Abstract
Background: Despite the availability of a universal influenza vaccination program in the United States and Canada, seasonal influenza vaccine (SIV) uptake among the elderly remains suboptimal. Understanding the factors that determine SIV uptake in this important population subgroup is essential for designing effective interventions to improve seasonal influenza vaccination among the elderly. We evaluated the determinants of SIV uptake in the elderly in the United States and Canada. Methods: We systematically searched relevant bibliographic databases and websites from 2000 to 2017 for population-based clinical trials or observational studies conducted in community-based elderly individuals in the United States or Canada, irrespective of health status. Two reviewers independently screened the identified citations for eligibility using a two-stage sifting approach to review the title/abstract and full-text article. We gathered data on determinants of uptake (any vaccine receipt) and adherence (receipt of vaccine in more than one season) to seasonal influenza vaccination. Where possible, we pooled the data using inverse variance methods to minimize the variance of the weighted average. Results: Five cross-sectional studies on SIV uptake (none on adherence) from the United States met our eligibility criteria. Being older (pooled odds ratio [POR] = 1.44, 95% Confidence Interval [CI] = 1.11, 1.86); White (POR = 1.33, 95% CI = [1.10, 1.64]); and having higher income (POR = 1.06, 95% CI = [1.04, 1.09]); and health insurance (POR = 1.40, 95% CI = [1.25, 1.55]) were associated with increased SIV uptake. Conclusion: Older, ethnically White, higher income elderly individuals with access to health insurance coverage and a regular health care provider have higher SIV uptake in the United States. There was limited evidence for other socioeconomic and health-related determinants. Further studies are needed to provide an evidence base for planning more effective influenza vaccination programs in the United States.
Keywords: systematic review/meta-analysis, seasonal influenza vaccination, uptake/adherence, elderly, determinants, United States, Canada
Introduction
Influenza remains a major public health concern in Canada and the United States, with a substantial disease and economic burden. An estimated 12,200 hospitalizations and 3,500 deaths are associated with influenza every year in Canada (Schanzer, Sevenhuysen, Winchester, & Mersereau, 2013). In the United States, an estimated 9.2 to 35.6 million illnesses, 140,000 to 710,000 hospitalizations, and 12,000 to 56,000 deaths have been attributable to influenza annually since 2010 (Centers for Disease Control and Prevention, 2017).
Both countries have implemented vaccination programs to prevent influenza and to reduce the impact of influenza outbreaks. In both countries, annual administration of seasonal influenza vaccines (SIVs) is recommended for groups at higher risk of serious illness and death due to influenza, including pregnant women, people with chronic diseases, and those 65 years or older (henceforth, elderly) (Grohskopf et al., 2017; National Advisory Committee on Immunization, 2017). However, SIV uptake among the elderly in both countries remains suboptimal even in jurisdictions with universal influenza immunization programs. For instance, only about 65% of elderly Canadians received the SIV during the 2015/2016 season (Public Health Agency of Canada, 2017); a figure that is consistent with estimates of vaccine uptake among this age group from the United States (Lu, O’Halloran, Ding, Greby, & Williams, 2015; Mereckiene et al., 2010). The number of those who consistently receive SIV yearly is likely much lower, although these figures are not known with certainty (Mahmud et al., 2012).
Generally, a person’s knowledge, perceptions, and attitudes toward influenza vaccination are important determinants of SIV uptake (Kamimura et al., 2017; Mytton, O’Moore, Sparkes, Baxi, & Abid, 2013). However, personal characteristics, such as gender and socioeconomic status, as well as health care provider and health care system characteristics, could either facilitate or hinder vaccine uptake and adherence. Given so many plausible determinants of SIV uptake, to date, the available evidence has not been well summarized. Understanding these factors and their interactions is essential for designing effective interventions to improve SIV uptake and adherence. It is also important for effective planning, optimization, and evaluation of influenza vaccination programs and for public health decision making.
We undertook a systematic review to identify, critically appraise, and summarize the findings of published studies that examined determinants of SIV uptake and adherence among the elderly in the United States and Canada.
Methods
We undertook a systematic review following the Cochrane Handbook for Systematic Reviews of Interventions guidelines (Higgins & Green, 2011), and reported the findings following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher, Liberati, Tetzlaff, Altman, & Group, 2010). As per best practice, we developed and registered a systematic review protocol prior to executing our search strategy (Protocol Registration: PROSPERO CRD42018086803). The review team consisted of two methodologists, a reviewer, a librarian, and a content expert.
Eligible studies included clinical trials or observational studies carried out in the years 2000 to 2017 in the United States or Canada that recruited community-based elderly persons, irrespective of health status. Our decision to search for literature from 2000 was because a publicly funded influenza vaccination program was first introduced in Canada in 1999 (Hilderman et al., 2011), and in the United States in 1993, but became only widely available toward the end of the 1990s (Hinman, Orenstein, & Rodewald, 2004). Only study results published in a full-text English manuscript were considered for inclusion. We were interested in identifying any factors (henceforth, determinants) influencing uptake (any vaccine receipt) or adherence (receipt of vaccine in more than one season) to seasonal influenza vaccination (Supplementary Table 1). We excluded studies of determinants of uptake or adherence to the 2009 pandemic vaccine; studies based on analysis of self-reported intentions or attitudes toward vaccination; noncommunity-based studies such as studies conducted in schools and personal care homes; mathematical modeling studies; and studies without a full-text manuscript (e.g., letter to the editor and conference abstract).
