Abstract
Background. Effective antihypertensive treatment depends on patient compliance regarding prescribed medications. We assessed the impact of beliefs related towards antihypertensive medication on blood pressure control in a population-based sample treated for hypertension. Methods. We used data from the Characteristics and Course of Heart Failure Stages A-B and Determinants of Progression (STAAB) study investigating 5000 inhabitants aged 30 to 79 years from the general population of Würzburg, Germany. The Beliefs about Medicines Questionnaire German Version (BMQ-D) was provided in a subsample without established cardiovascular diseases (CVD) treated for hypertension. We evaluated the association between inadequately controlled hypertension (systolic RR >140/90 mmHg; >140/85 mmHg in diabetics) and reported concerns about and necessity of antihypertensive medication. Results. Data from 293 participants (49.5% women, median age 64 years [quartiles 56.0; 69.0]) entered the analysis. Despite medication, half of the participants (49.8%) were above the recommended blood pressure target. Stratified for sex, inadequately controlled hypertension was less frequent in women reporting higher levels of concerns (OR 0.36; 95%CI 0.17-0.74), whereas no such association was apparent in men. We found no association for specific-necessity in any model. Conclusion. Beliefs regarding the necessity of prescribed medication did not affect hypertension control. An inverse association between concerns about medication and inappropriately controlled hypertension was found for women only. Our findings highlight that medication-related beliefs constitute a serious barrier of successful implementation of treatment guidelines and underline the role of educational interventions taking into account sex-related differences.
1. Introduction
Although high blood pressure is a well modifiable risk factor, hypertension control remains unsatisfactory in the general population in Germany [1].
The reasons for noncompliance to pharmacotherapeutic recommendations are multifaceted. It has been proposed that patients' disease-modified beliefs may have a greater impact on medication adherence than external barriers as, e.g., cost, access to refills, logistic issues, or hospitalization [2–6]. The Necessity-Concern-Framework demonstrated that, in patients suffering from a variety of long-term conditions including hypertension, adherence to therapy was influenced by implicit judgments regarding personal needs for (i.e., necessity beliefs) and concerns about the prescribed medication [7]. The present investigation into medication-related beliefs focused on adherence measurement scales as primary outcome, rather than on objectively measured clinical outcomes, such as hypertension control.
We aimed to evaluate the impact of individuals' beliefs of specific-concerns and specific-necessity towards prescribed antihypertensive medication on inadequate blood pressure control and potential sex-related differences in a population-based sample of the general population without established cardiovascular disease (CVD) treated for hypertension.
2. Methods
We present data of the Characteristics and Course of Heart Failure Stages A–B and Determinants of Progression (STAAB) cohort study. The detailed study protocol and data collection have been published previously [8].
The Beliefs about Medicines Questionnaire developed by Horne was validated in a broad range of diseases, including cardiac samples, e.g., hypertension, to assess patient beliefs towards medication [9–11]. We used the Beliefs about Medicines Questionnaire specific subscales of the German version (BMQ-D) to assess personal beliefs about specific-concerns (6 items; e.g., danger of dependence or long-term toxicity) and specific-necessity of their prescribed medication (5 items; e.g., importance of prescribed therapy regarding their health status now and in the future), ranging from 1 “strongly disagree” to 5 “strongly agree”. Higher scores indicate higher levels of concerns (range 0-30) or necessity (range 0-25) [12]. A priori, a set of covariates was identified potentially related to blood pressure control including sociodemographic status (age, sex, and education), current smoking, self-reported diabetes, and body mass index (BMI) [13–16]. Sociodemographic status, self-reported diabetes, and information on current smoking were obtained via face-to-face interview. Blood pressure values were given as median of up to three valid measurements in sitting position. Study physicians assessed self-reported history of CVD (coronary artery disease, peripheral artery disease and stroke) and medication intake. BMI was calculated divided weight in kilograms by the square of height in meters. Target blood pressure of <140/90 mmHg (<140/85 mmHg in diabetics) and overweight (BMI >25 kg/m2) were applied according to recent European Guidelines on CVD prevention in clinical practice (version 2016) [17]. Antihypertensive pharmacotherapy included substances classified in ATC group C01 up to C10.
