Abstract
Background and Objectives:
Poor sleep is prevalent among individuals with social anxiety disorder (SAD) and may affect treatment outcome. We examined whether: (1) individuals with SAD differed from healthy controls (HCs) in sleep quality, (2) baseline sleep quality moderated the effects of treatment (Cognitive-behavioral group therapy [CBGT] vs. mindfulness-based stress reduction [MBSR] vs. waitlist [WL]) on social anxiety, (3) sleep quality changed over treatment, and (4) changes in sleep quality predicted anxiety 12-months post-treatment.
Design:
Participants were 108 adults with SAD from a randomized controlled trial of CBGT vs. MBSR vs. WL and 38 HCs.
Methods:
SAD and sleep quality were assessed pre-treatment and post-treatment, and SAD was assessed again 12-months post-treatment.
Results:
Participants with SAD reported poorer sleep quality than HCs. The effect of treatment condition on post-treatment social anxiety did not differ as a function of baseline sleep quality. Sleep quality improved in MBSR, significantly more than WL, but not CBGT. Sleep quality change from pre- to post-treatment in CBGT or MBSR did not predict later social anxiety.
Conclusions:
MBSR, and not CBGT, improved sleep quality among participants. Other results were inconsistent with prior research; possible explanations, limitations, and implications for future research are discussed.
Keywords: Social anxiety disorder, treatment, sleep quality, mindfulness-based stress reduction, cognitive-behavior therapy
Introduction
Social anxiety disorder (SAD) is characterized by intense fear and avoidance of social situations (American Psychiatric Association [APA], 2013). SAD is highly prevalent (lifetime prevalence 12.1%; Kessler, Chiu, Demler, Merikangas, & Walters, 2005), and individuals with SAD experience decreased life satisfaction (Eng, Coles, Heimberg, & Safren, 2005; Hambrick, Turk, Heimberg, Schneier, & Liebowitz, 2003; Olatunji, Cisler, & Tolin, 2007) and impaired functioning across multiple domains including work, school, and general social functioning (Aderka et al., 2012; Katzelnick et al., 2001; Ruscio et al., 2008). In addition, SAD is often associated with increased sleep dysfunction (e.g., Buckner, Bernert, Cromer, Joiner, & Schmidt, 2008; Ramsawh, Stein, Belik, Jacobi, & Sareen, 2009; Roth et al., 2006), the presence of which has been associated with greater severity of symptoms among individuals with SAD (Kushnir, Marom, Mazar, Sadeh, & Hermesh, 2014).
Sleep dysfunction is a widespread problem, with about 30% of the general population reporting at least some symptoms of insomnia and sleep-related disturbances (Ancoli-Israel & Roth, 1999; Morin, Leblanc, Daley, Gregoire, & Merette, 2006). Past research has indicated that many anxiety disorders, including SAD, are associated with sleep dysfunction; one study found that, after controlling for past month substance use and mood disorders, SAD, along with generalized anxiety disorder (GAD) and agoraphobia, was associated with a three-to-fourfold increase in the likelihood of reported sleep difficulties (Ramsawh et al., 2009). Overall, however, the literature on the association between SAD and sleep dysfunction is somewhat less consistent than the literature on the association between sleep dysfunction and other anxiety disorders, such as GAD, posttraumatic stress disorder (PTSD), and panic disorder (Mellman 2006; Mellman 2008); some studies have demonstrated that sleep disturbance among individuals with generalized SAD is only mildly elevated (Pace-Schott et al., 2018) or is no worse than that of non-anxious controls (Brown, Black, & Uhde, 1994). However, studies that do find an association between SAD and sleep disturbance have report the percentage of individuals with SAD reporting such disturbances to be around 50-60% (e.g., Stein, Kroft, & Walker, 1993; Zalta et al., 2013). When present, the association between SAD and sleep dysfunction may be explained in part by the close relationship between repetitive negative thinking—an important cognitive process in the characterization and maintenance of SAD (e.g., Brozovich & Heimberg, 2008)—and reductions in sleep quality (Guastella & Moulds, 2007; Harvey & Payne, 2002). Evidence also suggests that poor sleep may lead to greater social avoidance (Simon & Walker, 2018) and that there is a bidirectional relationship between sleep problems and anxiety more generally (Alvaro, Roberts, & Harris, 2013), suggesting that poor sleep may, in turn, worsen social avoidance and anxiety over time. Additionally, there is evidence to suggest that poor sleep may impair extinction learning, which in turn contributes to the etiology and perpetuation of multiple anxiety disorders (e.g., Pace-Schott, Germain, & Milad, 2015). Therefore, it is important to both clarify the association between SAD and sleep dysfunction and to address such problems in treatment for SAD when they are present.
Cognitive-behavioral therapy (CBT), an efficacious treatment for anxiety disorders (e.g., Olatunji, Cisler, & Deacon, 2010), appears to be associated with moderate improvements in sleep over the course of treatment for numerous anxiety-related conditions that are associated with sleep difficulties, such as GAD, panic disorder, and PTSD; however, little data exist on whether improvements in sleep occur over the course of CBT for SAD (Belleville, Cousineau, Levrier, St.-Pierre-Delorme, & Marchand, 2010). In addition, no data exist on improvements in sleep over the course of other treatments for SAD, such as mindfulness-based treatments, which have also been shown to be efficacious in the treatment of SAD (e.g., Koszycki, Benger, Shlik, & Bradwejn, 2007; Norton, Abbott, Norberg, & Hunt, 2015; Hjeltnes et al., 2017; Goldin et al., 2016). Therefore, it is important to investigate whether there are concomitant improvements in sleep quality over the course of effective treatments for SAD, as well as whether certain modes of treatment for SAD are more effective in improving sleep quality than others. Furthermore, it is important to determine whether improvements in sleep quality over treatment for SAD are associated with subsequent improvements in social anxiety symptoms, in order to clarify the extent to which improvements in sleep contribute to more holistic improvements for individuals with SAD over time.
