Abstract
Background:
Congenital insensitivity to pain (CIP) is an extremely rare condition in which there is a failure of the development of the afferent sensory nerves in the dorsal root ganglia resulting in indifference to painful stimuli. The associated orthopedic manifestations are various and often present a diagnostic quandary for the treating surgeon.
Purpose:
This population study provides insight into the orthopedic manifestations and functional scores in patients with CIP, to guide prognosis and management.
Patients and Methods:
We retrospectively review and describe the orthopedic manifestations of all cases of CIP in Malta. All patients were then scored for upper and lower limb function using the abridged version of the Disability of Arm, Shoulder, and Hand score (QuickDASH) and the Lower Extremity Functional Score (LEFS).
Results:
Nine patients were recruited in total. Mean age at the time of recruitment into this study was of 33.7 years (range 15–58). All patients were Caucasian of Maltese heritage. None had consanguineous parents. All patients had been diagnosed with the condition in childhood (mean age 8.9 years). In total, these patients had 6 long bone fractures, 1 vertebral fracture, 39 upper limb surgical procedures, 88 lower limb surgical procedures, and 7 major lower limb amputations. These are discussed in detail. The main QuickDASH score was 23.97. The main LEFS was 42.22.
Conclusions:
This paper is the first population-based study of this condition and one of the largest series with functional scores. A multidisciplinary approach is essential in managing these patients. The surgical treatment of these conditions is often difficult and protracted, and judicious and careful consideration to both the bony and soft tissues aspects of the management need to be taken into account, with functional limb amputation not necessarily being considered as a last resort.
Keywords: Amputation, congenital insensitivity to pain, osteomyelitis, pediatrics
Introduction
Congenital insensitivity to pain (CIP) is a form of hereditary sensory and autonomic neuropathy (HSAN type IV). It is an extremely rare condition in which there is a failure of the development of the afferent sensory nerves in the dorsal root ganglia resulting in indifference to painful stimuli. If associated with failure of the autonomic sympathetic innervation of the sweat glands, patients with this condition will also suffer from anhidrosis. Furthermore, alteration in the function of nerve growth factor, in turn, alters the normal process of fracture consolidation.1 Normal osteoblast differentiation and proliferation are hindered, tending to result in fibroblast differentiation of pluripotent stromal mesenchymal cells and periosteal cells. Bone metabolism is also affected by the lack of nociceptive fibers in the skin and skeletal system.2 Due to the trophic role that nociceptive fibers may play in the skeletal system, bone fractures are common.3 Most of the orthopedic manifestations relate to the neuropathic arthropathy rather than to the fractures. The dissolution and fragmentation seen as part of the natural history of this condition is an expression of this. As we will illustrate, the high complication rate of treatment with the failure of fusions is probably related to this neuropathy and normal process of osteoblast function.
The first reference to CIP was in the early 1900s, and a review of the literature showed that overall only a few cases of this condition have been reported, with no study focusing on the orthopedic manifestations and management of CIP, or on obtaining functional scores from these patients.4,5,6,7,8,9,10
We describe our experience of nine patients with CIP. They all had several musculoskeletal problems including, fractures, avascular necrosis, joint dislocations, soft tissue, and bone infections requiring a multitude of surgical procedures. The severity and combination of these problems presented complex diagnostic and therapeutic dilemmas. Apart from reviewing the orthopedic manifestations, upper and lower limb functional scores were assessed in this cohort of patients. We hope this paper will provide clinicians with insight into the natural history and the likely course of events in patients with CIP to guide prognosis and management.
Patients and Methods
All nine patients identified as having the condition were recruited to the study. All patients were diagnosed by joint clinical and laboratory assessments carried out by a neurologist and a pediatrician. In the older patients, the diagnosis was confirmed following a sural nerve biopsy or using a quantitative sweat test and/or an intradermal histamine test. In two of the younger patients, formal genetic analysis was performed.
All patients who presented to any Maltese medical institution with features of CIP were included. The exclusion criteria were patients with arthropathy that was not due to CIP, patient refusal to be a part of the study (n = 0), patient or legal guardian unable to give consent (n = 0), or patients known to have CIP but with missing or incomplete medical notes (n = 1). Due to the small size of the island of Malta and the fact that there are only two main state hospitals, which have one common orthopedic department, we feel this cohort of patients represents the total number of patients with CIP in the Maltese Islands.