Search Strategy
A knowledge synthesis librarian designed the original search strategy, and this was peer-reviewed by a second, independent librarian using the Peer Review of Electronic Search Strategies (PRESS) checklist (McGowan et al., 2016). The final executed search strategy is listed in Supplementary Table 2. We searched MEDLINE (Ovid), Embase (Ovid), CINAHL (EbscoHost), and Scopus (Elsevier) bibliographic databases. We also searched relevant websites including www.cdc.gov, www.bccdc.ca, and www.who.int. We conducted all literature searches in January 2018.
Study Selection
Two reviewers independently screened the identified citations for eligibility using a two-stage sifting approach to review the title/abstract and full-text article. We recorded the number of ineligible citations at the abstract screening stage and both the number and reason for ineligibility at the full-text article screening stage. Disagreements during these screening stages were resolved by discussion or by involving a third reviewer, when necessary.
Data Extraction
We created a data extraction spreadsheet in MS Excel 2016 (Microsoft Corporation, Redmond, WA, USA) and piloted it on a small selection of studies. One reviewer independently extracted data from the included studies and a second reviewer independently checked the extracted data for errors. Disagreements were resolved by discussion between the two reviewers or by involving a third reviewer, when necessary. We extracted the following data: study details (study identifier, first author, year the study was conducted, year of publication, country, province/state/region, number of sites, funding source), study population (number of study participants, average age and range, sex), outcome (SIV uptake and adherence, and how they were measured), determinants included in the analysis (including how they were measured and represented in the analysis), results (multivariate effect estimates and associated 95% confidence intervals [CIs] of the association between each determinant and outcome), and details relevant to study quality assessment (see below).
Study Quality Assessment
Two reviewers independently assessed study quality using the National Institutes of Health (NIH) quality assessment tool for observational cohort and cross-sectional studies (NIH, 2014). This tool uses 14 criteria to assess and determine study quality including clarity of the research question and objectives; appropriateness of study population and participants’ selection; sample size justification; and quality of measurements and data analysis. We judged a study to be of high quality if it satisfied all assessed parameters; of good quality if it satisfied all but one parameter; of moderate quality if it did not satisfy two to four parameters; and of poor quality if it did not satisfy more than four parameters.
Data Synthesis and Analysis
Reported odds ratios and CIs for association between reported determinants and SIV uptake were converted to their natural logs and then pooled (where possible) using inverse variance methods to minimize the variance of the weighted average. Where pooling was not possible, we synthesized data narratively. We also provided tabular descriptions of specific study characteristics, quality assessments, and results from the included studies.
Results
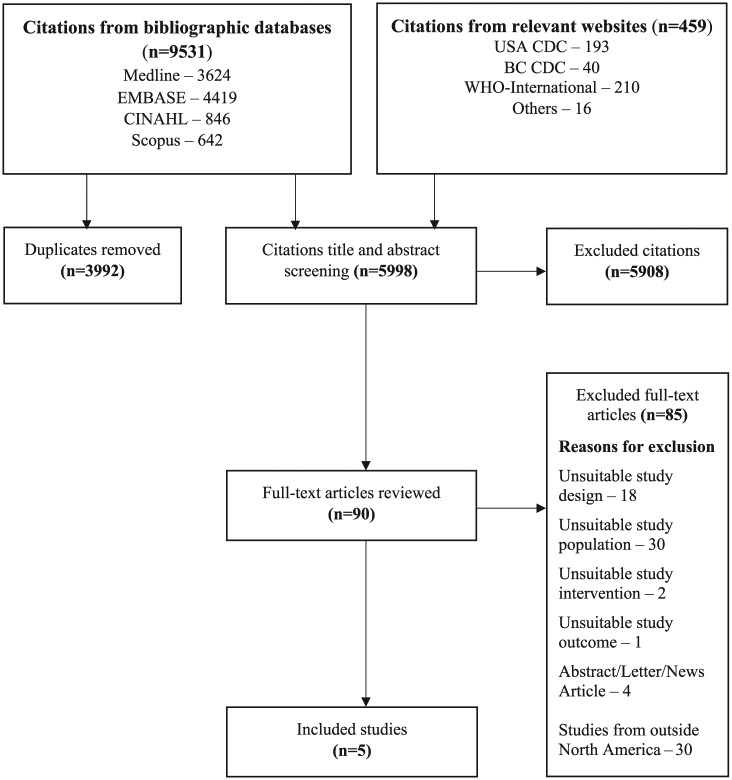
We identified 9,990 citations, of which only five cross-sectional studies met our inclusion criteria (see Figure 1 for details). The included studies were all conducted in the United States between 2001 and 2015, were published from 2005 to 2018, and were all focused on SIV uptake. We did not identify any Canadian studies or studies that reported on determinants for adherence to seasonal influenza vaccination. Of the included studies, one was limited to people who had three primary care visits in the previous 2 years (Appel, Everhart, Mehler, & MacKenzie, 2006) and one study excluded those who self-identified as Pacific Islanders or had a mixed-descent background (J. Y. Chen, Diamant, Pourat, & Kagawa-Singer, 2005). The other studies did not report their inclusion or exclusion criteria, but based on their findings, we believe they met our inclusion criteria. One study did not report the number of participants (La et al., 2018). The other studies had participants between 740 and 13,106,163 (Table 1).
Figure 1.
Summary of literature search and screening process (PRISMA flow diagram).
