Abstract
Background:
Contemporary ceramic articulation in total hip arthroplasty (THA) has shown successful clinical and radiologic outcomes at mid-to-long term. Delta ceramic, which includes 24% zirconia, has been developed to reduce the rate of ceramic fracture. However, the phase transformation of the zirconia that might cause surface roughness, ceramic wear, and subsequent osteolysis remains a concern. The purpose of this study was to evaluate clinicoradiological outcomes, ceramic-related complications, and survivorship of THA with the use of hybrid ceramic bearing; BIOLOX delta liner-on-BIOLOX forte head articulation at a minimum followup of 10 years.
Materials and Methods:
One hundred cementless THAs (85 patients) were performed with the use of 36-mm hybrid ceramic bearing. The thickness of the delta ceramic liner was 4–6 mm. Four patients (4 hips) were lost and six patients (6 hips) died within 10 years after the operation. Thus, the remaining 75 patients (90 hips) were followed up for 10–12 years. There were 43 men and 32 women. The mean age of these patients at the index operation was 58 years (21–78 years).
Results:
There were no fractures of ceramic liner or head. There was no measurable ceramic wear, and neither pelvic nor femoral osteolysis was identified. All acetabular and femoral components were bone-ingrown. Three (3/90, 3.3%) patients noted noise of clicking sound. The mean Harris hip score was 87 points (range 72–99 points) at the time of final followup. THA survivorship with revision surgery as an endpoint was 97.8% (95% confidence interval: 91.4%–99.8%).
Conclusions:
The long term result of cementless THA with the use of a large BIOLOX forte head on the BIOLOX delta liner showed an encouraging result. Wear or osteolysis associated with composite of 24% zirconia in the fourth-generation ceramic was not observed at a minimum followup of 10 years.
Keywords: Cementless, delta liner, large diameter femoral head, survival, total hip arthroplasty
Introduction
Contemporary alumina ceramic bearing was introduced to reduce wear. Although medium-to-long term followup results of ceramic total hip arthroplasty (THA) were encouraging, ceramic fracture appeared as a matter of concern.1,2,3 To reduce the incidence of ceramic fracture, the newest ceramic composite, so-called delta ceramic, which included 21% zirconium, was introduced in 2005.4,5,6,7,8,9,10,11
Composite of the fourth-generation ceramic can increase the strength and toughness of the material and reduce the fracture rate of ceramic. So far, fracture rates of the fourth-generation ceramics are much lower than those of the third-generation ceramic with short and mid term followups.9,10,11 In addition, clinical and radiologic outcomes of fourth-generation ceramics are comparable to those of third-generation ceramics.
Previously, we have reported a minimum 5-year followup study of BIOLOX delta liner-on-BIOLOX forte head articulation in patients with THA.12 There was no osteolysis or ceramic related complications such as fracture or squeaking.12 Although the fourth-generation ceramic articulation has successful clinical and radiologic outcomes with reduced fracture rates, the transformation of the zirconia that can cause surface roughness, ceramic wear, and subsequent osteolysis remains a concern.
Therefore, the purpose of this study was to assess the incidence of ceramic related complications, the survival rate of the implant, and clinicoradiological results of THA with use of the hybrid ceramic bearing at a minimum of 10-year followup.
Materials and Methods
This retrospective study was approved by the Institutional Review Board of our hospital. Between August 2005 and August 2007, 100 primary cementless THAs (85 patients) were done with the use of delta ceramic liner (BIOLOX Delta; CeramTec, Plochingen, Germany) and alumina ceramic head (BIOLOX Forte; CeramTec). The diameter of the ceramic head was 36 mm in all hips.
Acetabular component was a porous-coated hemispherical titanium cup (Delta PF, Lima-Lto, Lima, Udine, Italy). The thickness of the liner was 4–6 mm for all sizes of acetabular components. The femoral component was a tapered, rectangular, grit blasted, collarless titanium alloy stem (C2, Lima).