Written consent was obtained for inclusion in the study in all cases. The clinical review was performed by the authors, and upper limb and lower limb function scores obtained. The validated functional scores used in this series were the abridged version of the Disability of Arm, Shoulder, and Hand score (QuickDASH) score and the Lower Extremity Functional Score (LEFS). Patient notes and imaging were reviewed by the senior authors from birth until study recruitment. All patients were followed up until the point of collection of data and writing of the paper.
Results
There were five females and four males. The mean age at the time of recruitment into this study was of 33.7 years (range 15–58). All patients were Caucasian of Maltese heritage. None had consanguineous parents. All patients had been diagnosed with the condition in childhood (mean age 8.9 years).
Of the eight patients, there were siblings from two separate families (Cases 1, 2, and 7 in one family and Cases 4 and 6 in another family), two patients who were distant cousins (Cases 3 and 8) and one seemingly isolated case in a family (Case 5). All had unaffected parents. In all patients, there was no documented mental retardation.
Two patients (Cases 2 and 7) had documented delayed milestones in childhood. In the majority of cases, the most severe manifestations were present peripherally, in the hands and feet, with the neuropathy decreasing more centrally. One patient had a documented vertebral wedge fracture, which was attributed to a fall during wheelchair transfers (Case 7) and being less likely to be related to her CIP. The details of the lower and upper limb manifestations are elaborated on further beneath the relevant subheadings in the Discussion section.
Tables 1 and 2a-c summarize the demographic details, ambulatory, and mental status of the patients, and some of the main orthopedic manifestations in this cohort of patients. In Table 2, the figures in parenthesis alongside each surgical procedure represent the documented number of times that particular procedure was formally performed in theatre. A revision procedure is indicated by the repeated annotation of the same procedure on the same body part.
Table 1.
Demographics of patients suffering from congenital insensitivity to pain
| Case | Gender | Current age | Age at diagnosis | Affected siblings | Ambulatory status | Mental status |
|---|---|---|---|---|---|---|
| 1 | Male | 39 | 16 | 2 | Independently mobile | Normal |
| 2 | Male | 25 | 5 | 2 | Independently mobile | Normal |
| 3 | Male | 37 | 8 | 1* | Independently mobile for short distances | Normal |
| 4 | Female | 43 | 6 | 1 | Independently mobile | Normal |
| 5 | Female | 58 | 8 | 1 | Wheelchair ambulator | Normal |
| 6 | Female | 18 | 10 | 1 | Independently mobile | Normal |
| 7 | Female | 34 | 10 | 2 | Wheelchair ambulator | Normal |
| 8 | Female | 34 | 8 | 0 | Independently mobile | Normal |
| 9 | Male | 15 | 5 | 0 | Community wheelchair ambulatory, home independent ambulator | Normal |
*One sibling still undergoing genetic testing at the time of writing this paper although clinical manifestations are consistent with CIP. CIP=Congenital insensitivity to pain
Table 2a.
Summary of orthopedic patients suffering from congenital insensitivity to pain (continued on next page)
| Case | Limbs and joints affected | Long bone fractures (excluding phalanges) | Surgical procedures of upper limb** | Surgical procedures of lower limb** | Major amputations of upper limb*** | Major amputations of lower limb*** |
|---|---|---|---|---|---|---|
| 1 | Bilateral feet and ankles; right knee; bilateral hands | None | Debridement of bilateral hand ulcers (3) | Bilateral foot and ankle debridements (4); ankle washout and stabilization with spanning ankle external fixator (1); right knee fusion (1) | None | Left below knee amputation |
| 2 | Bilateral feet and ankles; right knee | None | None | Bilateral foot and ankle debridements (4); right hindfoot fusion (2); right knee fusion (1) | None | None |
| 3 | Bilateral feet and hands; bilateral femurs | Right first metatarsal; right femoral diaphysis; left proximal femur | Progressive fingertip debridements (23); all distal phalanges amputated left hand; amputation of distal and middle phalanges all fingers right hand, and of both phalanges of thumb | Toe debridements (14); left foot forefoot amputation; nonspanning external fixator right femur (1); plate fixation left femur (1) | None | None |
| 4 | Right foot and ankle | None | None | Bilateral foot and ankle debridements (11); open ankle washout (1) | None | None |
**Figure in parenthesis represents the total number of individual operative procedures, ***Excludes amputations of up to 2 phalanges (hand or foot)
Table 2c.
