Introduction
Herpes zoster (HZ), also known as shingles, occurs as a result of reactivation of varicella-zoster virus. The virus initially causes infection during childhood as varicella, or chickenpox, and becomes dormant in the dorsal root ganglia of the nerves. Once the virus is reactivated, a vesicular eruption appears along a dermatome and can cause pain.1 Postherpetic neuralgia is a well-known complication of HZ; however, motor complications are seldom recognized by many physicians. Motor complications often occur in the muscles of the head, trunk, or extremities and may also involve the visceral nerves, causing colonic pseudo-obstruction. The pathogenesis of such complications is still debated, but it is speculated that viral spreading to the ventral root of the nerves might cause motor complications.1 Here, we report 3 cases of pseudohernia as a result of motor complications of HZ.
Case reports
Case 1
A 67-year-old man visited the emergency room complaining of constipation, pain, and bulging in the left lower abdomen, which had started 2 days earlier (Fig 1, A and B). Abdominal computed tomography (CT) and ultrasonography were conducted to evaluate the possibility of abdominal hernia, but neither test showed signs of hernia. Without a specific cause for his abdominal herniation, the patient was advised to visit the general surgery department for further evaluation. However, grouped erythematous vesicles developed approximately 2 days later along the left T9-10 dermatome where the bulging had occurred. A diagnosis of HZ was then reached, and the patient was given famciclovir for a week. Skin lesions improved, but the bulging remained, and the patient still complained of constipation. Electromyography (EMG) of the abdominal muscles showed decreased thickness in the left internal oblique abdominis and tibialis anterior muscle compared with the right side. Pseudohernia associated with HZ was then diagnosed, and the patient is under close observation. He was given a prescription for magnesium oxide for constipation and was advised to practice abdominal respiration and use a waist band for strengthening abdominal muscle as a conservative treatment for pseudohernia. His bulge showed complete resolution in 8 months, and constipation improved after 1 month.
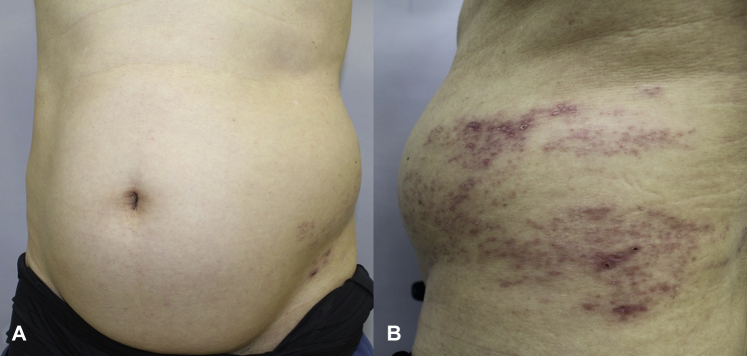
Fig 1.
Case 1. A, Bulging is seen in the left abdomen. B, Erythematous maculopatches with crusts are observed along the left T9-10 dermatome, consistent with the area where bulging is seen.
Case 2
A 68-year-old man with medical history of hypertension, diabetes mellitus (DM), and ischemic heart disease came to the clinic complaining of postherpetic neuralgia that had started a month earlier after rash occurred along his right T12-L1 dermatome. He also complained that his right abdomen showed bulging approximately a day after the rash appeared (Fig 2, A and B). Abdominal CT did not show any signs of abdominal hernia (Fig 2, C). Abdominal pseudohernia due to HZ was diagnosed. No treatment was given for the bulging, but the patient was given gabapentin to relieve postherpetic neuralgia. His pain subsided approximately 2 months after the treatment, and his bulging improved approximately 5 months after the onset (Fig 2, D).