3. Data Analysis
We calculated median (quartiles) for continuous variables and proportions for categorical variables. In univariable analyses, Fisher's exact test or χ2- test for categorical and binary variables were used as appropriate. Due to right-skewed distribution of the BMQ-D specific-concerns scale, both specific subscales were dichotomized at the median score obtained per scale. As a sensitivity analysis, we also included the subscales as a continuous variable to the model. We performed multivariable logistic regression analysis to assess the association of specific-concerns and specific-necessity on inadequately controlled hypertension adjusted for sociodemographic status (age, sex, education), overweight (BMI >25 kg/m2), self-reported smoking status, and self-reported diabetes. Possible interactions between sex and beliefs regarding prescribed antihypertensive medication were assessed by adding terms of interaction to the regression model. In case of significant terms of interaction, univariable logistic regression (crude odds ratio [OR] with 95% confidence intervals [CI]) on inadequately controlled hypertension stratified for sex was performed and then adjusted for all covariables (adjusted OR). P-values <0.05 were considered statistically significant. Analyses were performed with IBM SPSS Statistics 23 (IBM® SPSS® Statistics Version 23).
4. Results
We applied the BMQ-D in a sex- and age-stratified subsample of 1295 participants in STAAB recruited via protocol-defined send-out waves (batches) 6 to 23. Of 759 participants receiving any kind of medication, 710 (93.5%) had complete information on both specific subscales. Of those, 634 were free of self-reported CVD, and 296 out of those received antihypertensive medication; 3 participants with missing values in blood pressure measurement or age older than 79 years were excluded. Therefore, 293 participants free of CVD taking antihypertensive drugs and with complete information on BMQ-D specific subscales entered the analyses (Figure 1).
Figure 1.
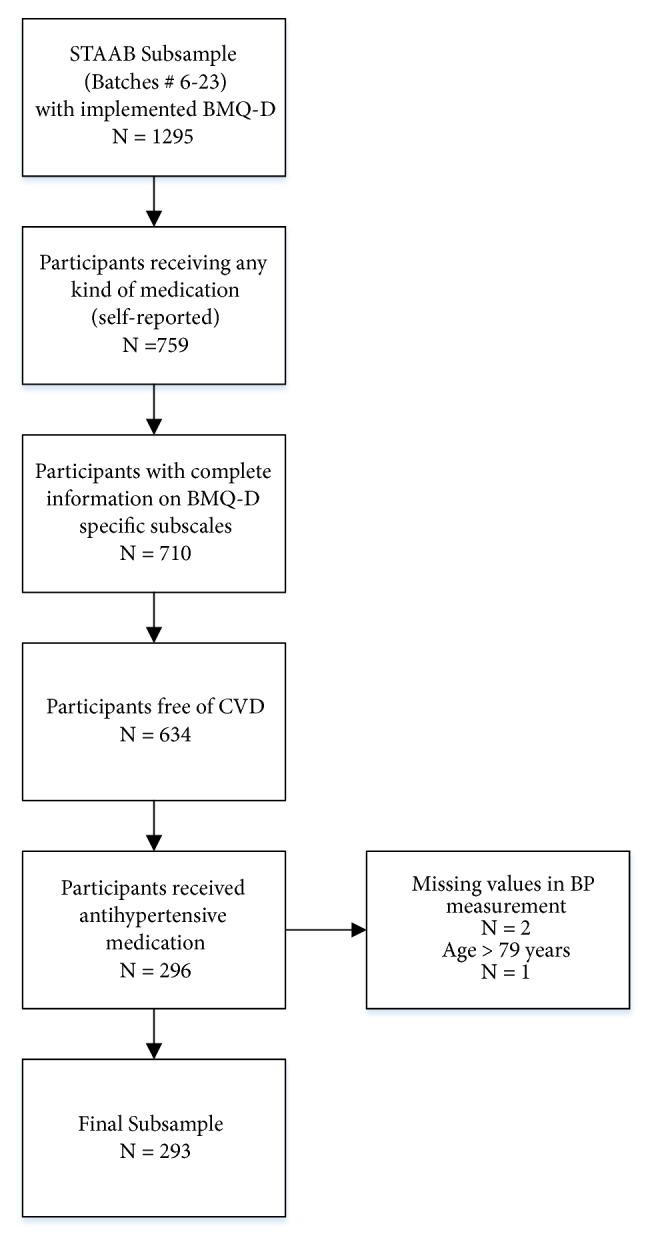
Sample Selection. BMQ-D, Beliefs about Medicines Questionnaire (German version); CVD, cardiovascular disease; BP, blood pressure.