Four patients (4 hips) were not followed up for a minimum of 10 years, and 6 patients (6 hips) died within 10 years after the operation. In the remaining 75 patients (90 hips), the latest followup evaluations were done at 10–12 years (mean, 11 years) after the arthroplasty [Figure 1]. There were 43 men and 32 women. The mean age of these patients at the index operation was 58 years (range 21–78 years) and their body mass index ranged from 20.7 to 25.7 kg/m2. The primary diagnosis was femoral head osteonecrosis in 63 hips, osteoarthritis in 19, femoral neck fracture in five, rheumatoid arthritis in two, and sequelae of pyogenic infection in one hip. The mean preoperative Harris hip score was 36 points (range, 13–85 points).
Figure 1.
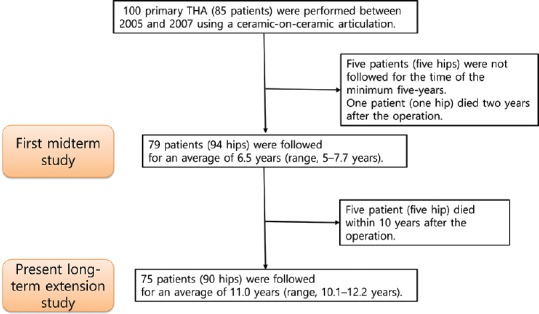
Flowchart of this study
All operations were performed by one surgeon using a posterolateral approach. All acetabular and femoral components were inserted in a press-fit manner. Patients were instructed to walk with partial weight-bearing using two crutches for 4 weeks after the arthroplasty.
Patients were followed at postoperative 6 weeks, 3, 6, 9, and 12 months, and yearly thereafter. At each visit, patients were asked whether they had any noise arising from the operated hip. If they had, the noise was classified as snapping, clicking, popping, grinding, or squeaking.13 Clinical evaluation was performed using the Harris hip scoring system. Radiographic evaluations included the assessment of fixation of femoral and acetabular components,14,15 ceramic components wear,16 osteolysis,17,18,19 and heterotopic ossification.20
Radiographic evaluations were done by two independent observers, who did not participate in the index operation. Details of clinical and radiological evaluations were described elsewhere.12
The Kaplan–Meier survival analysis was performed with the revision of either component as the endpoint.21
Results
There was no case of ceramic fracture until the time of final followup [Figure 2]. Three patients (3 hips, 3.3%) reported intermittent clicking sound. None of them had pain or any modification of daily activities. All clicking occurred when the patient was rising from a squatting position. No significant associations were found between hip noise and patient- or prosthesis-related factors, including age, sex, weight, height, body mass index, position of the implant, or neck length of the femoral component. Ten patients (10 hips, 10.6%) suffered intermittent thigh pain. In six hips, the pain disappeared during the followup. In four (4.4%) hips, the pain persisted until the latest followup. However, no patient needed any kind of medication or walking support. There was no symptomatic deep-venous thrombosis or pulmonary emboli. No patient had periprosthetic joint infection. The mean Harris hip score was 87 points (range 72–99 points) at the time of final followup.
Figure 2.
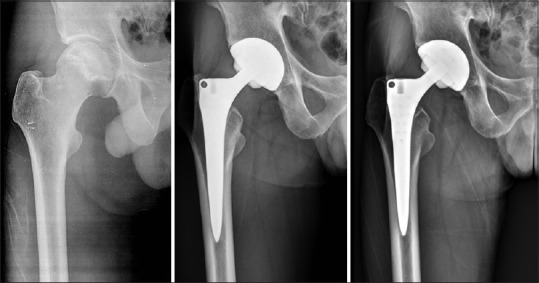
(a-c) A 51-year-old male underwent a total hip arthroplasty because of femoral head osteonecrosis. There was no detectible wear or osteolysis. Prostheses showed bone-ingrown stability on serial radiographs at preoperation (a), 5 years postoperatively (b), and 10 years after operation (c)
All acetabular cups and femoral stems had radiographic evidence of bone ingrown stability. All femurs had cortical thinning in the calcar femorale (Gruen zone 7) possibly due to the cancellation of the cortex.22 Thinning was evident at 3 months postoperatively, and was not progressive on serial radiographs. Three (3.3%) femurs had cortical hypertrophy in Gruen zone 5, which was evident at 6 months to 1 year after the operation. Periprosthetic osteolysis was not detected around any cup. Reactive radiolucent line was seen in the proximal femur (Gruen zones 1 and 7) of 27 (28.7%) hips. However, the radiolucent line did not progress distally on serial radiographs. There was no measurable wear in any of the 90 hips. Heterotopic ossification developed in seven hips (7.8%). Four hips had Grade-I ossification, and three had Grade-II ossification.