Another important area of investigation is whether and how pre-treatment sleep difficulties may affect the progression and outcome of the original target of treatment for SAD. There are several reasons to conjecture that sleep difficulties may impede learning and dampen the effects of both CBT and mindfulness-based treatments for SAD, such as mindfulness-based stress reduction (MBSR). Accumulated evidence suggests that reduced sleep impairs the abilities to reason logically (Blagrove, Alexander, & Horne, 1995), sustain focus on complex cognitive tasks, and think flexibly (Gobin, Banks, Fins, & Tartar, 2015; Harrison & Horne, 1999; Horne, 1988), and improvements during both CBT and MBSR often rely on such cognitively taxing activities. For instance, cognitive reappraisal—defined as an emotion regulation strategy that involves modifying the meaning of a stimulus or context that gives rise to an emotion (Gross, 2013)—mediates improvements in social anxiety during CBT for SAD (Goldin et al., 2012; Goldin et al., 2016), and there is evidence to suggest that poorer sleep quality is associated with reduced ability to use cognitive reappraisal to decrease negative emotion (Mauss, Troy, & LeBourgeois, 2013). In addition, mindfulness-based treatments such as MBSR place a large emphasis on engaging attention and “mindful awareness” (Kabat-Zinn, 1990). However, because alertness and vigilance are the cognitive capacities most consistently and severely affected by poor sleep (Gobin et al., 2015; Goel et al., 2009; Lim & Dinges, 2008; McCarthy & Waters, 1997; Van Dongen et al., 2003), it also seems likely that individuals experiencing poor sleep quality may have difficulty cultivating the focused attention and awareness that are central to mindfulness-based treatment modalities. Other important mechanisms of treatment for SAD that may be affected by poor sleep include memory and learning; sleep has been shown to be important in supporting memory consolidation processes (Diekelmann & Born, 2010), and poor sleep likely interferes with the fear extinction learning that takes place in the exposure exercises integral to treatments like CBGT (e.g., Craske et al., 2008; Silvestri & Root, 2008). Few studies thus far have examined the dampening effect poor sleep quality may have on the improvement of social anxiety symptoms during treatment. Zalta and colleagues (2013) demonstrated that poorer baseline sleep quality was associated with slower improvement over time and poorer endpoint outcome among individuals in group CBT for SAD. However, the effect of poor sleep on improvement in social anxiety symptoms over the course of other efficacious treatments for SAD (e.g., MBSR) has not yet been examined. More work is needed to replicate and expand on initial supporting evidence that poor sleep quality is associated with worse outcomes in treatment for SAD.
In the present study, we examined four questions: (1) whether self-reported sleep quality differed in individuals with SAD compared to healthy controls, (2) whether sleep quality moderated treatment outcome in CBGT vs. MBSR vs. WL for SAD (3) whether sleep quality improved over the course of CBGT or MBSR relative to WL and to each other, and (4) whether changes in sleep quality during treatment predicted social anxiety 12 months post-treatment.
Hypothesis 1: We expected that individuals with SAD would report lower sleep quality compared to healthy controls. Hypothesis 2: We expected that sleep quality would moderate the effect of treatment on social anxiety symptoms, such that lower baseline sleep quality would be associated with less pronounced improvements in social anxiety symptoms for those in both CBGT and MBSR relative to WL. Hypothesis 3: We expected that sleep quality would significantly improve over the course of both CBGT and MBSR for SAD relative to WL, but not relative to each other. Hypothesis 4: We hypothesized that greater improvement in sleep quality over treatment would predict lower social anxiety symptoms 12 months post-treatment.
Method
Participants
Participants (N = 146) comprised 108 treatment-seeking adults with a primary diagnosis of generalized SAD according to DSM-IV (APA, 1994) who were enrolled in a RCT investigating the effects of CBGT vs. MBSR vs. WL for SAD (Goldin et al., 2016), as well as 38 healthy control participants (HCs). Sample characteristics are reported in Table 1. To be eligible for the RCT, participants had to be 18 years of age or older, have a primary diagnosis of generalized SAD as evidenced by greater than moderate fear in five or more distinct social situations listed in the social phobia module of the Anxiety Disorders Interview Schedule for the DSM-IV-Lifetime Version (ADIS-IV-L; Di Nardo, Brown, & Barlow, 1994), and score 60 or higher on the Liebowitz Social Anxiety Scale–Self-Report (LSAS-SR; Fresco et al., 2001; Liebowitz, 1987; Rytwinski et al., 2009). Participants were excluded if they had a lifetime history of neurological disorders, cardiovascular disorders, thought disorders, eating disorders, or bipolar disorder; significant symptoms of post-traumatic stress disorder or obsessive compulsive disorder; major depressive episode in the past month; current substance or alcohol abuse/dependence; pharmacotherapy, CBT for anxiety, or any other psychotherapy in the past year; or previous MBSR or long-term meditation experience. Less than half of participants in the RCT met criteria for one or more current comorbid conditions (42.6%), including generalized anxiety disorder (28.7%), specific phobia (17.6%), panic disorder (13%), agoraphobia (7.4%), dysthymia (6.5%), major depressive disorder (3.7%), and obsessive-compulsive disorder (0.9%). All participants gave informed consent. This study was approved by the Stanford University Institutional Review Board.
Table 1.