The median age of the sample was 64 years (quartiles 55.0; 69.0), 49.5% were women (Table 1), and the median blood pressure was 137.5/88.0 mmHg (women: 134.5/79.6 mmHg; men: 139.8/82.8 mmHg). Despite antihypertensive medication, half of the participants (49.8%) revealed a blood pressure value above the recommended target with a preponderance of men (57.5% vs. 42.5%, respectively).
Table 1.
Characteristics of the study population stratified according to achieved or not achieved recommended blood pressure target.
| NTotal | Target achieved 1 | Target not achieved | P-value | |
|---|---|---|---|---|
| 293 | 147 (50.2) | 146 (49.8) | ||
| Gender | 0.02 | |||
| Female | 145 (49.5) | 83 (56.5) | 62 (42.5) | |
| Male | 148 (50.5) | 64 (43.5) | 84 (57.5) | |
| Age in years | 0.49 | |||
| 30-39 | 4 (1.4) | 3 (2.0) | 1 (0.7) | |
| 40-49 | 36 (12.3) | 18 (12.2) | 18 (12.3) | |
| 50-59 | 52 (17.7) | 25 (17.0) | 27 (18.5) | |
| 60-69 | 131 (44.7) | 71 (48.3) | 60 (41.1) | |
| 70-79 | 70 (23.9) | 30 (20.4) | 40 (27.4) | |
| Education | 0.26 | |||
| primary | 107 (36.5) | 59 (40.1) | 48 (32.9) | |
| secondary | 94 (32.1) | 48 (32.7) | 46 (31.5) | |
| tertiary | 92 (31.4) | 40 (27.2) | 52 (35.6) | |
| Current smoking | 35 (11.9) | 22 (15.0) | 13 (8.9) | 0.11 |
| Self-reported diabetes | 50 (17.1) | 25 (50.0) | 25 (50.0) | 0.98 |
| BMI > 25 kg/m2 | 237 (82.3) | 122 (84.1) | 115 (80.4) | 0.41 |
| BMQ, n (%), ≥ median | ||||
| Specific - Concerns | 164 (56.0) | 90 (61.2) | 74 (50.7) | 0.07 |
| Specific - Necessity | 151 (51.5) | 78 (53.1) | 73 (50.0) | 0.60 |
Legend: data are count (percent). Analyses are restricted to patients without missing values in respective variables.
BMI, body mass index; BMQ, Beliefs about Medicine Questionnaire.
1 Recommended target for treated hypertension: ≤ 140/90 mmHg and for diabetics: ≤ 140/85 mmHg.
Regarding the BMQ-D, the median score was 12.0 (9.0; 16.0) for specific-concerns and 17.0 (14.0; 20.5) for specific-necessity. More than 20% of women with normotensive blood pressure under medication reported concerns about dependency compared to 4.5% with blood pressure values above 140/90 mmHg. In the multivariable logistic regression analysis identifying factors associated with hypertension control, the interaction between specific-concerns and sex was statistically significant (p=0.02). Thus, further analyses were stratified for sex. In the adjusted multivariable regression model for women, inadequately controlled hypertension was less frequent in subjects expressing higher levels of concerns with regard to their prescribed antihypertensive medication (adjusted OR 0.36; 95%CI 0.17-0.74). Sensitivity analysis showed a similar effect for the continuous specific-concern subscale: adjusted OR per scale point 0.92; 95%CI 0.85-0.99. By contrast, in the univariable regression model for men, smoking was positively associated with better treatment control (crude OR 0.34; 95%CI 0.14-0.87). However, this effect disappeared after adjustment for other covariables: adjusted OR 0.43; 95%CI 0.16; 1.13. No statistically significant associations were found for specific-necessity in any model (Table 2).