Note. CDC = Centers for Disease Control and Prevention; BC CDC = British Columbia Center for Disease Control; WHO = World Health Organization; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 1.
Characteristics of Included Studies (N = 5).
| Study (Design) |
Study year (State) |
Funding | Population (Number )Source |
Mean age (% male) |
Outcome (Effect estimate) |
Analysis type (Adjusted covariates) Data source |
Factors assessed |
|---|---|---|---|---|---|---|---|
|
Chen,
Diamant, Pourat, and Kagawa-Singer (2005)
(Cross-sectional design) |
2000-2001 (California) |
Robert Wood Johnson Foundation | ≥65 years old (10,724) Community-wide; random |
NR (NR) |
Vaccine uptake (OR) |
Multivariate (NR) Health interview survey |
Race/ethnicity |
|
Appel,
Everhart, Mehler, and MacKenzie (2006)
(Cross-sectional design) |
2001-2003 (Denver) |
NR | ≥66 years old (740) Community Health Centers |
74.5 years (35%) |
Vaccine uptake (OR) |
Multivariate (Gender; primary insurance; medical and psychiatric comorbidities; primary care site; age at end of audit year; primary care visit frequency) Chart audits |
Age; comorbidity; health insurance; hospital visits |
|
Takayama,
Wetmore, and Mokdad (2012)
(Cross-sectional design) |
2009 (National) |
NR | Adults but results reported for ≥65 years
old (134,101) Community-wide; random |
NR (NR) |
Vaccine uptake (OR) |
Multivariate (Age; sex; race; marital status; education; annual income; health care coverage; smoking; physical activity; fruit and vegetable consumption; BMI; frequency of poor physical health; history of hypertension; arthritis; asthma; diabetes; coronary heart disease; myocardial infarction, or stroke) Surveillance system database |
Age; race/ethnicity; marital status; level of education; annual income; health care coverage (insurance); smoking status; various individual chronic diseases |
|
Khan, Hall,
Tanner, and Marlow (2018)
(Cross-sectional design) |
2011-2015 (Florida) |
National Center for Birth Defects and Developmental Disability | ≥65 years old (13,106,163) Community-wide; random |
NR (50.4%) |
Vaccine uptake (OR) |
Multivariate (Age; gender; education; employment; income; marital status; Medicare; regular doctor; year of survey) Surveillance system database |
Age range; race/ethnicity; level of education; employment status; annual income; hospital visits; disability |
|
La et al.
(2018)
(Cross-sectional design) |
2011-2014 (10 states) |
GlaxoSmithKline Biologicals SA | Adults ≥ 65 years old (Unclear) Community-wide; random |
NR (NR) |
Vaccine uptake (OR) |
Multivariate (State of residence; sociodemographic status; health status characteristics; health behaviors) Surveillance system database |
Age range; gender; level of education; health status; last checkup |
Note. NR = not reported; OR = odds ratio; NR = not reported; BMI = body mass index.
The included studies examined sociodemographic characteristics, clinical factors, health behaviors, and organizational factors as determinants of SIV uptake, focusing on receipt of an SIV in the previous year and employing multivariable analysis. They all adjusted for varied demographic and socioeconomic characteristics, and health-seeking behaviors. One study was funded by industry (La et al., 2018), two studies were funded by nonindustry sources (J. Y. Chen et al., 2005; Khan, Hall, Tanner, & Marlow, 2018) and two studies did not report funding source (Table 1) (Appel et al., 2006; Takayama, Wetmore, & Mokdad, 2012).
Study Quality Assessment
Most of the studies did not report on the justification of their sample size (Appel et al., 2006; Khan et al., 2018; La et al., 2018; Takayama et al., 2012), and two studies did not apply well-defined eligibility criteria, having recruited participants from diverse populations at local, state, and national levels (La et al., 2018; Takayama et al., 2012). We judged one study to be of high quality, having satisfied all assessed parameters (J. Y. Chen et al., 2005). Two studies did not report on one assessed parameter (sample size justification) and were judged to be of good quality (Appel et al., 2006; Khan et al., 2018). A further two studies did not report on sample size justification and also did not apply participant eligibility uniformly and, as such, were judged to be of moderate quality (Supplementary Figure 1) (La et al., 2018; Takayama et al., 2012).
Individual Sociodemographic Determinants of SIV Uptake
Four studies examined the effect of age on SIV uptake; with age measured in 1-year increments in two studies (Appel et al., 2006; Takayama et al., 2012), and in groups in two studies (Khan et al., 2018; La et al., 2018). All studies showed a statistically significant increase in SIV uptake with advancing age. The pooled odds ratio (POR) was 1.01 (95% CI = [1.00, 1.03]) when age was measured in 1-year increments, and 1.44 (95% CI = [1.11, 1.86]) when comparison was made by age group (Table 2).
Table 2.