Sample demographic characteristics.
| SAD (n = 108) | HC (n = 38) | |
|---|---|---|
| Age (M[SD]) | 32.70 (7.99) | 32.02 (8.43) |
| Gender (% female) | 55.6% | 60% |
| Race/Ethnicity (%) | ||
| White | 43.5% | 52.5% |
| Black | 0.9% | 0% |
| Asian | 38.9% | 32.5% |
| American Indian/Alaskan Native | 0.9% | 0% |
| Hispanic | 9.3% | 7.5% |
| Mixed | 6.5% | 7.5% |
| Income (%) | ||
| <10,000 | 5.6% | 2.5% |
| 10-25,000 | 8.3% | 7.5% |
| 25-50,000 | 13.9% | 22.5% |
| 50-75,000 | 13.0% | 25.0% |
| 75-100,000 | 10.2% | 10.0% |
| >100,000 | 25.9% | 22.5% |
| Not reported | 22.2% | 10.0% |
| Current Axis I Comorbidity, (n, %) | ||
| Generalized anxiety disorder | 31 (28.7%) | |
| Specific phobia | 19 (17.6%) | |
| Panic disorder | 14 (13.0%) | |
| Major depressive disorder | 4 (3.7%) | |
| Dysthymic disorder | 7 (6.5%) | |
| Obsessive compulsive disorder | 1 (0.9%) |
Note. M(SD) = mean and standard deviation; SAD = social anxiety disorder; HC = healthy controls
Procedure
Participants completed measures of social anxiety and perceived sleep quality, among other measures not considered here (for details, see Goldin et al., 2016). HCs completed these measures only once. Participants with SAD completed these measures prior to randomization to CBGT (n = 36), MBSR (n = 36), or WL (n = 36)1 and after completion of treatment or waitlist. Additionally, participants assigned to WL were randomized to CBGT or MBSR following the 12-week waiting period but their outcomes are not further considered here. All participants receiving CBGT or MBSR completed SAD symptom measures again 12 months post-treatment.
CBGT and MBSR were each comprised of 12 weekly, 2.5-hour sessions conducted in a group format with six participants per group. The CBGT protocol incorporated psychoeducation, cognitive restructuring skills, graduated exposure to feared social situations (both within session and at home), and an emphasis on relapse prevention and termination (Heimberg & Becker, 2002). Portions of the protocol developed by Hope, Heimberg, and Turk (2010) were also incorporated into the group treatment. The MBSR protocol followed the standard outline designed by Kabat-Zinn (1993), with some modifications to the protocol to match the duration of the CBGT group. The intervention included training in body scan meditation, sitting meditation, and mindful stretching, as well as a focus on the application of mindfulness as a method for noticing reactions and responding in new ways in social situations. The intervention also included additional readings and mindfulness exercises to supplement ongoing practice (Stahl & Goldstein, 2010). Detailed information about the methodology of the parent RCT is available in the primary outcome paper (Goldin et al., 2016).
Measures
Diagnostic Assessment.
Diagnostic interviews were conducted at baseline using the ADIS-IV-L (Di Nardo et al., 1994). The ADIS has previously demonstrated excellent inter-rater reliability (Brown, Di Nardo, Lehman & Campbell, 2001). In the present study, interviews were conducted by doctoral-level or masters-level clinicians and trained doctoral students, and 20% of the interviews were reviewed to assess inter-rater reliability. There was 100% agreement with the original principal diagnosis of SAD (κ = 1.0) in this study.
Perceived Sleep Quality.
Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989), a widely-used scale for the measurement of subjective sleep disturbance. The scale consists of seven component items: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficacy, sleep disturbances, use of sleep medication, and daytime dysfunction over the last month. Component items are scored from 0 (Not during the past month/Very good) to 3 (Three or more times a week/Very bad) and summed to create a global PSQI score ranging from 0-21, with higher scores reflecting poorer sleep quality. A score of 5 has been shown to differentiate between good sleep quality (lower scores) and poor sleep quality (higher scores). The PSQI has exhibited adequate internal consistency (α = .80), high convergent validity with other measures of sleep quality (rs > .69; Carpenter & Andrykowski, 1998), and good test-retest reliability over a two-day period (r = .90) and a 1.5-2 month period (r = .86) (Backhaus, Junghanns, Broocks, Riemann, & Hohagen, 2002). Internal consistency of the PSQI was adequate in the current sample (α = .74).
Treatment Outcome.
The primary outcome measure for this study was the Liebowitz Social Anxiety Scale-Self Report (LSAS-SR; Fresco et al., 2001; Liebowitz, 1987; Rytwinski et al., 2009). The LSAS-SR is a 24-item scale that assesses patients’ fear and avoidance of social and performance situations. Each item asks individuals to rate both their fear and avoidance of a situation over the past week on a 4-point Likert-type scale, with a range from 0 (None/Never) to 3 (Severe/Usually). Item ratings are summed to create a total score ranging from 0-144. The LSAS-SR has demonstrated high internal consistency (α = .96; Rytwinski et al., 2009) and is highly correlated with the original clinician-administered version (rs = .85-.98 among individuals with SAD; Fresco et al., 2001). It is sensitive to treatment change (e.g., S. Baker, Heinrichs, Kim, & Hofmann, 2002; Goldin et al., 2012, 2016) and has demonstrated strong convergent validity (r = .62-.71) with other measures of social anxiety among individuals with SAD (Fresco et al., 2001). The measure has also demonstrated good test-retest reliability (r = .83) over a 12-week period (S. Baker et al., 2002). The LSAS-SR exhibited high internal consistency (α = .92) in the current study.
Missing Data
All 108 participants with SAD and 38 healthy controls had complete data at baseline. There were 6 participants with SAD who dropped out of the parent RCT and did not have post-treatment data. In addition to the 6 individuals who dropped out, an additional 11 participants (10.8% of completers) did not have full post-treatment data. To examine whether those missing data at post-treatment significantly differed from those with full data at post-treatment on clinical (treatment condition, baseline social anxiety severity) and demographic (gender, age, race/ethnicity) characteristics, a series of t-tests (for continuous baseline variables) and chi-square tests (for categorical variables) were conducted comparing these groups. Those with complete data at post-treatment and those with missing data at post-treatment did not significantly differ on any of the baseline clinical or demographic characteristic examined. Therefore, listwise deletion was used to handle missing data when examining baseline sleep quality as a moderator of the effects of treatment on social anxiety, as well as to examine sleep quality improvement over treatment.
Of participants in the CBGT or MBSR conditions, post-treatment LSAS data were missing for 17 participants in the full sample (23.6%) and for 12 participants in the completer sample (17.9%). Because there was a high number of missing data at follow-up, we used multiple imputation to handle missing data at 12 months post-treatment and to conduct analyses examining changes in sleep quality as a predictor of follow-up social anxiety. These analyses were run in Mplus Version 7.31 (Muthén & Muthén, 2015).
