Abstract
Tumor-released extracellular vesicles (EVs) contain tumor-specific cargo distinguishing them from healthy EVs, and making them eligible as circulating biomarkers. Glypican 1 (GPC1)-positive exosome relevance as liquid biopsy elements is still debated. We carried out a prospective study to quantify GPC1-positive exosomes in sera from pancreatic ductal adenocarcinoma (PDAC) patients undergoing up-front surgery, as compared to controls including patients without cancer history and patients displaying pancreatic preneoplasic lesions. Sera were enriched in EVs, and exosomes were pulled down with anti-CD63 coupled magnetic beads. GPC1-positive bead percentages determined by flow cytometry were significantly higher in PDAC than in the control group. Diagnosis accuracy reached 78% (sensitivity 64% and specificity 90%), when results from peripheral and portal blood were combined. In association with echo-guided-ultrasound-fine-needle-aspiration (EUS-FNA) negative predictive value was 80% as compared to 33% for EUS-FNA only. This approach is clinically relevant as a companion test to the already available diagnostic tools, since patients with GPC1-positive exosomes in peripheral blood showed decreased tumor free survival.
Introduction
Pancreatic ductal adenocarcinoma (PDAC) is discovered at advanced stages because its clinical presentation is preceded by non-specific symptoms. The only curative treatment is surgery but only 20% of the patients are eligible for tumor resection [1], [2]. Several diagnostic tools such as imaging are needed, making diagnosis long and costly [3], [4]. PDAC management is complicated by the fact that the onset of neo-adjuvant or palliative therapies depends on the required histological proof of the presence of the tumor. This proof, routinely obtained by conventional biopsies, is risky for the patients. For example, endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) may result in cancer cell dissemination along the needle track, may provoke pancreatitis, and its predictive negative value is low [3]. When EUS-FNA is negative, the procedure is repeated leading to delayed patient management, which worsens the prognosis [5]. The CA19-9 (Carbohydrate Antigen) or CEA (Carcinoembryonic Antigen) plasma biomarkers have poor sensitivity and specificity and are not recommended for PDAC diagnosis [6], [7], [8]. Finally, even when resection is possible and complete, a high percentage of patients develop metastatic disease, without possible identification before surgery by predictive markers [9], [10]. Thus, efforts aim at finding new diagnostic, predictive and prognostic tools for PDAC.
In 2015, a major advance was published by Melo et al. identifying PDAC by quantifying circulating tumor-specific exosomes enriched in the membrane protein heparan sulfate proteoglycan glypican 1 (GPC1) [11]. GPC1 is overexpressed in PDAC primary tumors [12] and supports tumor cell proliferation and migration [13]. Moreover, heparan sulfate proteoglycans, including GPC1 are involved and remain in exosome internalization [14]. GPC1 was found membrane bound to exosomes isolated from several cancer cell lines where it was also up-regulated as compared to healthy fibroblasts [11]. Based on this observation, a flow-cytometry test distinguished perfectly PDAC over healthy donors or patients with benign pancreatic diseases in exosome-enriched sera. Since this proof of principle, studies trying to confirm this crucial advance have reached various degrees of validation. In 2017, exosomal GPC1 quantified by liquid chromatography-mass spectrometry/mass spectrometry (LC–MS/MS), using a GPC1 specific peptide, did not identify PDAC patients over controls (healthy donors or chronic pancreatitis (CP), [15]). Instead, a 5-microRNA signature with high miR-10b, -21, -30c, and 181a and low let7a differentiated PDACs from controls. In the same way, a signature of 5 proteins (EGFR, EpCAM, MUC1, HER2, GPC1 and WNT2), found by EV (extracellular vesicle)-based protein marker profiling identified PDAC patients with a sensitivity of 86% and a specificity of 81% [16]. In this report, EV-GPC1 used alone did not distinguish PDAC patients from controls. In 2018, alternating current electrokinetic (ACE) microarray chip, capturing exosomes directly from plasma, followed by immunofluorescent detection and quantification of CD63 and GPC1 did identify PDAC over healthy patients [17]. This is the only independent study confirming the possibility to diagnose PDAC patients by quantifying CD63high/GPC1high exosomes. Thus, according to conflicting results in published data, a key question to answer is whether reported findings on GPC1-positive exosomes identifying PDAC can be validated independently in early stage patients.
We used a prospective cohort of patients who underwent up-front surgery without neo-adjuvant treatment for localized PDAC, because they are the population of patients for whom rapidity in diagnostic is crucial to avoid delay, and lower cancer progression risk. We pulled down GPC1-positive exosomes from sera from cancer patients and non-cancer controls, with anti-CD63 coupled magnetic beads and quantified them by flow cytometry. Importantly, we tested the hypothesis that GPC1-positive exosomes might be more numerous in portal blood drained from the primary tumor. We assessed the diagnostic accuracy of this method as compared to CA19-9 quantification, endoscopy ultrasound guided fine needle aspiration (EUS-FNA) tumor cell identification and KRAS circulating tumor DNA amplification.
Materials and Methods
Patients Demographics
Patients eligible for pancreatic surgery with suspicion of pancreatic cancer or IPMN (intraductal papillary and mucinous neoplasm) with worrisome features as determined by CT-scan (computerized tomography scanner) and or MRI (magnetic resonance imaging) without metastasis were enrolled at the department of hepatobiliary surgery of Bordeaux university hospital between February and November 2017. This prospective study was conducted according to the Declaration of Helsinki, the French rules (Law for Bioethics November 2016) and the recommendations of CNIL (Comité National Informatique et Liberté), and was approved by an Institutional Review Board. The biological collection was declared to and approved by the “comité de protection des personnes sud ouest outremer” under the number 2016-A00431-50 and the database was registered in Clinical Trials under the number: NCT03032913. Informed consent was obtained from patients and before surgery. Patients did not receive neoadjuvant therapy. A control group enrolled patients, with informed consent, undergoing surgery for benign pathologies, and with no history of cancer. Patient follow-up, completed until December 1, 2018, evaluated survival and disease recurrence.