Summary of orthopedic patients suffering from congenital insensitivity to pain
| Case | Limbs and joints affected | Long bone fractures (excluding phalanges) | Surgical procedures of upper limb** | Surgical procedures of lower limb** | Major amputations of upper limb*** | Major amputations of lower limb*** |
|---|---|---|---|---|---|---|
| 9 | Both hands and feet; right knee; left leg | None | Debridement fingertip ulcers and flexor sheath infections (4); Debridement right thumb osteomyelitis (3) | Debridement toe and foot ulcers (18); right hallux amputation; left hallux amputation; surgical exploration metatarsal osteomyelitis (1); amputation lesser toes left foot (2); right knee arthroscopic washout (3) | None | Left midfoot (Chopart) amputation (2); trans-tibial amputation left leg (1) |
**Figure in parenthesis represents the total number of individual separate operative procedures, ***Excludes amputations of up to 2 phalanges (hand or foot)
Table 2b.
Summary of orthopedic patients suffering from congenital insensitivity to pain
| Case | Limbs and joints affected | Long bone fractures (excluding phalanges) | Surgical procedures of upper limb** | Surgical procedures of lower limb** | Major amputations of upper limb*** | Major amputations of lower limb*** |
|---|---|---|---|---|---|---|
| 5 | Notes incomplete. Excluded from data gathering on manifestations but included in functional score review | |||||
| 6 | Right foot and ankle; left forefoot; bilateral hands and wrists | None | Fingertip debridements (6) | Arthroscopic removal of lateral talar dome osteochondral defect (1); right subtalar fusion (2) | None | None |
| 7 | Bilateral feet and ankles, right knee; bilateral wrists; lumbar spine | None | Bilateral wrist washouts (awaiting left wrist fusion) | Debridement foot wounds (5); Arthroscopic washout of right knee (3); left hindfoot fusion with circular frame (2); spanning external fixator right knee (1); right knee fusion (1) | None | Bilateral below knee amputations |
| 8 | Bilateral feet and ankles; left forearm; left leg | Proximal left tibial fracture; left distal tibial fracture; left ulnar shaft fracture. | None | Debridement foot wounds (4); left hindfoot fusion (1); right pantalar fusion (1); right hallux amputation (1); left ankle triple fusion (1) | None | Left below knee amputation |
**Figure in parenthesis represents the total number of individual separate operative procedures, ***Excludes amputations of up to 2 phalanges (hand or foot)
Figures 1-10 illustrate some of the radiographic findings of these patients. Each figure is annotated with the corresponding case.
Figure 1.

Images showing extensive left ankle destruction (Case 8)
Figure 10.

Nonunion of a proximal femoral fracture following infective failure of fixation (Case 3)
Figure 2.

Radiographs of a patient with a failed hindfoot fusion (Case 2)
Figure 3.
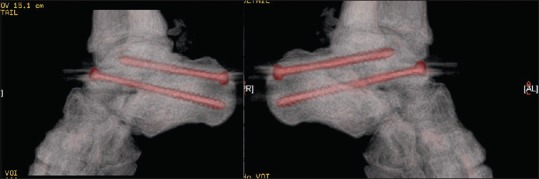
CT reconstructions of the patient with a successful hindfoot fusion (Case 6)
Figure 4.
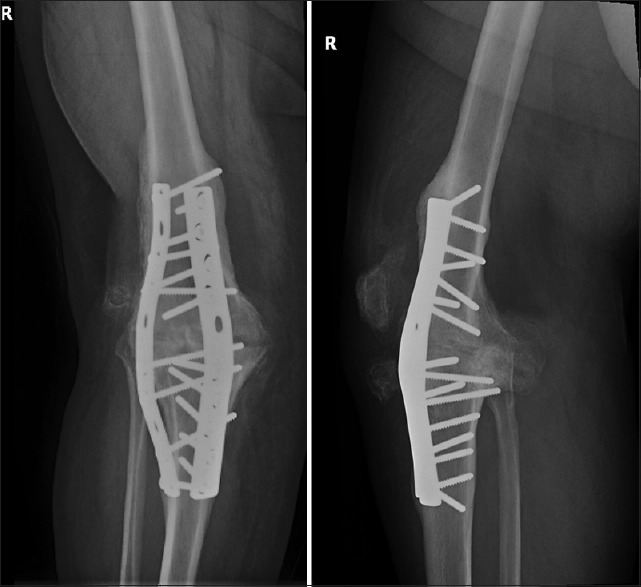
Radiographs of a patient who had successful knee fusion (Case 1)
Figure 5.