Results
Baseline sleep quality
Our first hypothesis was that individuals with SAD would report overall lower baseline sleep quality than HCs. To examine this question, we compared the pre-treatment sleep quality of individuals with SAD to that of HCs using an independent samples t-test. At baseline, individuals with SAD reported significantly poorer sleep quality than HCs. In addition, there was a significantly greater proportion of individuals with SAD who reported a global sleep quality score above the clinical cutoff of 5, with higher scores indicating poorer sleep quality (see Table 2 for complete results).
Table 2.
Baseline sleep quality comparisons.
| SAD vs. HC | Group differences | p | Effect size | |||
|---|---|---|---|---|---|---|
| SAD (n = 108) | HC (n = 38) | |||||
| Baseline PSQI (M[SD]) | 6.23(2.84) | 3.50(2.52) | t(144) = 5.24 | <.0001 | d = .68 | |
| PSQI clinical cut-off of 5 (% above) | 66.7% | 28.9% | χ2(1) = 16.30 | <.0001 | φ = .33 | |
| Treatment condition comparisons | ||||||
| CBGT (n = 36) | MBSR (n = 36) | WL (n = 36) | ||||
| Baseline PSQI (M[SD]) | 7.62(2.91) | 7.69(2.24) | 7.72(1.99) | F(2,105) = 0.34 | .71 | ηp2 = .006 |
| PSQI clinical cut-off of 5 (% above) | 58.3% | 72.2% | 69.4% | χ2 (2) = 0.18 | .42 | φ = .04 |
Note. M(SD) = mean and standard deviation; PSQI = Pittsburgh Sleep Quality Index; SAD = social anxiety disorder; HC = healthy controls; CBGT = cognitive-behavioral group therapy; MBSR = mindfulness-based stress reduction; WL = waitlist control
Among individuals with SAD, there were no significant differences in baseline sleep quality between participants in the CBGT, MBSR, and WL conditions. Using the cutoff score of 5 or above, there was no significant difference in distribution across groups of those who were considered poor sleepers at baseline (see Table 2).
Baseline sleep quality moderation of effect of treatments on social anxiety
As reported in Goldin et al. (2016), relative to WL, both CBGT and MBSR resulted in reliable and clinically significant improvement in social anxiety. In order to examine whether treatment condition (CBGT vs MBSR vs. WL) would differentially predict post-treatment social anxiety symptoms as a function of baseline sleep quality, we conducted a linear regression analysis. Treatment condition was dummy coded with WL as the reference group. Pre-treatment LSAS-SR and PSQI scores were mean-centered. The interaction between treatment condition and baseline sleep quality did not significantly predict outcome, as indexed by post-treatment social anxiety (LSAS-SR), controlling for baseline social anxiety (see Table 3).2
Table 3.
Results of multiple linear regression model of treatment condition predicting post-treatment social anxiety, moderated by baseline sleep quality.
| Step No. | Predictor | β | R | R2 Change |
|---|---|---|---|---|
| Step 1 | Baseline LSAS Total Baseline PSQI Total |
.43** −.12 |
.33 | .11** |
| Step 2 | CBGT (CBGT vs. WL) MBSR (MBSR vs. WL) |
−29.43** −21.86** |
.41 | .30*** |
| Step 3 | CBGT x baseline PSQI Total MBSR x baseline PSQI Total |
1.60 2.55 |
.42 | .02 |
Note.
p < .05,
p < .001;
p < .001;
LSAS = Liebowitz Social Anxiety Scale; PSQI = Pittsburgh Sleep Quality Index; CBGT = cognitive-behavioral group therapy dummy variable; MBSR = mindfulness based stress reduction dummy variable; WL = waitlist control; all baseline continuous variables are mean-centered.
Sleep quality improvement
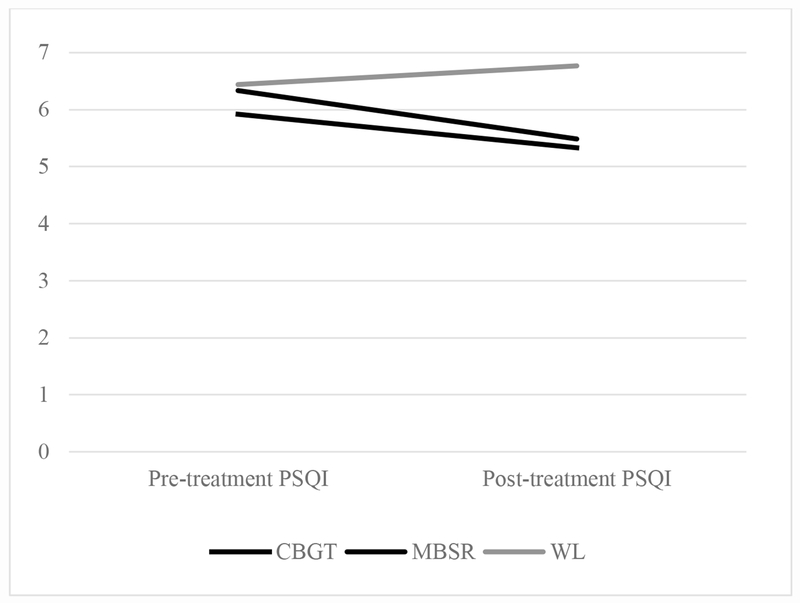
We next hypothesized that sleep quality would improve in both CBGT and MBSR relative to WL, but not relative to each other. We first examined whether there was an improvement in sleep quality from pre- to post-treatment in each treatment condition. Participants showed significant improvement in sleep quality over treatment in MBSR (Ftime(1,26) = 7.93, p < .01, ηp2 = .23) but not in CBGT (Ftime(1,29) = 1.42, p = .24, ηp2 = .05) or WL (Ftime(1,33) = 0.31, p = .58, ηp2 = .01). To examine our question of whether sleep quality improved in CBGT and MBSR relative to WL and to each other, we compared change in sleep quality from pre- to post-treatment in a series of 2 (time: pre-treatment, post-treatment) by 2 (treatment: CBGT vs WL, MBSR vs. WL, or CBGT vs. MBSR) mixed analyses of variance. Participants in MBSR showed significantly greater improvements in sleep quality compared to WL (F(1,59) = 6.55, p = .013, ηp2 = .10), but did not differ from those in CBGT (F(1,55) = 0.66, p = .42, ηp2 = .01). In addition, participants in CBGT did not show significant improvements in sleep relative to WL (F(1,62) = 1.78, p = .19, ηp2 = .03) (See Figure 1).