Blood Sampling
Two samples of 7.5 ml of blood were collected from the portal vein in BD vacutainer collection tubes without additives (SST tubes, Becton Dickinson, Le Pont de Claix, France), after laparotomy, before manipulation of the tumor. Two samples of 7.5 ml were collected during surgery in the median cephalic vein in BD vacutainer collection tubes without additives. A sample of 7.5 ml in BD vacutainer collection tube containing EDTA was collected for complete blood count, to determine neutrophil over leukocyte ratio in the patient group (DXH automated counter, Beckman Coulter, Villepinte, France). Median cephalic vein was punctured in the control group, to collect sample in vacutainer collection tubes without additives. Tubes were centrifuged quickly at 2000 g for 15 minutes to collect sera. Sera from patients were immediately used to determine CA19-9 concentration (Architect automated instrument, Abbott). Then sera were frozen at −80 °C until they were further processed. In addition, one tube (Cell free DNA collection tube©, Roche, Meylan, France) was collected in a peripheral vein for all patients and controls, and also in the portal vein for IPMN and PDAC groups for ctDNA analysis.
Exosome Isolation and Flow Cytometry
Sera were enriched in extracellular vesicles (EVs) using the Total Exosome Isolation kit (Thermofisher, Courtaboeuf, France), according to the manufacturer's instructions. Briefly, serum samples stored at −80 °C were thawed on ice and centrifuged at 2000 g for 30 minutes to remove cells and debris. Sera supernatants were incubated for 30 minutes with Total Exosome Isolation reagent at 4 °C and centrifuged for 10 minutes at 10,000 g. EV-enriched pellets were resuspended in Phosphate Buffered Saline (PBS), and stored at −20 °C. The Exosome-Human CD63 Isolation/Detection Reagent (Thermofisher) was used to pull down sera exosomes. Magnetic bead-coupled exosomes were stained with anti-CD63-FITC (Biolegend, London, UK) to validate exosome isolation. Flow cytometry analysis confirmed that 98 to 99% of the beads were CD63-positive (not shown). Anti-CD9-PE antibody (Biolegend) and anti-GPC1 primary antibody (PIPA528055, Thermofisher) revealed with Alexa Fluor 647 donkey anti rabbit IgG (Biolegend) were used together. All staining steps and washes were carried out in PBS1X/ BSA 0.1%. Samples were examined on a BD FACS CANTO II apparatus using unstained beads and beads stained with isotype controls (PE mouse IgG1 Kappa isotype control clone MOPC-21 (Biolegend) and rabbit igG isotype control Alexa Fluor 647 conjugate (OZYME, Montigny-le-Bretonneux, France)) to setup quantification areas on dot plots. Data were collected on FSC and SSC linear parameters (645 V and 520 V, respectively) and on a logarithmic scale for Alexa 647 and PE (455 V and 400 V, respectively). Data were analyzed with BD FACS Diva software (BD Biosciences, Le Pont de Claix, France). Each sample was analyzed twice in independent experiments.
Western Blot Analysis
Proteins from vesicle-enriched sera with Total Exosome Isolation kit, were extracted as already described [18]. We used the same primary antibodies as in flow cytometry analysis. Densitometry quantification was carried out with Image J 1.52a software [19].
ctDNA Quantification
Plasmas were collected in Cell free DNA collection tube and were subjected to DNA extraction (RSC ccfDNA plasma kit, Maxwell (Promega, Charbonnières-les-Bains, France)). Tissue DNA was extracted from FFPE specimens using Maxwell® RSC DNA FFPE Kit (Promega) according to the manufacturer's instructions. KRAS mutant alleles were detected by droplet digital PCR (ddPCR) with the KRAS G12/G13 Screening Kit (Biorad, Marne la Coquette, France).
Statistics
Qualitative and quantitative data were analyzed with usual statistic tools (including Student's-test, Chi-Square and Fisher exact tests) using GraphPad-Instat and GraphPad-Prism 8.0 software (GraphPad Software Inc., San Diego, CA, USA). The Spearman correlation coefficient was used to assess the correlation between different variables. Group differences were tested using the nonparametric Wilcoxon-Mann–Whitney test for two groups. Receiver operating curves (ROC) were obtained to describe the accuracy of detecting cancer. The cutoff points were selected using Youden's index, which maximizes the sum of sensitivity and specificity. ROCs and Youden's index calculation were performed using SAS software (version 9.4, SAS institute, Cary, NC, USA).
Results
Patient Characteristics
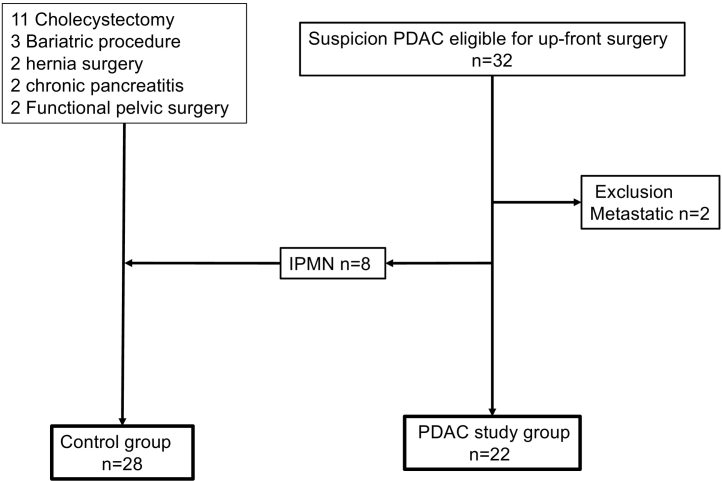
From February to November 2017, 72 patients underwent surgery for PDAC of which 32 had an up-front surgery for presumed PDAC without neo-adjuvant therapy (Figure 1). Among them, two patients were excluded because metastatic disease was discovered during surgery, and 8 patients were excluded from the cancer group and switched to the control group after definitive pathology analysis, because of non-invasive intraductal papillary mucinous neoplasm (IPMN) diagnostic. Thus, control group included 20 control patients operated in our surgical unit without neoplasia and without a history of cancer (including two chronic pancreatitis who underwent surgery for symptomatic reasons) and 8 IPMN (Figure 1). Demographic and clinicopathological characteristics are shown in Table 1. The groups were similar according to all clinical features (Table 1). Mean tumor size was 31 mm. All tumors were resectable without vascular involvement (i.e. superior mesenteric artery or superior mesenteric or portal vein).
Figure 1.
Patient selection criteria.
