Abstract
Aims:
The Veterans Health Administration (VA) promotes evidence-based complementary and integrative health (CIH) therapies as non-pharmacological approaches for chronic pain. We aimed to examine CIH use by gender among veterans with chronic musculoskeletal pain, and variations in gender differences by race/ethnicity and age.
Methods:
We conducted secondary analysis of electronic health records provided by all women (n=79,537) and men (n=389,269) veterans age 18–54 with chronic musculoskeletal pain who received VA-provided care between 2010–2013. Using gender-stratified multivariate binary logistic regression, we examined predictors of CIH use, tested a race/ethnicity-by-age interaction term, and conducted pairwise comparisons of predicted probabilities.
Results:
Among veterans with chronic musculoskeletal pain, more women than men use CIH (36% vs. 26%), with rates ranging from 25%−42% among women and 15%−29% among men, depending on race/ethnicity and age. Among women, patients under age 44 or Hispanic, White, or patients of other race/ethnicities are similarly likely to use CIH; in contrast, Black women, regardless of age, are least likely to use CIH. Among men, White and Black patients, and especially Black men under age 44, are less likely to use CIH than men of Hispanic or other racial/ethnic identities.
Conclusions:
Women veteran patients with chronic musculoskeletal pain are more likely than men to use CIH therapies, with variation in CIH use rates by race/ethnicity and age. Tailoring CIH therapy engagement efforts to be sensitive to gender, race/ethnicity, and age could reduce differential CIH use and thereby help to diminish existing health disparities among veterans.
Keywords: gender differences, race/ethnic differences, complementary and integrative health (CIH), complementary and alternative medicine (CAM), pain, musculoskeletal disorders, military veterans, Electronic Health Records (EHR)
Introduction
Opioid misuse and chronic pain among women military veterans
A national public health emergency, the opioid epidemic has resulted in extraordinary numbers of accidental injuries, infectious diseases, and premature deaths (Hedegaard et al., 2017; U.S. Surgeon General, 2016), contributing to a historically unprecedented shortening of American life expectancy (Kochanek et al., 2017). U.S. military veterans being treated for chronic pain are at a heightened risk for these adverse outcomes (Bohnert et al., 2014; Gaither et al., 2016), and women veterans may be especially impacted. Specifically, more women veterans than men are prescribed opioids for chronic pain (Kroll-Desrosiers et al., 2016; Mosher et al., 2015) and women veterans are more likely to have multiple pain condition diagnoses (Higgins et al., 2017; Weimer et al., 2014), self-report moderate to severe pain (Higgins et al., 2017), and have co-occurring mental health problems (Finlay et al., 2015; Higgins et al., 2017; Howe et al., 2014). These factors are well-established predictors of adverse health outcomes among veterans with chronic pain (Dobscha et al., 2013; Edlund et al., 2007). Findings underscore a critical need to better understand the gender-specific health services needs, utilization, and outcomes of veterans being treated for chronic pain.
Limited research on CIH and gender in veterans
Historically, opioid medications have been used in Veteran Healthcare Administration (VA) clinical settings despite acceptability of non-pharmacologic therapies for many pain patients (Howe and Sullivan, 2014; Simmonds et al., 2015). Signifying a major shift in practice, complementary and integrative health (CIH) therapies (e.g., meditation, yoga, acupuncture) are now being offered throughout the VA as non-pharmacological approaches for chronic pain because they have been found to be beneficial for some types of chronic pain and its physical and mental health comorbidities (Bawa et al., 2015; Goyal et al., 2014; Hempel et al., 2014; Hilton et al., 2017; MacPherson et al., 2017; Miake-Lye et al., 2016; Nahin et al., 2016). Expansion of the provision of CIH therapies as a non-pharmacological treatment for pain in the VA was mandated by Congress in the 2016 Comprehensive Addiction and Recovery Act (CARA) (U.S. Government Publishing Office, 2016). However, most of what is known about utilization of CIH therapies has been provided by general population studies of civilians (Clarke et al., 2015; Nahin et al., 2016; Stussman et al., 2012; Upchurch and Rainisch, 2015). Such studies report that common correlates of CIH utilization are diagnosed chronic physical and mental health conditions (Adams et al., 2017; Burke et al., 2017; Cramer et al., 2016a,b) and also sociodemographic characteristics (Zhang et al., 2016), particularly female gender (Burke et al., 2017; Cramer et al., 2016a,b; Park et al., 2015), non-Hispanic White race/ethnicity (Burke et al., 2017; Cramer et al., 2016a,b), and higher socioeconomic status (Cramer et al., 2016ab; Park et al., 2015), with mixed findings regarding age (Adams et al., 2017; Cramer et al., 2016a,b).
A critical limitation in knowledge is that gender differences in utilization of CIH therapies have been understudied, particularly in veteran populations. Also of potential import but little examined is that utilization of CIH therapies by veteran populations may vary by race/ethnicity and age, for example because of race/ethnic and age-related differences in factors that facilitate or impede CIH use such as economic resources and cultural/health beliefs (Chao et al., 2006; Goldstein et al., 2015; Hsiao et al., 2006). We addressed these gaps by conducting secondary analyses of data from a national population study (Taylor et al., 2018) of VA users age 18–54 with chronic musculoskeletal pain to examine whether there are gender differences in the prevalence and predictors of CIH therapy use, and whether any effect of gender is further moderated by race/ethnicity and age. The results of this analysis could point to gender-specific policy and practice solutions for addressing chronic pain. As such, it could lay a foundation for strengthening the health achieving capabilities of women and men veterans with chronic pain.
Materials and methods
Study design and participants
We conducted secondary analyses of electronic health record (EHR) data of a retrospective cohort of veterans age 18–54 with chronic musculoskeletal pain receiving VA healthcare anytime from 2010–2013 (see parent study for details) (Taylor et al., 2018). Briefly, informed by prior research (Goulet et al., 2016; Tian et al., 2013) we defined chronic musculoskeletal pain as having 2+ occurrences during 2010–2013 of either (1) any ICD-9-CM chronic pain codes recorded at visits separated by 30+ days within a year or (2) any of 201 common musculoskeletal ICD-9-CM codes and 2+ patient-reported pain scores ≥ 4 (0–10 scale) within a 90-day period (Taylor et al., 2018). Use of CIH therapy was determined by analyzing structured and unstructured data fields (e.g., clinical notes) (Taylor et al., 2018). These data encompassed 79,537 women and 389,269 men. Use of these data for research purposes was approved by the VA Institutional Review Board.
