Abstract
Introduction: Prolonged air leak is the most common complication after pulmonary resection. This occurs more frequently in patients with incomplete interlobar fissure, chronic obstructive pulmonary disease, or emphysema. Interlobar lymphadenopathy can make interlobar fissure division difficult.
Surgical technique: Several techniques of interlobar fissure division have been documented. The interlobar fissure is routinely divided using a stapler during pulmonary lobectomy. Normally, a stapler is used extravascularly. Here, we present a patient who successfully underwent interlobar fissure division wherein the jaw of the stapler passed through the interlobar pulmonary artery between A6 and A8 branches during resection of a lung squamous cell carcinoma in the left lower lobe with an interlobar lymphadenopathy.
Conclusion: Interlobar fissure division inserting a jaw of stapler into pulmonary artery is easy and useful option for left lower lobectomy. This technique is especially useful for a patient with an interlobar lymphadenopathy.
Keywords: interlobar fissure division, pulmonary artery, stapling, lymphadenopathy, left lower lobectomy
Introduction
The interlobar fissure is routinely divided using a stapler during pulmonary lobectomy. Normally, a stapler is used extravascularly. Here, we present a patient who successfully underwent interlobar fissure division by passing the jaw of the stapler through the interlobar pulmonary artery during resection of a lung squamous cell carcinoma in the left lower lobe with an interlobar lymphadenopathy.
Surgical Technique
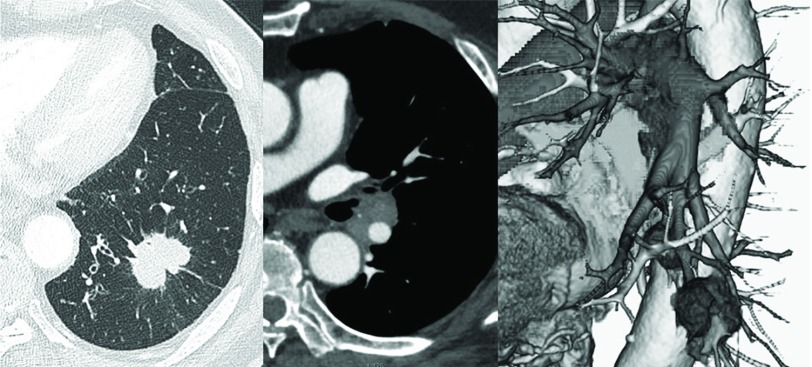
A 70-year-old male smoker, having a 3.1 × 2.5 cm squamous cell carcinoma in the lateral basal segment (S9) of the left lower lobe with an interlobar no. 11 lymphadenopathy and an intrapulmonary metastasis (cT3N1M0: stage IIIA), was admitted for surgery (Fig. 1). He previously underwent bilateral thoracic surgery for pulmonary tuberculosis and rib caries in addition to emphysema. Fluorodeoxyglucose positron emission tomography scan showed positive uptake at the tumor mass and an interlobar no. 11 lymph nodes. Chest computed tomography scan revealed mediastinal lingular artery, both superior and inferior lingular arteries descending between the upper pulmonary vein and bronchus from the left main pulmonary artery. We planned the intravascular stapling technique for incomplete interlobar fissure division.
Fig. 1. Preoperative chest computed tomography scan shows a 3.1 cm squamous cell carcinoma in the lateral basal segment (S9) of the left lower lobe with an interlobar lymphadenopathy, and both superior and inferior lingular arteries descending between the upper pulmonary vein and bronchus from the left main pulmonary artery.
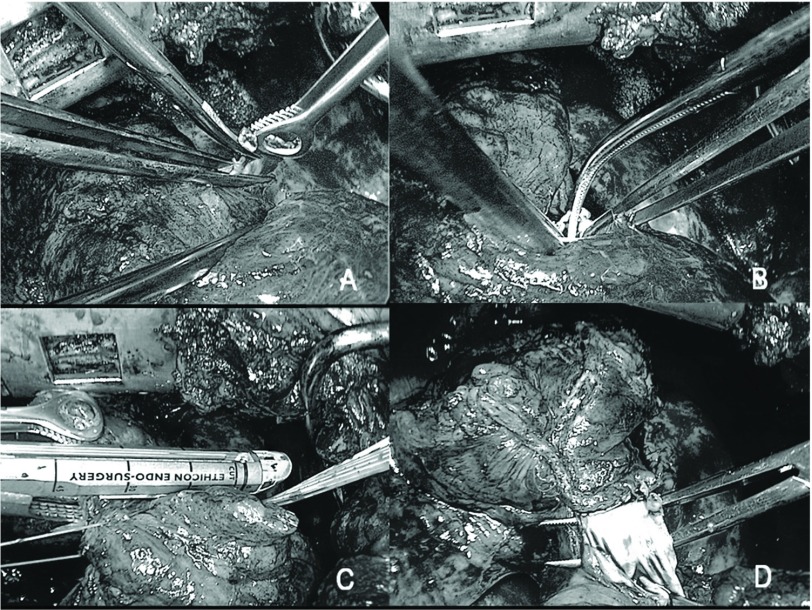
Posterolateral thoracotomy was performed. The lung strongly adhered to the chest wall in the whole thoracic cavity. Thus, adhesiolysis was performed first. The inferior pulmonary vein was dissected and closed using a vascular stapler after inferior pulmonary ligament division. The pulmonary artery was also transected using a vascular stapler between A1+2c branch and A6a branch (Fig. 2, Video). The anterior interlobar fissure between lingular segment and anterior basal segment was divided using a stapler. We made a small incision of the stump of interlobar pulmonary artery and confirmed absence of bleeding. We cut a peripheral resection stump of the interlobar pulmonary artery completely, inserted forceps into the interlobar pulmonary artery stump, and advanced the tip of the forceps from the A8 branch. A Penrose drain was inserted into the pulmonary artery. We passed the jaw of the stapler (Powered ECHELON FLEX GST System 60mm Green, Ethicon Inc., Somerville, NJ, USA) through the interlobar pulmonary artery following a Penrose drain guide. We dissected the interlobar fissure including the anterior wall of the interlobar pulmonary artery between A6 and A8 branches. We cut off the remaining posterior wall of the interlobar pulmonary artery and performed interlobar lymph node dissection. There was no air leak around the interlobar surface of the left upper lobe on a sealing test. The remaining upper lobe expanded fully without any collapse. The operative time was 361 minutes and total blood loss was 310 g. The patient had an uncomplicated postoperative course and discharged on postoperative day 8. Histopathological findings revealed interlobar no.11 lymph node was positive.