Table 2.
Crude and adjusted ORs (95%-CI) for failure to reach blood pressure target in women and men.
| Variables | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|
| Crude OR (95%CI) |
P-value | Adjusted OR (95%CI) |
P-value | Crude OR (95%-CI) |
P-value | Adjusted OR (95%-CI) |
P-value | |
| Age in years, n (%) | 0.72 | 0.63 | 0.26 | 0.35 | ||||
| ≤ 49 | 1 | 1 | 1 | 1 | ||||
| 50-59 | 1.39 (0.40; 4.80) | 1.34 (0.34; 5.30) | 1.08 (0.35; 3.32) | 1.53 (0.45; 5.21) | ||||
| 60-69 | 0.82 (0.27; 2.46) | 0.74 (0.23; 2.43) | 1.13 (0.44; 2.90) | 1.39 (0.51; 3.76) | ||||
| 70-79 | 0.96 (0.29; 3.18) | 1.15 (0.31; 4.27) | 2.50 (0.84; 7.40) | 2.75 (0.87; 8.67) | ||||
|
| ||||||||
| Education | 0.53 | 0.65 | 0.43 | 0.24 | ||||
| Tertiary | 1 | 1 | 1 | 1 | ||||
| Secondary | 1.02 (0.44; 2.35) | 1.06 (0.43; 2.64) | 0.64 (0.27; 1.47) | 0.45 (0.17; 1.18) | ||||
| Primary | 0.68 (0.29; 1.60) | 0.72 (0.28; 1.90) | 0.64 (2.30; 1.37) | 0.57 (0.24; 1.36) | ||||
| Current smoking | 0.94 | 0.62 | 0.02 | 0.09 | ||||
| No | 1 | 1 | 1 | 1 | ||||
| Yes | 0.96 (0.29; 3.16) | 0.71 (0.18; 2.77) | 0.34 (0.14; 0.87) | 0.43 (0.16; 1.13) | ||||
| Self-reported diabetes | 0.22 | 0.27 | 0.27 | |||||
| No | 1 | 1 | 1 | 1 | ||||
| Yes | 1.74 (0.72; 4.19) | 1.72 (0.66; 4.51) | 0.60 (0.25; 1.40) | 0.56 (0.22; 1.43) | ||||
| Body Mass Index | 0.38 | 0.45 | 0.57 | 0.88 | ||||
| BMI ≤ 25 kg/m2 | 1 | 1 | 1 | 1 | ||||
| BMI > 25 kg/m2 | 0.70 (0.31; 1.57) | 0.72 (0.30; 1.71) | 0.76 (0.29; 1.96) | 1.09 (0.38; 3.11) | ||||
| BMQ-Concerns | < 0.01 | < 0.01 | 0.77 | 0.57 | ||||
| Concerns ≤ median | 1 | 1 | 1 | 1 | ||||
| Concerns > median | 0.37 (0.19; 0.73) | 0.36 (0.17; 0.74) | 1.11 (0.57; 2.13) | 1.23 (0.60; 2.56) | ||||
| BMQ-Necessity | 0.24 | 0.32 | 0.42 | 0.37 | ||||
| Necessity ≤ median | 1 | 1 | 1 | 1 | ||||
| Necessity > median | 0.67 (0.34; 1.30) | 0.68 (0.32; 1.45) | 1.31 (0.68; 2.52) | 1.38 (0.68; 2.82) | ||||
Data are odds ratios (OR) with 95% confidence intervals (CI). For adjustment procedure refers to Method.
