Abstract
Background
Management of mechanical ventilation (MV) is an important and complex aspect of caring for critically ill patients. Management strategies and technical operation of the ventilator are key skills for physicians in training, as lack of expertise can lead to substantial patient harm.
Objective
We performed a narrative review of the literature describing MV education in graduate medical education (GME) and identified best practices for training and assessment methods.
Methods
We searched MEDLINE, PubMed, and Google Scholar for English-language, peer-reviewed articles describing MV education and assessment. We included articles from 2000 through July 2018 pertaining to MV education or training in GME.
Results
Fifteen articles met inclusion criteria. Studies related to MV training in anesthesiology, emergency medicine, general surgery, and internal medicine residency programs, as well as subspecialty training in critical care medicine, pediatric critical care medicine, and pulmonary and critical care medicine. Nearly half of trainees assessed were dissatisfied with their MV education. Six studies evaluated educational interventions, all employing simulation as an educational strategy, although there was considerable heterogeneity in content. Most outcomes were assessed with multiple-choice knowledge testing; only 2 studies evaluated the care of actual patients after an educational intervention.
Conclusions
There is a paucity of information describing MV education in GME. The available literature demonstrates that trainees are generally dissatisfied with MV training. Best practices include establishing MV-specific learning objectives and incorporating simulation. Next research steps include developing competency standards and validity evidence for assessment tools that can be utilized across MV educational curricula.
Introduction
Mechanical ventilation (MV) is a life-saving intervention in respiratory failure; however, it is complex and requires critical thinking. When managed inappropriately it carries a risk of major harm. Education related to appropriate MV management is imperative for all physicians in training who are caring for critically ill patients, including those in the areas of anesthesiology, emergency medicine, general surgery, internal medicine, critical care medicine, pediatric critical care medicine, and pulmonary and critical care medicine.1–6
Even among practicing intensivists, who are expected to be experts, there is evidence of insufficient knowledge of MV.7–11 Intensivists perform poorly in interpreting ventilator waveforms for patient-ventilator dyssynchrony7 and are poorly adherent to low tidal volume ventilation strategies for adult and pediatric patients with acute respiratory distress syndrome (ARDS) despite evidence of clear benefit.8–11
Commonly, MV is managed by physicians without subspecialized training in critical care, and there is evidence of insufficient MV education for this group.12 A recent survey revealed that only 56% of reporting hospital critical care units had intensivists present during daytime hours or available for urgent consultation.13 Furthermore, 77% of surveyed hospitalists reported providing critical care services and 66% reported serving as primary physicians in the intensive care unit (ICU).12 When hospitalists were primarily managing ICU patients, intensivists were responsible for all ventilator management in less than half of cases. In addition, 35% of nonacademic hospitalists and 24% of academic hospitalists reported being expected to practice beyond their scope of residency training, and 85% of hospitalists managing critically ill patients expressed a need for further training in MV.12 Patient outcomes are also negatively affected, as MV is specifically associated with a longer length of stay in ICUs managed by nonintensivists.14 These findings are particularly concerning given the expected upcoming intensivist shortage.15 In the emergency department, less than half of patients with identified ARDS received low tidal volume ventilation.16 For patients not meeting ARDS criteria initially, there is an association with inappropriate initial ventilator settings and the subsequent development of ARDS.17 Graduating from an emergency medicine training program that emphasizes MV education, however, correlates with better test scores on objective assessment of MV knowledge, including knowledge of low tidal volume ventilation.18
Our aim was to review the literature to determine best practices related to MV education regarding curricular content and formats as well as learner assessment. In this narrative review, we describe the available literature regarding MV training across graduate medical education (GME) specialties, identify areas where further research is needed, and formulate a strategy for improving the educational environment.
Methods
We conducted a narrative review of the available evidence for GME training in MV. Our authorship group was formed through the American Thoracic Society Section on Medical Education as an interest group focused on MV education. The group has diverse experience and includes pulmonary and critical medicine fellows in training, fellowship program directors, and division chiefs. We represent 8 institutions with broad geographic variability, including an international representative. When comparing our own institutional experiences, there was considerable variability in curricula, methods of instruction, and assessments being performed.