Meta-Analysis of Comparisons Between Reported Determinants and SIV Uptake.
| Determinants | Comparison made | Number of studies | Total population size | POR [95% CI] | I2 statistic (%) |
|---|---|---|---|---|---|
| Age | By one-year increment in age | 2 | 134,841 | 1.01 [1.00, 1.03] | 28.7 |
| Older age compared with younger age | 2 | Unclear | 1.44 [1.11, 1.86] | 26.4 | |
| Ethnicity | African Americans compared with Whites | 4 | Unclear | 0.60 [0.49, 0.73] | 37.6 |
| Hispanics compared with Whites | 2 | 13,116,887 | 0.69 [0.53, 0.89] | 63.6 | |
| Asians compared with Whites | 2 | 13,116,887 | 1.01 [0.50, 2.05] | 80.6 | |
| Ethnic minorities compared with Whites | 5 | Unclear | 0.75 [0.61, 0.91] | 86.1 | |
| Income | Low compared with high income | 2 | 13,106,163 | 0.94 [0.92, 0.96] | 0 |
| Marital status | Married compared with not married | 2 | 13,240,264 | 1.10 [0.89, 1.37] | 0 |
| Education | Higher compared with lower education | 3 | 13,240,264 | 1.28 [0.97, 1.68] | 74.4 |
| Comorbidity | Comorbidity compared with no comorbidity | 2 | Unclear | 1.31 [0.75, 2.30] | 71.6 |
| Health care insurance | Health insurance compared with no insurance | 4 | 13,285,379 | 1.40 [1.25, 1.55] | 0.1 |
Note. SIV = seasonal influenza vaccine; POR = pooled odds ratio; CI = confidence interval; Unclear = one study population size was not reported.
Note: Bold values shows statistically significant results.
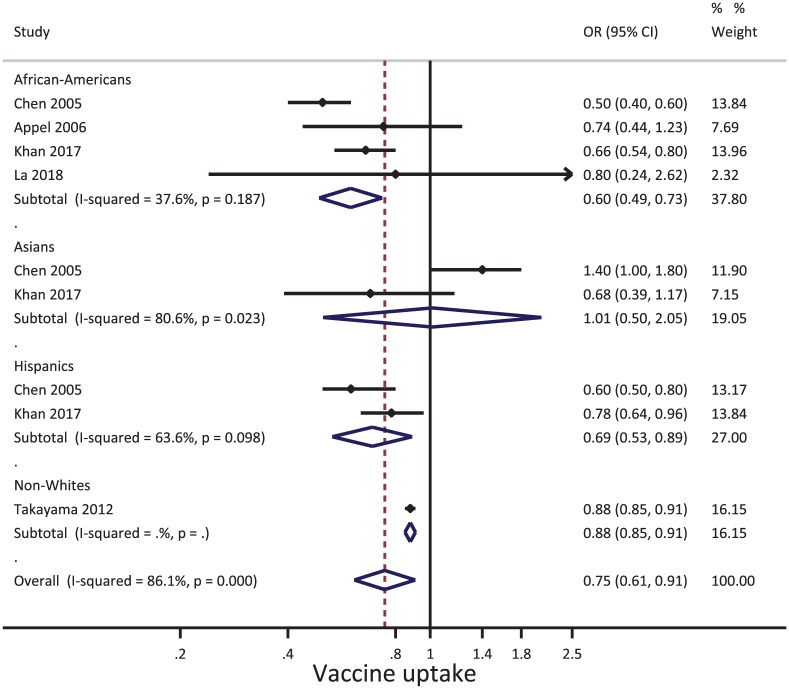
Only one study examined gender, reporting a nonstatistically significant association with SIV uptake: OR = 0.92, 95% CI = [0.59, 1.44] (La et al., 2018). All included studies examined the effect of ethnicity or “race” (Figure 2). Generally, ethnic minorities, compared with Whites, had lower SIV uptake (POR = 0.75; 95% CI = [0.61, 0.91]) albeit with substantial heterogeneity (I2 = 86.1%). All studies of African American and Hispanic people found lower SIV uptake than in White people with pooled estimates of 0.60 (95% CI = [0.49, 0.73]) for African Americans and 0.69 (95% CI = [0.53, 0.89]) for Hispanics. The two studies that compared Asians with Whites reported conflicting findings: a 40% higher uptake for Asians in one (J. Y. Chen et al., 2005) and 30% lower uptake for Asians in the other (Khan et al., 2018).
Figure 2.
Forest plot of the association between ethnicity (ethnic minorities compared with Whites) and seasonal influenza vaccine uptake.
Note. OR = odds ratio; CI = confidence interval.
Two studies examined the effect of annual income (Khan et al., 2018; Takayama et al., 2012). Earning a higher income was associated with increased SIV uptake (1.06, 95% CI = [1.04, 1.09]). Being married (two studies) (Khan et al., 2018; Takayama et al., 2012) and having a higher level of education (three studies) (Khan et al., 2018; La et al., 2018; Takayama et al., 2012) were both associated with increased vaccine uptake, although the pooled estimates were statistically nonsignificant and quite heterogeneous for the latter.
Clinical, Health Behavioral, and Organizational Determinants of SIV Uptake
Four studies examined clinical factors (Table 2) (Appel et al., 2006; Khan et al., 2018; La et al., 2018; Takayama et al., 2012). In pooled analyses, having unspecified comorbidity (two studies) (Appel et al., 2006; La et al., 2018) was associated with increased SIV uptake although the individual estimates were heterogeneous. Another study examined the effect of having a specified illness (hypertension, arthritis, asthma, diabetes, coronary heart disease, myocardial infarction, or stroke) (Takayama et al., 2012) and reported a statistically significant increase in SIV uptake for all illnesses except myocardial infarction and stroke (Supplementary Table 3). A fourth study found that having a disability was associated with increased SIV uptake (Khan et al., 2018).
A study that compared smokers against nonsmokers (Takayama et al., 2012) reported a small but statistically significant decrease in SIV uptake among smokers (OR 0.94, 95% CI = [0.89, 0.99]).