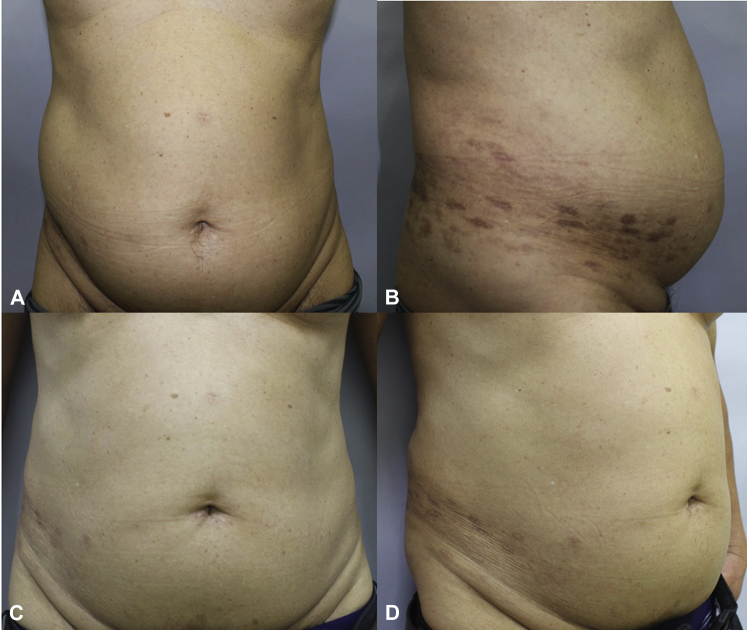
Fig 2.
Case 2. A, Mild bulging is seen in the right abdomen. B, Hyperpigmented macules and patches are observed along the right T12-L1 dermatome. C and D, Pseudohernia spontaneously improved 5 months after onset.
Case 3
A 75-year-old woman with a history of DM for 30 years visited our clinic complaining of grouped vesicles along left T10-11 dermatome, which had started 10 days earlier, and left flank bulging, which had appeared approximately a day after the vesicles appeared. She did not feel much pain due to HZ but, rather, complained of an itching sensation along the left T10-11 dermatome. Abdominal CT did not show any signs of mass or fluid collection. Valacyclovir was prescribed for a week, and her itching sensation and skin lesions resolved, but the bulging remained. The patient is still under close observation, but the bulge did not show any improvement after 2 months of follow-up.
Discussion
HZ usually occurs from viral multiplication and spreads within the dorsal root ganglia (the sensory axons), causing severe pain and postherpetic neuralgia among its main complications. However, motor complications can occur when the virus attacks the ventral root (motor axons).2, 3 Approximately 5% of patients with HZ experience motor complications such as facial palsy, Ramsay Hunt syndrome, or segmental paresis of the limbs.3, 4, 5 Pseudohernia due to HZ is also a rare motor complication of HZ and occurs in approximately 0.17% of cases.3, 4, 5 Pseudohernia is defined as bulging of the abdominal wall that is not caused by structural defects, collection of fluid, or a mass but, rather, muscle paralysis.5 The causes include a complication of DM, such as diabetic radiculoneuropathy; trauma, such as ventral root injury from tumor removal and prolapsed intravertebral disk; and infections, such as Lyme disease, poliomyelitis, and HZ.5, 6 Pseudohernia due to HZ is also known as abdominal wall postherpetic pseudohernia, HZ-induced abdominal paresis, and segmental zoster abdominal paresis.1, 2, 3, 4, 5, 6 Elderly and immunocompromised patients are at higher risk of developing motor deficits due to HZ.4, 6 Motor deficits usually occur in the same or adjacent levels as where the virus is infected.5
According to Chernev and Dado,1 the age range of patients with pseudohernia due to HZ was 45 to 84 years, with a mean age of 67.5 years, and more men were affected than women. Abdominal bulging usually occurred between 7 and 60 days after the rash, with a mean period of 24 days after the onset of cutaneous rash.1, 3 Generally, abdominal bulging due to HZ is asymptomatic, but when the visceral nerve is involved in the gastrointestinal tracts, colonic pseudo-obstruction and constipation-associated symptoms can concur.1, 7 A few hypotheses have been made to explain the pathogenesis of visceral involvement. The first is the direct invasion of varicella-zoster virus in the intrinsic intestinal autonomic nervous system. Another hypothesis is that the vesicular eruption can cause visceral peritoneal inflammation, thus causing pain or constipation in the gastrointestinal tracts. The final explanation is the involvement of autonomic ganglion caused by the infection of the ventral horn of the spinal cord.8 In a case review of 36 patients with pseudohernia due to HZ, approximately 19.4% complained of accompanying gastrointestinal complications such as constipation or colonic pseudo-obstruction.1 The age range of the patients from our cases was 67 to 75 years. In 2 cases, bulging occurred after the cutaneous manifestations of HZ, but in 1 case, bulging occurred 2 days before the vesicles appeared; 1 patient showed signs of visceral involvement, with severe abdominal pain and constipation. The characteristics of our patients are summarized in Table I.