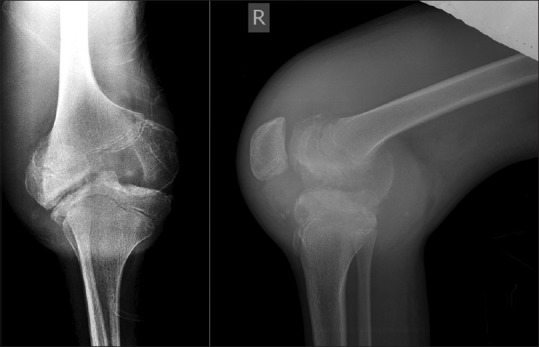
Radiographs showing painless knee destruction in a pediatric patient (Case 9)
Figure 6.

Radiographs of a painless ulnar fracture associated with the use of walking aids due to extensive lower limb manifestations (Case 8)
Figure 7.

Radiograph of a foot showing amputation of all toe phalanges and distal metatarsals (Case 3)
Figure 8.

Radiographs showing distal phalangeal involvement in one patient (Cases 3)
Figure 9.

Radiographs of a patient with wrist arthropathy and destruction (Case 7)
Lower limb manifestations
All patients had lower limb manifestations that varied greatly in severity and will be described by joint below.
Foot and ankle
Painless infected ulcers were located typically at toes or at the medial and plantar midfoot due to planovalgus or rockerbottom feet commonly seen in Charcot foot. Wound debridement, followed by cast immobilization, was the mainstay of treatment in these cases.
As the mid-foot and hind-foot destruction progressed through the recognized stages of a neuropathic foot, that is from the initial acute fragmentation to coalescence to attempted reconstitution and consolidation, the surgical management centered around extensive debridement and supramaximal fixation. This was not without risk of complications as the altered pain and healing response in these patients compounded by the potential risk for persistent deep low-grade infection meant that the arthrodesis was likely to fail to unite fully. This was the case in all five patients who underwent this procedure. On further review, two of these cases had persistent painless hindfoot movement and instability (Cases 1 and 6); one underwent a revision hindfoot fusion (Case 2); while the other three required a below-knee amputations (Cases 7, 8, and 9). The techniques employed for fusion in our patients ranged from traditional screws to the use of circular frames.
Knee
Knee joint destruction with or without fractures around the knee joint often resulted in significant instability and deformity. In the four cases with significant knee destruction (Cases 1, 2, 7, and 9), we initially employed the use of casts or hinged knee braces, walking aids, and/or the use of a wheelchair. Three patients subsequently required a knee arthrodesis (Cases 1, 2, and 7); this was performed using a plate in two cases, and an external fixator in the third case.
One patient (Case 3) had two separate posttraumatic femoral fractures, one of which was treated conservatively and the other operatively with a proximal femoral plate. Even though the proximal femoral fracture progressed to infective nonunion requiring plate removal, the patient was still able to mobilize short distances without a wheelchair.
Amputations
In this series, five major lower limb amputations were performed in four patients in the presence of major bone destruction, osteomyelitis, or significant systemic upset and sepsis. In general, these patients did well if the amputation was carried out through a relatively more sensate level (see functional scores), but the need to use walking aides for a prolonged time lead to upper limb complications in some cases. Two of the three patients with major lower limb amputations required wheelchairs for community ambulation. One, however, did well with a below-knee amputation prosthesis and ambulated independently.
Upper limb manifestations
The upper limb manifestations in our series can broadly be divided into two categories. The first category and most common manifestation were spontaneous or posttraumatic fingertip ulcers that often required community care and protracted courses of oral antibiotics, but sometimes required formal surgical debridement (Cases 3, 6, and 9) and eventually phalangeal amputation (Cases 3 and 9). Two of the cases who had significant and persistent fingertip wounds had pronounced anhidrosis, which contributed to the formation of deep skin cracks and subsequent infection.
The second category of upper limb manifestations was those related to the use of walking aides. In Case 1, 7, and 8, patients developed bony changes to their hand, wrist or forearms related to the increased use of crutches and wheelchairs. One patient, Case 8, developed an insufficiency fracture of the ulna following the use of a walking aid that required cast immobilization for 8 weeks. Another patient, Case 7, developed bilateral carpal destruction due to prolonged use of a wheelchair and crutches while rehabilitating from bilateral below knee amputations.
There were no major upper limb amputations in any of the patients in our series.