Two authors (J.M.K. and N.S.) searched MEDLINE, PubMed, and Google Scholar from the year 2000 through July 2018 using the following key words: mechanical ventilation education, mechanical ventilation training, graduate medical education, housestaff, resident, and fellow. No additional publications were identified after reviewing the references from identified articles. Studies were included if they were published in English-language, peer-reviewed journals and the abstracts described instruction, assessment, or opinions pertaining to MV in GME. Articles were excluded if they focused on non-GME learning groups or if no description of educational intervention or assessment was included. The full text of each article was reviewed by the coauthors to confirm inclusion.
The articles reviewed had considerable variability and heterogeneity in populations, methods, and analyses. The results were not amenable to traditional meta-analysis.19 We synthesized the available literature using a narrative review approach involving critical evaluation of individual articles and their results.20,21 We then identified the key points of the literature and generated consensus themes by discussion. After a preliminary review of included articles, the authors used a consensus approach to categorize studies: surveys of residents, fellows, or program directors regarding self-perceived MV skills and needs; articles describing objective assessments of MV education; articles defining ideal learning objectives for MV education; and studies implementing educational interventions to improve MV education.
Results
The literature search yielded 76 articles, of which 15 met the inclusion criteria. The excluded articles lacked educational interventions or assessments or did not pertain to the GME population. The search results are summarized in the Table.
Table.
Summary of Studies in Mechanical Ventilation Training During Graduate Medical Education
| Category | Article | Learners | Description |
| Surveys of trainees and program directors regarding adequacy of MV training | Cox et al,22 2003 | Senior IM residents |
|
| Brescia et al,23 2008 | PCCM and CCM fellows |
|
|
| Tallo et al,24 2017 | IM residents in Brazil |
|
|
| Wilcox et al,25 2015 | EM residents |
|
|
| Objective assessment of the current state of MV education | Cox et al,22 2003 | Senior IM residents |
|
| Tallo et al,24 2017 | IM residents |
|
|
| Development of assessment tools in MV education | Richards et al,26 2016 | EM residents |
|
| O'Boyle et al,27 2014 | Pediatric CCM fellows |
|
|
| Define learning objectives for MV education | Goligher et al,28 2012 | IM and anesthesia residents |
|
| Dorman et al,29 2004 | Residents and fellows |
|
|
| O'Boyle et al,27 2014 | Pediatric CCM fellows |
|
|
| Educational intervention | Schroedl et al,30 2012 | IM residents (n = 60) |
|
| Singer et al,31 2013 | IM residents (n = 40) |
|
|
| Yee et al,32 2016 | EM and surgery residents (n = 17) |
|
|
| Educational intervention | Spadaro et al,33 2017 | Anesthesia residents (n = 50) |
|
| Mireles-Cabodevila et al,34 2015 | PCCM or CCM fellows (n = 36) |
|
|
| Ramar et al,35 2016 | PCCM or CCM fellows (n = 13) |
|
Abbreviations: MV, mechanical ventilation; IM, internal medicine; PCCM, pulmonary and critical care medicine; CCM, critical care medicine; EM, emergency medicine; ARDS, acute respiratory distress syndrome; PEEP, positive end-expiratory pressure; ICU, intensive care unit.
P < .05 for all comparisons.
Target Audience
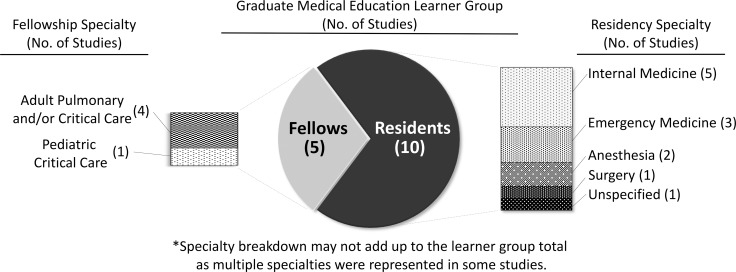
The included publications represented resident and fellow learners, with specialty representation from anesthesiology, emergency medicine, general surgery, and internal medicine, as well as subspecialty training in critical care medicine, pediatric critical care medicine, and pulmonary and critical care medicine.
The majority of the MV educational data pertains to residents (Figure 1). One study was not specialty-specific. No studies pertained to pediatrics or family medicine residents and MV education.
Figure 1.
