 Dietary Reference Intakes (50), with SD values calculated to identify implausible dietary reports using the formula provided by Huang et al. (51) (see Supplementa l Figure 1). The formula accounts for variability in daily intakes and predicted requirements, as well as in estimated energy expenditure using doubly labeled water. Accelerometry data to assess physical activity levels (PALs) were available only for NHANES 2003–2006 (52). Therefore, SD bounds were estimated assuming sedentary PALs to identify implausibly low intake and very active PALs to identify likely overreporters. The final sample included 17,579 children over all 6 survey cycles, with a total of 32,914 diet recalls (87% of the sample had 2 recalls). The sociodemographic distribution of the sample is shown in detail in Supplemental Table 1. Because other groups were small and heterogeneous in composition, analyses of SSB intake among racial/ethnic groups focused only on Mexican Americans (MAs), non-Hispanic blacks (NHBs), and non-Hispanic whites (NHWs).
SSB definitions
SSBs were defined as all nonalcoholic, nondiet beverages sweetened with sugars of any type, either as purchased or added after purchase (53). Combination codes were used to identify beverages (kilocalories per day) sweetened by the consumer after purchase, such as powdered drink mixes or teas to which sugars were added during preparation, as well as juices combined with water and caloric sweeteners. This definition excluded soy, yogurt, or milk-based beverages, for which a large proportion of calories do not come from added sugars, as well as 100% fruit juices and vegetable juices, consistent with previous studies (1, 28). This exclusion included juice with added caloric sweeteners but no water or other ingredients, because this was reported very infrequently (e.g., n = 4 times in all youth aged 2–18 y in 2013–2014). Diet or low-calorie beverages were defined as beverages with ≤5 kcal/100 mL. Food codes and descriptors were used to classify SSBs into 3 subtypes as regular sodas (i.e., sweetened carbonated beverages), fruit drinks (i.e., noncarbonated beverages containing fruit juices or flavors, excluding fruit-flavored regular soda), and other SSBs (including sports drinks, energy drinks, and sweetened teas or coffees), as detailed in Supplemental Table 2. Although we describe trends, we did not analyze intake disparities for “other SSBs” in detail due to methodologic concerns related to sparse sample size (see Discussion).
Statistical analyses
The NCI has developed a statistical method that uses information from multiple 24-h recalls to estimate the distribution of usual intake of nutrients or episodically consumed foods (36, 37, 54). We used the NCI method to estimate empirically the distribution (means and percentiles) of SSB usual intake in children using What We Eat in America–NHANES. The NCI method allows 1) estimating the within- and between-person variance components and correcting for the high intraindividual variation intrinsic to 24-h recalls and 2) adjusting for important covariates, which helps improve the estimates by explaining the variability (e.g., intake differences due to recall sequence, or weekend consumption). A 2-part correlated model was utilized due to skewed distributions with large proportions of nonconsumers (55, 56). Specifically, the 2-part nonlinear mixed model on SSBs (kilocalories per day) for repeated 24-h recalls was fit by using the NCI MIXTRAN macro (36, 57). Part 1 of the model estimates the probability of SSB consumption including a person-specific random effect, and part 2 estimates the amount of SSBs in kilocalories per day consumed with the use of a nonlinear Box-Cox transformation on the original scale also including a person-specific effect. The Box-Cox exponential power parameter and the covariate effects are estimated at the same time during the model fitting so that the best transformation is chosen after adjusting for these covariates. Parts 1 and 2 are linked by allowing the 2 person-specific random effects to be correlated, accounting for the association between probability of consumption and amount (i.e., individuals who consume SSBs most frequently tend to consume more SSB kilocalories per day).
Covariates included in the model were NHANES cycle year, age group (2–5, 6–11, or 12–18 y), sex, race/ethnicity (NHW, NHB, MA, other Hispanic, other/mixed race), parental education (defined as less than, equal to, or more than a high school education), and per capita household income as a percentage of the FPL, weekend (including Friday), as well as season of data collection (“November–April” or “May–October”), self-reported intake amount (more, same, or less than usual), and recall sequence (first or second). Income was defined as low for households at <185% of the FPL (the criterion used to define eligibility for the Special Supplemental Nutrition Program for Women, Infants, and Children and for reduced-price school meals), medium for those between 185% and 400% of the FPL, and high for those at ≥400% of the FPL. An a priori interest was racial/ethnic intake disparities in intake over time. Therefore, the model included 2-way interactions between race/ethnicity and all other covariates (survey year, age group, household income, parental education, and child sex), allowing the relation between usual SSB intake and the main covariates to vary by race/ethnicity. In addition, 2-way interactions between all covariates and both survey year and age group were also included to allow estimated intakes for each age group in each wave to vary by SES and sex. Regression coefficients from this model are provided in Supplemental Table 3 (NCI model). Because NHANES uses a complex, multistage probability design, variance estimation was carried out via the Balanced Repeated Replication technique and Fay coefficient of 0.3 (58).
The primary aim of this study was to estimate how race/ethnicity was associated with heavy and median SSB intake, rather than only with mean intake, from 2003–2004 to 2013–2014. Quantile regression (59, 60) was used to test whether shifts over time in usual SSB intake at the 50th and 90th quantiles differed by race/ethnicity, and to examine the magnitude of overall disparities in intake. Specifically, usual SSB intake (kilocalories per day) was predicted for each individual with the NCI INDIVINT macro using previously estimated parameters from the 2-part nonlinear mixed model on SSBs for repeated 24-h recalls. Thus, estimates of the association are based on the predicted usual intake distribution and not based on a single-day observation. Quantile regression was then used to examine the significance of differences in SSB usual intakes at the 50th and 90th percentiles by race/ethnicity, and to examine interactions indicating whether racial/ethnic disparities in intake were modified by SES. In addition to coefficients from the quantile regression models, predicted marginals were obtained from the quantile regression to show the size of the effects, using models that included significant pairwise interaction terms. These data are presented as Figures 1–3 shown in the main text for adole-scents, and in Supplemental Figures S2-S3 for younger age groups. Predicted intakes at the 50th and 90th percentiles in the simulated predicted intake distribution were also obtained for comparison indicating similar results; thus, the data are not shown. Analyses accounted for the complex survey design and sampling weights (dietary recall weights for day 1) using SAS version 9.3 software (SAS Institute), and the qreg2 command in Stata version 14.2 (StataCorp) to perform quantile regression with robust and clustered SEs.