Microorganisms and antibiotics
The spectrum of microorganisms cultured from the numerous wound swabs and tissue samples submitted for culture and sensitivity was large and varied, with the majority of the organisms being of the genus Staphylococcus or Streptococcus, and various species subtypes. Pseudomonas was also a common genus encountered. Furthermore, organisms resistant to several antibiotics and certain superbugs such as methicillin-resistant Staphylococcus aureus were also often cultured. This is related to the use of antibiotics for several weeks and months to treat chronic ulcers, and also to the high prevalence of these microbes in the community.
Upper and lower limb functional scores
The validated functional scores used in this series were the abridged version of the Disability of Arm, Shoulder and Hand score, the QuickDASH score and the LEFS.11,12 These results are shown below in Table 3.
Table 3.
Upper (Quick disability of arm, shoulder, and hand) and lower limb (lower extremity functional score) functional scores
| Case | QuickDASH 0 (min)=No disability 100 (max)=Most disability | LEFS 0 (min)=Very low function 80 (max)=Very high function |
|---|---|---|
| 1 | 13.6 | 54 |
| 2 | 11.4 | 15 |
| 3 | 36.8 | 40 |
| 4 | 0 | 52 |
| 5 | 0 | 58 |
| 6 | 0 | 53 |
| 7 | 72.7 | 15 |
| 8 | 0 | 59 |
| 9 | 81.25 | 34 |
LEFS=Lower extremity functional score, DASH=Disability of arm, shoulder, and hand
Discussion
CIP is an extremely rare autosomal recessive disorder first described in 1963.9 It is characterized by profound insensitivity to painful stimuli with or without the absence of sweating, as well as complications such as repeated injuries, often involuntarily self-inflicted, bony destruction, recurrent febrile episodes, and even sepsis.13,14 Delayed developmental milestones, hyperactivity, emotional lability, and intellectual disability are also observed to varying degrees.15
CIP is characterized by the absence of sensory and sympathetic postganglionic neurons.16,17,18 There is a genetic loss-of-function mutation of the NTKR1 gene amongst other more recently described mutations19,20,21 which are beyond the remit of this clinical paper. This lack of neurons is present not only in the skin but also in the skeletal system and due to the trophic role that nociceptive fibers may play in the skeletal system, bone fractures are very common.2,3
Although the genetics of the condition is relatively well understood, knowledge of the condition itself among medical practitioners, its manifestations, and the therapeutic options is less well understood.4,22,23,24 Furthermore, there is little in the literature on the effect this condition has on the overall function of patients with this debilitating condition. This paper is a population study encompassing both clinical manifestation and limb functional scores.
As illustrated in our paper, the majority of orthopedic manifestations of this condition involve the foot and ankle. Most patients had infected toe ulcers that necessitated prolonged antibiotic courses and both outpatient and inpatient wound care. However, recurrent midfoot involvement with the development of chronic trophic ulcers often required more intensive inpatient care, prolonged cast immobilization and was more likely in our series to lead to surgical treatment of the bony destruction. This destruction results in significant deformity, albeit painless, which has implications on mobility and gait; hence, the aim of surgery was to try to maintain the midfoot and hindfoot in a position of function. Due to the neuropathy with the absence of any protective sensation, the associated impaired bone healing, as well as protracted deep infections, fusions of the midfoot and hindfoot in our series, were not without complications, with only one patient having a relatively satisfactory result with incomplete union but enough joint stability to function normally. Two cases who underwent foot fusions went on to require below knee amputations due to persistent infection and bony destruction, and a further case was asymptomatic with no evidence of sepsis or skin breakdown despite the fact that he had a complete failure of the fusion at the time of writing this paper. The situation was similar in those patients who required knee fusion due to extensive bony destruction when neither of the two patients who underwent the attempted arthrodesis procedure had a successfully fused and stable knee joint at long term followup.
In patients with early changes such as those seen in HSAN types III, the osteonecrosis and osteochondral fragments are typically more amenable to surgical treatment. However, in CIP (HSAN type IV), progression to Charcot arthropathy affecting both sides of the involved joint with evidence of collapse and fragmentation and joint subluxation or dislocation mean joint preservation surgery is often not an option. This is supported by Feldman et al.25
One patient had documented spinal collapse with significant back pain that limited mobility (Case 7). Since this was painful, it was likely that the fracture was an insufficiency fracture rather than due to CIP.