Figure 1.
Sleep quality significantly improved over treatment for the MBSR condition only. These changes were significant in comparison to WL, but not CBGT. PSQI = Pittsburgh Sleep Quality Index; MBSR = mindfulness-based stress reduction; CBGT = cognitive-behavioral group therapy; WL = waitlist control.
Change in sleep quality as a predictor of follow-up social anxiety
To examine whether treatment-related changes in sleep quality in the overall sample predicted follow-up social anxiety symptoms, we conducted a linear regression with a residualized change score for sleep quality predicting social anxiety symptoms 12 months post-treatment for participants receiving CBGT or MBSR, controlling for pre-treatment social anxiety. No association was found between changes in sleep quality from pre- to post-treatment and social anxiety symptoms at follow-up (β = .16, p =.28)
Discussion
Poor sleep is common and prevalent in anxiety disorders such as SAD. However, literature on the relationship between SAD and sleep dysfunction has not always been consistent, and little is known how sleep quality both affects and is affected by treatment for SAD. In the present study, we investigated differences in perceived sleep quality between individuals with SAD and healthy controls, sleep quality as a potential moderator of treatment outcome among individuals with SAD, changes in sleep quality over the course of treatment for SAD, as well as change in sleep quality over treatment as a predictor of social anxiety symptoms one year post-treatment.
Our first hypothesis, that sleep quality would be significantly lower among individuals with SAD compared to healthy controls, was supported. In addition, two-thirds of the study participants with SAD reported poor sleep quality at baseline, consistent with research suggesting that sleep disturbance is highly prevalent among individuals with anxiety disorders (Cox & Olatunji, 2016; Roth et al., 2006) including individuals with SAD (Ramsawh et al., 2009; Stein et al., 1993; Zalta et al., 2013).
Our second hypothesis was that baseline sleep quality would moderate the effect of treatment on outcome such that treatment gains for individuals in CBGT and MBSR would be less pronounced relative to WL among those with poor sleep quality at baseline. However, our results did not support this hypothesis; sleep quality was not a significant moderator of the relationship between treatment condition and outcome, suggesting that social anxiety outcome was not impacted by sleep quality. These results were surprising given existing evidence from one previous study that poor sleep quality had a significant influence on the course and outcome of social anxiety symptoms in group CBT for SAD (Zalta et al., 2013). There are a few possible explanations for this unexpected result. First, it is possible that sleep quality truly does not affect treatment outcome in the way that we would expect, despite accumulated research on the effect of sleep disturbance on important cognitive and attentional mechanisms (e.g. Gobin et al., 2015; Lim & Dinges, 2008) that are likely implicated in both CBGT and MBSR, as well Zalta et al.’s (2013) finding of a negative effect of poor baseline sleep quality on the course and outcome of CBT for SAD. In the current study, there were significant, but only moderate, effects of the difference in sleep quality between participants with SAD and healthy controls, which may perhaps indicate that, although individuals with SAD experience sleep difficulties, these are not severe enough to play a significant role in SAD symptomatology and treatment. Another possible explanation for these results is that, while many studies that examine the relationship of poor sleep and related deficits rely on manipulated sleep disturbance, including extensive sleep deprivation, to study these effects (e.g., Lim & Dinges, 2008), we relied on a measure of naturally-occurring sleep quality to examine the relationship between sleep quality and outcome. Therefore, it is possible that the effects were less pronounced then they would be under conditions in which sleep quality is manipulated (or, as stated above, in a sample with more severe sleep dysfunction).
Out next hypothesis was that that sleep quality would improve in both CBGT and MBSR relative to WL (but not relative to each other). Most research on the improvement of sleep during anxiety treatment is both limited to studies focused on anxiety disorders other than SAD and studies examining only CBT (Belleville et al., 2010). Few studies have examined whether sleep quality concomitantly improves during mindfulness-based treatments for anxiety, although some pilot research suggests that it does (Yook et al., 2008). Our results indicated that only individuals in the MBSR treatment condition reported significant improvements in sleep quality, both within-condition and relative to WL. Individuals in the CBGT condition experienced a non-significant improvement in sleep quality at post-treatment, and this was not different from WL. Furthermore, there was no significant difference between the MBSR and CBGT groups in changes in sleep quality over treatment. Overall, these results may suggest that mindfulness-based approaches may be particularly helpful in reducing sleep difficulties among individuals with SAD. One possible explanation for this finding is that although neither CBGT or MBSR involve any intervention specifically directed at sleep dysfunction, the mindfulness skills taught in MBSR are more easily generalizable by individuals with SAD and are able to address a broader range of symptoms in this population, including poor sleep.
Our final hypothesis, that changes in sleep quality over treatment would predict lower social anxiety 12 months post-treatment, was also not supported. Although there were improvements in sleep for some individuals in the study over the course of treatment, our findings suggest that these changes do not necessarily predict later improvement in social anxiety symptoms. These findings perhaps indicate that improvements in sleep quality that take place during treatment do not precede reduction in social anxiety symptoms, but instead may follow from positive treatment outcomes.
Our study had a few limitations that should be noted. One limitation of our study was its sole reliance on self-report measures of sleep quality. Although the investigation of perceived sleep quality is both important and informative in understanding the subjective experience of individuals undergoing treatment, some research suggests that self-report measures of sleep quality and duration are not as highly correlated with more objective measures of sleep quality, such as actigraphy and polysomnography, as they are with other subjective measures of sleep quality (Backhaus, Junghanns, Broocks, Riemann, Hohgen, 2002; F. Baker, Maloney, & Driver, 1999; Lauderdale, Knutson, Yan, Liu, & Rathouz, 2008). Therefore, it is possible that the associations between sleep quality and treatment outcome that we predicted may differ when examining objective versus subjective measures of sleep quality. Furthermore, the self-report measure used is a retrospective measure of sleep quality that asks participants to recall sleep difficulties over the past month. Other subjective measures, such as daily sleep diaries or a report of sleep quality more proximal to treatment sessions, may have proven more informative or pertinent to the questions of the current study.