PDAC, pancreatic ductal adenocarcinoma; IPMN, intraductal papillary and mucinous neoplasm.
Table 1.
Clinical and histological features of the cohort
| Variables | PDAC group (n = 22) N (%) |
Control group (n = 28) N (%) |
|---|---|---|
| Age, y, (median; range) | 68.8 (69.5; 57-81) | 58.3 (61;22-73) |
| Male gender, n (%) | 13 (59) | 8 (28) |
| Serum CA19-9 (n = 19 PDAC group) | ||
| Normal | ||
| Elevated | 16 (84) | 23 (82) |
| 3 (16) | 5 (IPMN) (18) | |
| NLR mean (med; range) | 7.19 (3.7; 0.69-21) | |
| EUS-FNA | Total n = 18 | |
| Positive n = 8 | ||
| Negative n = 10 | ||
| Pathology: Macroscopic | ||
| Tumor size (mm) mean (med; range) | 31 (30; 11-50) | |
| Tumor stage (mean) | Stage 1a: 1 (5) | |
| Stage 1b: 4 (18) | ||
| Stage 2b: 11 (50) | ||
| Stage 3: 6 (59.2) | ||
| Glandular Differentiation (%) | Well 3 (13.6) | |
| Moderately 11 (50) | ||
| Poorly 8 (36.4) | ||
| KRAS status all primary tumors were positive for KRAS: | ||
| Mutant allele frequency mean (med; range) | 26.15 (17.45;0.35-77.6) |
IPMN (n = 8) are included in the control group. Med, median; PDAC, pancreatic ductal adenocarcinoma; IPMN, intraductal papillary and mucinous neoplasm; EUS-FNA endoscopic ultrasound-guided fine needle aspiration; NLR, neutrophil to lymphocyte ratio; med, median; Note that CA19-9 dosages for 3 PDAC patients were uninterpretable because of jaundice.
GPC1 Positive Exosomes in Peripheral Blood
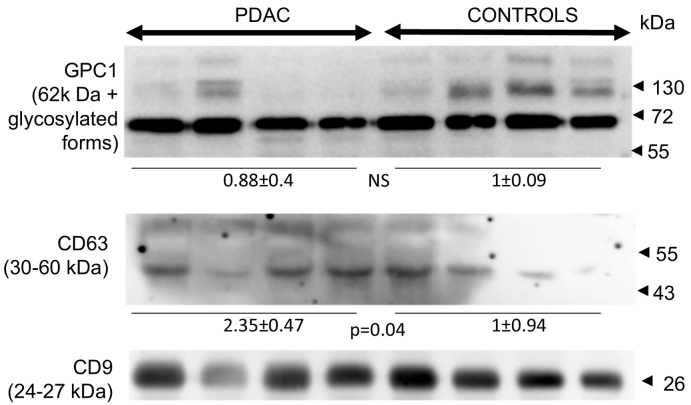
We tested the presence of GPC1, CD9 and CD63 proteins extracted from vesicle-enriched sera of patients and controls. Western blot analysis found expected signals for the exosomes markers CD63 and CD9 and GPC1 (Fig. 2). Densitometry analysis showed that GPC1 expression levels were similar in PDAC and control groups. By contrast CD63 signals were higher in the PDAC group by almost twofold (P = .04, n = 4).
Figure 2.
GPC1 is present in patient and control EV-enriched sera.
Proteins extracted from patient and control sera were analyzed by western blotting for the presence of CD63 and CD9 exosome markers and for GPC1 proteins. Protein sizes of marker are indicated by arrow heads in kDa. A Student's t test was used to compare densitometry values of CD63 and GPC1 band intensities over CD9 signal.
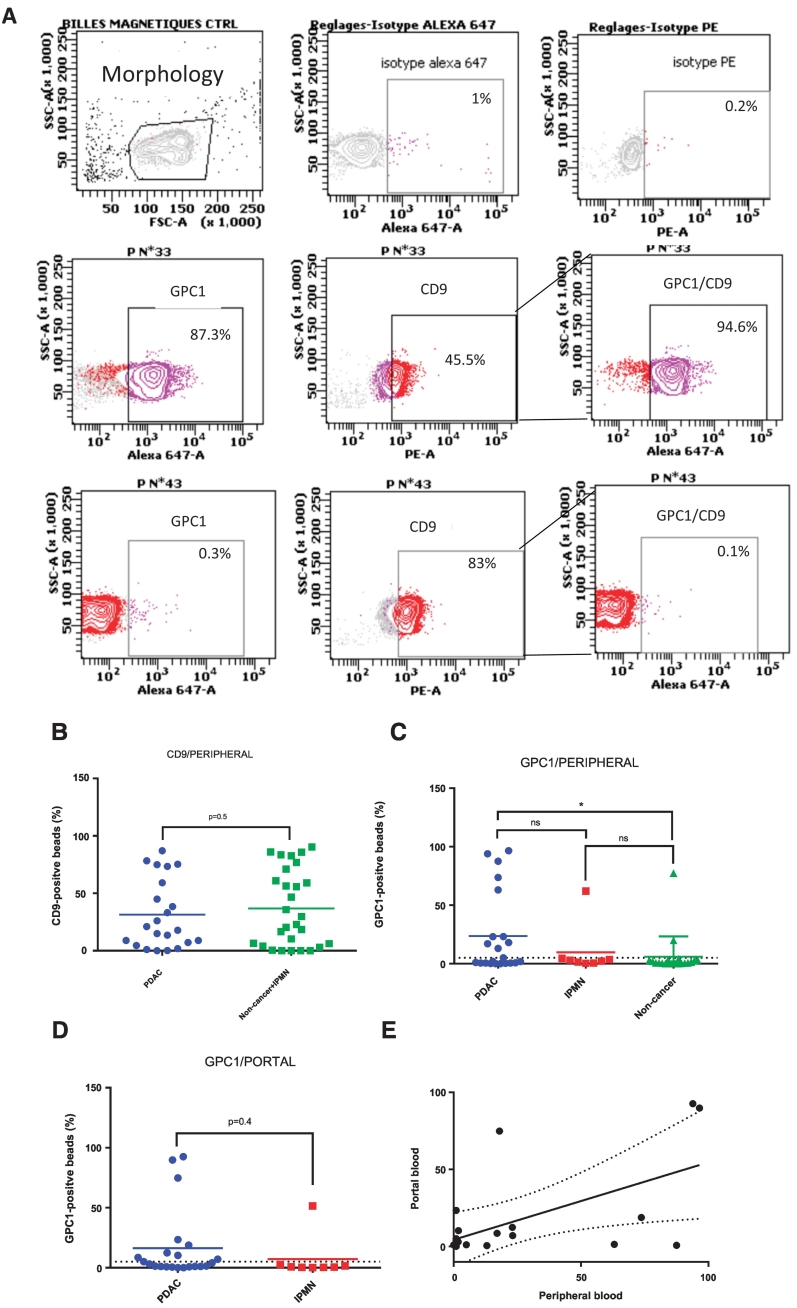
Previous data reported that PDAC exosomes overexpressed both CD63 and GPC1 as measured by alternative current electrokinetic (ACE) [17]. In their working model the authors used both biomarkers to discriminate PDACs from healthy donors. Our total EV GPC1 levels were similar in both groups by western blot, so we hypothesized that pooling down CD63-positive EVs followed by GPC1 detection would distinguish cancer patients from non-cancer controls. First, anti-CD63 magnetic beads were used to obtain CD63-positive exosomes from peripheral blood. As expected, they were positive for the exosome specific CD9 marker with no difference between PDAC and control groups, including healthy volunteers and patients with IPMNs (P = .5, Figure 3, A and B, Table 2). Interestingly, mean percentages of GPC1-positive beads were significantly higher in the PDAC group as compared to non-cancer patients (23.7 ± 7.31, n = 22 and 5.7 ± 3.88, n = 20, respectively, P = .04 by unpaired Student's t test, Figure 3, A and C, Table 2). The IPMN group was not significantly different from both other groups (9.71 ± 7.50, n = 8, P > .05 by unpaired Student's t test). The positivity threshold for GPC1 exosomes calculated using the Youden index was 5%. Fifty percent of the patients were above this threshold.