Target Learner Groups From Studies of Mechanical Ventilation Training
Surveys Regarding Adequacy of MV Training
Four articles reported survey responses regarding experience with MV education from physician trainees and program directors.22–25 Surveys asked about satisfaction or comfort level with the current training environment. Two studies reported good response rates of 70% or higher,22,25 1 had a poor response rate of 23%,23 and 1 did not provide response rate information.24 No studies included validity evidence for survey development.
The largest study, published in 2003, surveyed 259 graduating internal medicine residents, and found that nearly half were dissatisfied with their training in MV and perceived their knowledge to be close to minimum standards.22 The disparity between resident and program director perceptions was noteworthy: 70% of internal medicine program directors indicated that they were satisfied with their program's MV instruction. Findings for pulmonary and critical care medicine and critical care medicine fellows were similar: 50% reported satisfaction with their education in MV in the 2008 study evaluating fellow satisfaction, though the response rate was very low.23
In a 2017 study of internal medicine residents in Brazil, nearly 30% of third-year residents said they would fear for patient safety if their patients required MV, and only 52% thought they would be able to safely manage a ventilated patient with significant airflow obstruction.24 In a 2015 study, only 53% of emergency medicine residents reported feeling comfortable caring for mechanically ventilated patients despite having frequent contact with ventilated patients.25 In the study, 77% of residents reported having 3 hours or less of MV education in the past year. We found no data pertaining to satisfaction with MV education or comfort with MV management in anesthesia, surgical, or pediatric GME programs.
Objective Assessment of MV Education
Two studies evaluated current trainee knowledge in MV.22,24 The largest and most rigorous was the 2003 survey study of internal medicine residents.22 Knowledge of respiratory physiology and MV management was evaluated among 259 graduating internal medicine residents using 19 case-based multiple-choice questions. Response rate was satisfactory at 74%. Residents scored above 70% on questions related to the topics of noninvasive ventilation, measurement of auto-positive end-expiratory pressure (auto-PEEP), and diagnosing tension pneumothorax. The lowest scores were seen with management of ARDS, hypoxemia, and ventilator weaning, which are fundamental tenets of MV management. Only 52% of respondents applied the correct tidal volume in the case study of a patient with ARDS. In the 2017 study of Brazilian internal medicine residents, there was overall poor performance on knowledge testing.24 For example, 59% of residents inappropriately indicated that they would start MV based on a patient's actual weight rather than predicted body weight. This study was of low quality, however, and lacked a reported response rate, validity assessment, or further details of the assessment tool.
Development of Assessment Tools in MV Education
Two studies described the development and performance characteristics of knowledge assessment tools in MV education.26,27 A 2016 study involved a 9-question multiple-choice assessment for emergency medicine residents.26 The questions were developed by expert consensus, pretested and piloted, then given to residents with a reasonable 69% response rate. The study reported adequate internal reliability and an appropriate mix of item difficulty, suggesting that this assessment tool was sufficiently rigorous for evaluating emergency medicine residents. A study from 2014 evaluated a 35-item knowledge assessment tool of MV knowledge in pediatric critical care medicine fellows that had robust content validity, construct validity, internal consistency, and reliability metrics.27 Experts performed best on the assessment tool, with a mean score of 75%, compared with 59% and 35% in the advanced and novice groups, respectively. The authors described this as the first example of a knowledge assessment tool in MV with validity evidence and suggested that it can be utilized to assess competency and identify knowledge gaps in MV training for pediatric critical care medicine fellows.
Learning Objectives
Learning objectives are important to establish for complex learning tasks, including MV training. Reported discontent with MV education was, in fact, noted to be highest among training programs that lacked learning objectives specific to MV.22 Three studies sought to define learning objectives for MV education.27–29 In the largest study, from 2012, a panel of 14 content experts, educators, and trainees from internal medicine and anesthesia specialties generated learning objectives with high agreement through a Delphi consensus process.28 Though the report included objectives pertaining to respiratory physiology, modes of ventilation, use of noninvasive ventilation, monitoring, complications of MV, and appropriate removal of MV, it did not describe any formal assessment using the defined learning objectives. In 2004, an expert panel associated with the American College of Critical Care Medicine identified both the management of invasive devices and the understanding of sedation and analgesia principles as core clinical topics with which all residents should demonstrate knowledge and technical skills. More advanced ventilation techniques, including use of multiple ventilator types, were identified as fellow-level objectives.29 No information was provided, however, as to the process of developing the objectives. The 2014 study of MV education in pediatric critical care medicine sought to identify learning objectives for management of pediatric MV in addition to the published assessment tool.27 The 10 objectives developed by consensus of the authors addressed knowledge of ventilation modes and their impact on physiological parameters.