Measures
The dependent variable is use of any CIH therapy (yes/no) during 2010–2013, occurring after first diagnosis of chronic musculoskeletal pain during that timeframe. CIH therapy was defined as any use of meditation, yoga, tai chi, acupuncture, chiropractic care, biofeedback, guided imagery, therapeutic massage, or hypnosis.
The key independent variable is gender. One moderator variable is race/ethnicity, defined according to five categories: (1) Hispanic/Latino and non-Hispanic/Latino categories of (2) White, (3) Black, (4) other (i.e., Asian, Native Hawaiian, other Pacific Islander, Native American, Alaskan Native, other), and (5) missing (representing 5%). To better understand the characteristics of this group, and per other research (Long et al., 2006), we included the “missing” race/ethnic category. A second moderator variable is age, coded into three categories: 18–34, 35–44, and 45–54.
Other patient characteristics are marital status and two proxy indicators of socio-economic status: 1) health insurance type (e.g., Medicaid enrollees are generally poorer and sicker) and 2) co-payment status because patients with copayments tend to have more income and less disability. Patient need for care is indicated by four comorbid health conditions: depression, anxiety, post-traumatic stress disorder (PTSD), and substance abuse (i.e., problematic use, not necessarily substance use disorder) or having a musculoskeletal pain diagnosis (e.g., back or neck pain, osteoarthritis, fibromyalgia, etc.) (see Table 1).
Table 1.
Characteristics of VA users with chronic musculoskeletal pain by gender and use of complementary and integrative health (CIH) therapies (n=468,806)
| Women (n=79,537) | Men (n=389,269) | |||
|---|---|---|---|---|
| Used CIH? n (%) |
Used CIH? n (%) |
|||
| Yes 28,463 (35.8) |
No 51,074 (64.2) |
Yes 99,369 (25.5) |
No 289,900 (74.5) |
|
| Agea, b | ||||
| 18–34 | 8,798 (30.9) | 17,039 (33.4) | 31,583 (31.8) | 88,258 (30.4) |
| 35–44 | 9,583 (33.7) | 16,563 (32.4) | 30,971 (31.2) | 90,105 (31.1) |
| 45–54 | 10,082 (35.4) | 17,472 (34.2) | 36,815 (37.1) | 111,537 (38.5) |
| Race/Ethnicitya, b | ||||
| White, Non-Hispanic | 15,590 (54.8) | 25,178 (49.3) | 61,101 (61.5) | 176,262 (60.8) |
| Black, Non-Hispanic | 8,128 (28.6) | 17,694 (34.6) | 20,192 (20.3) | 63,922 (22.1) |
| Hispanic or Latino/a | 2,364 (8.3) | 3,682 (7.2) | 10,296 (10.4) | 24,015 (8.3) |
| Other, Non-Hispanic | 1,236 (4.3) | 1,931 (3.8) | 4,041 (4.1) | 9,951 (3.4) |
| Missing | 1,145 (4.0) | 2,589 (5.1) | 3,739 (3.8) | 15,750 (5.4) |
| Marital Statusa, b | ||||
| Married | 9,120 (32.0) | 18,804 (36.8) | 43,701 (44.0) | 147,490 (50.9) |
| Divorced/Separated/Widowed | 11,259 (39.6) | 18,099 (35.4) | 30,473 (30.7) | 75,296 (26.0) |
| Single/Never Married | 8,043 (28.3) | 14,001 (27.4) | 25,023 (25.2) | 66,025 (22.8) |
| Missing/Unknown | 41 (0.14) | 170 (0.33) | 172 (0.17) | 1,089 (0.38) |
| Copaymenta, b | ||||
| Exempt | 43,543 (85.3) | 25,732 (90.4) | 84,793 (85.3) | 236,812 (81.7) |
| Required | 5,189 (10.2) | 1,471 (5.2) | 6,683 (6.7) | 37,851 (13.1) |
| Other + missing | 2,342 (4.6) | 1,260 (4.4) | 7,893 (7.9) | 15,237 (5.3) |
| Insurance Statusa, b | ||||
| VA | 16,823 (59.1) | 30,796 (60.3) | 63,048 (63.5) | 182,435 (62.9) |
| Private | 5,426 (19.1) | 12,764 (25.0) | 16,243 (16.4) | 67,145 (23.2) |
| Non-VA government | 6,214 (21.8) | 7,514 (14.7) | 20,078 (20.2) | 40,320 (13.9) |
| Comorbid Conditions | ||||
| Depressiona, b | 20,003 (70.3) | 21,549 (42.2) | 64,517 (64.9) | 96,506 (33.3) |
| Substance abusea, b | 11,813 (41.5) | 14,747 (28.9) | 59,971 (60.4) | 119,342 (41.2) |
| Post-traumatic stress disordera, b | 14,920 (52.4) | 13,321 (26.1) | 55,489 (55.8) | 84,260 (29.1) |
| Anxietya, b | 11,453 (40.2) | 11,069 (21.7) | 35,008 (35.2) | 50,023 (17.3) |
| Sleepa, b | 7,424 (26.1) | 8,630 (16.9) | 33,198 (33.4) | 67,061 (23.1) |
| Traumatic brain injurya, b | 2,288 (8.0) | 1,613 (3.2) | 19,618 (19.4) | 22,626 (7.8) |
| Musculoskeletal Pain Diagnoses | ||||
| Back paina, b | 13,670 (48.0) | 22,469 (44.0) | 56,589 (57.0) | 148,482 (51.2) |
| Joint paina, b | 8,941 (31.4) | 21,090 (41.3) | 32,931 (33.1) | 121,854 (42.0) |
| Neck paina, b | 6,386 (22.4) | 8,606 (16.9) | 19,235 (19.4) | 41,864 (14.4) |
| Fibromyalgiaa, b | 4,173 (14.7) | 5,506 (10.8) | 6,437 (6.5) | 16,866 (5.8) |
| Osteoarthritisa, b | 1,662 (5.8) | 3,301 (6.5) | 7,275 (7.3) | 23,109 (8.0) |
| Tempo-mandibular disordera, b | 334 (1.2) | 421 (0.8) | 478 (0.5) | 947 (0.3) |
Among women, differences between CIH users and non-users are statistically significant p<0.001.