In one hip, a malseating of the ceramic liner with dissociation from the metal shell was detected at postoperative 5 days. It was treated with a change of the ceramic liner. One hip dislocated recurrently. In this case, malposition of the acetabular component (60° abduction and 0° anteversion) was thought to be the reason for dislocation. This hip was treated with a revision of the acetabular component. With revision surgery as an endpoint, the survivorship was 97.8% (95% confidence interval: 91.4%–99.8%) [Figure 3].
Figure 3.
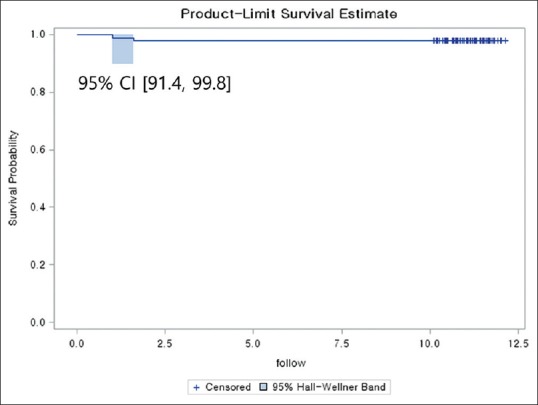
The Kaplan–Meier probability was 97.8% (95% confidence interval: 91.4%–99.8%) at followup of 12.2 years when revision for any reason was the end point
Discussion
Since the 1990s, the mechanical strength of alumina has been substantially improved. In 1995, third-generation alumina ceramic was introduced. The latest ceramic is delta ceramic, which incorporates 24% zirconia to alumina ceramic, was introduced in 2005.
In previous studies, the midterm results of the alumina and delta ceramic articulations were excellent.2,3,10
Previously, midterm survival rate of the fourth-generation ceramic articulations has been found to be excellent. However, we could not conclude that this type of ceramic coupling is safe and durable because BIOLOX delta liner includes 24% zirconia. A phase transformation of the zirconia is a possible cause of surface roughness, ceramic wear, and subsequent osteolysis.12 With a minimum followup of 10 years, clinical and radiologic results of this study were comparable to those of the previous study. Thus, the fourth-generation ceramic composite of 24% zirconia might not cause wear or osteolysis. This finding is consistent with a previous study of Choy et al.23 With component revision for any reason as an endpoint, they found that the survival rate was 96.7% without osteolysis due to phase transformation after a minimum followup of 10 years in 92 hips (85 patients) using alumina head on delta liner for THA.23
The fourth-generation ceramic bearing was developed to prevent ceramic fracture. However, most published studies were only case reports or small number series. Regarding ceramic fracture after using delta ceramic articulations, Howard et al.24 have recently analyzed data of 223,362 bearings from 111,681 primary CoC THAs and 182 linked revisions for bearing fracture using the National Joint Registry data and reported that the revision rate of ceramic fractures is 0.009% (7 out of 79, 442) for Biolox Delta heads, 0.119% (38 out of 31,982) for Biolox Forte heads, 0.126% (101 out of 80,170) for Biolox Delta liners, and 0.112% (35 of 31,258) for Biolox Forte liners. They reported that the fourth-generation of ceramic greatly reduced the odds of head fracture, but not that of liner fracture. This might be due to different mechanisms of ceramic fractures between head and liner.5,6 Ceramic liner fractures are associated with impingement between the neck of the femoral stem and the anterior rim. Although a large diameter articulation can reduce the risk of impingement and subsequent fracture of ceramic liner, malseated liner and suboptimally placed acetabular cup are also important risk factors for ceramic liner fracture.9,23,25 In this study, there was no ceramic fracture with a minimum followup of 10 years. However, other studies regarding the fourth-generation ceramics have consistently reported ceramic liner fracture due to impingement or malseated liner.9,23,25
This study has several limitations. First, this study was a retrospective one performed in a cohort of prospectively observed patients. Ten patients (10 hips) were lost of followup (4 patients) or deceased (6 patients) within the followup period of 10 years. However, causes of death in six patients were not related to THA. Second, in this study, we could not find wear or osteolysis at the latest followup and concluded that composite of 24% zirconia in the fourth-generation ceramic might not be cause of wear or osteolysis. However, we could not directly confirm phase transformation through retrieval analysis. Finally, although long term result of alumina head on delta liner articulation THA was successful in this study, these combinations are not popular. Further followup study might be mandatory.