Educational Interventions
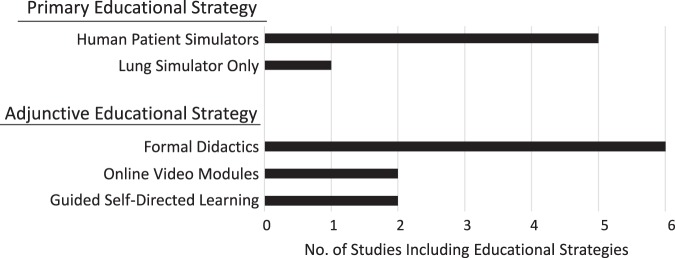
Six studies, published between 2012 and 2017, evaluated educational interventions related to MV (Figure 2).30–35 All studies incorporated hands-on simulation training, and all assessments were limited to pretesting and immediate postintervention testing. No studies assessed skill or knowledge retention beyond 1 month. All studies included outcomes related to change in learning or knowledge, in addition to self-reported satisfaction or reaction of participants.36 Four studies included assessment of MV management skills using a performance checklist,30–33 and 2 studies included only evaluation of trainee knowledge through multiple-choice questions.34,35 Two studies uniquely showed change in trainee performance scores during evaluation with actual patients after simulation-based educational interventions.30,31 These 2 studies also most extensively described the validity evidence for the assessment tools. Overall satisfaction was highest for simulation-based interventions compared with other methodologies across studies. No studies evaluated patient-level outcomes, such as ventilator free days, ICU length of stay, or mortality.
Figure 2.
Educational Strategies Employed in Published Studies of Mechanical Ventilation Training
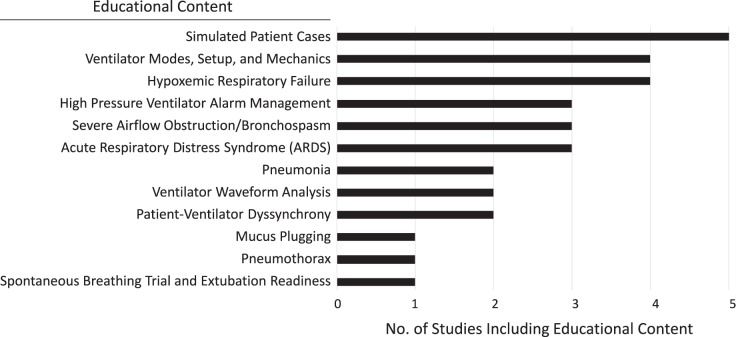
Educational content varied considerably across studies, including such topics as respiratory physiology, ventilator setup and waveform analysis, case-based management of ARDS, bronchospasm, patient-ventilator dyssynchrony, chronic obstructive pulmonary disease, and severe hypoxemia (Figure 3).
Figure 3.
Educational Content Delivered in Published Studies of Mechanical Ventilation Training
Across all studies, the average time spent on an educational intervention for MV was 7 ± 3 hours, and the average number of learners was 37 ± 17 (Figure 4).
Figure 4.
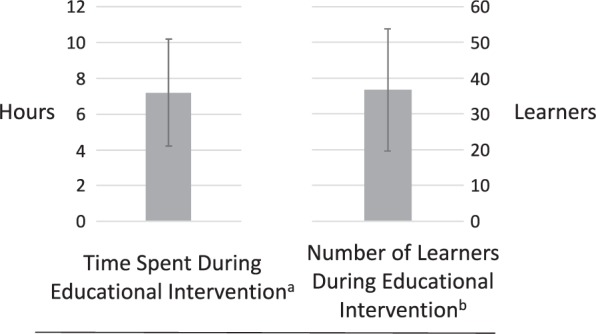
Educational Interventions in Published Studies of Mechanical Ventilation Training
a The average time spent was 7 ± 3 hours.
b The average number of learners was 37 ± 17.