Figure 3.
GPC1-positive exosomes partially identify PDAC patients.
(A) Representative dot plots of PDAC and controls for the quantification of positive exosomes for the exosome specific marker CD9, and the GPC1 protein. Top three panels show bead detection according to physical criteria (size, FSC and granularity, SSC, left panel), rabbit igG isotype control Alexa Fluor 647 control stain (medium top panel) and PE mouse IgG1 Kappa isotype (right top panel). Three medium panels show representative results for a PDAC patient and lower three panels show representative results for a control. Percentages of stained beads are indicated in each dot plot. GPC1/CD9 results correspond to % of GPC1-positive beads within the CD9-positive population. Individual results are plotted for each group of participants, for CD9-positive exosome counts in peripheral blood (B), GPC1-positive exosome counts in peripheral blood (C), GPC1-positive exosome counts in portal blood (D). Correlation of GPC1-positive exosome counts in peripheral blood versus portal blood has been plotted in (E). The dashed lines delineate the positivity threshold. Ns: not significant. ∗: P < .05.
Table 2.
Numeric results of exosome quantification in PDAC patients and control group.
| Sample | PDAC group | Control group |
|---|---|---|
| Portal samples (n) | 22 | 8 (IPMN) |
| Peripheral samples (n) | 22 | 28 |
| CD9 positive (n (%)) peripheral blood | 22 (100%) | 28 (100%) |
| CD9 positive beads rate peripheral blood mean (med; range) | 31.4 (19.45;1-87.1) | 42.7 (41.2;1-90.3) |
| CD9 positive beads (n (%)) portal blood | 22 (100%) | 8 (100%) |
| CD9 positive beads rate portal blood mean (med; range) | 22.5 (12.45;1-94) | 36.4 (40;1-91.8) |
| GPC1 positive (n (%)) peripheral blood | 11 (50%) | 3 (10.7%) |
| GPC1 positive beads rate peripheral blood mean (med; range) | 23.7 (3.45;1-96.5) | -IPMN:9.71 (2.65;0.3-62.1) |
| -Control (without-IPMN n = 20): 5.7 (0.7;0-77.3) | ||
| -Control (with IPMN n = 28): 7.02 (1.35;0-77.3) |
||
| GPC1 positive (n (%)) portal blood | 10 (46%) | 1 (12%) |
| GPC1 positive beads rate portal blood mean (med; range) | 16.33 (3.6;1-92.6) | 7.3 (0.7;0.6-51.4) |
| GPC1 positive portal and peripheral n (%) | 14 (63%) | 3 (10.7%) |
med, median; PDAC, pancreatic ductal adenocarcinoma; IPMN, intraductal papillary and mucinous neoplasm.
GPC1 Positive Exosomes in Portal Blood
We hypothesized that circulating tumor exosomes could be more numerous in a blood sample drawn from the portal vein, near the tumor, as compared to peripheral blood drawn from the median cephalic vein. Portal samples were obtained only in the operated patients. GPC1-positive bead percentages were not significantly different in peripheral and portal samples (16.33 ± 6.19, n = 22 and 7.3 ± 6.31, n = 8, respectively, P = .42, Figure 3D), even if they tended to be lower in the portal samples. Next, as we had both portal and peripheral blood samples of the 31 patients we assessed whether GPC1-positive bead percentages matched between samples (Figure 3E). Three patients presented discordant results, but overall, percentages were correlated with Pearson's test (ρ = 0.59, P = .037).