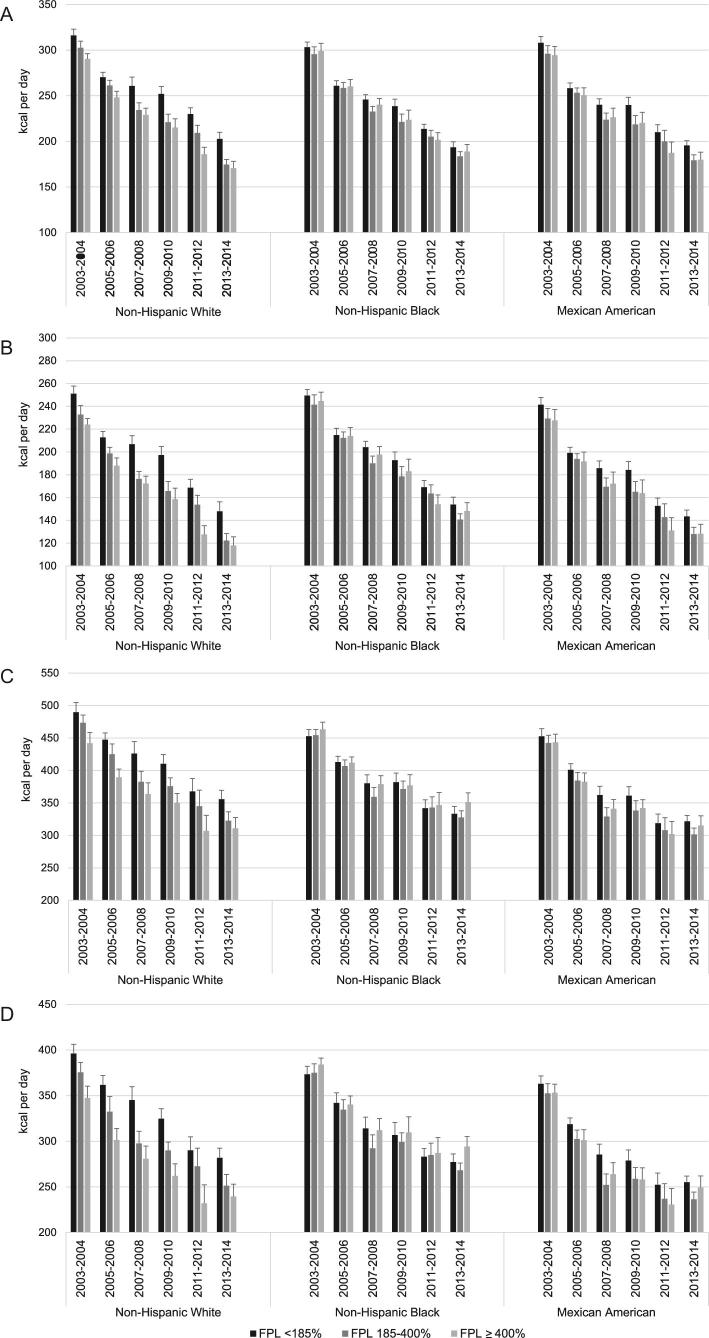
FIGURE 1.
Total SSB intake by race/ethnicity and household income as a percentage of poverty in participants aged 12–18 y (usual intake quantile regression results). Total SSB intakes of males aged 12–18 y (50th percentile) (A), females aged 12–18 y (50th percentile) (B), males aged 12–18 y (90th percentile) (C), and females aged 12–18 y (90th percentile) (D). Values are predicted intakes from multivariable-adjusted quantile regression (for details, see Supplemental Table 4), which found significant (*P < 0.05, †P < 0.01, ‡P < 0.001) associations with the following. Panels A and B—50th percentile, total SSBs: 1) main effects: NHB*, 12–18 y‡, male sex‡, survey wave 2013–14‡; 2) survey wave interactions: male × 2007–2008*, 2009–2010*, and 2013–2014†; 12–18 y × 2005–2006†, 2007–2008†, 2009–2010†, 2011–2012‡, and 2013–14‡; 3) other interactions: male × 12–18 y†, NHB × male†, MA × 12–18 y†, NHB × 12–18 y†. Panels C and D—90th percentile, total SSBs: 1) main effects: 12–18 y‡; male sex‡, income >400% FPL*; survey waves 2007–2008†, 2009–2010*, 2011–2012*, and 2013–2014‡; 2) income interactions: MA × >400% FPL*, NHB × >400% FPL†, NHB × <185% FPL*; 3) survey wave interactions: male × 2011–2012* and 2013–2014†; 12–18 y × 2007–2008*, 2009–2010†, 2011–12‡, and 2013–14‡; 4) other interactions: 12–18 y × male‡, NHB × male*, MA × 12–18 y†. FPL, federal poverty level; MA, Mexican American; NHB, non-Hispanic black; SSB, sugar-sweetened beverage.
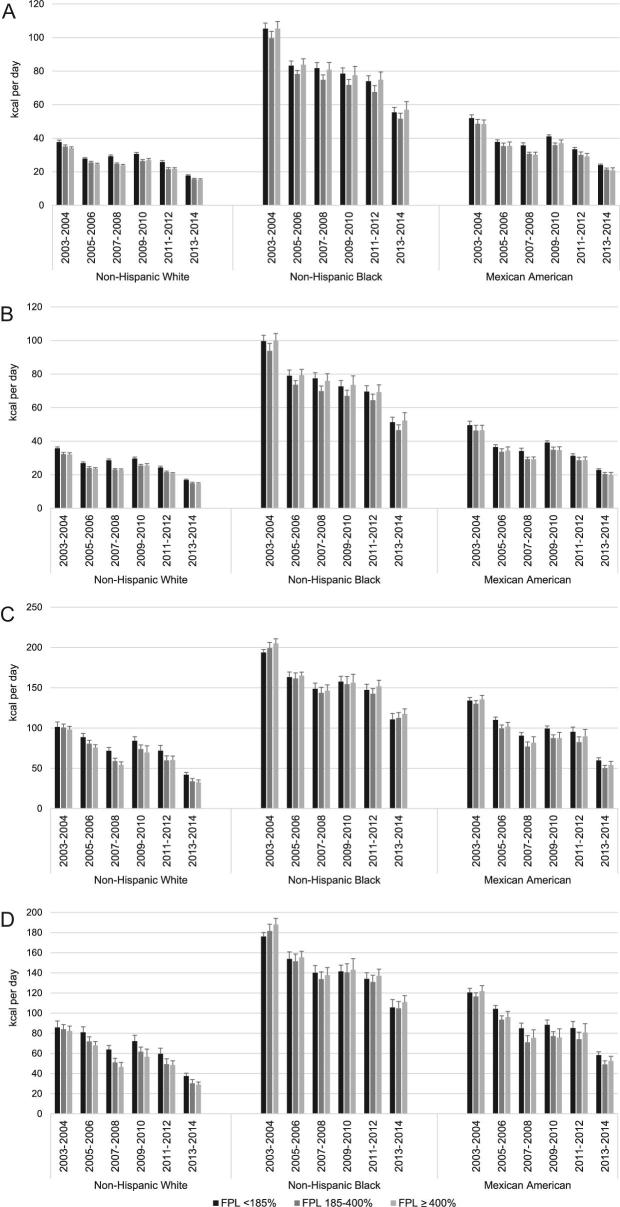
FIGURE 3.