5. Discussion
The current study observed insufficient blood pressure control in about half of the patients with a preponderance for men. This is in line with previous reports and [18] constitutes a major challenge for prevention of cardiovascular diseases.
The median BMQ scores for specific-concerns of 17.0 and specific-necessity of 12.0 were lower when compared to previous reports, which might be due to potentially healthier individuals with less comorbidity in our population-based sample [2, 3].
Potential sex-related differences in medication-related beliefs have been controversially discussed in previous studies [2, 19, 20]. Previous, qualitative studies showed that individuals, who do not perceive hypertension as a serious problem, have less controlled hypertension [21, 22]. In our study, we observed marked sex-related differences of such beliefs regarding inappropriate blood pressure control. Being less concerned about the prescribed antihypertensive medication was associated with worse blood pressure control in women, but not in men. In this context, considering that our finding was limited to women might indicate that adherence in female participants treated for hypertension is worse if their health perception is positive.
On the other hand, a study by Theunissen et al. showed that discussing cognitive or emotional illness representations (i.e., a process where patients are made aware of the significance of their health threat) or action plans regarding adherence to medical advice in a patient-provider-interaction led to more concerns about medication and increased patients' wish to follow lifestyle recommendations. This may additionally have strengthened their aversion to medication use [23]. Thus, illness representations may be both an indicator for better adherence and increased concerns. Therefore, well-informed patients knowing about the long-term consequences of uncontrolled hypertension might show better adherence to their medication regimes, despite higher concerns about medications.
In men, we did not find an association between specific scales of the BMQ-D and blood pressure targets. However, smoking was a factor associated with better treatment control in the unadjusted model, but the effect disappeared after adjustment for the other covariables, possibly due to the limited size of the sample. One study reported that more men than women believed in the serious longer-term consequences of hypertension [2]. Because of their higher CVD risk, male smoking participants with their additional cardiovascular risk factor of hypertension might be more aware of their blood pressure. Therefore, they might at least have their blood pressure treated appropriately if they cannot stop smoking.
No significant association was found for blood pressure control and the BMQ-D specific-necessity subscale. A systematic review by Horne and colleagues reported also no statistically significant association regarding necessity and adherence to antihypertensive medication [7]. There may be a link between the necessity of taking prescribed medication and the presence or absence of symptoms. When suffering from a predominantly asymptomatic condition such as hypertension, the benefits may be imperceptible to the participants [2, 9, 24]. Therefore, it is challenging for physicians to advise patients with hypertension to take their medication as prescribed because they tend to underestimate the long-term benefits of adherence to medication [2, 3, 12, 25]. Furthermore, in a condition that is mainly asymptomatic, medication-related side effects may more readily be perceived as unacceptable [2].
Recent studies have shown that educational interventions in hypertensive patients are able to influence the awareness of hypertension as a modifiable condition and the knowledge about prescribed therapy leading into a significant reduction in blood pressure values [26, 27]. The role of educational interventions on medication-related beliefs taking into account sex-related differences needs to be further investigated.
6. Limitations
There are limitations of our study. We report data from selected participants diagnosed with hypertension from an age- and sex-stratified population-based study with potentially limited generalizability to other populations and disease groups. Furthermore, our study may include healthier subjects with a higher proportion of asymptomatic blood pressure and less severe forms of hypertension due to the voluntary participation. Thus, medication-related beliefs might be underestimated. In addition, single-occasion measurements for hypertension may lead to false positive associations despite standardized measurements. Furthermore, we had no information about the number and dose of antihypertensive medication taken per day as well as the intensity of physicians' supervision, adherence to medication, and counselling that might influence medication-related beliefs. Last, the multivariable model only accounted for measured factors leaving room for residual confounding.