Additionally, our study examined measures taken only at baseline and post-treatment. Because we did not examine week-to-week changes in sleep quality and outcome, our study may have been limited in elucidating our understanding of how sleep quality affects changes in social anxiety over the course of treatment. It is possible and likely that sleep quality affects anxiety symptoms on a week-to-week basis, as was shown in the Zalta et al. (2013) study. Because our study only measured sleep quality at two time points, we may not have accurately captured the ways in which sleep quality affects psychological symptoms over time. Alternatively, it may be the case that sleep quality is simply not a powerful predictor of treatment outcome over time. Our finding that changes in sleep quality over treatment did not significantly predict social anxiety 12 months post-treatments does seem to support this notion, indicating that improvements in sleep quality do not necessarily precede improvements in social anxiety.
Our study found that individuals with SAD report significantly lower sleep quality than healthy controls and that sleep quality improves over the course of MBSR, but not CBGT, for SAD. However, our study does not support the current literature on the relationship between poor sleep quality and poorer treatment outcome for SAD. Further studies are needed to replicate past findings on the relationship between sleep quality and SAD treatment outcome for a more conclusive understanding of these relationships, potentially adding more extensive measures of objective and subjective sleep quality over time. In addition, more research is needed to replicate our finding that sleep significantly improves over the course of MBSR treatment for SAD. These future directions will allow us to better understand if and under what conditions concurrent sleep interventions are a necessary augmentation to SAD treatment.
Acknowledgments
Disclosure of interest:
This research was supported by an NIMH Grant R01 MH092416, awarded to James J. Gross. Richard G. Heimberg is the author of the commercially available CBT protocol which was utilized in this study. None of the remaining authors of this manuscript have any financial interests or potential conflicts of interest.
Footnotes
ClinicalTrials.gov identifier: .
These numbers exclude one group randomized to MBSR, for which adherence ratings indicated non-adherence to the treatment protocol.
At the suggestion of an anonymous reviewer, we ran the same moderation analyses with six of the seven PSQI subscale scores (sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction) in addition to the total PSQI score. Results for all analyses were also non-significant, with no specific components of the PSQI at baseline moderating the relationship between treatment condition and post-treatment social anxiety. We do not report full details of these post hoc analyses here but will provide them to interested parties on request.
Data availability statement:
The data that support the findings of this study are available on request from the corresponding author, Richard G. Heimberg. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
References
- Aderka IM, Hofmann SG, Nickerson A, Hermesh H, Gilboa-Schechtman E, & Marom S (2012). Functional impairment in social anxiety disorder. Journal of Anxiety Disorders, 26, 393–400. doi: 10.1016/j.janxdis.2012.01.003 [DOI] [PubMed] [Google Scholar]
- Ancoli-Israel S, & Roth T (1999). Characteristics of insomnia in the United States: Results of the 1991 National Sleep Foundation Survey. I. Sleep, 22, 347–353. [PubMed] [Google Scholar]
- Alvaro PK, Roberts RM, & Harris JK (2013). A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep, 36, 1059–1068. doi: 10.5665/sleep.2810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders, 4th edition (DSM-IV). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, 5th edition (DSM-5). Arlington, VA: American Psychiatric Publishing. doi: 10.1176/appi.books.9780890425596.744053 [DOI] [Google Scholar]
- Backhaus J, Junghanns K, Broocks A, Riemann D, & Hohagen F (2002). Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. Journal of Psychosomatic Research, 53, 737–740. doi: 10.1016/s0022-3999(02)00330-6 [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, & Toney L (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13, 27–45. doi: 10.1177/1073191105283504 [DOI] [PubMed] [Google Scholar]
- Baker FC, Maloney S, & Driver HS (1999). A comparison of subjective estimates of sleep with objective polysomnographic data in healthy men and women. Journal of Psychosomatic Research, 47, 335–341. doi: 10.1016/s0022-3999(99)00017-3 [DOI] [PubMed] [Google Scholar]
- Baker SL, Heinrichs N, Kim HJ, & Hofmann SG (2002). The Liebowitz Social Anxiety Scale as a self-report instrument: A preliminary psychometric analysis. Behaviour Research and Therapy, 40, 701–715. doi: 10.1016/s0005-7967(01)00060-2 [DOI] [PubMed] [Google Scholar]
- Belleville G, Cousineau H, Levrier K, St-Pierre-Delorme ME, & Marchand A (2010). The impact of cognitive-behavior therapy for anxiety disorders on concomitant sleep disturbances: A meta-analysis. Journal of Anxiety Disorders, 24, 379–86. doi: 10.1016/j.janxdis.2010.02.010 [DOI] [PubMed] [Google Scholar]
- Blagrove M, Alexander C, & Horne JA (1995). The effects of chronic sleep reduction on the performance of cognitive tasks sensitive to sleep deprivation. Applied Cognitive Psychology, 9, 21–40. doi: 10.1002/acp.2350090103 [DOI] [Google Scholar]
- Brown TM, Black B, Uhde TW (1994). The sleep architecture of social phobia. Biological Psychiatry, 35, 420–421. doi: 10.1016/0006-3223(94)90009-4 [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, & Campbell LA (2001). Reliability of DSM-IV anxiety and mood disorders: implications for the classification of emotional disorders. Journal of Abnormal Psychology, 110, 49–58. doi: 10.1037/0021-843X.110.1.49 [DOI] [PubMed] [Google Scholar]