Among men, differences between CIH users and non-users are statistically significant p<0.001.
Data analysis
First, we examined for women and men separately the bivariate differences in characteristics between patients who used CIH therapies and those who did not. Among patients who used CIH therapies, we also examined differences by gender in use of several types of CIH therapies (e.g., meditation, yoga, acupuncture, etc.). Next, we used a multivariate binary logistic regression model for women and men separately to assess associations between use of CIH therapies (yes/no), race/ethnicity, and age, controlling for covariates. Using these models, we tested a “race/ethnicity-by-age” interaction term. We used the moderation models to calculate and graph the predicted probabilities with 95% confidence intervals for use of CIH therapies in relation to race/ethnicity and age. Finally, to assess whether moderation by race/ethnicity and age was different by gender, we used the full model and tested a 3-way interaction term (gender by race/ethnicity by age). We used a two-tailed significance level at p <0.05 for all statistical tests. All analyses were conducted using STATA 14.0 (STATA Corp LP, 2017).
Results
Gender differences in use of CIH therapies
Of VA patients with chronic musculoskeletal pain, more women than men use CIH therapies (35.8% vs. 25.5%, p<0.001) (Table 1).
For both women and men, CIH therapy users and nonusers differ statistically for all socio-demographic and health characteristics examined. Also, given the large sample sizes, both large and small differences are statistically significant. Therefore, we summarize those patterns that differ by gender, focusing on differences that are greater than ~5%. Specifically, women CIH therapy users, compared to non-users, tend to be White (54.8% vs. 49.3%) and are less likely to be Black (28.6% vs. 34.6%), and more of them have copayment requirements (10.2% vs. 5.2%); among men, fewer CIH therapy users (6.7%) than non-users (13.1%) have copayments. The remaining sociodemographic differences between CIH therapy users and non-users are mostly small and similar by gender.
Gender differences in type of CIH therapy used
Type of CIH therapy used, stratified by gender, is presented in Table 2. Of patients who use any type of CIH therapy (n=127,832; 27.3% of total n=468,806), more women than men use yoga (16.8% vs. 9.9%) and fewer women than men use meditation (37.2% vs. 42.0%). Gender differences are statistically significant but small for chiropractic care, guided imagery, massage, and tai chi. There are no gender differences in the proportion of patients who use acupuncture (~15%), biofeedback (~6%), and hypnosis (<1%).
Table 2.
Type of CIH therapies used by women and men VA users (n=127,832)
| Women (n=28,463) n (%) |
Men (n=99,369) n (%) |
|
|---|---|---|
| Type of CIH therapy | ||
| Meditation a | 10,594 (37.2) | 41,759 (42.0) |
| Yoga a | 4,792 (16.8) | 9,819 (9.9) |
| Acupuncture | 4,287 (15.1) | 14,576 (14.7) |
| Chiropractic a | 3,987 (14.0) | 14,952 (15.1) |
| Biofeedback | 1,641 (5.8) | 5,685 (5.7) |
| Massage a | 1,603 (5.6) | 6,203 (6.2) |
| Guided imagery a | 988 (3.5) | 4,237 (4.3) |
| Tai Chi a | 539 (1.9) | 2,268 (2.3) |
| Hypnosis | 112 (0.4) | 370 (0.4) |
CIH = Complementary and integrative health.
The sample size reflects only those patients who used CIH (n=127,832) and omits patients who did not use CIH (n=340,974).
Patients could have used more than one type of CIH, and therefore column totals may exceed 100%.
Differences between women and men are statistically significant p<0.001.
Multivariate predictors of CIH therapy use among women and men
Results from the gender-stratified main effects models for women (Model 1a) and men (Model 1b) indicated Black women are less likely than White women (odds ratio 0.81, 95% CI 0.79–0.84, p<0.001) to use CIH therapies, while Black men are more likely than White men to use CIH therapies (odds ratio 1.04, 95% CI 1.02–1.06, p<0.001).
Other predictors of CIH therapy use are not different by gender. For both women and men, CIH therapy use is positively associated with older age (ref: 18–34), Hispanic/Latino and other race/ethnicity (ref: White), being single/never married or divorced/separated/widowed (ref: married), having non-VA government insurance (ref: VA), each comorbid health condition, and certain pain conditions (back pain, neck pain, tempo-mandibular disorder, fibromyalgia). Also, CIH therapy use is negatively associated with having a required copayment (ref: exempt), private health insurance (ref: VA), joint pain, and osteoarthritis.
Differences in CIH therapy use by gender, race/ethnicity, and age
An omnibus test of the race/ethnicity-by-age interaction term indicated that it was significant for women (Model 2a) and men (Model 2b) (p<0.001). Moreover, in a model that included data for both women and men and all covariates, an omnibus test of a 3-way interaction term (gender-by-race/ethnicity-by-age) indicated that it was significant at p=0.03 [data not shown]. Therefore, for women and men we used gender-stratified models to calculate and plot the predicted probabilities (with 95% confidence intervals [CI]) of CIH therapy use in relation to race/ethnicity and age, adjusting for covariates (Figure 1).
Figure 1. Predicted probabilities (with 95% confidence intervals) of CIH therapy use in relation to race/ethnicity and age, stratified by gender.