Regular soda intake by race/ethnicity and household income as a percentage of poverty in participants aged 12–18 y (usual intake quantile regression results). Regular soda intakes of males aged 12–18 y (50th percentile) (A), females aged 12–18 y (50th percentile) (B), males aged 12–18 y (90th percentile) (C), and females aged 12–18 y (90th percentile) (D). Values are predicted intakes from multivariable-adjusted quantile regression (for details, see Supplemental Table 4), which found significant (*P < 0.05, †P < 0.01, ‡P < 0.001) associations with the following. Panels A and B—50th percentile, regular soda: 1) main effects: NHB‡; 12–18 y‡; male sex‡; income >400% FPL*; survey waves 2005–2006‡, 2007–2008*, 2009–2010‡, 2011–2012‡, and 2013–2014‡; 2) survey wave interactions: male × 2005–2006*, 2007–2008*, 2009–2010†, 2011–2012†, and 2013–2014‡; 12–18 y × 2005–2006‡, 2007–2008‡, 2009–2010‡, 2011–2012‡, and 2013–2014‡; 3) other interactions: male × 12–18 y‡, NHB × male‡, NHB × 12–18 y‡. Panels C and D—90th percentile, regular soda: 1) main effects: NHB‡; 12–18 y‡; male sex‡, income >400% FPL†; survey waves 2005–2006†, 2007–2008†, 2009–2010‡, 2011–2012‡, and 2013–2014‡; 2) income interactions: MA × income >400% FPL*, NHB × income >400% FPL†; 3) survey wave interactions: NHB × 2009–2010*, 2011–2012†, 2013–2014‡; 12–18 y × 2005–2006†, 2007–2008‡, 2009–2010‡, 2011–2012‡, and 2013–2014‡; 4) other interactions: 12–18 y × male‡, NHB × male‡, MA × 12–18 y†, NHB × 12–18 y‡. FPL, federal poverty level; MA, Mexican American; NHB, non-Hispanic black.
Results
Coefficients for associations between estimated usual SSB intake and survey years, age group, sex, race/ethnicity, and income from quantile regression models are shown in Supplemental Table 4. On the basis of these models, adjusted SSB usual intake quantiles (median and 90th percentile) by sex, income, and race/ethnicity over time are shown for adolescents (12–18 y) in Figure 1, for school-aged children (6–11 y) in Supplemental Figure 1, and for preschoolers (2–5 y) in Supplemental Figure 2.
Heavy (90th percentile) compared with median SSB intake
Patterns and trends in usual SSB intake were generally similar at the median and 90th percentile (e.g., see Figure 1 among adolescents). However, intakes were considerably higher among the heavy consumers at the 90th percentile than at the median. In quantile regression models shown in Supplemental Table 4, the intercept ± SE representing baseline SSB intake in kilocalories per day in 2003–2004 was 76.3 ± 8.4 (P < 0.001) at the median, with intakes approximately twice as high (160.1 ± 13.2; P < 0.001) at the 90th percentile.
Disparities in total SSB intake
Overall, multivariable-adjusted associations between SSB intake and NHB or MA race/ethnicity, relative to NHW children, were small and largely nonsignificant (see Supplemental Table 4). The adjusted difference in intake between NHB and NHW youth was 16.9 ± 8.1 kcal/d (P < 0.05) at the 50th percentile and 9.8 ± 15.1 kcal/d (P = NS) at the 90th percentile. For MA compared with NHW youth, these differences were −1.1 ± 9.4 (NS) and −7.2 ± 13.9 (NS) kcal at the 50th and 90th percentiles, respectively. Declines in intake over time were similar across racial/ethnic groups (NHB and MA × survey year interactions were consistently small and NS; see Supplemental Table 4). Unlike the small main effects of race/ethnicity, in the NHW referent group higher household income was associated with a larger and significant reduction in heavy SSB intake (β ± SE for the association with higher compared with moderate income at the 90th percentile: −26.4 ± 13.4; P < 0.05). Moreover, there were interactions indicating that the income disparity in SSB intake varied by race/ethnicity. In contrast to NHW youth, among NHB and MA children, higher income was associated with increases in heavy SSB intake (at the 90th percentile—higher income × NHB interaction: 35.6 ± 11.9; P < 0.01; higher income × MA: 27.7 ± 11.3; P < 0.05). Income associations did not reach significance for median intake (−6.0 ± 7.7; NS for higher compared with moderate income), nor did race/ethnicity × income interactions (see Supplemental Table 4).
Older age [β ± SE for 12–18 y compared with preschoolers: 165.3 ± 5.4 (P < 0.001) and 225.8 ± 11.4 (P < 0.001) at the 50th and 90th percentiles] and male sex [β ± SE compared with females: 25.4 ± 5.1 (P < 0.001) and 46.2 ± 9.8 (P < 0.001) at the 50th and 90th percentiles] were also associated with higher SSB intake. Declines over time also varied by age and sex, with larger reductions in the older groups and among male children who had initially higher intakes (P < 0.05 for most sex and age group × survey year interactions; see Supplemental Table 4).