Table I.
Reported cases of pseudohernia due to HZ in the dermatologic literature and our cases
| Number | Reported case | Age in years/sex | Onset of pseudohernia | Dermatome | Comorbidity | Associated symptoms | Remission |
|---|---|---|---|---|---|---|---|
| — | Sharma et al3 | 55/M | 30 days before rash | Left T10, T11 | None | Cough reflex | Not mentioned |
| — | Giuliani et al4 | 75/M | 60 days after rash | Left T10, T11 | Sigmoid colon cancer | None | Mild improvement after 7 months |
| — | Chiu and Lin5 | 73/M | 20 days after rash | Left T11, T12 | Hypertension, DM | Cough reflex | 7 months |
| 1 | Our cases | 67/M | 2 days before rash | Left T9, T10 | None | Constipation | Mild improvement after 6 months |
| 2 | 68/M | 30 days after rash | Right T12, L1 | Hypertension, DM, ischemic heart disease | None | 5 months | |
| 3 | 75/F | 1 day after rash | Left T10, T11 | DM | None | No improvement after 2 months |
DM, Diabetes mellitus; F, female; M, male.
A diagnosis of pseudohernia due to HZ is based on clinical suspicion with previous or present history of HZ and abdominal-wall bulging that is not associated with a structural defect.6 For evaluation, EMG can be used to detect any nerve-conduction abnormality in the abdominal wall muscles.1, 2, 4, 6, 9, 10, 11, 12, 13, 14 Also, CT should be used to rule out the possibility of abdominal wall hernia due to structural defect, mass, or fluid collection in the affected area.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 In our first case, there were abnormal spikes in the involved area on EMG compared with normal findings on the unaffected side. None of our 3 cases showed any signs of hernia, mass, or fluid collection on abdominal CT.
Pseudohernia due to HZ usually shows good prognosis, with self-regression after few months.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 In most reported cases, symptoms resolved without treatment between 3 and 12 months after onset. In 2 of our cases, the bulge improved after 2 and 8 months after onset, and in 1 case, the patient did not show any improvement after 2 months of follow-up, but she is still under close observation. According to previous studies, 55% to 85% of patients with zoster paresis showed improvement without any treatment.1
More than 30 cases of pseudohernia due to HZ have been published in the English literature,3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 and most case reports or reviews have been reported in the neurology, general surgery, and emergency medicine literatures.6, 7, 8, 9, 10, 11, 12, 13, 14, 15 Although dermatologists are primary physicians who diagnose and manage HZ, only 3 cases have been reported in the dermatology literature (Table I).3, 4, 5 This might be because patients can be unaware of such symptoms when the changes are minimal and when skin lesions and pain are so critical that they do not notice abdominal bulging or because dermatologists are unfamiliar with such adverse effects and seldom notice them. Another explanation is that patients are more likely to visit the surgery or emergency departments, assuming that abdominal bulging might have occurred because of a structural defect or abdominal mass.
In conclusion, we report 3 cases of abdominal bulging associated with HZ so that dermatologists are aware that such rare complications can occur as a result of HZ affecting the motor neurons. Physicians should also inform patients that the symptoms will self-regress after few months.
Acknowledgments
We thank the patients for their cooperation, which helped us prepare this report.
Footnotes
Funding sources: The publication fee will be paid by the funding from the National Research Foundation in Korea (NRF-2018R1D1A1B07041219).
Conflicts of interest: None disclosed.