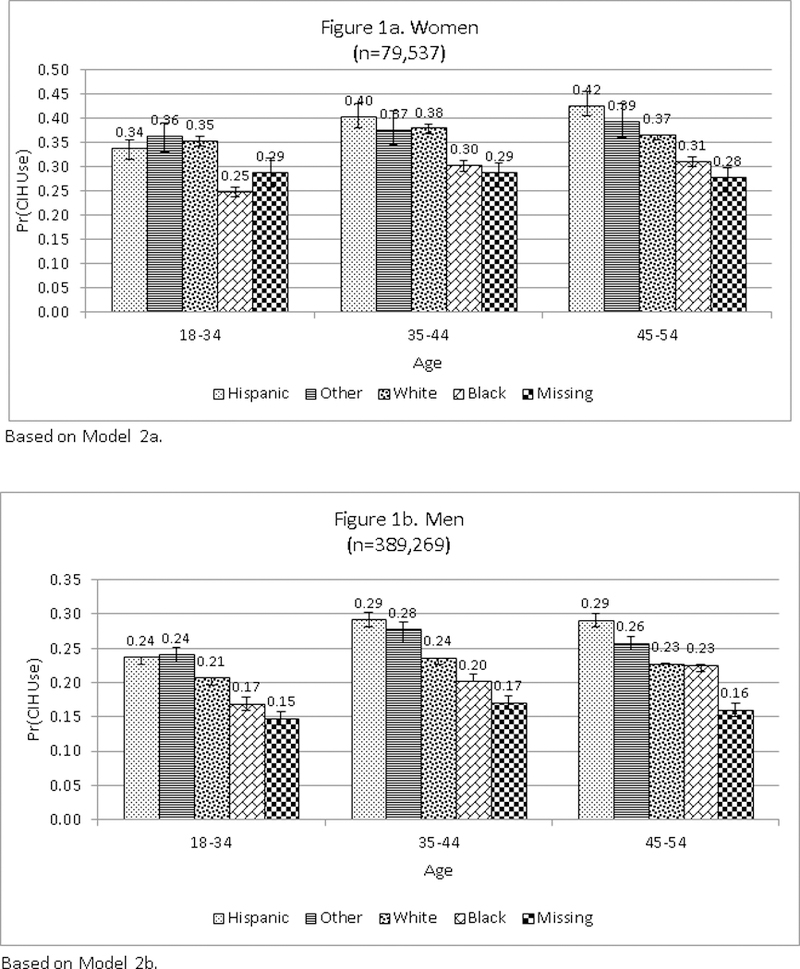
CIH = Complementary and integrative health
Non-overlapping confidence interval bars indicate that the difference in predicted probability is significant statistically.
Among women (Figure 1a), younger patients (age 18–34 and 35–44) who are Hispanic/Latina, White, or other race/ethnicity are each similarly likely to use CIH therapies (i.e., 34%−40%). However, among older women (age 45–54), White women are less likely than Hispanic/Latina women to use CIH therapies (37% vs. 42%, p<0.001). Finally, Black women, compared to other women, are least likely to use CIH therapies regardless of age (i.e., 25%−31%). In other analysis, we found that meditation was used by more Black women (40%) than each of the other racial/ethnic groups (32–37%), and fewer Black women used yoga (13% vs. 17–20%) (data not shown).
Among men (Figure 1b), in contrast to women, irrespective of age, White and Black veterans are less likely to use CIH therapies (i.e., 17%−24%) than Hispanic/Latino men or men of other race/ethnicities (i.e., 24%−29%). Also, among younger men (age 18–34 and 35–44) Black veterans are least likely to use CIH therapies (17% and 20%, respectively). Among 45–54 year old men, this difference disappears such that the probability of CIH therapy use among Black men matches that of White men (23%), but it is still lower than men of Hispanic/Latino (29%) or other race/ethnicity (26%).
Discussion
Of U.S. military veterans age 18–54 with chronic musculoskeletal pain who use VA healthcare, women are more likely than men to use CIH therapies (36% vs. 26%). Also, there are gender differences in the type of CIH therapy they use, with more women than men using yoga, and fewer women using meditation, chiropractic care, guided imagery, massage, and tai chi. We also found variation in rates of CIH therapy utilization by race/ethnicity and age, among both women and men, such that it is least likely to be used by younger Black or White veterans. Another striking result is that, among women, Black women are the least likely to use CIH therapies, irrespective of age. Finally, we found generally higher rates of CIH therapy use by Hispanic veterans of both genders with chronic musculoskeletal pain, compared to their similarly-aged White, Black, and other race/ethnicity counterparts.
Implications for practice and policy
Differences by gender in prevalence and type of CIH therapy used may reflect differences in veterans’ preferences and goals regarding such use or in type and severity of underlying pain and comorbid conditions. Nevertheless, findings suggest that focusing CIH therapy engagement in ways that are tailored to gender might increase CIH therapy use. For example, more men veterans with chronic musculoskeletal pain might use CIH therapies, and at an earlier stage in the course of their health conditions, if engagement and therapeutic efforts specifically incorporated information regarding how CIH therapies can prevent or alleviate specific comorbid conditions (e.g., substance use disorders, sleep disorders, traumatic brain injury) and pain diagnoses (e.g., back pain).
An implication of variation in rates of CIH therapy utilization by race/ethnicity and age is that efforts to engage more veterans in use of CIH therapies should specifically target certain groups. In particular, it is especially concerning that Black women veterans with chronic musculoskeletal pain are the least likely of women veterans with this condition to use CIH therapies. Black women are a significant and growing proportion of the veteran population (U.S. Department of Veterans Affairs, 2016). Also, Black adults are less likely to be prescribed opioids (Burgess et al., 2014) or monitored by a pain specialist (Hausmann et al., 2013). Furthermore, untreated physical pain is a critical reason why women veterans initiate illicit use of opioids and other substances (Evans et al., 2018). Therefore, Black women veterans may have significant unmet needs for pain relief services, which could elevate their risk for opioid and other substance use disorders.
We found higher rates of CIH therapy use by Hispanic veterans. This finding is contrary to general population studies showing lower CIH therapy use overall by Hispanics (Olano et al., 2015) but supports studies showing increases in use of certain CIH practices, especially yoga (Clarke et al., 2015). Hispanic veterans could be using CIH therapies more than others because they are less likely to receive opioids (Pletcher et al., 2008), or they have a greater willingness to try traditional healing practices or other alternative therapies for chronic pain (Kennedy et al., 2016; Tafur et al., 2009). More research is needed to understand why Hispanic women and men veterans with chronic musculoskeletal pain are more likely to use CIH therapies than other racial/ethnic groups. Findings could inform efforts to engage other patient groups in CIH care.
Limitations and strengths
Our findings are tempered by several limitations. First, we do not know if patients used CIH therapies to treat chronic musculoskeletal pain or for another reason. To address this issue we only included CIH therapy use that began after patients’ receipt of a musculoskeletal diagnosis, and we controlled for comorbid conditions. Also, results may be impacted by omitted variable bias (i.e., we did not consider several factors that may be related to CIH therapy use and also vary by gender, race/ethnicity, and age, such as pain ascertainment and severity, and physician and patient attitudes, knowledge, and preferences regarding CIH services.) We analyzed all patients age 18–54 with musculoskeletal pain who accessed healthcare at the VA during a certain time-period (2010–2013), and so findings may not be representative of military veterans with this condition who are older than age 54 or treated in other types of healthcare settings, or representative of how veterans are being treated more recently. Finally, our analyses relied on administrative EHR data which are subject to reporting biases, however these data have also been found to be valuable for investigating pain and health services utilization among VA patients (Abel et al., 2016; Goulet et al., 2016). Related to this limitation, documentation of race/ethnicity relied on VA EHR data, a source that more accurately documents White and Black race/ethnicity than it does Hispanic and non-Black minority race/ethnicity (Hamilton et al., 2009; Mor, 2018), constituting a potential source of bias in the present study. Also, approximately 5% of patients were missing race/ethnicity information. The proportion of patients missing race/ethnicity was not substantively different by gender or CIH use. Finally, we did not examine variation in availability of CIH therapies (VHA HAIG, 2015) and its association with CIH use, underscoring an area for future research.