Upper limb manifestations in our series were less common and less severe. While fingertip wounds and infections were common, these often did not require formal amputation and could be treated conservatively with rest, elevation in a sling, regular wound cleaning, and debridement and if necessary, antibiotics. In our series, only two patients required formal amputations of fingertips due to persistent infected nonhealing ulcers. Although this study was not powered to assess for an association between the two, there is a possible link between anhidrosis and severity of the hand ulcers. Therefore, we feel that one of the mainstays of prevention and treatment of hand ulcers is proper hand care and hygiene combined with the use of topical emollients to prevent skin breakdown. Furthermore, the use of walking aids for prolonged periods was associated with wrist and distal forearm manifestations. In two patients (Cases 7 and 8), the prolonged use of crutches and walking aids resulted in significant wrist destruction in one patient, and a distal ulnar fracture in another. In a third patient (Case 3), the prolonged use of a wheelchair due to femoral fractures resulted in multiple hand ulcers that required a long course of treatment.
The functional scores used were the QuickDASH score to assess upper limb function and the LEFS score for lower limb function. Both scores are widely used and validated tools of upper and lower limb function.11,12,26,27,28 Our results demonstrate that in most cases, despite the limb manifestations of this condition, the functional scores are higher than would be expected. This is likely to be due to three points; first, the early presentation and manifestations of this condition allows children and patients to adapt and learn to cope and function well; second, the anatomical changes evolve gradually over time, therefore allowing them to adjust to the new structure of their anatomy; and third, the absence of pain means that even in the most badly deformed or infected limbs, patients are still able to make use of the affected limb. The need for a major limb amputation was not always associated with a high degree of loss of function. In our series, two of the patients who underwent below-knee amputations (Cases 1 and 8) had among the highest lower limb functional scores (54/80 and 59/80, respectively). Conversely, loss of phalanges and protracted hand or wrist manifestations were associated with greater losses of upper limb function, as illustrated by Cases 3 and 7, with both having decreased grip strength.
From our experience of treating these patients, we would recommend the following. When treating the lower limb manifestations, an essential part of the preventative treatment is a daily thorough inspection of the feet and ankles by the patient and/or by a relative to identify pressure areas early. When ulcers develop, these should be graded according to the Wagner grading system for neuropathic ulcers and the treatment tailored accordingly.29 The mainstay of treatment should be conservative with pressure-free casts, strict nonweight bearing, regular wound review and debridement as necessary. The use of antibiotics should be avoided as much as possible unless evidence of cellulitis or osteomyelitis due to the likelihood of requiring antibiotics in the future as well as the risk of developing multidrug-resistant bacteria. Should surgery be required to debride an infected wound or bone, the debridement should be thorough and in liaison with plastic surgeons as these patients often require definitive soft tissue cover. In cases of joint instability, the timing of surgery is of the utmost importance. We would recommend a period of close in-patient rest of the affected limb and monitoring with regular clinical review and the aid of diagnostic tools such as inflammatory markers, bone scans, and magnetic resonance imaging (MRI) to ensure surgery is performed when there are no signs of deep infection and careful soft-tissue coverage can be planned preoperatively if necessary. Furthermore, we feel that patients should be counseled early about the potential need for major limb amputation, the reasons being twofold. First, because complex mid-foot and hindfoot fusions tend to be fraught with complications and second because if the patient develops aggressive osteomyelitis proximal to the ankle joint and/or systemic sepsis, major limb amputation is the only treatment option available to treat the persistent lower limb infections and bone destruction.
With regard to the treatment of the upper limb manifestations, we recommend good hand hygiene and regular use of topical emollients. The application of the latter also gives the patients an opportunity to inspect the hand for insensate injuries. Once patients develop ulcers on the hand, these should be treated with rest, elevation in a sling, regular wound cleaning and debridement and antibiotics, if required. Surgical debridement should be reserved for those patients in whom a strict period of rest, elevation and wound cleaning has failed to prevent the development of osteomyelitis. Similarly to the lower limb cases, we advocate a period of close preoperative monitoring and investigation with an MRI scan to ensure excision of all infected bone and soft tissue of dubious viability, followed by adequate soft-tissue coverage.
A multidisciplinary approach is essential and should involve a pediatrician or neurologist depending on the age of the patient, a geneticist and clinical psychologist in the early diagnostic stages. With orthopedic manifestations, the team should also include an orthopedic surgeon, infection disease specialist, musculoskeletal radiologist, physiotherapist, and occupational therapist, with access to an orthotist and prosthetist.
This paper is the first population-based study of this condition and one of the larger series with functional scores. There are certainly other aspects to the condition that needs to be further investigated. These include patient-related aspects such as the effects of the condition on the patients’ quality of life, psychosocial and employment issues. From a health service aspect, analysis of the impact of this condition and its treatment on the orthopedic service, with regard to cost, as well as issues such as having patients with open wounds and possibly multi-resistant bacteria in wards with patients who have recently undergone a joint arthroplasty or insertion of metalwork.