Diagnostic Performance
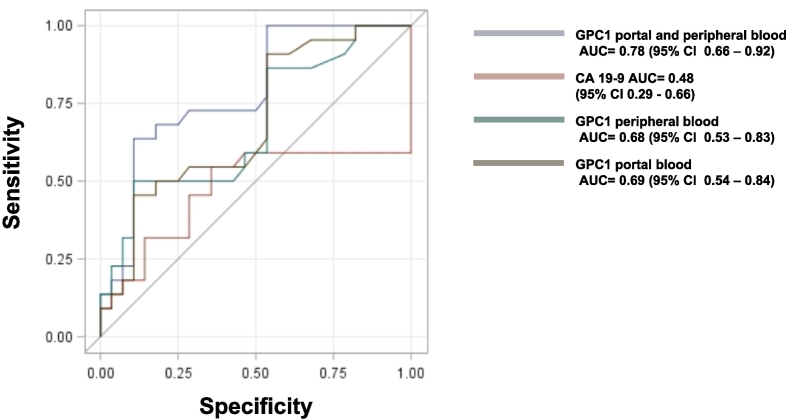
Diagnostic performance was evaluated by determining accuracy, sensitivity and specificity (Table 3). Overall, diagnosis accuracy of GPC1-positive exosomes was better in peripheral blood than in portal blood. A total of 63% (14 out of 22) of patients were detected for GPC1 positive exosomes in portal and/or peripheral blood. Both sampling sites showed better performance than CA19-9. EUS-FNA carried strong specificity, but poor negative predictive value, as expected. Interestingly, combining all three diagnostic tools led to high sensitivity and specificity (82% and 86%, respectively), and highest diagnosis accuracy (84%, Table 3). ROC curves showed that GPC1-positive exosomes in peripheral blood displayed higher area under the curve (AUC) than CA19-9 in peripheral blood (Figure 4).
Table 3.
Diagnosis values of GPC1 positive exosomes, CA19-9 and EUS-FNA
| Test | Sensitivity (95% CI) | Specificity (95%CI) | Positive predictive value (95%CI) |
Negative predictive Value (95%CI) |
Diagnosis accuracy (95%CI) |
|---|---|---|---|---|---|
| EVs GPC1 portal vein | 46 (27-66) |
88 (53-99) |
91 (63-99) |
36 (20-59) |
57 (50-64) |
| EVs GPC1 peripheral vein | 50 (31-70) |
90 (77-99) |
79 (58-98) |
70 (54-82) |
72 (65-78) |
| ∗EVs GPC1 peripheral and/or portal vein | 64 (43-81) |
90 (73-97) |
83 (59-94) |
76 (59-88) |
78 (72-83) |
| CA19-9 | 37 (19-59) |
87 (72-95) |
63 (36-85) |
69 (54-82) |
68 (61-74) |
| EUS FNA (n = 18; PDAC n = 15; IPMN n = 3) | 60 (36-81) |
100 (31-99) |
100 (60--99) |
33 (13-65) |
66 (59-73) |
| ∗EVs GPC1 and CA19-9 | 72 (52-87) |
93 (78-99) |
89 (68-99) |
81 (65-92) |
84 (78-89) |
| CA19-9 and EUS-FNA | 50 (31-70) |
92 (78-99) |
86 (58-98) |
70 (55-83) |
74 (67-80) |
| ∗EVs GPC1 and EUS FNA | 73 (52-87) |
86 (69-95) |
80 (59-92) |
80 (63-91) |
80 (74–85) |
| ∗EVs GPC1 + CA19-9+ EUS FNA | 82 (62-93) |
86 (69-95) |
82 (62-93) |
86 (69-95) |
84 (78-89) |
PDAC, pancreatic ductal adenocarcinoma; IPMN, intraductal papillary and mucinous neoplasm; EUS-FNA endoscopic ultrasound-guided fine needle aspiration. ∗EVs GPC1, quantification in peripheral and portal vein.
Figure 4.
ROC curves for GPC1-positive exosomes and CA19–9.
The ROC curves were built with data obtained from peripheral blood for markers used alone (GPC1-positive exosome (green curve) and CA 19–9(pink curve)), or for GPC1-positive exosome measured in portal blood (brown curve), or for combined GPC1-positive exosomes measured in portal and peripheral blood (gray curve); for each pair, we took the lowest %GPC1+ exosomes of PDAC and the highest lowest %GPC1+ exosomes of controls. AUC, area under the curve.
ctDNA Detection
All patients and controls were negative for circulating KRAS mutant DNA in peripheral or portal blood, whereas both our metastatic patients had detectable KRAS mutant alleles (data not shown and mutant allelic frequency in peripheral blood: 1.6% and 0.6%; in portal blood 0.41%and 0.4%). Thus, ctDNA did not distinguish PDAC patients from controls.
Importantly, all primary tumors were KRAS mutant with a mean mutant allele frequency of 26.15 (Table 1).
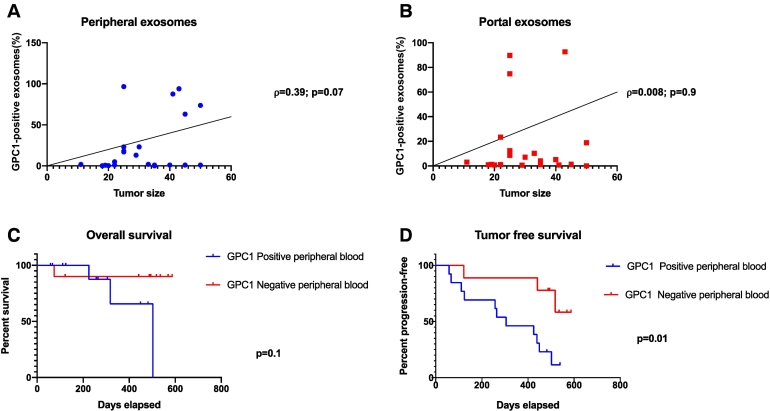
Correlation of Exosome Levels to Clinicohistopathologic Risk Factors and Prognostic Values
The median follow-up was 18 months (range 2-23). All data were included until December 2018. A low positive correlation between the percentage of GPC1-positive exosomes in peripheral blood (Figure 5A), but not in portal blood (Figure 5B) and the tumor size was found (Pearson's test ρ = 0.39, Figure 5A), with a p value close to statistical significance (P = .07). Exosome rate did not correlate with other histolopathological parameters, including tumor stage, the number of invaded lymph nodes and carcinoma differentiation. Despite the short follow-up period (median 554 days; mean 532 days; range 74-718 days) and the small size of the cohort, we analyzed the exosome results in the context of the clinical follow-up. Among the 22 patients, 14 developed tumor recurrences (64%), including metastatic relapses in the liver and other organs. Four patients died (18%). Kaplan–Meier analysis indicated that overall survival did not correlate patients with GPC1 positive exosome in peripheral blood above the threshold (Figure 5C) but they relapsed sooner than patients with GPC1-positive exosomes below the threshold (P = .01, Figure 5D).
Figure 5.
Analysis of GPC1-positive exosome quantification according to clinical and pathological criteria.