This study has a number of strengths. It uses the veteran population, which is racially and ethnically diverse (e.g., ~40% of women veterans are racial/ethnic minorities) and, as such, facilitates the examination of racial and ethnic disparities. Also, we capitalized on the sophisticated VA EHR system which facilitates linking diagnosis and health services utilization records. These data enabled us to examine all patients of the healthcare system and, unlike most studies of musculoskeletal pain and CIH use, not only those treated in hospitals and specialty clinics (Callahan et al., 2009; Rhee et al., 2016). Our work contributes new knowledge regarding the gender-specific correlates of musculoskeletal pain and the factors that might explain differences in CIH use. CIH therapies are one potentially promising practice for addressing opioid misuse among veteran populations with chronic musculoskeletal pain. A next step for research is to determine whether differences in CIH use by gender translate into similar gender-based differences in patient outcomes such as pain, mental health, and opioid misuse.
Conclusion
Among military veterans with chronic musculoskeletal pain we found differential use of CIH therapies by gender, race/ethnicity, and age. These differences in CIH therapy use are important because they might be partially contributing to existing disparities in pain and opioid use. Our findings suggest that VA clinicians might want to tailor their CIH engagement efforts to be sensitive to gender, race/ethnicity, and age.
Table 3.
Predictors of patient use of CIH therapies (yes vs. no), stratified by gender
| Women (n=79,537) |
Men (n=389,269) |
|||
|---|---|---|---|---|
| 1a. Main effects model |
2a. Model 1a plus interactions |
1b. Main effects model |
2b. Model 1b plus interactions |
|
| Odds ratio (95% CI) |
Odds ratio (95% CI) |
Odds ratio (95% CI) |
Odds ratio (95% CI) |
|
| Age (ref: 18–34) | ||||
| 35–44 | 1.18*** (1.13–1.22) |
1.12*** (1.06–1.18) |
1.20*** (1.18–1.23) |
1.19*** (1.16–1.22) |
| 45–54 | 1.16*** (1.12–1.21) |
1.06* (1.00–1.12) |
1.21*** (1.18–1.23) |
1.14*** (1.11–1.17) |
| Race/Ethnicity (ref: White) | ||||
| Hispanic/Latina/o | 1.15*** (1.09–1.22) |
1.01 (0.92–1.10) |
1.39*** (1.35–1.42) |
1.27*** (1.22–1.33) |
| Black | 0.81*** (0.79–0.84) |
0.70*** (0.65–0.75) |
1.04*** (1.02–1.06) |
0.92*** (0.88–0.96) |
| Other | 1.13** (1.05–1.23) |
1.13 (0.99–1.28) |
1.29*** (1.24–1.34) |
1.29*** (1.21–1.39) |
| Missing | 0.86*** (0.79–0.93) |
0.94 (0.81–1.08) |
0.88*** (0.84–0.91) |
0.89** (0.82–0.96) |
| Marital Status (ref: Married) | ||||
| Single/Never Married | 1.26*** (1.21–1.31) |
1.26*** (1.21–1.31) |
1.32*** (1.29–1.35) |
1.32*** (1.29–1.35) |
| Divorced/Separated/Widowed | 1.15*** (1.11–1.19) |
1.15*** (1.11–1.19) |
1.18*** (1.15–1.20) |
1.18*** (1.15–1.20) |
| Missing | 0.61** (0.43–0.88) |
0.61** (0.42–0.87) |
0.74*** (0.63–0.88) |
0.74*** (0.63–0.88) |
| Copayment (ref: Exempt) | ||||
| Required | 0.60*** (0.57–0.64) |
0.60*** (0.57–0.64) |
0.64*** (0.61–0.65) |
0.64*** (0.62–0.65) |
| Other + missing | 0.94 (0.88–1.02) |
0.95 (0.88–1.02) |
1.40*** (1.36–1.45) |
1.40*** (1.36–1.45) |
| Insurance Status (ref: VA) | ||||
| Private | 0.89*** (0.86–0.93) |
0.89*** (0.86–0.93) |
0.86*** (0.84–0.88) |
0.86*** (0.84–0.87) |
| Non-VA government | 1.31*** (1.25–1.36) |
1.31*** (1.25–1.36) |
1.26*** (1.24–1.29) |
1.26*** (1.24–1.29) |
| Comorbid Conditions | ||||
| Depression (ref: No) | 2.01*** (1.95–2.09) |
2.02*** (1.95–2.09) |
2.23*** (2.19–2.27) |
2.23*** (2.19–2.27) |
| Anxiety (ref: No) | 1.49*** (1.44–1.55) |
1.49*** (1.44–1.54) |
1.52*** (1.49–1.55) |
1.52*** (1.49–1.55) |
| Post-traumatic stress disorder (ref: No) | 2.03*** (1.96–2.10) |
2.03*** (1.96–2.10) |
1.84*** (1.81–1.88) |
1.84*** (1.81–1.87) |
| Traumatic brain injury (ref: No) | 1.67*** (1.56–1.80) |
1.67*** (1.56–1.80) |
1.80*** (1.76–1.84) |
1.80*** (1.75–1.84) |
| Substance abuse (ref: No) | 1.24*** (1.20–1.28) |
1.24*** (1.20–1.28) |
1.54*** (1.51–1.56) |
1.54*** (1.51–1.56) |
| Sleep disorder (ref: No) | 1.23*** (1.18–1.27) |
1.23*** (1.18–1.27) |
1.19*** (1.16–1.21) |
1.19*** (1.16–1.21) |
| Musculoskeletal Pain Diagnoses | ||||
| Back pain (ref: No) | 1.16*** (1.12–1.21) |
1.17*** (1.12–1.21) |
1.15*** (1.13–1.17) |
1.15*** (1.13–1.17) |
| Neck pain (ref: No) | 1.34*** (1.28–1.40) |
1.34*** (1.28–1.40) |