Discussion
Our narrative review of the literature demonstrated substantial heterogeneity within MV education. Learners in GME are generally dissatisfied with their training in MV22–25 and perform suboptimally on objective testing of MV management knowledge.22,24 There are indications that the lack of educational rigor translates to the clinical environment, with practicing physicians demonstrating variable adoption of best practices and evidence-based interventions and inadequately recognizing important complications of MV, including ventilator-induced lung injury, delayed MV liberation, and patient-ventilator dyssynchrony.7–11,14,16,17,36
While most organizations governing the education of trainees involved in the management of critically ill patients recognized that ventilator management is an educational priority,2,4–6 surprisingly little is known regarding the ideal methods for instruction and assessment. Few studies have attempted to rigorously define learning objectives for MV education and develop validity evidence for evaluation tools to assess training, typically formulated through expert consensus.26–28 Studies evaluating educational interventions in MV are generally low quality with poor evaluation of validity evidence, and only 2 studies have assessed postintervention trainee performance in caring for actual patients.30,31
Several best practices emerge from analysis of the available literature base. Every GME program where critically ill patients are managed should establish or adopt MV-specific learning objectives and incorporate simulation into training curricula. Simulation interventions, especially with case-based scenarios, generally improved MV knowledge and technical skills beyond other instructional methods and were highly rated by participants. The curriculum should also incorporate interprofessional collaboration with those directly involved in day-to-day management of MV, such as nurses or respiratory therapists. Once the curriculum is in place, there should be a framework to assess the curriculum over time and allow for retraining when new ventilators or technology are introduced.
Limitations of the review include a low number of studies pertaining to MV education and difficulty aggregating the available data given inconsistency in educational methods and assessments. In addition, most studies lacked validity evidence for assessments, and only 2 studies assessed outcomes at the patient level.
Future studies of MV education should focus on patient-level outcomes as much as possible, rather than improvement in satisfaction or knowledge scores alone. Given that these studies are logistically difficult, starting with simulated patient models is reasonable. Published MV curricula use a variety of methods and content, which is expected across multiple levels of trainee expertise, though minimum performance standards need to be established. While statistically significant improvements in postintervention performance scores are a start, we need to first define minimum performance scores and then assess whether residents and fellows are achieving them. High-quality, rigorously tested assessment tools are needed, coupled with specialty-specific competencies.
Conclusion
Proficiency in MV management is an educational priority for physician trainees involved in critical care, yet they are generally dissatisfied with MV education and feel ill-prepared for ventilator management in clinical practice. Programs should have MV-specific learning objectives and incorporate simulation into MV training, although more work is needed to define specialty-specific competencies and develop assessment tools.
References
- 1.Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Emergency Medicine. 2017 https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/110_emergency_medicine_2017-07-01.pdf?ver=2017-05-25-084936-193 Accessed May 22, 2019.
- 2.Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Pediatric Critical Care Medicine. 2013 https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/323_pediatric_critical_care_medicine_2017-07-01.pdf?ver=2017-06-30-083428-177 Accessed May 22, 2019.
- 3.Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Anesthesiology Critical Care Medicine. 2017 https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/045_critical_care_anes_2017-07-01.pdf?ver=2017-05-17-155711-140 Accessed May 22, 2019.
- 4.Accreditation Council for Graduate Medical Education. The Anesthesiology Milestone Project. 2015 http://www.acgme.org/Portals/0/PDFs/Milestones/AnesthesiologyMilestones.pdf Accessed May 22, 2019.
- 5.Accreditation Council for Graduate Medical Education. Case Minimum Requirements: Surgical Critical Care Effective Beginning Academic Year 2019–2020. 2017 http://www.acgme.org/Portals/0/Defined_Category_Minimum_Numbers_Surgical_Critical_Care.pdf Accessed May 22, 2019.