Disparities in usual intake for total SSBs over time: adolescents (12–18 y)
At the 50th percentile (Figure 1A, B for males and females, respectively), total SSB usual intake in adolescents declined significantly over time (P < 0.001 for each survey year). The net decline in median intake between 2003–2004 and 2013–2014 was on the order of 100 kcal/d. Despite this reduction, median intake in 2013–2014 remained high, on the order of 200 kcal/d among low-income NHW and MA adolescent males and across all income groups for NHB males (Figure 1A). Patterns and trends in usual intake at the 90th percentile were generally similar to those at the median. However, as expected, the magnitude of intake was considerably higher (Figure 1C, D), exceeding 400 kcal/d in 2003–2004 and remaining well above 300 kcal/d in 2013–2014 among adolescent males (Figure 1C). As shown (Figure 1A compared with Figure 1C for adolescent males; Figure 1B compared with Figure 1D for females), large differences in SSB intakes of heavy compared with median consumers—on the order of ˜100 kcal/d among adolescents—persisted over time.
The racial/ethnic disparity in the relation between SES and total SSB intake was especially marked at the 90th percentile. Although the amounts of heavy SSB intake were highest among NHW children from lower-income households during the entire period, among NHB adolescents heavy intake was often highest among those from the high-income households. Heavy SSB intake was generally similar among MA adolescents from low- and high-income households, with the lowest intakes associated with moderate income.
Disparities in total SSB usual intake: younger children (2–11 y)
As expected, SSB usual intakes in younger children were significantly lower than those in adolescents, by ˜88 kcal/d for school-aged children aged 6–11 y and 165 kcal/d for preschoolers aged 2–5 y (P < 0.05) at the median (Supplemental Table 4). Patterns and trends of disparity in intake for school-aged (Supplemental Figure 2) and preschool (Supplemental Figure 3) children resembled those seen among adolescents in terms of race, sex, and income.
Disparities in SSB usual intake by beverage type
Fruit drink usual intake
Overall, fruit drink consumption was the dominant source of SSBs among NHB children but not among NHW children [NHBs—β ± SE for fruit drinks: 50.4 ± 5.5 (P < 0.001) and 64.2 ± 7.8 (P < 0.001) at the 50th and 90th percentiles; Supplemental Table 4], contrasting sharply with the weak associations for total SSBs. MA ethnicity was also associated with significantly higher fruit drink intakes compared with those of NHW children, although intake differences were smaller [13.4 ± 2.6 (P < 0.001) and 16.5 ± 5.5 (P < 0.001) at the 50th and 90th percentiles, respectively].
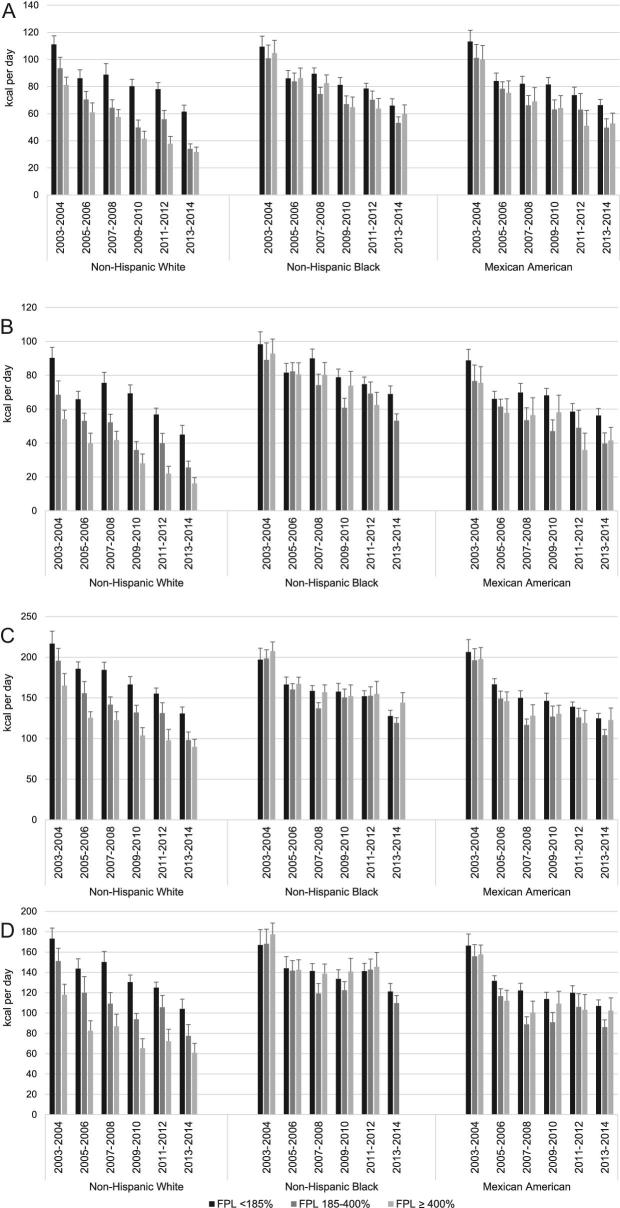
As shown for adolescents in Figure 2, patterns and trends in fruit drink usual intake were similar at the 50th and 90th percentiles. As for total SSBs, usual intakes were higher in males than in females. Despite greater declines over time in fruit drink intake among NHBs than whites (P < 0.05 for NHB × survey year interactions for most periods; see Supplemental Table 4), intakes of this type of beverage remained considerably higher in NHBs than other racial/ethnic groups, as shown in Figure 2. In 2013–2014, median and heavy intakes of fruit drinks in NHB adolescent males remained on the order of 50 and 100 kcal/d, respectively, more than twice as high (20 and 40 kcal/d) as intakes reported by NHW males in this age group (Figures 2A, C). With regard to total SSBs, there were racial/ethnic differences in the relation between household income and intake, but these disparities were much less marked for fruit drinks (NHB and MA × income interactions: NS).
FIGURE 2.