(A) Pearson correlation between positive GPC1 exosomes in peripheral blood and tumor size. (B) Pearson correlation between positive GPC1 exosomes in portal blood and tumor size. (C) Overall survival according to presence of GPC1-positive exosomes in peripheral blood. (D) Tumor free survival according to presence of GPC1-positive exosomes in peripheral blood. Positivity threshold for GPC1 positive exosomes = 5% as determined by Youden's index. ρ, Pearson correlation coefficient.
Thus, the diagnostic value of GPC1 positive exosomes is superior when combining portal and peripheral analyses, but the prognostic value is only retained for GPC1 positive exosomes in the peripheral blood.
Discussion
Tumor EVs carry sufficient information to control the activity of recipient cells, whether they are tumoral [20] or healthy [21], leading to responses supporting tumor growth or dissemination. Thus, they seem to be very relevant material as circulating tumor biomarkers carriers, such as nucleic acids, proteins or lipids. In this way, the identification of GPC1-positive exosomes as highly specific and sensitive biomarkers to diagnose PDAC was very exciting [11]. A few reports have been published to test this potentially powerful diagnostic tool. Our study aimed at confirming this breakthrough finding in a group of PDAC patients eligible for up-front surgery, considered detected early in the course of the disease [22]. Moreover, as for circulating tumor cells, it is possible that such patients might release less tumor-related elements in the blood circulation as the disease is less advanced [23], making their detection even more challenging.
First, we detected GPC1 protein at the expected size in vesicle-enriched sera by western-blot and found no difference in signal intensity between patients and healthy controls. We tested very few samples (n = 4 in each group) as the main aim of our work was to quantify GPC1-positive exosomes. Increasing the number of samples might identify significant differences in both groups as published for serum GPC1 levels measured by ELISA [24]. This latter work however, found that serum GPC1 was inferior to CA19-9 in terms of diagnosis accuracy, suggesting that this approach is not relevant for PDAC.
The first publication proposing GPC1-positive exosomes for identifying PDAC reported 100% sensitivity and 100% specificity [11]. Yang et al. [16] described an EV protein signature (EGFR, EpCAM, MUC1, HER2, GPC1 and WNT2), by measuring antibody-linked fluorescence intensity of ultracentrifuged plasma EVs, identifying PDAC with a diagnostic accuracy of 84%, a sensitivity of 86% and a specificity of 81%. Detecting GPC1 alone showed a lower diagnosis accuracy of 67%, a sensitivity of 82% and a specificity of 52% (n = 43). We found a similar accuracy of 72% but a lower sensitivity (50%) and a higher specificity (90%). In addition, Lai et al. [15] did not report diagnostic performance for GPC1-positive exosome but did not find significant difference in levels of GPC1 protein in exosomes from PDAC versus controls, in small groups (n = 3 and n = 6, respectively), and using LC–MS/MS, although a trend for higher expression was visible. In the same way, Frampton et al. were unable to distinguish PDAC from benign pancreatic disease using ultracentrifuged plasma and ELISA [25]. A recent publication identified PDAC patients with alternating current electrokinetic (ACE) microarray chip, capturing nanoscale objects, including exosomes, directly from plasma, followed by immunofluorescent detection and quantification of CD63 and GPC1. Although high sensitivity and specificity (99% and 82%, respectively) were achieved, false-positive and false-negative results were obtained [17]. Even more recently, enumeration of GPC1-positive EVs, solely or in conjunction with Glycoprotein 2, did not distinguish PDAC from benign pancreatic diseases, using direct EVs detection with a nanoscale flow cytometer and an anti-GPC1 antibody different from Melo's [26]. Thus, GPC1 positive exosome quantification showed various results in terms of diagnostic accuracy. The discrepancies might originate from different technical approaches to measure exosome-GPC1 levels. For example, with our approach, it is possible that the reagent used to isolate EVs might interfere with GPC1 immunodetection on the magnetic beads. We did test ultracentrifugation followed by latex beads coupling and did not distinguish PDAC from controls (n = 6 PDACs n = 19 controls, not shown). Thus, as the first enrichment step in EVs, we used a density-based separation kit coupled to magnetic beads decorated with anti-CD63, limiting the analysis to the exosome population [27]. CD9 positivity was various among patients. This could be explained by the variety of EVs presenting the CD63 tetraspanin at their surface, such as non exosomal microvesicles [28]. We used the same antibody as Melo, because this parameter seemed crucial in reproducing their results. This approach improved PDAC patient identification. Our results are similar to already published results [15], [16], [25].
As blood from portal vein is enriched in circulating tumor cells [29], [30], we hypothesized that GPC1-positive EVs were more numerous in portal samples. To our knowledge, this series is the first testing GPC1-EVs in portal vein samples. In fact, we found that although not significantly different, GPC1-positive EVs tended to be less concentrated in portal blood as compared to peripheral blood. Sensitivity and specificity were similar but positive predictive value was higher (91% vs 79%) suggesting that that portal sample can improve PDAC identification. Moreover, combined results found better AUC in ROC curves (Figure 4). In the same way, combining peripheral and portal blood analysis led to better diagnostic performance (Table 3). Noticeably, this approach is valid since portal blood sampling is feasible. Indeed, authors reported sampling of portal vein for 18 patients during EUS FNA for circulating tumor cells enrichment [31].
As already published, ctDNA did not identify early stage PDAC as we only detected our two metastatic patients [23]. Recently, it was reported that quantifying tumor DNA in exosome might not be more useful since only 25% to 29% of PDAC patient had KRAS or TP53 mutant DNA in exosomes [16].
Our cohort is prospective and homogenous since composed of patients all eligible for up-front surgery, which was confirmed by histopathological analysis. Previous studies identifying circulating tumor elements in PDAC included mainly advanced stages or metastatic patients. At this stage of the disease, our control group is interesting because it consists of heterogeneous pathologies, two patients with chronic pancreatitis and eight patients with pre-neoplastic cystic lesions. Nevertheless, the cohort presents limits. In particular, the number of patients is small and conclusions need to be validated in a larger prospective cohort. This is especially true when we analyzed correlations between exosomes levels and clinicohistopathologic data. Pearson correlation coefficient showed a low positive correlation between exosomes levels and tumor size and P value was 0.07. This is in accordance with a recent study showing that patients with high GPC1 in circulating exosomes had larger tumors [12], [25].It is probable that increasing cohort size would reach statistical significance. Importantly, as previously suggested, our results even on a small cohort show that GPC1-positive exosomes carry prognostic value for disease relapse [12], [24]. Determining the levels of GPC1-positive exosomes might help setting up neoadjuvant strategy for these patients [32].