7. Conclusion
In contrast to previous studies examining medication-related beliefs towards adherence as a primary outcome, we assessed the association of medication-related beliefs with a clinical outcome, i.e., blood pressure control in a population-based sample. In our study, lower concerns about prescribed medication were associated with worse blood pressure control in women, but not in men. Our findings highlight the importance that medication-related beliefs constitute a serious barrier of successful implementation of treatment guidelines and underline the role of educational interventions taking into account sex-related differences. The unexpected finding of an inverse association regarding concerns about medication and blood pressure control needs to be replicated and further investigated in different populations with clinical outcomes.
Acknowledgments
On behalf of the STAAB consortium, S. Frantz (Dept. of Medicine I, Div. of Cardiology, University Hospital Würzburg); C. Maack (Comprehensive Heart Failure Center, University Hospital and University of Würzburg); G. Ertl (University Hospital Würzburg); M. Faßnacht (Dept. of Medicine I, Div. of Endocrinology, University Hospital Würzburg); C. Wanner (Dept. of Medicine I, Div. of Nephrology, University Hospital Würzburg); R. Leyh (Dept. of Cardiovascular Surgery, University Hospital Würzburg); J. Volkmann (Dept. of Neurology, University Hospital Würzburg); J. Deckert (Dept. of Psychiatry, Psychosomatics and Psychotherapy, Center of Mental Health, University Hospital Würzburg); H. Faller (Dept. of Medical Psychology, University of Würzburg); R. Jahns (Interdisciplinary Bank of Biomaterials and Data Würzburg, University Hospital Würzburg), we greatly appreciate the time of all STAAB participants and their willingness to provide data to the study. We also thank the Mayor of the City of Würzburg and the local registration office for their kind and sustained support of our study. Further, we thank the Department of Clinical Psychology and Psychotherapy, Philipps-University of Marburg, for the German translated of the German version of BMQ and Yvonne Nestoriuc from the University of Hamburg for her support. Finally, we thank the entire study team including F. Eichner, V. Ceijka, R. Mattern, C. Morbach, M. Breunig, study nurses, technicians, data managers, and students for their efforts on the STAAB study. We also thank Rudy Meijer from Meijer Medical Ultrasound, Vorschooten, The Netherlands, for external training and certification in vessel ultrasound as well as M. Ertl, G. Fette, and F. Puppe from the CHFC DataWarehouse, Institute of Informatics VI, University of Würzburg. The study is supported by the German Ministry of Research and Education within the Comprehensive Heart Failure Centre Würzburg (BMBF 01EO1004 and 01EO1504). This publication was funded by the German Research Foundation (DFG) and the University of Würzburg in the funding programme Open Access Publishing.
Data Availability
All data necessary for interpreting the study results and supporting its conclusions are included in the present publication. The authors have full control of all primary data. Individual patient data are available upon request from STAAB principal investigators in accordance with local data security restrictions and ethics recommendations.
Ethical Approval
The STAAB cohort study was approved by the Ethics Committee of the Medical Faculty (vote 98/13) and the data protection officer of the University of Würzburg (J-117.605-09/13). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent
Informed consent was obtained from all individual participants included in the study.
Disclosure
The content of this publication is within responsibility of the author.
Conflicts of Interest
Stefan Störk reports research grants from the German Ministry of Education and Research, European Union, University Hospital Würzburg, principal investigator in trials (cosponsored by BOEHRINGER, NOVARTIS, BAYER; speaker honoraria by BOEHRINGER, SERVIER, NOVARTIS, ASTRA-ZENECA, PFIZER, BAYER). Peter U. Heuschmann reports research grants from the German Ministry of Research and Education, German Research Foundation, European Union, Federal Joint Committee (G-BA) within the Innovationfond, Charité, Berlin Chamber of Physicians, German Parkinson Society, University Hospital Würzburg, Robert-Koch-Institute, German Heart Foundation, Charité–Universitätsmedizin Berlin (within MonDAFIS; MonDAFIS is supported by an unrestricted research grant to the Charité from Bayer), University Göttingen (within FIND-AF-randomized; FIND-AF randomized is supported by an unrestricted research grant to the University Göttingen from Boehringer-Ingelheim), and University Hospital Heidelberg (within RASUNOA-prime; RASUNOA-prime is supported by an unrestricted research grant to the University Hospital Heidelberg from Bayer, BMS, Boehringer-Ingelheim, Daiichi Sankyo), outside submitted work. Caroline Morbach reports a speakers honorarium from Amgen, a travel grant from Thermo Fisher, Orion Pharma, and Alnylam, and participation in Scientific Advisory and Patient Eligibility Boards sponsored by AKCEA, Alnylam, and EBR Systems outside the submitted work. Theresa Tiffe, Götz Gelbrich, Hermann Faller, Viktoria Rücker, and Martin Wagner declare that they have no conflicts of interest.