Fig. 2. Intraoperative view of interlobar fissure division. (A) Cutting a peripheral resection stump of the interlobar pulmonary artery. (B) Inserting forceps into the interlobar pulmonary artery stump. (C) Passing the jaw of the stapler through the interlobar pulmonary artery following a Penrose drain guide. (D) The remaining posterior wall of the interlobar pulmonary artery.
Video legend (The video is available online)
Intraoperative video from transection of the pulmonary artery to interlobar lymph node dissection. The pulmonary artery was also transected using a vascular stapler between A1+2c branch and A6a branch. Cutting a peripheral resection stump of the interlobar pulmonary artery. Inserting forceps into the interlobar pulmonary artery stump. Passing the jaw of the stapler through the interlobar pulmonary artery following a Penrose drain guide. Dissecting the interlobar fissure including the anterior wall of the interlobar pulmonary artery between A6 and A8 branches. The interlobar lymph node dissection after cutting remaining posterior wall of the interlobar pulmonary artery.
Discussion
In cases of an incomplete interlobar fissure, dissection may be difficult and time-consuming, and there is high risk of prolonged air leakage.1) In particular, chronic obstructive pulmonary disease and emphysema lead to an increased risk of air leakage.2) Several techniques and instruments of interlobar fissure division have been documented.3–5) Though the interlobar fissure is routinely divided using a stapler during pulmonary lobectomy, there are some reports on the usage of new devices, such as laser and bipolar sealing instruments.4,5)
Though this technique is limited to the left lower lobectomy for a patient whose superior and inferior lingular arteries descending between the upper pulmonary vein and bronchus from the left main pulmonary artery, this technique is an easy and useful option for interlobar fissure division during pulmonary lobectomy. Although this technique can also be applied to thoracoscopic surgery, it is necessary to make a precise assessment of lingular arteries preoperatively and sufficient preparation to hemorrhage. This technique is especially useful for a patient with an interlobar lymphadenopathy, such as in this case, because it is impossible to divide the left lower bronchus before interlobar fissure division.
In conclusion, interlobar fissure division inserting a jaw of stapler into pulmonary artery is easy and useful option for left lower lobectomy.
Disclosure Statement
All authors has no conflict of interest.
References
- 1).Gómez-Caro A, Calvo MJ, Lanzas JT, et al. The approach of fused fissures with fissureless technique decreases the incidence of persistent air leak after lobectomy. Eur J Cardiothorac Surg 2007; 31: 203-8. [DOI] [PubMed] [Google Scholar]
- 2).Liang S, Ivanovic J, Gilbert S, et al. Quantifying the incidence and impact of postoperative prolonged alveolar air leak after pulmonary resection. J Thorac Cardiovasc Surg 2013; 145: 948-54. [DOI] [PubMed] [Google Scholar]
- 3).Stamenovic D, Bostanci K, Messerschmidt A, et al. Fissureless fissure-last video-assisted thoracoscopic lobectomy for all lung lobes: a better alternative to decrease the incidence of prolonged air leak? Eur J Cardiothorac Surg 2016; 50: 118-23. [DOI] [PubMed] [Google Scholar]
- 4).Sakuragi T, Takeda Y, Teishikata T, et al. Is bipolar thermofusion an acceptable option for unseparated interlobar fissure division in pulmonary lobectomy? Interact Cardiovasc Thorac Surg 2013; 17: 26-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5).Marulli G, Droghetti A, Di Chiara F, et al. A prospective randomized trial comparing stapler and laser techniques for interlobar fissure completion during pulmonary lobectomy. Laser Med Sci 2013; 28: 505-11. [DOI] [PubMed] [Google Scholar]