Conclusions
This paper is the first population-based study of this condition and one of the largest series with functional scores. A multidisciplinary approach is essential in managing these patients. The surgical treatment of these conditions is often difficult and protracted, and judicious and careful consideration to both the bony and soft tissues aspects of the management need to be taken into account, with functional limb amputation not necessarily being considered as a last resort.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published, and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
Each author certifies that he/she has no commercial associations (e.g. consultancies, stock ownership, equity interest, and patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Melamed I, Levy J, Parvari R, Gelfand EW. A novel lymphocyte signaling defect: Trk a mutation in the syndrome of congenital insensitivity to pain and anhidrosis (CIPA) J Clin Immunol. 2004;24:441–8. doi: 10.1023/B:JOCI.0000029106.84310.5e. [DOI] [PubMed] [Google Scholar]
- 2.Derwin KA, Glover RA, Wojtys EM. Nociceptive role of substance-P in the knee joint of a patient with congenital insensitivity to pain. J Pediatr Orthop. 1994;14:258–62. doi: 10.1097/01241398-199403000-00024. [DOI] [PubMed] [Google Scholar]
- 3.Hill EL, Elde R. Distribution of CGRP-, VIP-, D beta H-, SP-, and NPY-immunoreactive nerves in the periosteum of the rat. Cell Tissue Res. 1991;264:469–80. doi: 10.1007/BF00319037. [DOI] [PubMed] [Google Scholar]
- 4.Bar-On E, Weigl D, Parvari R, Katz K, Weitz R, Steinberg T, et al. Congenital insensitivity to pain. Orthopaedic manifestations. J Bone Joint Surg Br. 2002;84:252–7. doi: 10.1302/0301-620x.84b2.11939. [DOI] [PubMed] [Google Scholar]
- 5.Dearborn G. A case of congenital general pure analgesia. J Nerv Ment Dis. 1932;75:612–5. [Google Scholar]
- 6.Gao L, Guo H, Ye N, Bai Y, Liu X, Yu P, et al. Oral and craniofacial manifestations and two novel missense mutations of the NTRK1 gene identified in the patient with congenital insensitivity to pain with anhidrosis. PLoS One. 2013;8:e66863. doi: 10.1371/journal.pone.0066863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pérez-López LM, Cabrera-González M, Gutiérrez-de la Iglesia D, Ricart S, Knörr-Giménez G. Update review and clinical presentation in congenital insensitivity to pain and anhidrosis. Case Rep Pediatr. 2015;2015:589852. doi: 10.1155/2015/589852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosemberg S, Marie SK, Kliemann S. Congenital insensitivity to pain with anhidrosis (hereditary sensory and autonomic neuropathy type IV) Pediatr Neurol. 1994;11:50–6. doi: 10.1016/0887-8994(94)90091-4. [DOI] [PubMed] [Google Scholar]
- 9.Swanson AG. Congenital insensitivity to pain with anhydrosis. A unique syndrome in two male siblings. Arch Neurol. 1963;8:299–306. doi: 10.1001/archneur.1963.00460030083008. [DOI] [PubMed] [Google Scholar]
- 10.Tunçbilek G, Oztekin C, Kayikçioǧlu A. Calcaneal ulcer in a child with congenital insensitivity to pain syndrome. Scand J Plast Reconstr Surg Hand Surg. 2005;39:180–3. doi: 10.1080/02844310410004865. [DOI] [PubMed] [Google Scholar]
- 11.Beaton DE, Wright JG Katz JN Upper Extremity Collaborative Group. Development of the QuickDASH: Comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87:1038–46. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]
- 12.Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale (LEFS): Scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation research Network. Phys Ther. 1999;79:371–83. [PubMed] [Google Scholar]
- 13.Freeman R. Autonomic peripheral neuropathy. Lancet. 2005;365:1259–70. doi: 10.1016/S0140-6736(05)74815-7. [DOI] [PubMed] [Google Scholar]