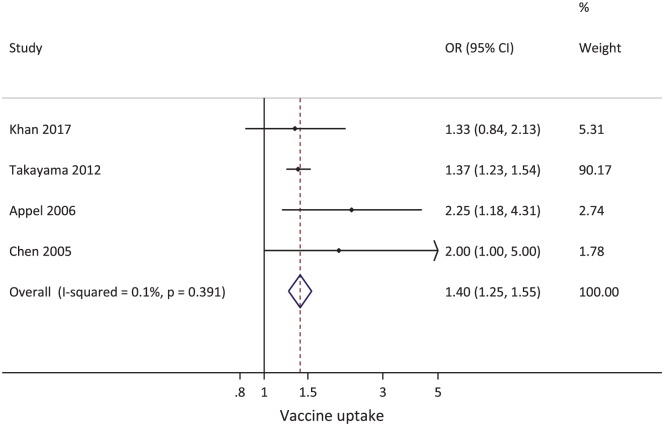
Four studies evaluated the effects of having health insurance on SIV uptake (Appel et al., 2006; J. Y. Chen et al., 2005; Khan et al., 2018; Takayama et al., 2012); all reporting higher SIV uptake among the insured (POR = 1.40, 95% CI = [1.25, 1.55]) (Figure 3).
Figure 3.
Forest plot of the association between health insurance (insured compared with uninsured) status and seasonal influenza vaccine uptake.
Note. OR = odds ratio; CI = confidence interval.
One study found that having a regular health care provider was associated with higher SIV uptake (OR = 2.18, 95% CI = [1.71, 2.79]) (Khan et al., 2018). Another study found that compared with having had a checkup within the past year, both having had a checkup 1 to 2 years ago and having had a checkup 2 years or more ago were associated with lower SIV uptake: OR = 0.33, 95% CI = [0.15, 0.72] and OR = 0.21, 95% CI = [0.06, 0.75], respectively (La et al., 2018).
Discussion
In this systematic review, we found that older, ethnically White, higher income elderly individuals with access to health care insurance coverage and a regular health care provider have higher SIV uptake in the United States. We found statistically significant lower SIV uptake among the elderly African Americans and Hispanics compared with Whites, but the two studies of the elderly Asians produced conflicting results, likely because of significant income differences between the included Asians populations.
It was not clear from the reviewed studies which factors contributed to lower SIV uptake among ethnic minorities. Ethnicity is associated with educational achievement (Hochschild & Shen, 2014; Maestri, 2017; Sander, 1992; Singleton, 1977), employment status, and income (Byars-Winston, Fouad, & Wen, 2015; Djamba & Kimuna, 2011; Zwysen & Longhi, 2018). For example, compared with Whites, ethnic minorities in the United States seem to have had a consistently lower income from 1988 to 2009 (Monnat, Raffalovich, & Tsao, 2012). Ethnicity (Ashton et al., 2003; Egede, 2006), income (Chokshi, 2018; Tumin, Menegay, Shrider, Nau, & Tumin, 2018), and education (Fletcher & Frisvold, 2009; Zajacova & Lawrence, 2018) have all been shown to influence access and utilization patterns of health care services in the United States. In addition, the extent of health care insurance coverage is often determined by an individual’s ethnicity, employment status, and income (J. Chen, Vargas-Bustamante, Mortensen, & Ortega, 2016; Fox & Shaw, 2014). Ethnicity is also a strong determinant of overall health status (D. R. Williams, Priest, & Anderson, 2016). The extent to which each of these factors has contributed to lower SIV uptake was not examined in the reviewed studies. However, a cross-sectional study of community-dwelling elderly Americans, utilizing data on influenza vaccination history from the 2010/2011 influenza season, and using the Blinder–Oaxaca decomposition method to assess characteristics associated with racial/ethnic disparities in influenza vaccination, found that only about 45% of unadjusted disparities in vaccination between ethnically Whites and African Americans, and between ethnically Whites and Spanish-speaking Hispanics, were due to differences in the distribution of varied sociodemographic variables (Yoo, Hasebe, & Szilagyi, 2015). A better understanding of the interplay of the other factors is essential to devising effective policy and program changes to increase SIV uptake among ethnic minorities. It is however noteworthy that what constitutes an ethnic group or ethnicity is hugely debatable, and that measure of ethnicity often differs between studies (Connelly, Gayle, & Lambert, 2016; M. Williams & Husk, 2013).
The strongest reported associations with SIV uptake were with having access to the services of a regular health care provider (120% increased uptake) and having had a recent checkup (200%). These findings are similar to the finding from an analysis of the 1999 National Health Interview Survey (NHIS) among adult Americans which showed that those with ≥10 physician visits annually were significantly associated with increased likelihood of receipt of the SIV (134%) compared with those with no physician visits (Egede, 2003). We also found that older elderly individuals were more likely to have received the SIV. This was similar to the finding by Ryu and colleagues (Ryu, Kim, Park, & Park, 2011), and may reflect increased incidence of chronic diseases and possibly having more frequent contact with health care providers.