Traditional tools for the diagnosis of PDAC include CA19-9 and histologic proof currently obtained by EUS-FNA [10]. Patients with early-stage disease are more difficult to diagnose by EUS-FNA. Cytopathological specimens, may reach high sensitivity (75%–98%), specificity (71%–100%), but are not devoid of post-procedure morbidity, especially pancreatitis. The presence of pancreatitis decreases sensitivity to 74% as compared to 91% with normal surrounding pancreatic parenchyma. Current data show that the negative predictive value of EUS-FNA actually ranks between 33 and 85% [3], [10], [33]. This is probably due to the histological nature of the tumor, rich in fibrosis and often poor in tumor cells. Our series presented the most difficult diagnostic conditions since patients were all at an early stage with small lesions. Moreover, PDAC management tends now to perform neoadjuvant therapy even for patients eligible for up-front surgery. So, the low negative predictive value of EUS-FNA is becoming problematic [5]. Quantifying GPC1 positive EVs in the peripheral and/or the portal blood as a companion test might improve the diagnostic leading to a negative predictive value of 80% (as compared to 33% for EUS-FNA alone).
CA19-9 had sensitivity and specificity as low as 70% and 68% respectively, which is in agreement to recommendations to not use it routinely for diagnosis [7], [8]. In the same way, CA19-9 is not a good prognostic marker for early stages [9]. Accordingly, we found a very low sensitivity (37%) and a specificity of 87%. Interestingly however, combining all three diagnostic tools, i.e. GPC1-positive EVs, CA19-9 and EUS-FNA improved all diagnostic performance parameters (Table 3), and displayed the best diagnosis accuracy (84%). Consequently, it would be very interesting to test in a larger cohort a patient early management strategy including GPC1-positive exosome quantification. Indeed, liquid biopsy is a very low risk procedure and additional cost is manageable.
Acknowledgments
Acknowledgements
The authors are grateful to Katia Obama and Isabelle Lamy for administrative assistance and fund management. We thank the Pr. Louis Buscail and Pr. Jean-Philippe Merlio for critical reading of the manuscript. We thank the Cancer Biobank of CHU Bordeaux for contribution (no. BRIF: BB-0033-00036).
Author's contributions
EB: conception, design, analysis, assembly and interpretation of data, financial support, manuscript writing.
AC: collection and assembly of data, interpretation of data.
PQ: collection and assembly of data, interpretation of data.
OD: collection and assembly of data, interpretation of data.
CB: Statistical analyses.
IL: collection and assembly of data.
IM: collection and assembly of data.
CC: design, collection of data, interpretation of data.
SV: design, collection of data, interpretation of data.
AB: design, final approval of the manuscript.
MM: analysis and interpretation of data, final approval of the manuscript.
LC: design, patient inclusion, final approval of the manuscript.
CL: design, patient inclusion, final approval of the manuscript.
VV: interpretation of data, final approval of the manuscript.
FMG: design, financial support, final approval of the manuscript.
ABe: conception, design, analysis, interpretation of data, final approval of the manuscript.
SD: conception, design, collection, analysis, assembly and interpretation of data, financial support, manuscript writing.
Conflict of interest
The authors declare no conflict of interest.
Funding
This research was supported in part by Patrick Brou de Laurière Fondation and the Celgene company. It was funded by the Groupement Interregional de Recherche Clinique et d'Innovation Sud-Ouest OutreMer (GIRCI-SOOM).
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 2.Buscail L. Commentary: Pancreatic cancer: is the worst to come? Int J Epidemiol. 2017;46:1774–1775. doi: 10.1093/ije/dyx143. [DOI] [PubMed] [Google Scholar]
- 3.Storm AC, Lee LS. Endoscopic ultrasound-guided techniques for diagnosing pancreatic mass lesions: Can we do better? World J Gastroenterol. 2016;22:8658–8669. doi: 10.3748/wjg.v22.i39.8658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Best LM, Rawji V, Pereira SP, Davidson BR, Gurusamy KS. Imaging modalities for characterising focal pancreatic lesions. Cochrane Database Syst Rev. 2017;4 doi: 10.1002/14651858.CD010213.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gobbi PG, Bergonzi M, Comelli M, Villano L, Pozzoli D, Vanoli A. The prognostic role of time to diagnosis and presenting symptoms in patients with pancreatic cancer. Cancer Epidemiol. 2013;37:186–190. doi: 10.1016/j.canep.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Goonetilleke KS, Siriwardena AK. Systematic review of carbohydrate antigen (CA 19-9) as a biochemical marker in the diagnosis of pancreatic cancer. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2007;33:266–270. doi: 10.1016/j.ejso.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Wu E, Zhou S, Bhat K, Ma Q. CA 19-9 and pancreatic cancer. Clin Adv Hematol Oncol HO. 2013;11:53–55. [PMC free article] [PubMed] [Google Scholar]
- 8.Poruk KE, Gay DZ, Brown K, Mulvihill JD, Boucher KM, Scaife CL. The clinical utility of CA 19-9 in pancreatic adenocarcinoma: diagnostic and prognostic updates. Curr Mol Med. 2013;13:340–351. doi: 10.2174/1566524011313030003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bhat K, Wang F, Ma Q, Li Q, Mallik S, Hsieh T-C. Advances in biomarker research for pancreatic cancer. Curr Pharm Des. 2012;18:2439–2451. doi: 10.2174/13816128112092439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou B, Xu J-W, Cheng Y-G, Gao J-Y, Hu S-Y, Wang L. Early detection of pancreatic cancer: Where are we now and where are we going? Int J Cancer. 2017;141:231–241. doi: 10.1002/ijc.30670. [DOI] [PubMed] [Google Scholar]