Fruit drink intake by race/ethnicity and household income as a percentage of poverty in participants aged 12–18 y (usual intake quantile regression results). Fruit drink intakes of males aged 12–18 y (50th percentile) (A), females aged 12–18 y (B) (50th percentile), males aged 12–18 y (90th percentile) (C), and females aged 12–18 y (90th percentile) (D). Values are predicted intakes from multivariable-adjusted quantile regression (for details, see Supplemental Table 4), which found significant (*P < 0.05, †P < 0.01, ‡P < 0.001) associations with the following. Panels A and B—50th percentile, fruit drinks: 1) main effects: NHB*; male sex*; survey waves 2005–2006†, 2007–2008†, 2009–2010*, 2011–2012†, 2013–2014‡; 2) income interactions: NHB × income >400% FPL*; 3) survey wave interactions: NHB × 2005–2006†, 2007–2008‡, 2009–2010‡, 2011–2012‡, and 2013–2014‡; MA × 2007–2008†, 2011–2012†, and 2013–2014‡; 4) other interactions: male × 12–18 y†, NHB × male†, NHB × 12–18 y†. Panels C and D—90th percentile, fruit drinks: 1) main effects: NHB‡, MA†; male sex‡; survey waves 2005–2006*, 2007–2008‡, 2011–2012‡, and 2013–2014‡; 2) income interactions: income ≤185% FPL × 2007–2008*, MA × >400% FPL*, NHB × >400% FPL†, NHB × <185% FPL*; 3) survey wave interactions: male × 2013–2014†; NHB × 2005–2006*, 2009–2010*, 2012–2012*, 2013–2014†; MA × 2009–2010‡ and 2013–2014‡; 4) other interactions: NHB × 12–18 y‡, MA × 12–18 y‡. FPL, federal poverty level; MA, Mexican American; NHB, non-Hispanic black.
Regular soda usual intake
In contrast to fruit drinks, overall, usual intakes of regular soda were highest in NHW and MA children, with considerably lower intakes among NHB children [overall differences in kcal/d compared with NHWs at the 50th and 90th percentiles: −11.4 ± 4.7 (NS) and −3.8 ± 8.6 (NS) for MAs; −21.7 ± 4.4 (P < 0.001) and −31.6 ± 8.8 (P < 0.001) for NHBs; Supplemental Table 4]. Like total SSB intake, the intake of regular soda was lower in higher income households, particularly for heavy intake [β ± SE at the 50th and 90th percentiles: −8.5 ± 4.1 (P < 0.05) and −21.3 ± 7.8 (P < 0.01)]. As for total SSBs, this income disparity in heavy intake—albeit not in median intake—varied by racial/ethnic group. For heavy consumers, the markedly higher intake of regular soda seen among white children from lower compared with higher income households was not apparent among NHB and MA children [high income × NHB: 17.2 ± 5.8 (P < 0.01); high income and MA: 17.9 ± 9.1 (P < 0.05) at the 90th percentile; interactions were weak and NS at the median].
Intake patterns for regular soda are shown for adolescents in Figure 3. Despite substantial declines, the median intake of regular soda remained high in 2013–2014, on the order of 100 kcal/d at the median for NHW and MA adolescent males and 200 kcal/d for heavy consumers. Although regular soda intakes remained markedly lower in NHB than in NHW and MA adolescents, beginning in 2009–2010 there were smaller declines over time in intakes at the 90th percentile among NHBs compared with whites (P < 0.05 for NHBs × survey year from 2009–2010 onward), suggesting that the temporal decline in heavy intake has slowed in NHB youth.
Discussion
SSBs have been linked to increased childhood obesity and excessive weight gain in an array of randomized controlled trials and longitudinal cohort research (9, 61) and are thought to be particularly important in the vulnerable racial/ethnic and socioeconomic groups in whom high levels of obesity persist (20). This analysis aimed to improve the understanding of disparities in usual intake trends in these vulnerable groups. In order to evaluate heavy usual intake, we examined disparities and trends in intake at the 90th percentile in addition to the median. Because most studies on trends in SSB intake have examined declines in mean intake, changes in intake among children with the highest amounts of SSB consumption—most likely to contribute to obesity risk—are understudied (28). The extent to which heavy intakes of SSBs may be more likely to persist among vulnerable population groups is therefore unknown. This study is unique in its use of usual intake methods to examine trends in usual intake that account for both the probability of consumption and the amount consumed, appropriate for episodically consumed beverages such as SSBs. This approach allows us to fully utilize both days of data when available to create a more statistically robust estimate of usual SSB consumption at both the median and 90th percentile.
With the use of data from NHANES surveys starting in 2003–2004, we found that children's daily usual intake of SSBs, at both the median and the 90th percentile, declined in each wave through 2013–2014. However, despite a considerable decline—on the order of 100 kcal/d in adolescents—usual intakes remained high, particularly among heavy consumers. In 2013–2014, the median intake of total SSBs was on the order of 150 kcal/d among adolescents, 100 kcal/d among 6- to 11-y-olds, and 75 kcal/d in children aged 2–5 y. The 90th percentile remained >300 kcal/d among adolescent males, >250 kcal/d among adolescent females, and on the order of 100 and 200 kcal/d among children aged 2–5 and 6–11 y, respectively.
There were important disparities in SSB intake, with considerably higher usual intakes in several vulnerable groups, including adolescents and children from lower-income households. Interestingly, racial/ethnic disparities in total SSB intake varied by income group. A strong income gradient in SSB usual intake was apparent among NHW children and to a lesser extent among MAs, but SSB usual intake among NHB children was similarly high across households of diverse income levels. As a result, although overall SSB usual intakes were somewhat higher among NHB than NHW and MA children at both the median and 90th percentile, among low-income households, SSB usual intake was highest among NHW children. These results suggest that it may be important to ensure that strategies to reduce heavy consumption of SSBs among children adequately reach socioeconomically diverse NHB children as well as lower-income households (62).
The usual intake of SSBs across different racial/ethnic groups was also disproportionate by beverage type. The high amount of total SSB intake in NHB children was attributable to the markedly greater consumption of fruit drinks in this racial/ethnic group compared with both NHW and MA children. Compared with NHWs, in 2003–2004, fruit drink usual intakes among NHB adolescent males from households of varied income were 65–70 kcal higher at the median and 92–107 kcal higher at the 90th percentile. These disparities declined but remained considerable in 2013–2014 (differences of 36–42 kcal/d at the median and 69–85 kcal/d at the 90th percentile). Thus, although intakes of fruit drinks and regular soda among NHB adolescent males at the 90th percentile of usual intake were comparable (˜100–150 kcal/d in 2013–2014), the 90th percentile of usual intake among NHWs and MAs was ∼4 times that for regular soda compared with fruit drinks (∼200 compared with ∼50 kcal/d). An earlier study on SSB usual intakes that analyzed NHANES data through 2007–2008 (28) reported higher fruit drink consumption associated with the NHB racial/ethnic group. However, this pronounced racial/ethnic disparity in SSB type has not been highlighted in more recent studies on SSB trends. Results suggest that, particularly among NHB children, it is critical that strategies to promote further reductions in SSB intake focus on fruit drinks as well as sodas.