1.18*** (1.16–1.21) |
1.18*** (1.16–1.21) |
| Joint pain (ref: No) | 0.83*** (0.80–0.87) |
0.83*** (0.80–0.87) |
0.80*** (0.78–0.81) |
0.80*** (0.78–0.81) |
| Osteoarthritis (ref: No) | 0.90** (0.84–0.97) |
0.90** (0.84–0.97) |
0.92*** (0.89–0.95) |
0.92*** (0.89–0.95) |
| Tempo-mandibular disorder (ref: No) | 1.32*** (1.12–1.54) |
1.31*** (1.12–1.53) |
1.29*** (1.14–1.45) |
1.29*** (1.14–1.45) |
| Fibromyalgia (ref: No) | 1.35*** (1.28–1.42) |
1.35*** (1.28–1.42) |
1.10*** (1.07–1.14) |
1.10*** (1.07–1.14) |
| Interaction term: Age (ref: 18–34) × Race/ethnicity (ref: White) | -- | Omnibus test p<0.001 | -- | Omnibus test p<0.001 |
| 35–44 Black | -- | 1.18*** (1.08–1.29) |
-- | 1.05 (0.99–1.11) |
| 35–44 Hispanic/Latina/o | -- | 1.18* (1.03–1.36) |
-- | 1.12*** (1.05–1.20) |
| 35–44 Other | -- | 0.95 (0.78–1.14) |
-- | 1.02 (0.92–1.12) |
| 35–44 Missing | -- | 0.89 (0.73–1.08) |
-- | 1.01 (0.91–1.11) |
| 45–54 Black | -- | 1.29*** (1.18–1.41) |
-- | 1.26*** (1.20–1.33) |
| 45–54 Hispanic/Latina/0 | -- | 1.37*** (1.18–1.60) |
-- | 1.17*** (1.09–1.25) |
| 45–54 Other | -- | 1.07 (0.88–1.31) |
-- | 0.97 (0.87–1.07) |
| 45–54 Missing | -- | 0.89 (0.74–1.08) |
-- | 0.97 (0.88–1.07) |
CIH = Complementary and integrative health.
p<0.001
p<0.01
<0.05
Acknowledgments
Funding for this research was provided by the Department of Veterans Affairs, Health Services Research and Development Service, 1 R01 HX001704-1. Dr. Elizabeth Evans was also supported by the Iris Cantor-UCLA Women’s Health Center Advisory Board (NCATS UCLA CTSI UL1TR001881) and The Greenwall Foundation.
Author bios
Elizabeth A. Evans, PhD, MA, is an Assistant Professor of Health Promotion and Policy at the University of Massachusetts Amherst. A public health scientist, she has expertise in women’s health, substance use disorders, and mining electronic health records and other big data to understand health services utilization and outcomes.
Patricia M. Herman, PhD, ND, MS, is a senior behavioral scientist at the RAND Corporation and a member of the Pardee RAND Graduate School faculty. Her research centers on health economics, innovative care models, and overall quality of life.
Donna L. Washington, MD, MPH, is the Women’s Health Focused Research Area Lead, VA HSR&D’s Center for the Study of Healthcare Innovation, Implementation and Policy; and Professor of Medicine, UCLA. Her research interests include the health care needs of women and vulnerable/underserved populations.
Karl A. Lorenz, MD, MSHS, is a general internal medicine and palliative care physician, and Section Chief of the VA Palo Alto-Stanford Palliative Care Program. He has contributed to the field of global palliative care, serving the World Health Organization in its development of Palliative Care for Older People and leading methods for Palliative Care Essential Medications.
Anita Yuan, PhD, is a Research Health Scientist at the HSR&D Center for the Study of Healthcare Innovation, Implementation, and Policy (CSHIIP). She studies health services utilization, the impacts of services for homeless veterans, and complementary and integrative health.
Dawn M. Upchurch, PhD, Lac, is Professor of Public Health at the UCLA Fielding School of Public Health. She studies women’s health and well-being, emphasizing psychosocial stressors and lifestyle behaviors on health, and alternative and integrative medicine strategies to improve women’s health.
Nell Marshall, DrPH, MPH, is a Health Scientist at the VA Palo Alto Health Care System. Her research interests include implementation science, complementary and integrative health, and models for genetic consultation.
Alison B. Hamilton, PhD, MPH, Associate Director for Implementation Science at the HSR&D Center for the Study of Healthcare Innovation, Implementation, and Policy (CSHIIP), is a medical anthropologist with expertise in implementation science, women’s health, mental health, and qualitative methods.
Stephanie L. Taylor, PhD, MPH, is Associate Director of the VA GLA HSR&D COIN and Director of the Complementary and Integrative Health Evaluation Center. A medical sociologist and health services researcher, she studies environmental and organizational influences on health and health care, and implementation, with expertise in complementary and integrative health, patient safety and women’s health.
Footnotes
All authors report no conflicts of interest.