- 11.Melo SA, Luecke LB, Kahlert C, Fernandez AF, Gammon ST, Kaye J. Glypican-1 identifies cancer exosomes and detects early pancreatic cancer. Nature. 2015;523:177–182. doi: 10.1038/nature14581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu H, Niu F, Liu F, Gao J, Sun Y, Zhao X. Elevated glypican-1 expression is associated with an unfavorable prognosis in pancreatic ductal adenocarcinoma. Cancer Med. 2017;6:1181–1191. doi: 10.1002/cam4.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kleeff J, Ishiwata T, Kumbasar A, Friess H, Büchler MW, Lander AD. The cell-surface heparan sulfate proteoglycan glypican-1 regulates growth factor action in pancreatic carcinoma cells and is overexpressed in human pancreatic cancer. J Clin Invest. 1998;102:1662–1673. doi: 10.1172/JCI4105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Christianson HC, Svensson KJ, van Kuppevelt TH, Li J-P, Belting M. Cancer cell exosomes depend on cell-surface heparan sulfate proteoglycans for their internalization and functional activity. Proc Natl Acad Sci U S A. 2013;110:17380–17385. doi: 10.1073/pnas.1304266110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lai X, Wang M, McElyea SD, Sherman S, House M, Korc M. A microRNA signature in circulating exosomes is superior to exosomal glypican-1 levels for diagnosing pancreatic cancer. Cancer Lett. 2017;393:86–93. doi: 10.1016/j.canlet.2017.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang KS, Im H, Hong S, Pergolini I, Del Castillo AF, Wang R. Multiparametric plasma EV profiling facilitates diagnosis of pancreatic malignancy. Sci Transl Med. 2017;9 doi: 10.1126/scitranslmed.aal3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lewis JM, Vyas AD, Qiu Y, Messer KS, White R, Heller MJ. Integrated analysis of exosomal protein biomarkers on alternating current electrokinetic chips enables rapid detection of pancreatic cancer in patient blood. ACS Nano. 2018;12:3311–3320. doi: 10.1021/acsnano.7b08199. [DOI] [PubMed] [Google Scholar]
- 18.Lafitte M, Moranvillier I, Garcia S, Peuchant E, Iovanna J, Rousseau B. FGFR3 has tumor suppressor properties in cells with epithelial phenotype. Mol Cancer. 2013;12:83. doi: 10.1186/1476-4598-12-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nat Methods. 2012;9:671–675. doi: 10.1038/nmeth.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Steinbichler TB, Dudás J, Riechelmann H, Skvortsova I-I. The role of exosomes in cancer metastasis. Semin Cancer Biol. 2017;44:170–181. doi: 10.1016/j.semcancer.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 21.Kalluri R. The biology and function of exosomes in cancer. J Clin Invest. 2016;126:1208–1215. doi: 10.1172/JCI81135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Versteijne E, Vogel JA, Besselink MG, Busch ORC, Wilmink JW, Daams JG. Meta-analysis comparing upfront surgery with neoadjuvant treatment in patients with resectable or borderline resectable pancreatic cancer. Br J Surg. 2018;105:946–958. doi: 10.1002/bjs.10870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Imamura T, Komatsu S, Ichikawa D, Kawaguchi T, Miyamae M, Okajima W. Liquid biopsy in patients with pancreatic cancer: Circulating tumor cells and cell-free nucleic acids. World J Gastroenterol. 2016;22:5627–5641. doi: 10.3748/wjg.v22.i25.5627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou C-Y, Dong Y-P, Sun X, Sui X, Zhu H, Zhao Y-Q. High levels of serum glypican-1 indicate poor prognosis in pancreatic ductal adenocarcinoma. Cancer Med. 2018;7:5525–5533. doi: 10.1002/cam4.1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frampton AE, Prado MM, López-Jiménez E, Fajardo-Puerta AB, Jawad ZAR, Lawton P. Glypican-1 is enriched in circulating-exosomes in pancreatic cancer and correlates with tumor burden. Oncotarget. 2018;9:19006–19013. doi: 10.18632/oncotarget.24873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lucien F, Lac V, Billadeau DD, Borgida A, Gallinger S, Leong HS. Glypican-1 and glycoprotein 2 bearing extracellular vesicles do not discern pancreatic cancer from benign pancreatic diseases. Oncotarget. 2019;10:1045–1055. doi: 10.18632/oncotarget.26620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tauro BJ, Greening DW, Mathias RA, Ji H, Mathivanan S, Scott AM. Comparison of ultracentrifugation, density gradient separation, and immunoaffinity capture methods for isolating human colon cancer cell line LIM1863-derived exosomes. Methods San Diego Calif. 2012;56:293–304. doi: 10.1016/j.ymeth.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 28.Willms E, Cabañas C, Mäger I, Wood MJA, Vader P. Extracellular Vesicle Heterogeneity: Subpopulations, Isolation Techniques, and Diverse Functions in Cancer Progression. Front Immunol. 2018;9:738. doi: 10.3389/fimmu.2018.00738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bissolati M, Sandri MT, Burtulo G, Zorzino L, Balzano G, Braga M. Portal vein-circulating tumor cells predict liver metastases in patients with resectable pancreatic cancer. Tumour Biol J Int Soc Oncodevelopmental Biol Med. 2015;36:991–996. doi: 10.1007/s13277-014-2716-0. [DOI] [PubMed] [Google Scholar]
- 30.Denève E, Riethdorf S, Ramos J, Nocca D, Coffy A, Daurès J-P. Capture of viable circulating tumor cells in the liver of colorectal cancer patients. Clin Chem. 2013;59:1384–1392. doi: 10.1373/clinchem.2013.202846. [DOI] [PubMed] [Google Scholar]
- 31.Catenacci DVT, Chapman CG, Xu P, Koons A, Konda VJ, Siddiqui UD, et al. Acquisition of Portal Venous Circulating Tumor Cells From Patients With Pancreaticobiliary Cancers by Endoscopic Ultrasound. Gastroenterology. 2015;149:1794–1803.e4. [DOI] [PMC free article] [PubMed]
- 32.Qian L, Yu S, Chen Z, Meng Z, Huang S, Wang P. Functions and clinical implications of exosomes in pancreatic cancer. Biochim Biophys Acta Rev Cancer. 1871;2018:75–84. doi: 10.1016/j.bbcan.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 33.McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS. Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2018;24:4846–4861. doi: 10.3748/wjg.v24.i43.4846. [DOI] [PMC free article] [PubMed] [Google Scholar]