- 6.Fessler HE, Addrizzo-Harris D, Beck JM, Buckley JD, Pastores SM, Piquette CA, et al. Entrustable professional activities and curricular milestones for fellowship training in pulmonary and critical care medicine: report of a multisociety working group. Chest. 2014;146(3):813–834. doi: 10.1378/chest.14-0710. [DOI] [PubMed] [Google Scholar]
- 7.Colombo D, Cammarota G, Alemani M, Carenzo L, Barra FL, Vaschetto R, et al. Efficacy of ventilator waveforms observation in detecting patient–ventilator asynchrony. Crit Care Med. 2011;39(11):2452–2457. doi: 10.1097/CCM.0b013e318225753c. [DOI] [PubMed] [Google Scholar]
- 8.Weiss CH, Baker DW, Weiner S, Bechel M, Ragland M, Rademaker A, et al. Low tidal volume ventilation use in acute respiratory distress syndrome. Crit Care Med. 2016;44(8):1515–1522. doi: 10.1097/CCM.0000000000001710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ward SL, Quinn CM, Valentine SL, Sapru A, Curley MA, Willson DF, et al. Poor adherence to lung-protective mechanical ventilation in pediatric acute respiratory distress syndrome. Pediatr Crit Care Med. 2016;17(10):917–923. doi: 10.1097/PCC.0000000000000903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spece LJ, Mitchell KH, Caldwell ES, Gundel SJ, Jolley SE, Hough CL. Low tidal volume ventilation use remains low in patients with acute respiratory distress syndrome at a single center. J Crit Care. 2018;44:72–76. doi: 10.1016/j.jcrc.2017.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 12.Sweigart JR, Aymond D, Burger A, Kelly A, Marzano N, McIlraith T, et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2017;13(1):6–12. doi: 10.12788/jhm.2886. [DOI] [PubMed] [Google Scholar]
- 13.The Leapfrog Group. Factsheet: ICU Physician Staffing Challenges to IPS Implementation. 2018 www.leapfroggroup.org/survey Accessed May 22, 2019.
- 14.Wise KR, Akopov VA, Williams BR, Jr, Ido MS, Leeper KV, Jr, Dressler DD, et al. Hospitalists and intensivists in the medical ICU: a prospective observational study comparing mortality and length of stay between two staffing models. J Hosp Med. 2012;7(3):183–189. doi: 10.1002/jhm.972. [DOI] [PubMed] [Google Scholar]
- 15.Halpern NA, Pastores SM, Oropello JM, Kvetan V. Critical care medicine in the United States: addressing the invensivist shortage and image of the specialty. Crit Care Med. 2013;41(12):2754–2761. doi: 10.1097/CCM.0b013e318298a6fb. [DOI] [PubMed] [Google Scholar]
- 16.Fuller BM, Mohr NM, Miller CN, Deitchman AR, Levine BJ, Castagno N, et al. Mechanical ventilation and ARDS in the ED: a multicenter, observational, prospective, cross-sectional study. Chest. 2015;148(2):365–374. doi: 10.1378/chest.14-2476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gajic O, Frutos-Vivar F, Esteban A, Hubmayr RD, Anzueto A. Ventilator settings as a risk factor for acute respiratory distress syndrome in mechanically ventilated patients. Intensive Care Med. 2005;31(7):922–926. doi: 10.1007/s00134-005-2625-1. [DOI] [PubMed] [Google Scholar]
- 18.Wilcox SR, Strout TD, Schneider JI, Mitchell PM, Smith J, Lutfy-Clayton L, et al. Academic emergency medicine physicians' knowledge of mechanical ventilation. West J Emerg Med. 2016;17(3):271–279. doi: 10.5811/westjem.2016.2.29517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cook DA, West CP. Conducting systematic reviews in medical education: a stepwise approach. Med Educ. 2012;46(10):943–952. doi: 10.1111/j.1365-2923.2012.04328.x. [DOI] [PubMed] [Google Scholar]
- 20.Colliver JA, Kucera K, Verhulst SJ. Meta-analysis of quasi-experimental research: are systematic narrative reviews indicated? Med Educ. 2008;42(9):858–865. doi: 10.1111/j.1365-2923.2008.03144.x. [DOI] [PubMed] [Google Scholar]
- 21.Eva KW. On the limits of systematicity. Med Educ. 2008;42(9):852–853. doi: 10.1111/j.1365-2923.2008.03140.x. [DOI] [PubMed] [Google Scholar]
- 22.Cox CE, Carson SS, Ely EW, Govert JA, Garrett JM, Brower RG, et al. Effectiveness of medical resident education in mechanical ventilation. Am J Respir Crit Care Med. 2003;167(1):32–38. doi: 10.1164/rccm.200206-624OC. [DOI] [PubMed] [Google Scholar]