References
- Abel EA, Brandt CA, Czlapinski R, & Goulet JL (2016). Pain research using Veterans Health Administration electronic and administrative data sources. J Rehabil Res Dev, 53(1):1–12. [DOI] [PubMed] [Google Scholar]
- Adams J, Peng W, Cramer H, Sundberg T, Moore C, Amorin-Woods L, Sibbritt D, & Lauche R (2017). The prevalence, patterns, and predictors of chiropractic use among US adults: results from the 2012 National Health Interview Survey. Spine, 42(23):1810–1816. [DOI] [PubMed] [Google Scholar]
- Bawa FL, Mercer SW, Atherton RJ, Clague F, Keen A, Scott NW, & Bond CM (2015). Does mindfulness improve outcomes in patients with chronic pain? Systematic review and meta-analysis. Br J Gen Pract, 65(635):e387–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnert AS, Ilgen MA, Trafton JA, Kerns RD, Eisenberg A, Ganoczy D, & Blow FC (2014). Trends and regional variation in opioid overdose mortality among Veterans Health Administration patients, fiscal year 2001 to 2009. Clin J Pain, 30(7):605–12. [DOI] [PubMed] [Google Scholar]
- Burgess DJ, Nelson DB, Gravely AA, Bair MJ, Kerns RD, Higgins DM, van Ryn M, Farmer M, & Partin MR (2014). Racial differences in prescription of opioid analgesics for chronic noncancer pain in a national sample of veterans. J Pain, 15(4):447–55. [DOI] [PubMed] [Google Scholar]
- Burke A, Lam CN, Stussman B, & Yang H (2017). Prevalence and patterns of use of mantra, mindfulness and spiritual meditation among adults in the United States. BMC Complement Altern Med, 17(1):316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callahan LF, Wiley-Exley EK, Mielenz TJ, Brady TJ, Xiao C, Currey SS, Sleath BL, Sloane PD, DeVellis RF, & Sniezek J (2009). Use of complementary and alternative medicine among patients with arthritis. Prev Chronic Dis, 6(2):A44. [PMC free article] [PubMed] [Google Scholar]
- Chao MT, Wade C, Kronenberg F, Kalmuss D, Cushman LF (2006). Women’s reasons for complementary and alternative medicine use: racial/ethnic differences. J Altern Complement Med, 12(8):719–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke TC, Black LI, Stussman BJ, Barnes PM, & Nahin RL (2015). Trends in the use of complementary health approaches among adults: United States, 2002–2012. Natl Health Stat Report, (79):1–16. https://nccih.nih.gov/research/statistics/NHIS. Accessed 1 April 2018. [PMC free article] [PubMed] [Google Scholar]
- Cramer H, Hall H, Leach M, Frawley J, Zhang Y, Leung B, Adams J, & Lauche R (2016). Prevalence, patterns, and predictors of meditation use among US adults: A nationally representative survey. Sci Rep, 6:36760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer H, Ward L, Steel A, Lauche R, Dobos G, & Zhang Y (2016). Prevalence, patterns, and predictors of yoga use: results of a us nationally representative survey. Am J Prev Med, 50(2):230–5. [DOI] [PubMed] [Google Scholar]
- Dobscha SK, Morasco BJ, Duckart JP, Macey T, & Deyo RA (2013). Correlates of prescription opioid initiation and long-term opioid use in veterans with persistent pain. Clin J Pain, 29(2):102–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund MJ, Steffick D, Hudson T, Harris KM, & Sullivan M (2007). Risk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non-cancer pain. Pain, 129(3):355–62. [DOI] [PubMed] [Google Scholar]
- Evans EA, Glover DL, Washington DL, & Hamilton AB (2018). Psychosocial factors that shape substance abuse and related mental health of women military veterans who use community-based services. Subst Use Misuse, 27:1–15. [DOI] [PubMed] [Google Scholar]
- Finlay AK, Binswanger IA, Smelson D, Sawh L, McGuire J, Rosenthal J, Blue-Howells J, Timko C, Blodgett JC, Harris AH, Asch SM, & Frayne S (2015). Sex differences in mental health and substance use disorders and treatment entry among justice-involved Veterans in the Veterans Health Administration. Med Care, 53(4 Suppl 1):S105–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaither JR, Goulet JL, Becker WC, Crystal S, Edelman EJ, Gordon K, Kerns RD, Rimland D, Skanderson M, Justice AC, & Fiellin DA (2016). The association between receipt of guideline-concordant long-term opioid therapy and all-cause mortality. J Gen Intern Med, 31(5):492–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein JN, Ibrahim SA, Frankel ES, & Mao JJ (2015). Race, pain, and beliefs associated with interest in complementary and alternative medicine among inner city veterans. Pain Med, 16(8):1467–1474. [DOI] [PubMed] [Google Scholar]
- Goulet JL, Kerns RD, Bair M, Becker WC, Brennan P, Burgess DJ, Carroll CM, Dobscha S, Driscoll MA, Fenton BT, Fraenkel L, Haskell SG, Heapy AA, Higgins DM, Hoff RA, Hwang U, Justice AC, Piette JD, Sinnott P, Wandner L, Womack JA, & Brandt CA. (2016). The musculoskeletal diagnosis cohort: examining pain and pain care among veterans. Pain, 157(8):1696–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, Berger Z, Sleicher D, Maron DD, Shihab HM, Ranasinghe PD, Linn S, Saha S, Bass EB, & Haythornthwaite JA (2014). Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med, 174(3):357–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton NS, Edelman D, Weinberger M, & Jackson GL (2009). Concordance between self-reported race/ethnicity and that recorded in a Veteran Affairs electronic medical record. N C Med J, 70(4):296–300. [PubMed] [Google Scholar]
- Hausmann LR, Gao S, Lee ES, & Kwoh CK (2013). Racial disparities in the monitoring of patients on chronic opioid therapy. Pain, 154(1):46–52. [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Warner M, & Miniño AM (2017). Drug overdose deaths in the United States, 1999–2016 NCHS Data Brief, 294 Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Hempel S, Taylor SL, Marshall NJ, Miake-Lye IM, Beroes JM, Shanman R, Solloway MR, & Shekelle PG (2014). Evidence Map of Mindfulness. VA-ESP Project #05–226; 2014 https://www.ncbi.nlm.nih.gov/books/NBK268640/ Accessed 1 April 2018. [PubMed] [Google Scholar]
- Higgins DM, Fenton BT, Driscoll MA, Heapy AA, Kerns RD, Bair MJ, Carroll C, Brennan PL, Burgess DJ, Piette JD, Haskell SG, Brandt CA, & Goulet JL (2017). Gender differences in demographic and clinical correlates among veterans with musculoskeletal disorders. Womens Health Issues, 27(4): 463–470. [DOI] [PubMed] [Google Scholar]
- Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, Colaiaco B, Maher AR, Shanman RM, Sorbero ME, & Maglione MA (2017). Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann Behav Med, 51(2):199–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe CQ, & Sullivan MD (2014). The missing ‘P’ in pain management: how the current opioid epidemic highlights the need for psychiatric services in chronic pain care. Gen Hosp Psychiatry, 36(1):99–104. [DOI] [PubMed] [Google Scholar]