Our findings confirm that some sociodemographic and economic factors influence SIV uptake among the elderly. Similar findings were observed for uptake of other vaccines (e.g., human papillomavirus (Agénor, Pérez, Peitzmeier, & Borrero, 2018), pneumococcal vaccines (Black et al., 2017; Daniels, Gouveia, Gildengorin, & Winston, 2006), and various vaccines for subgroups [adult diabetics] (Egede & Zheng, 2003)) in the United States. To the best of our knowledge, this study is the only available recent systematic review of determinants of SIV uptake among the elderly in the United States and Canada. A 2011 systematic review by Nagata et al. (2013) examined social determinants of seasonal influenza vaccination among the elderly globally and concluded that sociodemographic determinants such as age, sex, marital status, education, ethnicity, and others factors influenced seasonal influenza vaccination. However, this was a narrative synthesis and covered only social determinants, unlike our review which examined all determinants and involved meta-analyses. Yeung, Lam, and Coker (2016) systematically reviewed factors associated with the uptake of seasonal influenza vaccination, but in adults aged 18 to 64 years. They found that older age and having chronic diseases were strongly predictive of vaccination uptake. Dyda et al. (2016) systematically reviewed factors associated with influenza vaccination among adults, and, similar to our findings, old age, education and income were found to be determinants of seasonal influenza vaccination. However, the review was limited to Australian adults.
Limitations of the Reviewed Studies
Both the measurements of the outcome (receipt of influenza vaccine) and exposures (determinants) were self-reported in the included studies, which increases the likelihood for reporting, social desirability, and recall biases. The studies were conducted in different regions/states of the United States, so it is difficult to separate individual effects from regional effects (e.g., effectiveness of vaccine policies and programs). There were also differences between studies in categorization of variables, reference groups used in the analyses, and how statistical models were constructed, which may explain the heterogeneity in some of their findings.
Review Limitations
We included only full-text articles of studies published in English. This was because of the lack of resources to support professional translation of articles. However, none of the retrieved citations and full-text articles were in any language other than English. Moreover, it is expected that a study conducted in the United States or Canada would be reported in English, even if also reported in Spanish (in some regions of the United States) or French (in Canada). Our decision to only include papers published since 2000 limited the number of included studies, but allowed us to focus on recent and possibly more relevant literature published since influenza vaccination became freely available for the elderly in the United States and Canada. The small number of studies did not permit subgroup analyses according to study characteristics as we originally intended and also did not allow for formal assessment of publication bias in the reporting of the determinants assessed.
Review Strengths
Based on good practice, we registered a protocol in PROSPERO prior to executing our search strategy, and we conducted the review to the highest expected standards and reported in accordance to the PRISMA guidelines. Appropriate bibliographic databases were duly searched for literature using a peer-reviewed and piloted comprehensive literature search strategy. The quality of included studies was properly assessed using the NIH quality assessment tool for observational cohort and cross-sectional studies.
Conclusion
We found that older, ethnically White, higher income elderly individuals with access to health insurance coverage and a regular health care provider have higher SIV uptake in the United States. We found statistically significant lower SIV uptake in elderly African Americans and Hispanics. There was limited evidence for other socioeconomic and health-related determinants of SIV uptake among the elderly. More research is needed to provide a stronger evidence base for planning more effective influenza vaccine policies and programs in the United States.
Supplemental Material
Supplemental material, GGM870345_Supplementary_material_CLN for Determinants of Seasonal Influenza Vaccine Uptake Among the Elderly in the United States: A Systematic Review and Meta-Analysis by George N. Okoli, Ahmed M. Abou-Setta, Christine J. Neilson, Ayman Chit, Edward Thommes and Salaheddin M. Mahmud in Gerontology and Geriatric Medicine
Footnotes
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: A.C. and E.T. are employees of Sanofi Pasteur, Swiftwater, PA, USA. S.M. has received unrestricted research grants from GlaxoSmithKline, Merck, Sanofi Pasteur, Pfizer, and Roche-Assurex for unrelated studies.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by a research grant from Sanofi Pasteur, Swiftwater, PA, USA.
ORCID iD: George N. Okoli  https://orcid.org/0000-0002-6437-930X
https://orcid.org/0000-0002-6437-930X
Supplemental Material: Supplemental material for this article is available online.
References
- Agénor M., Pérez A. E., Peitzmeier S. M., Borrero S. (2018). Racial/ethnic disparities in human papillomavirus vaccination initiation and completion among U.S. women in the post-Affordable Care Act era. Ethnicity & Health, 18, 1-15. doi: 10.1080/13557858.2018.1427703 [DOI] [PubMed] [Google Scholar]
- Appel A., Everhart R., Mehler P. S., MacKenzie T. D. (2006). Lack of ethnic disparities in adult immunization rates among underserved older patients in an urban public health system. Medical Care, 44, 1054-1058. [DOI] [PubMed] [Google Scholar]