- Brozovich F, & Heimberg RG (2008). An analysis of post-event processing in social anxiety disorder. Clinical Psychology Review, 28, 891–903. doi: 10.1016/j.cpr.2008.01.002 [DOI] [PubMed] [Google Scholar]
- Buckner JD, Bernert RA, Cromer KR, Joiner TE, & Schmidt NB (2008). Social anxiety and insomnia: The mediating role of depressive symptoms. Depression and Anxiety, 25, 124–130. doi: 10.1002/da.20282 [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28, 193–213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Carpenter JS, & Andrykowski MA (1998). Psychometric evaluation of the Pittsburgh Sleep Quality Index. Journal of Psychosomatic Research, 45, 5–13. doi: 10.1016/s0022-3999(97)00298-5 [DOI] [PubMed] [Google Scholar]
- Cox RC, & Olatunji BO (2016). A systematic review of sleep disturbance in anxiety and related disorders. Journal of Anxiety Disorders, 37, 104–129. doi: 10.1016/j.janxdis.2015.12.001 [DOI] [PubMed] [Google Scholar]
- Craske MG, Kircanski K, Zelikowsky M, Mystkowski J, Chowdhury N, & Baker A (2008). Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy, 46, 5–27. doi: 10.1016/j.brat.2007.10.003 [DOI] [PubMed] [Google Scholar]
- Di Nardo PA, Brown TA, & Barlow DH (1994). Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L). New York, NY: Oxford University Press. [Google Scholar]
- Eng W, Coles ME, Heimberg RG, & Safren SA (2005). Domains of life satisfaction in social anxiety disorder: Relation to symptoms and response to cognitive-behavioral therapy. Journal of Anxiety Disorders, 19, 143–156. doi: 10.1016/j.janxdis.2004.01.007 [DOI] [PubMed] [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB, & Goetz D (2001). The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine, 31, 1025–1035. doi: 10.1017/s0033291701004056 [DOI] [PubMed] [Google Scholar]
- Gobin CM, Banks JB, Fins AI, & Tartar JL (2015). Poor sleep quality is associated with a negative cognitive bias and decreased sustained attention. Journal of Sleep Research, 24, 535–542. doi: 10.1111/jsr.12302 [DOI] [PubMed] [Google Scholar]
- Goel N, Rao H, Durmer J, & Dinges D (2009). Neurocognitive consequences of sleep deprivation. Seminars in Neurology, 29, 320–339. doi: 10.1055/s-0029-1237117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Morrison A, Jazaieri H, Brozovich F, Heimberg R, & Gross JJ (2016). Group CBT versus MBSR for social anxiety disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 84, 427–437. doi: 10.1037/ccp0000092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Ziv M, Jazaieri H, Werner K, Kraemer H, Heimberg RG, & Gross JJ (2012). Cognitive reappraisal self-efficacy mediates the effects of individual cognitive-behavioral therapy for social anxiety disorder. Journal of Consulting and Clinical Psychology, 80, 1034–1040. doi: 10.1037/a0028555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ (Ed.). (2013). Handbook of emotion regulation. New York, NY: Guilford Publications. [Google Scholar]
- Guastella AJ, & Moulds ML (2007). The impact of rumination on sleep quality following a stressful life event. Personality and Individual Differences, 42, 1151–1162. doi: 10.1016/j.paid.2006.04.028 [DOI] [Google Scholar]
- Hambrick JP, Turk CL, Heimberg RG, Schneier FR, & Liebowitz MR (2003). The experience of disability and quality of life in social anxiety disorder. Depression and Anxiety, 18, 46–50. doi: 10.1002/da.10110 [DOI] [PubMed] [Google Scholar]
- Harrison Y, & Horne JA (1999). One night of sleep loss impairs innovative thinking and flexible decision making. Organizational Behavior and Human Decision Processes, 78, 128–145. doi: 10.1006/obhd.1999.2827 [DOI] [PubMed] [Google Scholar]
- Harvey AG, & Payne S (2002). The management of unwanted pre-sleep thoughts in insomnia: Distraction with imagery versus general distraction. Behaviour Research and Therapy, 40, 267–277. doi: 10.1016/s0005-7967(01)00012-2 [DOI] [PubMed] [Google Scholar]
- Hjeltnes A, Molde H, Schanche E, Vøllestad J, Lillebostad Svendsen J, Moltu C, & Binder PE (2017). An open trial of mindfulness‐based stress reduction for young adults with social anxiety disorder. Scandinavian Journal of Psychology, 58, 80–90. doi: 10.1111/sjop.12342 [DOI] [PubMed] [Google Scholar]
- Horne JA (1988). Sleep loss and “divergent” thinking ability. Sleep, 11, 528–536. doi: 10.1093/sleep/11.6.528 [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (1993) Mindfulness Meditation: Health Benefits of an Ancient Buddhist Practice In: Goleman D and Garin J, Eds., Mind/Body Medicine, Consumer Reports, Yonkers, New York, 257–276. [Google Scholar]
- Kabat-Zinn J (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Dell Publishing. [Google Scholar]
- Katzelnick DJ, & Greist JH (2001). Social anxiety disorder: An unrecognized problem in primary care. Journal of Clinical Psychiatry, 62 (Suppl 1), 11–15. [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 709–709. doi: 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koszycki D, Benger M, Shlik J, & Bradwejn J (2007). Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behavior Research and Therapy, 45, 2518–2526. doi: 10.1016/j.brat.2007.04.011 [DOI] [PubMed] [Google Scholar]
- Lauderdale DS, Knutson KL, Yan LL, Liu K, & Rathouz PJ (2008). Self-reported and measured sleep duration: How similar are they? Epidemiology, 19, 838–845. doi: 10.1097/ede.0b013e318187a7b0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebowitz MR (1987). Social phobia. Modern Problems of Pharmacopsychiatry, 22, 141–173. doi: 10.1159/000414022 [DOI] [PubMed] [Google Scholar]