Authors' Contributions
Stefan Störk and Peter U. Heuschmann contributed equally.
References
- 1.Diederichs C., Neuhauser H. The incidence of hypertension and its risk factors in the German adult population: results from the German National Health Interview and Examination Survey 1998 and the German Health Interview and Examination Survey for Adults 2008-2011. Journal of Hypertension. 2017;35(2):250–258. doi: 10.1097/HJH.0000000000001151. [DOI] [PubMed] [Google Scholar]
- 2.Ross S., Walker A., MacLeod M. J. Patient compliance in hypertension: Role of illness perceptions and treatment beliefs. Journal of Human Hypertension. 2004;18(9):607–613. doi: 10.1038/sj.jhh.1001721. [DOI] [PubMed] [Google Scholar]
- 3.Shiri C. The role of insight into and beliefs about medicines of hypertensive patients. Cardiovascular Journal of Africa. 2007;18(6):353–357. [PMC free article] [PubMed] [Google Scholar]
- 4.Phatak H. M., Thomas J. Relationships Between Beliefs about Medications and Nonadherence to Prescribed Chronic Medications. Annals of Pharmacotherapy. 2016;40(10):1737–1742. doi: 10.1345/aph.1H153. [DOI] [PubMed] [Google Scholar]
- 5.Horne R. Patients' beliefs about treatment: the hidden determinant of treatment outcome? Journal of Psychosomatic Research. 1999;47(6):491–495. doi: 10.1016/s0022-3999(99)00058-6. [DOI] [PubMed] [Google Scholar]
- 6.Gagnon M. D., Waltermaurer E., Martin A., Friedenson C., Gayle E., Hauser D. L. Patient Beliefs Have a Greater Impact Than Barriers on Medication Adherence in a Community Health Center. The Journal of the American Board of Family Medicine. 2017;30(3):331–336. doi: 10.3122/jabfm.2017.03.160129. [DOI] [PubMed] [Google Scholar]
- 7.Horne R., Chapman S. C. E., Parham R., Freemantle N., Forbes A., Cooper V. Understanding patients' adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the Necessity-Concerns Framework. PLoS ONE. 2013;8(12) doi: 10.1371/journal.pone.0080633.e80633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wagner M., Tiffe T., Morbach C., Gelbrich G., Störk S., Heuschmann P. U. Characteristics and Course of Heart Failure Stages A–B and Determinants of Progression – design and rationale of the STAAB cohort study. European Journal of Preventive Cardiology. 2017;24(5):468–479. doi: 10.1177/2047487316680693. [DOI] [PubMed] [Google Scholar]
- 9.Horne R., Weinman J. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. Journal of Psychosomatic Research. 1999;47(6):555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 10.Horne R., Weinman J., Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychology & Health. 1999;14(1):1–24. doi: 10.1080/08870449908407311. [DOI] [Google Scholar]
- 11.Figueiras M., et al. Patients' illness schemata of hypertension: The role of beliefs for the choice of treatment. Psychology & Health. 2010;25(4):507–517. doi: 10.1080/08870440802578961. [DOI] [PubMed] [Google Scholar]
- 12.Horne R., Clatworthy J., Hankins M. High adherence and concordance within a clinical trial of antihypertensives. Chronic Illness. 2010;6(4):243–251. doi: 10.1177/1742395310369018. [DOI] [PubMed] [Google Scholar]
- 13.Leng B., Jin Y., Li G., Chen L., Jin N. Socioeconomic status and hypertension: a meta-analysis. Journal of Hypertension. 2015;33(2):221–229. doi: 10.1097/HJH.0000000000000428. [DOI] [PubMed] [Google Scholar]
- 14.Di Giosia P., Giorgini P., Stamerra C. A., Petrarca M., Ferri C., Sahebkar A. Gender Differences in Epidemiology, Pathophysiology, and Treatment of Hypertension. Current Atherosclerosis Reports. 2018;20(3) doi: 10.1007/s11883-018-0716-z. [DOI] [PubMed] [Google Scholar]