- 14.van den Bosch GE, Baartmans MG, Vos P, Dokter J, White T, Tibboel D, et al. Pain insensitivity syndrome misinterpreted as inflicted burns. Pediatrics. 2014;133:e1381–7. doi: 10.1542/peds.2013-2015. [DOI] [PubMed] [Google Scholar]
- 15.Axelrod FB, Gold-von Simson G. Hereditary sensory and autonomic neuropathies: Types II, III, and IV. Orphanet J Rare Dis. 2007;2:39. doi: 10.1186/1750-1172-2-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Langer J, Goebel HH, Veit S. Eccrine sweat glands are not innervated in hereditary sensory neuropathy type IV. An electron-microscopic study. Acta Neuropathol. 1981;54:199–202. doi: 10.1007/BF00687742. [DOI] [PubMed] [Google Scholar]
- 17.Nolano M, Crisci C, Santoro L, Barbieri F, Casale R, Kennedy WR, et al. Absent innervation of skin and sweat glands in congenital insensitivity to pain with anhidrosis. Clin Neurophysiol. 2000;111:1596–601. doi: 10.1016/s1388-2457(00)00351-5. [DOI] [PubMed] [Google Scholar]
- 18.Swanson AG, Buchan GC, Alvord EC., Jr Anatomic changes in congenital insensitivity to pain. Absence of small primary sensory neurons in ganglia, roots, and Lissauer's tract. Arch Neurol. 1965;12:12–8. doi: 10.1001/archneur.1965.00460250016002. [DOI] [PubMed] [Google Scholar]
- 19.Indo Y, Mardy S, Tsuruta M, Karim MA, Matsuda I. Structure and organization of the human TRKA gene encoding a high affinity receptor for nerve growth factor. Jpn J Hum Genet. 1997;42:343–51. doi: 10.1007/BF02766957. [DOI] [PubMed] [Google Scholar]
- 20.Indo Y, Tsuruta M, Hayashida Y, Karim MA, Ohta K, Kawano T, et al. Mutations in the TRKA/NGF receptor gene in patients with congenital insensitivity to pain with anhidrosis. Nat Genet. 1996;13:485–8. doi: 10.1038/ng0896-485. [DOI] [PubMed] [Google Scholar]
- 21.Lin YP, Su YN, Weng WC, Lee WT. Novel neurotrophic tyrosine kinase receptor type 1 gene mutation associated with congenital insensitivity to pain with anhidrosis. J Child Neurol. 2010;25:1548–51. doi: 10.1177/0883073810375464. [DOI] [PubMed] [Google Scholar]
- 22.Daneshjou K, Jafarieh H, Raaeskarami SR. Congenital insensitivity to pain and anhydrosis (CIPA) syndrome; a report of 4 cases. Iran J Pediatr. 2012;22:412–6. [PMC free article] [PubMed] [Google Scholar]
- 23.Nabiyev V, Kara A, Aksoy MC. Multidisciplinary assessment of congenital insensitivity to pain syndrome. Childs Nerv Syst. 2016;32:1741–4. doi: 10.1007/s00381-016-3059-5. [DOI] [PubMed] [Google Scholar]
- 24.Zhang Y, Haga N. Skeletal complications in congenital insensitivity to pain with anhidrosis: A case series of 14 patients and review of articles published in Japanese. J Orthop Sci. 2014;19:827–31. doi: 10.1007/s00776-014-0595-2. [DOI] [PubMed] [Google Scholar]
- 25.Feldman DS, Ruchelsman DE, Spencer DB, Straight JJ, Schweitzer ME, Axelrod FB, et al. Peripheral arthropathy in hereditary sensory and autonomic neuropathy types III and IV. J Pediatr Orthop. 2009;29:91–7. doi: 10.1097/BPO.0b013e31818f9cc4. [DOI] [PubMed] [Google Scholar]
- 26.Kennedy CA, Beaton DE. A user's survey of the clinical application and content validity of the DASH (Disabilities of the arm, shoulder and hand) outcome measure. J Hand Ther. 2017;30:30–40.e2. doi: 10.1016/j.jht.2016.06.008. [DOI] [PubMed] [Google Scholar]
- 27.Mehta SP, Fulton A, Quach C, Thistle M, Toledo C, Evans NA, et al. Measurement properties of the lower extremity functional scale: A systematic review. J Orthop Sports Phys Ther. 2016;46:200–16. doi: 10.2519/jospt.2016.6165. [DOI] [PubMed] [Google Scholar]
- 28.Pan SL, Liang HW, Hou WH, Yeh TS. Responsiveness of SF-36 and lower extremity functional scale for assessing outcomes in traumatic injuries of lower extremities. Injury. 2014;45:1759–63. doi: 10.1016/j.injury.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 29.Wagner FW., Jr The diabetic foot. Orthopedics. 1987;10:163–72. doi: 10.3928/0147-7447-19870101-28. [DOI] [PubMed] [Google Scholar]