- 23.Brescia D, Pancoast TC, Kavuru M, Mazer M. A survey of fellowship education in mechanical ventilation. Chest. 2008;134(suppl 4):62. doi: 10.1378/chest.134.4_MeetingAbstracts.s62004. [DOI] [Google Scholar]
- 24.Tallo FS. de Campos Vieira Abib S, de Andrade Negri AJ, Cesar PF, Lopes RD, Lopes AC. Evaluation of self-perception of mechanical ventilation knowledge among Brazilian final-year medical students, residents and emergency physicians. Clinics (Sao Paulo) 2017;72(2):65–70. doi: 10.6061/clinics/2017(02)01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilcox SR, Seigel TA, Strout TD, Schneider JI, Mitchell PM, Marcolini EG, et al. Emergency medicine residents' knowledge of mechanical ventilation. J Emerg Med. 2015;48(4):481–491. doi: 10.1016/j.jemermed.2014.09.059. [DOI] [PubMed] [Google Scholar]
- 26.Richards JB, Strout TD, Seigel TA, Wilcox SR. Psychometric properties of a novel knowledge assessment tool of mechanical ventilation for emergency medicine residents in the northeastern United States. J Educ Eval Health Prof. 2016;13:10. doi: 10.3352/jeehp.2016.13.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O'Boyle AL, Mink RB, Anas NG, Kallay TC. Development of learning objectives and a validated testing tool for management of pediatric mechanical ventilation. Pediatr Crit Care Med. 2014;15(7):594–599. doi: 10.1097/PCC.0000000000000195. [DOI] [PubMed] [Google Scholar]
- 28.Goligher EC, Ferguson ND, Kenny LP. Core competency in mechanical ventilation. Crit Care Med. 2012;40(10):2828–2832. doi: 10.1097/CCM.0b013e31825bc695. [DOI] [PubMed] [Google Scholar]
- 29.Dorman T, Angood PB, Angus DC, Clemmer TP, Cohen NH, Durbin CG, Jr, et al. Guidelines for critical care medicine training and continuing medical education. Crit Care Med. 2004;32(1):263–272. doi: 10.1097/01.CCM.0000104916.33769.9A. [DOI] [PubMed] [Google Scholar]
- 30.Schroedl CJ, Corbridge TC, Cohen ER, Fakhran SS, Schimmel D, McGaghie WC, et al. Use of simulation-based education to improve resident learning and patient care in the medical intensive care unit: a randomized trial. J Crit Care. 2012;27(2):219.e7–219.e13. doi: 10.1016/J.JCRC.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 31.Singer BD, Corbridge TC, Schroedl CJ, Wilcox JE, Cohen ER, McGaghie WC, et al. First-year residents outperform third-year residents after simulation-based education in critical care medicine. Simul Healthc. 2013;8(2):67–71. doi: 10.1097/SIH.0b013e31827744f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yee J, Fuenning C, George R, Hejal R, Haines N, Dunn D, et al. Mechanical ventilation boot camp: a simulation-based pilot study. Crit Care Res Pract. 2016;2016:1–7. doi: 10.1155/2016/4670672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spadaro S, Karbing DS, Fogagnolo A, Ragazzi R, Mojoli F, Astolfi L, et al. Simulation training for residents focused on mechanical ventilation: a randomized trial using mannequin-based versus computer-based simulation. Simul Healthc. 2017;12(6):349–355. doi: 10.1097/SIH.0000000000000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mireles-Cabodevila E, Kapoor A, Duggal A, Chaisson NF, Ashton RW, Rathz DA, et al. Teaching mechanical ventilation in the era of 300 modes of ventilation. American Thoracic Society. Innovations in Fellowship Education. 2015 https://www.thoracic.org/professionals/career-development/fellows/innovations-in-fellowship-education/2015/cleveland-clinic.php Accessed May 22, 2019.
- 35.Ramar K, De Moraes AG, Selim B, Holets S, Oeckler R. Effectiveness of hands-on tutoring and guided self-directed learning versus self-directed learning alone to educate critical care fellows on mechanical ventilation—a pilot project. Med Educ Online. 2016;21:32727. doi: 10.3402/meo.v21.32727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Belfield C, Thomas H, Bullock A, Eynon R, Wall D. Measuring effectiveness for best evidence medical education: a discussion. Med Teach. 2001;23(2):164–170. doi: 10.1080/0142150020031084. [DOI] [PubMed] [Google Scholar]