- Lim J, & Dinges DF (2008). Sleep deprivation and vigilant attention. Annals of the New York Academy of Sciences, 1129, 305–322. doi: 10.1196/annals.1417.002 [DOI] [PubMed] [Google Scholar]
- Mauss IB, Troy AS, & LeBourgeois MK (2013). Poorer sleep quality is associated with lower emotion-regulation ability in a laboratory paradigm. Cognition and Emotion, 27(3), 567–576. doi: 10.1080/02699931.2012.727783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy ME, & Waters WF (1997). Decreased attentional responsivity during sleep deprivation: Orienting response latency, amplitude, and habituation. Sleep, 20, 115–123. doi: 10.1093/sleep/20.2.115 [DOI] [PubMed] [Google Scholar]
- Mellman TA (2006). Sleep and anxiety disorders. Psychiatric Clinics of North America, 29, 1047–1058. 10.1016/j.psc.2006.08.005 [DOI] [PubMed] [Google Scholar]
- Mellman TA (2008). Sleep and anxiety disorders. Sleep Medicine Clinics, 3, 261–268. doi: 10.1016/j.jsmc.2008.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin CM, LeBlanc M, Daley M, Gregoire JP, & Merette C (2006). Epidemiology of insomnia: Prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Medicine, 7, 123–130. doi: 10.1016/j.sleep.2005.08.008 [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO (1998–2015). Mplus User’s Guide, Seventh Edition Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Norton AR, Abbott MJ, Norberg MM, & Hunt C (2015). A systematic review of mindfulness and acceptance-based treatments for social anxiety disorder. Journal of Clinical Psychology, 71, 283–301. doi: 10.1002/jclp.22144 [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, & Deacon BJ (2010). Efficacy of cognitive behavioral therapy for anxiety disorders: A review of meta-analytic findings. Psychiatric Clinics of North America, 33, 557–577. doi: 10.1016/j.psc.2010.04.002 [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, & Tolin DF (2007). Quality of life in the anxiety disorders: A meta-analytic review. Clinical Psychology Review, 27, 572–581. doi: 10.1016/j.cpr.2007.01.015 [DOI] [PubMed] [Google Scholar]
- Pace-Schott EF, Bottary R, Kim SY, Rosencrans P, Vijayakumar S, Orr SP, Lasko NB, Goetter EM, Baker AM, Bianchi MT, Gannon K, Hofmann SG, Simon NM (2018) Effects of post-exposure naps on exposure therapy for social anxiety. Psychiatry Research, 270, 523–530. doi: 10.1016/j.psychres.2018.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace-Schott EF, Germain A, & Milad MR (2015). Sleep and REM sleep disturbance in the pathophysiology of PTSD: The role of extinction memory. Biology of Mood & Anxiety Disorders, 5, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers MB, Sigmarsson SR, & Emmelkamp PM (2008). A meta-analytic review of psychological treatments for social anxiety disorder. International Journal of Cognitive Therapy, 1, 94–113. doi: 10.1680/ijct.2008.1.2.94 [DOI] [Google Scholar]
- Ramsawh HJ, Stein MB, Belik SL, Jacobi F, & Sareen J (2009). Relationship of anxiety disorders, sleep quality, and functional impairment in a community sample. Journal of Psychiatric Research, 43, 926–933. doi: 10.1016/j.jpsychires.2009.01.009 [DOI] [PubMed] [Google Scholar]
- Roth T, Jaeger S, Jin R, Kalsekar A, Stang PE, & Kessler RC (2006). Sleep problems, comorbid mental disorders, and role functioning in the National Comorbidity Survey Replication. Biological Psychiatry, 60, 1364–1371. doi: 10.1016/j.biopsych.2006.05.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, & Kessler RC (2007). Social fears and social phobia in the USA: Results from the National Comorbidity Survey Replication. Psychological Medicine, 38, 15–28. doi: 10.1017/s0033291707001699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rytwinski NK, Fresco DM, Heimberg RG, Coles ME, Liebowitz MR, Cissell S, Hofmann SG (2009). Screening for social anxiety disorder with the self-report version of the Liebowitz Social Anxiety Scale. Depression and Anxiety, 26, 34–38. doi: 10.1002/da.20503 [DOI] [PubMed] [Google Scholar]
- Silvestri AJ, & Root DH (2008). Effects of REM deprivation and an NMDA agonist on the extinction of conditioned fear. Physiology & Behavior, 93, 274–281. doi: 10.1016/j.physbeh.2007.08.020 [DOI] [PubMed] [Google Scholar]
- Simon EB, & Walker MP (2018). Sleep loss causes social withdrawal and loneliness. Nature Communications, 9, 1–9. doi: 10.1038/s41467-018-05377-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahl B, & Goldstein E (2010). A mindfulness-based stress reduction workbook. Oakland, CA: New Harbinger Publications. [Google Scholar]
- Stein MB, Kroft CD, & Walker JR (1993). Sleep impairment in patients with social phobia. Psychiatry Research, 49, 251–256. doi: 10.1016/0165-1781(93)90065-O [DOI] [PubMed] [Google Scholar]
- Van Dongen HP, Maislin G, Mullington JM, & Dinges DF (2003). The cumulative cost of additional wakefulness: Dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep, 26, 117–129. doi: 10.1093/sleep/26.2.117 [DOI] [PubMed] [Google Scholar]
- Verwoerd J, de Jong PJ, & Wessel I (2008). Low attentional control and the development of intrusive memories following a laboratory stressor. Journal of Psychopathology and Behavioral Assessment, 30, 291–297. doi: 10.1007/s10862-008-9080-6 [DOI] [Google Scholar]
- Yook K, Lee SH, Ryu M, Kim KH, Choi TK, Suh SY, & Kim MJ (2008). Usefulness of mindfulness-based cognitive therapy for treating insomnia in patients with anxiety disorders: A pilot study. The Journal of Nervous and Mental Disease, 196, 501–503. doi: 10.1097/nmd.0b013e31817762ac [DOI] [PubMed] [Google Scholar]
- Zalta AK, Dowd S, Rosenfield D, Smits JA, Otto MW, Simon NM, & Pollack MH (2013). Sleep quality predicts treatment outcome in CBT for social anxiety disorder. Depression and Anxiety, 30, 1114–1120. doi: 10.1002/da.22170 [DOI] [PMC free article] [PubMed] [Google Scholar]