We did not evaluate population subgroup disparities in other SSBs due to the low prevalence of intake and the likelihood of high within-person variability for this subtype, which makes it uncertain to what extent subgroup estimates are valid and reliable. Recent studies show that for foods with never- or nonconsumers on the order of 30–40%, the usual intake distribution may be estimated poorly, particularly at extremes such as the 90th percentile (63). However, as noted in previous reports analyzing all youth aged 2–19 y (1), NHANES data suggest that children's intake of other SSBs besides fruit drinks and regular sodas has been increasing. In 2003–2004 and 2013–2014, respectively, among boys, the prevalences of other SSB intake were as follows—2–5 y: 17.8% and 30.0%; 6–11 y: 31.4% and 35.9%; and 12–18 y: 39.4% and 48.4%. In girls, the prevalences were as follows—2–5 y: 19.0% and 23.0%; 6–11 y: 28.6% and 35.5%; and 12–18 y: 33.8% and 49.7%, respectively.
Other research has shown a decline in the proportion of added sugar in children's diets coming from beverages (26, 29, 64, 65) and research has accumulated to show that both added sugars in food and beverages adversely affect health (12, 66, 67). Because of the high concentrations of added sugar in beverages and lack of energy compensation when consuming an SSB, the adverse health impact of added sugar from beverages might be greater than from food (12, 66, 68, 69). These results, which show the persistence of elevated intake of SSBs in population subgroups in whom high levels of obesity persist, highlight that significant shifts in the US culture of drinking must continue to address the continued excessive intakes of added sugars from SSBs.
This research represents an improvement in estimates of SSB intake by using the NCI method based on a 2-step NCI model of ever consuming and then conditional on any consumption, estimation of the amount consumed. However, the trends and patterns shown are not significantly different from those of the studies that used 1 d of intake (28). Another important strength was the focus on patterns and trends in heavy intake, which is more likely to pose a threat to health, rather than examining only mean or median intake. The use of the NCI method aimed to improve the reliability of estimates of intake near the upper tail of the distribution, as well as for estimating intake of an episodically consumed beverage (70). In addition, by examining variability in how SES relates to intake patterns within racial/ethnic groups, rather than examining these variables separately, we provide greater insights for appropriately targeting policies and programs aiming to reduce the disparities that persist in children's SSB intake. However, challenges common to self-reported dietary intake, such as misreporting of foods and beverages perceived as less healthy, and the moderate sample size remain limitations of this analysis.
Overall, these results point to promising trends; nonetheless, levels at the 90th percentile remain high. There is still a need for vigilance given the continued promotion and marketing of SSBs to vulnerable groups including children and racial/ethnic minorities (62, 71, 72), as well as further assessment of the effectiveness of policies and programs to reduce intake (21, 23, 24, 73, 74). Public policies such as the SSB tax in Philadelphia, Berkeley, Chicago, San Francisco, and Oakland require careful evaluation for their impact (75). The positive results found in Mexico with its SSB tax (76, 77) and activities underway in an array of other countries to reduce SSB intake (78) provide ample opportunity for the United States to gain insights on public policies used elsewhere to reduce the consumption of this one component for diet for which no clear nutritional benefits and clear adverse effects on health exist, particularly for children who are the most vulnerable to adapting life-long dietary behaviors.
Supplementary Material
Acknowledgements
We thank Phil Bardsley for organization of the beverage intake measures; Victor Kipnis, NCI, for assistance with the statistical programming; Frances Burton for administrative assistance; and Denise Ammons for graphics support.
The authors’ responsibilities were as follows—MAM, JMP, and BMP: design; MAM, DRM, and DS-A: statistical development; MAM: initial write-up of results; MAM, DRM, JMP, DS-A, and BMP: writing of the manuscript and overall review; MAM, JMP, and BMP: discussion; and all authors: read and approved the final manuscript. None of the authors had a conflict of interest of any type with respect to this article.
Notes
Supported by the Robert Wood Johnson Foundation (grant 70017), the NIH (R01DK098072 and DK056350), and the CPC (P2C HD050924).
Supplemental Figures 1–3 and Supplemental Tables 1–4 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/ajcn/.
Abbreviations used: FPL, federal poverty level; MA, Mexican American; NCI, National Cancer Institute; NHB, non-Hispanic black; PAL, physical activity level; SES, socioeconomic status; SSB, sugar-sweetened beverage.
References
- 1. Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am J Clin Nutr 2013;98(1):180–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Reedy J, Krebs-Smith SM. Dietary sources of energy, solid fats, and added sugars among children and adolescents in the United States. J Am Diet Assoc 2010;110(10):1477–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mesirow MS, Welsh JA. Changing beverage consumption patterns have resulted in fewer liquid calories in the diets of US children: National Health and Nutrition Examination Survey 2001–2010. J Acad Nutr Diet 2015;115(4):559–66, e4. [DOI] [PubMed] [Google Scholar]
- 4. Slining MM, Mathias KC, Popkin BM. Trends in food and beverage sources among US children and adolescents: 1989–2010. J Acad Nutr Diet 2013;113(12):1683–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ng SW, Ostrowski JD, Li KP. Trends in added sugars from packaged beverages available and purchased by US households, 2007–2012. Am J Clin Nutr 2017;106(1):179–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Miller G, Merlo C, Demissie Z, Sliwa S, Park S. Trends in beverage consumption among high school students—United States, 2007–2015. MMWR Morb Mortal Wkly Rep 2017;66(4):112–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Miles G, Siega-Riz AM. Trends in food and beverage consumption among infants and toddlers: 2005–2012. Pediatrics 2017;139(6):e20163290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dunford EK, Popkin BM. 37 Year snacking trends for US children 1977–2014. Pediatr Obes 2017;13(4):247–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev 2013;14(8):606–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bucher Della Torre S, Keller A, Laure Depeyre J, Kruseman M. Sugar-sweetened beverages and obesity risk in children and adolescents: a systematic analysis on how methodological quality may influence conclusions. J Acad Nutr Diet 2015;116(4):638–59. [DOI] [PubMed] [Google Scholar]