- Ashton C. M., Haidet P., Paterniti D. A., Collins T. C., Gordon H. S., O’Malley K., . . .Street R. L. (2003). Racial and ethnic disparities in the use of health services: Bias, preferences, or poor communication? Journal of General Internal Medicine, 18, 146-152. doi: 10.1046/j.1525-1497.2003.20532.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black C. L., Williams W. W., Warnock R., Pilishvili T., Kim D., Kelman J. A. (2017). Pneumococcal vaccination among Medicare beneficiaries occurring after the advisory committee on immunization practices recommendation for routine use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults aged ≥65 years. Morbidity and Mortality Weekly Report, 66, 728-733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byars-Winston A., Fouad N., Wen Y. (2015). Race/ethnicity and sex in U.S. occupations, 1970-2010: Implications for research, practice, and policy. Journal of Vocational Behavior, 87, 54-70. doi: 10.1016/j.jvb.2014.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2017). 2015-2016 estimated influenza illnesses, medical visits, and hospitalizations averted by vaccination in the United States. Retrieved from https://www.cdc.gov/flu/about/disease/2015-16.htm
- Chen J., Vargas-Bustamante A., Mortensen K., Ortega A. N. (2016). Racial and ethnic disparities in health care access and utilization under the Affordable Care Act. Medical Care, 54, 140-146. doi: 10.1097/MLR.0000000000000467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J. Y., Diamant A., Pourat N., Kagawa-Singer M. (2005). Racial/ethnic disparities in the use of preventive services among the elderly. American Journal of Preventive Medicine, 29, 388-395. [DOI] [PubMed] [Google Scholar]
- Chokshi D. A. (2018). Income, poverty, and health inequality. Journal of the American Medical Association, 319, 1312-1313. [DOI] [PubMed] [Google Scholar]
- Connelly R., Gayle V., Lambert P. S. (2016). Ethnicity and ethnic group measures in social survey research. Methodological Innovations, 9, 1-10. doi: 10.1177/2059799116642885 [DOI] [Google Scholar]
- Daniels N. A., Gouveia S., Gildengorin G. L., Winston C. A. (2006). Acceptance of pneumococcal vaccine under standing orders by race and ethnicity. Journal of the National Medical Association, 98, 1089-1094. [PMC free article] [PubMed] [Google Scholar]
- Djamba Y. K., Kimuna S. R. (2011). The influence of race on employment status and earnings of African immigrant men in the United States. International Journal of Population Research, 2011, Article 305873. doi: 10.1155/2011/305873 [DOI] [Google Scholar]
- Dyda A., Karki S., Hayen A., MacIntyre C. R., Menzies R., Banks E., . . .Liu B. (2016). Influenza and pneumococcal vaccination in Australian adults: A systematic review of coverage and factors associated with uptake. BMC Infectious Diseases, 16(1), Article 515. doi: 10.1186/s12879-016-1820-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egede L. E. (2003). Association between number of physician visits and influenza vaccination coverage among diabetic adults with access to care. Diabetes Care, 26, 2562-2567. [DOI] [PubMed] [Google Scholar]
- Egede L. E. (2006). Race, ethnicity, culture, and disparities in health care. Journal of General Internal Medicine, 21, 667-669. doi: 10.1111/j.1525-1497.2006.0512.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egede L. E., Zheng D. (2003). Racial/ethnic differences in adult vaccination among individuals with diabetes. American Journal of Public Health, 93, 324-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher J. M., Frisvold D. E. (2009). Higher education and health investments: Does more schooling affect preventive health care use? Journal of Human Capital, 3, 144-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox J. B., Shaw F. E. (2014). Relationship of income and health care coverage to receipt of recommended clinical preventive services by adults—United States, 2011-2012. Morbidity and Mortality Weekly Report, 63, 666-670. [PMC free article] [PubMed] [Google Scholar]
- Grohskopf L. A., Sokolow L. Z., Broder K. R., Walter E. B., Bresee J. S., Fry A. M., Jernigan D. B. (2017). Prevention and control of seasonal influenza with vaccines: Recommendations of the advisory committee on immunization practices—United States, 2017-18 influenza season. MMWR: Recommendations and Reports, 66(2), 1-20. doi: 10.15585/mmwr.rr6602a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J. P. T., Green S. (2011). Cochrane handbook for systematic reviews of interventions. Available from https://handbook-5-1.cochrane.org/
- Hilderman T., Katz A., Derksen S., McGowan K., Chateau D., Kurbis C., . . .Reimer J. N. (2011). Manitoba immunization study. Retrieved from http://mchp-appserv.cpe.umanitoba.ca/reference/MB_Immunization_Report_WEB.pdf
- Hinman A. R., Orenstein W. A., Rodewald L. (2004). Financing immunizations in the United States. Clinical Infectious Diseases, 38, 1440-1446. doi: 10.1086/420748 [DOI] [PubMed] [Google Scholar]
- Hochschild J. L., Shen F. X. (2014). Race, ethnicity, and education policy. In Leal D. L., Lee T., Sawyer M. (Eds.), Oxford handbook of racial and ethnic politics in America (pp. 1-30). New York, NY: Oxford University Press. [Google Scholar]
- Kamimura A., Trinh H. N., Weaver S., Chernenko A., Nourian M. M., Assasnik N., Nguyen H. (2017). Knowledge and perceptions of influenza vaccinations among college students in Vietnam and the United States. Journal of Preventive Medicine & Public Health, 50, 268-273. doi: 10.3961/jpmph.17.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S. R., Hall A. G., Tanner R. J., Marlow N. M. (2018). Association between race/ethnicity and disability status and receipt of vaccines among older adults in Florida. Disability and Health Journal, 11, 339-344. [DOI] [PubMed] [Google Scholar]
- La E. M., Trantham L., Kurosky S. K., Odom D., Aris E., Hogea C. (2018). An analysis of factors associated with influenza, pneumococcal, Tdap, and herpes zoster vaccine uptake in the US adult population and corresponding inter-state variability. Human Vaccines & Immunotherapeutics, 14, 430-441. doi: 10.1080/21645515.2017.1403697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu P.-J., O’Halloran A., Ding H., Greby S. M., Williams W. W. (2015). Current status and uptake of influenza vaccination over time among senior adults in the United States. Human Vaccines & Immunotherapeutics, 11, 2849-2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maestri V. (2017). Can ethnic diversity have a positive effect on school achievement? Education Economics, 25, 290-303. doi: 10.1080/09645292.2016.1238879 [DOI] [Google Scholar]