Nevertheless these limitations, this hybrid articulation has several advantages. First, the fourth generation of ceramic liner has more fracture resistance than the third generation. Second, hybrid articulation has potential risk of phase transformation of zirconia and long term survivorship and this study could confirm safety and longevity. Finally, this hybrid articulation might be more cost-effectiveness than fourth-generation ceramic articulation.
Conclusions
The long term result of cementless THA with the use of a large BIOLOX forte head on BIOLOX delta liner showed an encouraging result. Wear or osteolysis associated with composite of 24% zirconia in the fourth-generation ceramic was not observed at a minimum followup of 10 years.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lee YK, Ha YC, Yoo JJ, Koo KH, Yoon KS, Kim HJ, et al. Alumina-on-alumina total hip arthroplasty: A concise followup, at a minimum of ten years, of a previous report. J Bone Joint Surg Am. 2010;92:1715–9. doi: 10.2106/JBJS.I.01019. [DOI] [PubMed] [Google Scholar]
- 2.Sugano N, Takao M, Sakai T, Nishii T, Miki H, Ohzono K, et al. Eleven- to 14-year followup results of cementless total hip arthroplasty using a third-generation alumina ceramic-on-ceramic bearing. J Arthroplasty. 2012;27:736–41. doi: 10.1016/j.arth.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 3.Kang BJ, Ha YC, Ham DW, Hwang SC, Lee YK, Koo KH, et al. Third-generation alumina-on-alumina total hip arthroplasty: 14 to 16-year followup study. J Arthroplasty. 2015;30:411–5. doi: 10.1016/j.arth.2014.09.020. [DOI] [PubMed] [Google Scholar]
- 4.Poggie RA, Turgeon TR, Coutts RD. Failure analysis of a ceramic bearing acetabular component. J Bone Joint Surg Am. 2007;89:367–75. doi: 10.2106/JBJS.F.00148. [DOI] [PubMed] [Google Scholar]
- 5.Ha YC, Kim SY, Kim HJ, Yoo JJ, Koo KH. Ceramic liner fracture after cementless alumina-on-alumina total hip arthroplasty. Clin Orthop Relat Res. 2007;458:106–10. doi: 10.1097/BLO.0b013e3180303e87. [DOI] [PubMed] [Google Scholar]
- 6.Koo KH, Ha YC, Jung WH, Kim SR, Yoo JJ, Kim HJ, et al. Isolated fracture of the ceramic head after third-generation alumina-on-alumina total hip arthroplasty. J Bone Joint Surg Am. 2008;90:329–36. doi: 10.2106/JBJS.F.01489. [DOI] [PubMed] [Google Scholar]
- 7.Lopes R, Philippeau JM, Passuti N, Gouin F. High rate of ceramic sandwich liner fracture. Clin Orthop Relat Res. 2012;470:1705–10. doi: 10.1007/s11999-012-2279-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lombardi AV, Jr, Berend KR, Seng BE, Clarke IC, Adams JB. Delta ceramic-on-alumina ceramic articulation in primary THA: Prospective, randomized FDA-IDE study and retrieval analysis. Clin Orthop Relat Res. 2010;468:367–74. doi: 10.1007/s11999-009-1143-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee YK, Ha YC, Yoo JI, Jo WL, Kim KC, Koo KH, et al. Mid-term results of the BIOLOX delta ceramic-on-ceramic total hip arthroplasty. Bone Joint J. 2017;99-B:741–8. doi: 10.1302/0301-620X.99B6.BJJ-2016-0486.R3. [DOI] [PubMed] [Google Scholar]