References
- 1.Chernev I., Dado D. Segmental zoster abdominal paresis (zoster pseudohernia): a review of the literature. PM R. 2013;5:786–790. doi: 10.1016/j.pmrj.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 2.Kesler A., Galili-Mosberg R., Gadoth N. Acquired neurogenic abdominal wall weakness simulating abdominal hernia. Isr Med Assoc J. 2002;4:262–264. [PubMed] [Google Scholar]
- 3.Sharma P., Gautam R., Basistha C., Jain R., Kar H. Abdominal hernia following abdominal herpes zoster. Indian J Dermatol Venereol Leprol. 2001;67:39. [PubMed] [Google Scholar]
- 4.Giuliani A., Galati G., Parisi L. Postherpetic paresis mimicking an abdominal herniation. Acta Derm Venereol. 2006;86:73–74. doi: 10.1080/00015550510042886. [DOI] [PubMed] [Google Scholar]
- 5.Chiu H.-Y., Lin S.-J. A painful bulge in the left flank. JAMA. 2013;310:639–640. doi: 10.1001/jama.2013.116866. [DOI] [PubMed] [Google Scholar]
- 6.Oliveira P.D., Dos Santos Filho P.V., De Menezes J.E.M.T., Oliveira I.C.D. Abdominal-wall postherpetic pseudohernia. Hernia. 2006;10:364–366. doi: 10.1007/s10029-006-0102-6. [DOI] [PubMed] [Google Scholar]
- 7.Healy C., Mcgreal G., Lenehan B., Mcdermott E., Murphy J. Self-limiting abdominal wall herniation and constipation following herpes zoster infection. QJM. 1998;91:788–789. doi: 10.1093/qjmed/91.11.788. [DOI] [PubMed] [Google Scholar]
- 8.Kim E.-D., Kang B.-G., Kim J.H., Roh M., Jo D.H. Abdominal distention and constipation followed by herpes zoster infection. Korean J Anesthesiol. 2013;65:S143. doi: 10.4097/kjae.2013.65.6S.S143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gottschau P., Trojaborg W. Abdominal muscle paralysis associated with herpes zoster. Acta Neurol Scand. 1991;84:344–347. doi: 10.1111/j.1600-0404.1991.tb04966.x. [DOI] [PubMed] [Google Scholar]
- 10.Dobrev H.P., Atanassova P.A., Sirakov V.N., Zisova L.G. A case of rheumatoid arthritis presenting with postherpetic neuralgia and abdominal-wall pseudohernia. Rheumatol Int. 2012;32:1775–1777. doi: 10.1007/s00296-009-1360-2. [DOI] [PubMed] [Google Scholar]
- 11.Ohno S., Togawa Y., Chiku T., Sano W. Case report: Postherpetic pseudohernia: delayed onset of paresis of abdominal muscles due to herpes zoster causing an ipsilateral abdominal bulge. BMJ Case Rep. 2016;2016 doi: 10.1136/bcr-2016-215377. :bcr2016215377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zuckerman R., Siegel T. Abdominal-wall pseudohernia secondary to herpes zoster. Hernia. 2001;5:99–100. doi: 10.1007/s100290100005. [DOI] [PubMed] [Google Scholar]
- 13.Tashiro S., Akaboshi K., Kobayashi Y., Mori T., Nagata M., Liu M. Herpes zoster–induced trunk muscle paresis presenting with abdominal wall pseudohernia, scoliosis, and gait disturbance and its rehabilitation: a case report. Arch Phys Med Rehabil. 2010;91:321–325. doi: 10.1016/j.apmr.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 14.Mancuso M., Virgili M.P., Pizzanelli C. Abdominal pseudohernia caused by herpes zoster truncal D12 radiculoneuropathy. Arch Neurol. 2006;63:1327. doi: 10.1001/archneur.63.9.1327. [DOI] [PubMed] [Google Scholar]
- 15.Shikino K., Miyahara M., Noda K., Ohira Y., Ikusaka M. Unilateral lower abdominal wall protrusion and umbilical deviation. Clin Case Rep. 2016;4:451–452. doi: 10.1002/ccr3.524. [DOI] [PMC free article] [PubMed] [Google Scholar]