- Hsiao AF, Wong MD, Goldstein MS, Yu HJ, Andersen RM, Brown ER, Becerra LM, Wenger NS (2006). Variation in complementary and alternative medicine (CAM) use across racial/ethnic groups and the development of ethnic-specific measures of CAM use. J Altern Complement Med, 12(3):281–90. [DOI] [PubMed] [Google Scholar]
- Kennedy L, Gonzales E, & Corbin L (2016). The effect of curanderismo on chronic non-malignant pain: a case report. Explore (NY), 12(4):263–7. [DOI] [PubMed] [Google Scholar]
- Kochanek KD, Murphy SL, Xu JQ, & Arias E (2017). Mortality in the United States, 2016 NCHS Data Brief, 293 Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Kroll-Desrosiers AR, Skanderson M, Bastian LA, Brandt CA, Haskell S, Kerns RD, & Mattocks KM (2016). Receipt of prescription opioids in a national sample of pregnant veterans receiving Veterans Health Administration care. Womens Health Issues, 26(2):240–6. [DOI] [PubMed] [Google Scholar]
- Long JA, Bamba MI, Ling B, & Shea JA (2006). Missing race/ethnicity data in Veterans Health Administration based disparities research: a systematic review. J Health Care Poor Underserved, 17(1):128–40. [DOI] [PubMed] [Google Scholar]
- MacPherson H, Vertosick EA, Foster NE, Lewith G, Linde K, Sherman KJ, Witt CM, & Vickers AJ (2017). The persistence of the effects of acupuncture after a course of treatment: a meta-analysis of patients with chronic pain. Pain, 158(5):784–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miake-Lye IM, Lee JF, Luger T, Taylor S, Shanman R, Beroes JM, & Shekelle PG (2016). Massage for Pain: An Evidence Map. VA ESP Project #05–226. https://www.hsrd.research.va.gov/publications/esp/massage.cfm Accessed 1 April 2018. [PubMed] [Google Scholar]
- Mor M (2018). Assessing race and ethnicity in VA eata. 2018 VIReC Databases and Methods Cyberseminar. Accessed 27 June 2018 https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/2410-notes.pdf [Google Scholar]
- Mosher HJ, Krebs EE, Carrel M, Kaboli PJ, Weg MW, & Lund BC (2015). Trends in prevalent and incident opioid receipt: an observational study in Veterans Health Administration 2004–2012. J Gen Intern Med, 30(5):597–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahin RL, Boineau R, Khalsa PS, Stussman BJ, & Weber WJ (2016). Evidence-based evaluation of complementary health approaches for pain management in the United States. Mayo Clin Proc, 91(9):1292–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olano HA, Kachan D, Tannenbaum SL, Mehta A, Annane D, & Lee DJ (2015). Engagement in mindfulness practices by U.S. adults: sociodemographic barriers. J Altern Complement Med, 21:100–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park CL, Braun T, & Siegel T (2015). Who practices yoga? A systematic review of demographic, health-related, and psychosocial factors associated with yoga practice. J Behav Med, 38(3):460–71. [DOI] [PubMed] [Google Scholar]
- Pletcher MJ, Kertesz SG, Kohn MA, & Gonzales R (2008). Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA, 2;299(1):70–8. [DOI] [PubMed] [Google Scholar]
- Rhee TG, Leininger BD, Ghildayal N, Evans RL, Dusek JA, & Johnson PJ (2016). Complementary and integrative healthcare for patients with mechanical low back pain in a U.S. hospital setting. Complement Ther Med, 24:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmonds MJ, Finley EP, Vale S, Pugh MJ, & Turner BJ (2015). A qualitative study of veterans on long-term opioid analgesics: barriers and facilitators to multimodality pain management. Pain Med, 16(4):726–32. [DOI] [PubMed] [Google Scholar]
- Stussman BJ, Black LI, Barnes PM, Clarke TC, & Nahin RL (2015). Wellness-related use of common complementary health approaches among adults: United States, 2012. Natl Health Stat Report, (85):1–12. [PubMed] [Google Scholar]
- Tafur MM, Crowe TK, & Torres E (2009). A review of curanderismo and healing practices among Mexicans and Mexican Americans. Occup Ther Int, 16(1):82–8. [DOI] [PubMed] [Google Scholar]
- Taylor SL, Herman PM, Marshall NJ, Zeng Q, Yuan A, Chu K, Shou Y, Morioka C, & Lorenz K (2018). Use of complementary and integrated health: a retrospective analysis of U.S. veterans with chronic musculoskeletal pain nationally. J Alternative and Complementary Medicine. [DOI] [PubMed] [Google Scholar]
- Tian TY, Zlateva I, & Anderson DR (2013). Using electronic health records data to identify patients with chronic pain in a primary care setting. J Am Med Inform Assoc, 20(e2):e275–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upchurch DM, & Rainisch BW (2015). The importance of wellness among users of complementary and alternative medicine: findings from the 2007 National Health Interview Survey. BMC Complement Altern Med, 15:362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs. (2016). Profile of Women Veterans: 2015. National Center for Veterans Analysis and Statistics; https://www.va.gov/vetdata/docs/SpecialReports/Women_Veterans_Profile_12_22_2016.pdf Accessed 1 April 2018. [Google Scholar]
- U.S. Government Publishing Office. (July 6, 2016). Comprehensive Addiction and Recovery Act of 2016. House Report 114–669. https://www.gpo.gov/fdsys/pkg/CRPT-114hrpt669/html/CRPT-114hrpt669.htm. Accessed 6 July 2018. [Google Scholar]
- U.S. Surgeon General. (2016). Facing addiction in America: The Surgeon General’s report on alcohol, drugs, and health. Washington, DC: HHS, November 2016. [PubMed] [Google Scholar]
- Veterans Healthcare Administration (VHA), Healthcare Analysis & Information Group (HAIG). (2015). FY 2015 VHA complementary and integrative health (CIH) services. Report prepared by a Field Unit of the Office of Strategic Planning & Analysis, Office of the ADUSH for Policy and Planning. https://sciencebasedmedicine.org/wp-content/uploads/2016/07/FY2015_VHA_CIH_signedReport.pdf. Accessed 6 July 2018. [Google Scholar]
- Weimer MB, Macey TA, Nicolaidis C, Dobscha SK, Duckart JP, & Morasco BJ (2013). Sex differences in the medical care of VA patients with chronic non-cancer pain. Pain Med, 14(12):1839–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Leach MJ, Bishop FL, & Leung BA (2016). Comparison of the characteristics of acupuncture- and non-acupuncture-preferred consumers: a secondary analysis of NHIS 2012 data. J Altern Complement Med, 22(4):315–22. [DOI] [PMC free article] [PubMed] [Google Scholar]