- 11. Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health 2007;97(4):667–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Te Morenga L, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. Br Med J 2013;346:e7492. [DOI] [PubMed] [Google Scholar]
- 13. Pan A, Malik VS, Hao T, Willett WC, Mozaffarian D, Hu FB. Changes in water and beverage intake and long-term weight changes: results from three prospective cohort studies. Int J Obes (Lond) 2013;37(10):1378–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Malik VS. Sugar sweetened beverages and cardiometabolic health. Curr Opin Cardiol 2017;32(5):572–9. [DOI] [PubMed] [Google Scholar]
- 15. Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care 2010;33(11):2477–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dabelea D, Mayer-Davis EJ, Saydah S, Imperatore G, Linder B, Divers J, Bell R, Badaru A, Talton JW, Crume T et al.. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 2014;311(17):1778–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bell RA, Mayer-Davis EJ, Beyer JW, D'Agostino RB Jr., Lawrence JM, Linder B, Liu LL, Marcovina SM, Rodriguez BL, Williams D et al.. Diabetes in non-Hispanic white youth: prevalence, incidence, and clinical characteristics: the SEARCH for Diabetes in Youth Study. Diabetes Care 2009;32(Suppl 2):S102–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Van Rompay MI, McKeown NM, Goodman E, Eliasziw M, Chomitz VR, Gordon CM, Economos CD, Sacheck JM. Sugar-sweetened beverage intake is positively associated with baseline triglyceride concentrations, and changes in intake are inversely associated with changes in HDL cholesterol over 12 months in a multi-ethnic sample of children. J Nutr 2015;145(10):2389–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bleich SN, Barry CL, Gary-Webb TL, Herring BJ. Reducing sugar-sweetened beverage consumption by providing caloric information: how black adolescents alter their purchases and whether the effects persist. Am J Public Health 2014;104(12):2417–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dodd AH, Briefel R, Cabili C, Wilson A, Crepinsek MK. Disparities in consumption of sugar-sweetened and other beverages by race/ethnicity and obesity status among United States schoolchildren. J Nutr Educ Behav 2013;45(3):240–9. [DOI] [PubMed] [Google Scholar]
- 21. Patel AI, Ritchie L. Striving for meaningful policies to reduce sugar-sweetened beverage intake among young children. Pediatrics 2013;132(3):566–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Vargas-Garcia EJ, El Evans C, Cade JE. Impact of interventions to reduce sugar-sweetened beverage intake in children and adults: a protocol for a systematic review and meta-analysis. Syst Rev 2015;4:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Levy DT, Friend KB, Wang YC. A review of the literature on policies directed at the youth consumption of sugar sweetened beverages. Adv Nutr 2011;2(Suppl):182s–200s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hsiao A, Wang YC. Reducing sugar-sweetened beverage consumption: evidence, policies, and economics. Curr Obes Rep 2013;2(3):191–9. [Google Scholar]
- 25. Lasater G, Piernas C, Popkin BM. Beverage patterns and trends among school-aged children in the US, 1989–2008. Nutr J 2011;10:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ng SW, Slining MM, Popkin BM. Turning point for US diets? Recessionary effects or behavioral shifts in foods purchased and consumed. Am J Clin Nutr 2014;99(3):609–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cavadini C, Siega-Riz AM, Popkin BM. US adolescent food intake trends from 1965 to 1996. Arch Dis Child 2000;83(1):18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Han E, Powell LM. Consumption patterns of sugar-sweetened beverages in the United States. J Acad Nutr Diet 2013;113(1):43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Powell ES, Smith-Taillie LP, Popkin BM. Added sugars intake across the distribution of US children and adult consumers: 1977–2012. J Acad Nutr Diet 2016;116(10):1543–50, e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. US Department of Health and Human Services; USDA; Dietary Guidelines Advisory Committee Dietary guidelines for Americans, 2015–2020. 8th ed Washington (DC): US Department of Health and Human Services and USDA;2015. [Google Scholar]
- 31. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311(8):806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. May AL, Freedman D, Sherry B, Blanck HM. Obesity—United States, 1999–2010. MMWR Surveill Summ 2013;62(Suppl 3):120–8. [PubMed] [Google Scholar]
- 33. Rossen LM, Schoendorf KC. Measuring health disparities: trends in racial-ethnic and socioeconomic disparities in obesity among 2- to 18-year old youth in the United States, 2001–2010. Ann Epidemiol 2012;22(10):698–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Frederick CB, Snellman K, Putnam RD. Increasing socioeconomic disparities in adolescent obesity. Proc Natl Acad Sci USA 2014;111(4):1338–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, Guenther PM, Krebs-Smith SM, Subar AF, Dodd KW. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med 2010;29(27):2857–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tooze JA, Midthune D, Dodd KW, Freedman LS, Krebs-Smith SM, Subar AF, Guenther PM, Carroll RJ, Kipnis V. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Nutr Diet 2006;106(10):1575–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. National Cancer Institute Epidemiology and Genomics Research Pro-gram. Available from: https://epi.grants.cancer.gov/diet/usualintakes/macros_single.html. accessed July 5, 2016. [Google Scholar]
- 38. National Center for Health Statistics ; CDC ; US Department of Health and Human Services National Health and Nutrition Examination Survey 2003-2004. Hyattsville (MD); 2003–2004. [Google Scholar]
- 39. National Center for Health Statistics ; CDC ; US Department of Health a nd Human Services National Health and Nutrition Examination Survey 2003-2004. Hyattsville (MD); 2007–2008. [Google Scholar]
- 40. National Center for Health Statistics ; CDC ; US Department of Health and Human Services National Health and Nutrition Examination Survey 2003-2004. Hyattsville (MD); 2005–2006. [Google Scholar]
- 41. Bodner J, Perloff B. Databases for analyzing dietary data—the latest word from What We Eat in America. J Food Compos Anal 2003;16(3):347–58. [Google Scholar]
- 42. USDA Food and Nutrient Database for Dietary Studies, 2.0. USDA, Agricultural Research Service, Food Survey Research Group; Washington (DC):2006. [Google Scholar]
- 43. USDA Food and Nutrient Database for Dietary Studies, 4.1. USDA, Agricultural Research Service, Food Survey Research Group; Washington (DC):2010. [Google Scholar]