- 10.Kim YH, Park JW, Kim JS. Alumina delta-on-alumina delta bearing in cementless total hip arthroplasty in patients aged <50 years. J Arthroplasty. 2017;32:1048–53. doi: 10.1016/j.arth.2016.10.035. [DOI] [PubMed] [Google Scholar]
- 11.Buttaro MA, Zanotti G, Comba FM, Piccaluga F. Primary total hip arthroplasty with fourth-generation ceramic-on-ceramic: Analysis of complications in 939 consecutive cases followed for 2-10 years. J Arthroplasty. 2017;32:480–6. doi: 10.1016/j.arth.2016.07.032. [DOI] [PubMed] [Google Scholar]
- 12.Kang BJ, Ha YC, Hwang SC, Lee YK, Koo KH. Midterm results of large diameter biolox forte ceramic head on delta ceramic liner articulation in total hip arthroplasty. J Arthroplasty. 2014;29:2412–4. doi: 10.1016/j.arth.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 13.Jarrett CA, Ranawat AS, Bruzzone M, Blum YC, Rodriguez JA, Ranawat CS, et al. The squeaking hip: A phenomenon of ceramic-on-ceramic total hip arthroplasty. J Bone Joint Surg Am. 2009;91:1344–9. doi: 10.2106/JBJS.F.00970. [DOI] [PubMed] [Google Scholar]
- 14.Latimer HA, Lachiewicz PF. Porous-coated acetabular components with screw fixation. Five to ten-year results. J Bone Joint Surg Am. 1996;78:975–81. doi: 10.2106/00004623-199607000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–28. [PubMed] [Google Scholar]
- 16.Livermore J, Ilstrup D, Morrey B. Effect of femoral head size on wear of the polyethylene acetabular component. J Bone Joint Surg Am. 1990;72:518–28. [PubMed] [Google Scholar]
- 17.Engh CA, Hooten JP, Jr, Zettl-Schaffer KF, Ghaffarpour M, McGovern TF, Macalino GE, et al. Porous-coated total hip replacement. Clin Orthop Relat Res. 1994;298:89–96. [PubMed] [Google Scholar]
- 18.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 19.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: A radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 20.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–32. [PubMed] [Google Scholar]
- 21.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457. [Google Scholar]
- 22.Knutsen AR, Lau N, Longjohn DB, Ebramzadeh E, Sangiorgio SN. Periprosthetic femoral bone loss in total hip arthroplasty: Systematic analysis of the effect of stem design. Hip Int. 2017;27:26–34. doi: 10.5301/hipint.5000413. [DOI] [PubMed] [Google Scholar]
- 23.Choy WS, Cha YH, Jeon CY, Lee KS, Kim HY. A minimum ten years of followup of alumina head on delta liner total hip arthroplasty. J Arthroplasty. 2018;33:470–6. doi: 10.1016/j.arth.2017.08.043. [DOI] [PubMed] [Google Scholar]
- 24.Howard DP, Wall PD, Fernandez MA, Parsons H, Howard PW. Ceramic-on-ceramic bearing fractures in total hip arthroplasty: An analysis of data from the national joint registry. Bone Joint J. 2017;99-B:1012–9. doi: 10.1302/0301-620X.99B8.BJJ-2017-0019.R1. [DOI] [PubMed] [Google Scholar]
- 25.Baek SH, Kim WK, Kim JY, Kim SY. Do alumina matrix composite bearings decrease hip noises and bearing fractures at a minimum of 5 years after THA? Clin Orthop Relat Res. 2015;473:3796–802. doi: 10.1007/s11999-015-4428-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