- Mahmud S. M., Van Caeseele P., Hammond G., Kurbis C., Hilderman T., Elliott L. (2012). No association between 2008–09 influenza vaccine and influenza A(H1N1)pdm09 virus infection, Manitoba, Canada, 2009. Emerging Infectious Diseases, 18(5), 801-810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan J., Sampson M., Salzwedel D. M., Cogo E., Foerster V., Lefebvre C. (2016). PRESS peer review of electronic search strategies: 2015 guideline statement. Journal of Clinical Epidemiology, 75, 40-46. doi: 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- Mereckiene J., Cotter S., D’Ancona F., Giambi C., Nicoll A., Levy-Bruhl D., . . .O’Flanagan D. (2010). Differences in national influenza vaccination policies across the European Union, Norway and Iceland 2008-2009. Euro Surveillance, 15(44), Article 19700. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G., Group P. (2010). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery, 8(5), 336-341. doi: 10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- Monnat S. M., Raffalovich L. E., Tsao H. (2012). Trends in the family income distribution by race/ethnicity and income source, 1988-2009. Population Review, 51, 85-115. [PMC free article] [PubMed] [Google Scholar]
- Mytton O. T., O’Moore E. M., Sparkes T., Baxi R., Abid M. (2013). Knowledge, attitudes and beliefs of health care workers towards influenza vaccination. Occupational Medicine, 63, 189-195. doi: 10.1093/occmed/kqt002 [DOI] [PubMed] [Google Scholar]
- Nagata J. M., Hernandez-Ramos I., Kurup A. S., Albrecht D., Vivas-Torrealba C., Franco-Paredes C. (2013). Social determinants of health and seasonal influenza vaccination in adults ≥65 years: A systematic review of qualitative and quantitative data. BMC Public Health, 13, Article 388. doi: 10.1186/1471-2458-13-388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Advisory Committee on Immunization. (2017). A Advisory Committee Statement: Canadian immunization guide chapter on influenza and statement on seasonal influenza vaccine for 2017-2018. Ottawa, Ontario: Government of Canada. [Google Scholar]
- National Institutes of Health. (2014). Quality assessment tool for observational cohort and cross-sectional studies. Retrieved from https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- Public Health Agency of Canada. (2017). Influenza vaccine uptake: Results from the 2015/16 national influenza immunization coverage survey in Canada. Retrieved from https://www.canada.ca/en/public-health/services/publications/healthy-living/vaccine-uptake-results-2015-16-national-influenza-immunization-coverage-survey.html
- Ryu S. Y., Kim S. H., Park H. S., Park J. (2011). Influenza vaccination among adults 65 years or older: A 2009-2010 community health survey in the Honam region of Korea. International Journal of Environmental Research and Public Health, 8, 4197-4206. doi: 10.3390/ijerph8114197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sander W. (1992). The effects of ethnicity and religion on educational attainment. Economics of Education Review, 11, 119-135. [Google Scholar]
- Schanzer D. L., Sevenhuysen C., Winchester B., Mersereau T. (2013). Estimating influenza deaths in Canada, 1992-2009. PLoS ONE, 8(11), e80481. doi: 10.1371/journal.pone.0080481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singleton J. (1977). Education and ethnicity. Comparative Education Review, 21, 329-344. doi: 10.1086/445946 [DOI] [Google Scholar]
- Takayama M., Wetmore C. M., Mokdad A. H. (2012). Characteristics associated with the uptake of influenza vaccination among adults in the United States. Preventive Medicine, 54, 358-362. [DOI] [PubMed] [Google Scholar]
- Tumin D., Menegay M., Shrider E. A., Nau M., Tumin R. (2018). Local income inequality, individual socioeconomic status, and unmet healthcare needs in Ohio, USA. Health Equity, 2(1), 37-44. doi: 10.1089/heq.2017.0058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., Priest N., Anderson N. (2016). Understanding associations between race, socioeconomic status and health: Patterns and prospects. Health Psychology, 35, 407-411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams M., Husk K. (2013). Can we, should we, measure ethnicity? International Journal of Social Research Methodology, 16, 285-300. doi: 10.1080/13645579.2012.682794 [DOI] [Google Scholar]
- Yeung M. P., Lam F. L., Coker R. (2016). Factors associated with the uptake of seasonal influenza vaccination in adults: A systematic review. Journal of Public Health, 38, 746-753. doi: 10.1093/pubmed/fdv194 [DOI] [PubMed] [Google Scholar]
- Yoo B., Hasebe T., Szilagyi P. G. (2015). Decomposing racial/ethnic disparities in influenza vaccination among the elderly. Vaccine, 33, 2997-3002. doi: 10.1016/j.vaccine.2015.03.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajacova A., Lawrence E. M. (2018). The relationship between education and health: Reducing disparities through a contextual approach. Annual Review of Public Health, 39, 273-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwysen W., Longhi S. (2018). Employment and earning differences in the early career of ethnic minority British graduates: The importance of university career, parental background and area characteristics. Journal of Ethnic and Migration Studies, 44, 154-172. doi: 10.1080/1369183x.2017.1338559 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, GGM870345_Supplementary_material_CLN for Determinants of Seasonal Influenza Vaccine Uptake Among the Elderly in the United States: A Systematic Review and Meta-Analysis by George N. Okoli, Ahmed M. Abou-Setta, Christine J. Neilson, Ayman Chit, Edward Thommes and Salaheddin M. Mahmud in Gerontology and Geriatric Medicine