- 15.Mancia G., Fagard R., Narkiewicz K. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) European Heart Journal. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 16.Hubert H. B., Feinleib M., McNamara P. M., Castelli W. P. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67(5):968–977. doi: 10.1161/01.cir.67.5.968. [DOI] [PubMed] [Google Scholar]
- 17.Piepoli M. F., et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts): Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) European Journal of Preventive Cardiology. 2016 doi: 10.1177/2047487316653709. [DOI] [PubMed] [Google Scholar]
- 18.Diederichs C., Neuhauser H. Regional variations in hypertension prevalence and management in Germany. Journal of Hypertension. 2014;32(7):1405–1414. doi: 10.1097/HJH.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 19.Isacson D., Bingefors K. Attitudes towards drugs--a survey in the general population. Pharmacy World and Science. 2002;24(3):104–110. doi: 10.1023/A:1016127320051. [DOI] [PubMed] [Google Scholar]
- 20.Viktil K. K., Frøyland H., Rogvin M., Moger T. A. Beliefs about medicines among Norwegian outpatients with chronic cardiovascular disease. European Journal of Hospital Pharmacy: Science and Practice. 2014;21(2):118–120. doi: 10.1136/ejhpharm-2013-000346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rahmawati R., Bajorek B. Understanding untreated hypertension from patients’ point of view: A qualitative study in rural Yogyakarta province, Indonesia. Chronic Illness. 2017;14(3):228–240. doi: 10.1177/1742395317718034. [DOI] [PubMed] [Google Scholar]
- 22.Bokhour B. G., et al. The role of patients' explanatory models and daily-lived experience in hypertension self-management. Journal of General Internal Medicine. 2012;12(27):1626–1634. doi: 10.1007/s11606-012-2141-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Theunissen N. C., de Ridder D. T., Bensing J. M., Rutten G. E. Manipulation of patient–provider interaction: discussing illness representations or action plans concerning adherence. Patient Education and Counseling. 2003;51(3):247–258. doi: 10.1016/S0738-3991(02)00224-0. [DOI] [PubMed] [Google Scholar]
- 24.Meyer D., Leventhal H., Gutmann M. Common-sense models of illness: the example of hypertension. Journal of Health Psychology. 1985;4(2):115–135. doi: 10.1037//0278-6133.4.2.115. [DOI] [PubMed] [Google Scholar]
- 25.Wilhelm M., Rief W., Doering B. K. It’s all a matter of necessity and concern: A structural equation model of adherence to antihypertensive medication. Patient Education and Counseling. 2018;101(3):497–503. doi: 10.1016/j.pec.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 26.Scala D., Menditto E., Caruso G., et al. Are you more concerned about or relieved by medicines? An explorative randomized study of the impact of telephone counseling by pharmacists on patients’ beliefs regarding medicines and blood pressure control. Patient Education and Counseling. 2018;101(4):679–686. doi: 10.1016/j.pec.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 27.Santschi V., Chiolero A., Colosimo A. L., et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. Journal of the American Heart Association. 2014;3(2):p. e000718. doi: 10.1161/JAHA.113.000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data necessary for interpreting the study results and supporting its conclusions are included in the present publication. The authors have full control of all primary data. Individual patient data are available upon request from STAAB principal investigators in accordance with local data security restrictions and ethics recommendations.