- 44. USDA Food and Nutrient Database for Dietary Studies, 3.0. USDA, Agricultural Research Service, Food Survey Research Group; Washington (DC):2008. [Google Scholar]
- 45. National Center for Health Statistics ; CDC ; US Department of Health and Human Services National Health and Nutrition Examination Survey 2003-2004. Hyattsville (MD); 2009–2010. [Google Scholar]
- 46. Slining MM, Ng SW, Popkin BM. Food companies' calorie-reduction pledges to improve U.S. diet. Am J Prev Med 2013;44(2):174–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Slining M, Popkin B. Trends in intakes and sources of solid fats and added sugars among U.S. children and adolescents: 1994–2010. Pediatr Obes 2013;8(4):307–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Agricultural Research Service What we eat in America, NHANES 2013–2014; USDA ARS. Washington (DC): USDA; 2017. [Google Scholar]
- 49. Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Ingwersen LA et al.. The US Department of Agriculture automated multiple-pass method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008;88(2):324–32. [DOI] [PubMed] [Google Scholar]
- 50. Institute of Medicine Dietary Reference Intakes for energy, carbohydrates, fiber, fat, protein and amino acids (macronutrients). Washington (DC): National Academies Press; 2005. [Google Scholar]
- 51. Huang TTK, Roberts SB, Howarth NC, McCrory MA. Effect of screening out implausible energy intake reports on relationships between diet and BMI. Obes Res 2005;13(7):1205–17. [DOI] [PubMed] [Google Scholar]
- 52. Tudor-Locke C, Camhi S, Troiano R. A catalog of rules, variables, and definitions applied to accelerometer data in the National Health and Nutrition Examination Survey, 2003–2006. Prev Chronic Dis 2012;9:E113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Miller PE, McKinnon RA, Krebs-Smith SM, Subar AF, Chriqui J, Kahle L, Reedy J. Sugar-sweetened beverage consumption in the U.S.: novel assessment methodology. Am J Prev Med 2013;45(4):416–21. [DOI] [PubMed] [Google Scholar]
- 54. Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, Guenther PM, Krebs-Smith SM, Subar AF, Dodd KW. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med 2010;29(27):2857–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Belotti F, Deb P, Manning WG, Norton EC. twopm: two-part models. Stata J 2015;15(1):3–20. [Google Scholar]
- 56. Haines PS, Popkin BM, Guilkey DK. Modeling food consumption decisions as a two-step process. Am J Agr Econ 1988;70(3):543–52. [Google Scholar]
- 57. Parsons R, Munuo S, Buckman D, Tooze J, Dodd K. User's guide for analysis of usual intakes. 2009. Available from: http://appliedresearch.cancer.gov/diet/usualintakes/Users_Guide_Mixtran_Distrib_Indivint_1.1.pdf. accessed July 5, 2016. [Google Scholar]
- 58. Korn EL, Graubard BI. Analysis of health surveys. Hoboken (NJ); John Wiley and Sons; 1999. [Google Scholar]
- 59. Cade BS, Noon B. A gentle introduction to quantile regression for ecologists. Frontiers Ecol Environ 2003;1(8):412–20. [Google Scholar]
- 60. Koenker R, Bassett G. Regression quantiles. Econometrica 1978;46(1):33–50. [Google Scholar]
- 61. Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr 2013;98(4):1084–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Powell LM, Wada R, Kumanyika SK. Racial/ethnic and income disparities in child and adolescent exposure to food and beverage television ads across the U.S. media markets. Health Place 2014;29:124–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ost C, De Ridder KAA, Tafforeau J, Van Oyen H. The added value of food frequency questionnaire (FFQ) information to estimate the usual food intake based on repeated 24-hour recalls. Arch Public Health 2017;75:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ervin RB, Kit BK, Carroll MD, Ogden CL. Consumption of added sugar among U.S. children and adolescents, 2005–2008. NCHS Data Brief 2012;(87):1–8. [PubMed] [Google Scholar]
- 65. Welsh JA, Sharma AJ, Grellinger L, Vos MB. Consumption of added sugars is decreasing in the United States. Am J Clin Nutr 2011;94(3):726–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Te Morenga LA, Howatson AJ, Jones RM, Mann J. Dietary sugars and cardiometabolic risk: systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids. Am J Clin Nutr 2014;100(1):65–79. [DOI] [PubMed] [Google Scholar]
- 67. WHO Draft guidelines on free sugars released for public consultation. Geneva (Switzerland): WHO; 2014. [Google Scholar]
- 68. DiMeglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes Relat Metab Disord 2000;24(6):794–800. [DOI] [PubMed] [Google Scholar]
- 69. Mourao D, Bressan J, Campbell W, Mattes R. Effects of food form on appetite and energy intake in lean and obese young adults. Int J Obes (Lond) 2007;31(11):1688–95. [DOI] [PubMed] [Google Scholar]
- 70. Ahluwalia N, Dwyer J, Terry A, Moshfegh A, Johnson C. Update on NHANES dietary data: focus on collection, release, analytical considerations, and uses to inform public policy. Adv Nutr 2016;7(1):121–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Kramer K, Schwartz L, Lafleur M, Williams J. Targeted marketing of junk food to ethnic minority youth: a report about fighting back with legal advocacy and community engagement. In: Williams JD, Pasch KE, Collins CA, editors. Advances in communication research to reduce childhood obesity. New York: Springer Science & Business Media; 2013. p. 389–405. [Google Scholar]
- 72. Kumar G, Onufrak S, Zytnick D, Kingsley B, Park S. Self-reported advertising exposure to sugar-sweetened beverages among US youth. Public Health Nutr 2015;18(7):1173–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev 2015;73(10):643–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Andreyeva T, Chaloupka FJ, Brownell KD. Estimating the potential of taxes on sugar-sweetened beverages to reduce consumption and generate revenue. Prev Med 2011;52(6):413–6. [DOI] [PubMed] [Google Scholar]
- 75. Silver LD, Ng SW, Ryan-Ibarra S, Taillie LS, Induni M, Miles DR, Poti JM, Popkin BM. Changes in prices, sales, consumer spending, and beverage consumption one year after a tax on sugar-sweetened beverages in Berkeley, California, US: a before-and-after study. PloS Med 2017;14(4):e1002283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Colchero MA, Popkin BM, Rivera JA, Ng SW. Beverage purchases from stores in Mexico under the excise tax on sugar sweetened beverages: observational study. BMJ 2016;352:h6704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Colchero MA, Rivera-Dommarco J, Popkin BM, Ng SW. In Mexico, evidence of sustained consumer response two years after implementing a sugar-sweetened beverage tax. Health Aff 2017;36(3):564–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Popkin BM, Hawkes C. Sweetening of the global diet, particularly beverages: patterns, trends, and policy responses. Lancet Diabetes Endocrinol 2016;4(2):174–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.