Abstract
Background/Aims
The anastomotic strictures are one of the most common colorectal surgery complications, and various endoscopic techniques have been defined. Balloon dilation is the most well-known and the simplest procedure. In this article, we aimed to present our series of endoscopic interventions and electroincision management for anastomotic strictures.
Materials and Methods
The files of 59 patients, who underwent colorectal surgery between January 2010 and September 2017 in our hospital and were diagnosed during the follow-up with anastomotic stricture, were analyzed. The outcomes of endoscopic interventions such as balloon dilation and electroincision were compared and reported.
Results
The mean age of the 59 patients included in the study was 59.5±16.26 years. The primary operative indications were colorectal cancer in 46, inflammatory bowel disease in 7, diverticulum in 5, and penetrating trauma in one patient. Single- or multiple-balloon dilations were successful in 48 patients. Electroincision was performed in 11 patients because of the balloon dilation failure. None of the patients needed a secondary surgery. During the mean 33.75 months of the follow-up, the stricture recurred in seven patients who had undergone balloon dilation. Repeated balloon dilation was successful in these patients without any need for an additional surgical intervention.
Conclusion
Balloon dilation can be performed safely as the primary treatment option, because of its easy access and noninvasive application. Electroincision is also a safe and effective endoscopic technique that can be preferred especially when the balloon dilation fails.
Keywords: Colorectal, anastomotic stricture, endoscopic, balloon dilation, electroincision
INTRODUCTION
Anastomosis leakage, fistula, bleeding, and stenosis are among the major complications that can develop following surgical procedures involving gastrointestinal system (GIS). Postoperative benign anastomotic stricture (POBAS) is one of the complications seen at rates between 3% and 30% following colorectal surgery (1). Although the definite pathological cause has not been established, several factors such as previous radiotherapy, improper stapler use, postoperative early complications, development of ischemia due to inadequate blood supply, and diagnosis of inflammatory bowel disease (IBD) were reported to increase the risk (2,3). Despite being a serious complication, it is possible to obtain favorable results with digital dilation or endoscopic methods. As reoperation has a high risk and high morbidity rate, endoscopic techniques became an appealing alternative. Bougie and balloon dilation are the most commonly used techniques (4). In addition, other techniques such as corticosteroid injection, stent placement, electroincision (electronic incision), or mitomycin-C injection are also available (5,6). Surgical treatment is performed to overcome the complications that develop during endoscopic interventions or for the recalcitrant cases.
In this study, we aimed to present our series of endoscopic interventions and electroincision management for anastomotic strictures.
MATERIALS AND METHODS
The study protocol was approved by the institutional Ethics Committee. Written informed consent was obtained from each patient. The study was conducted in accordance with the principles of the Declaration of Helsinki.
A total of 884 colorectal surgical procedures including anastomosis, 676 as elective and 208 as emergent cases, due to both benign and malignant causes, were performed in the General Surgery Department of our hospital between January 2010 and September 2017. The stenosis that did not allow a passage of the adult colonoscopy (of 12 millimeters) or that caused obstruction symptoms despite the presence of the passage was defined as POBAS (Figure 1).
Figure 1.
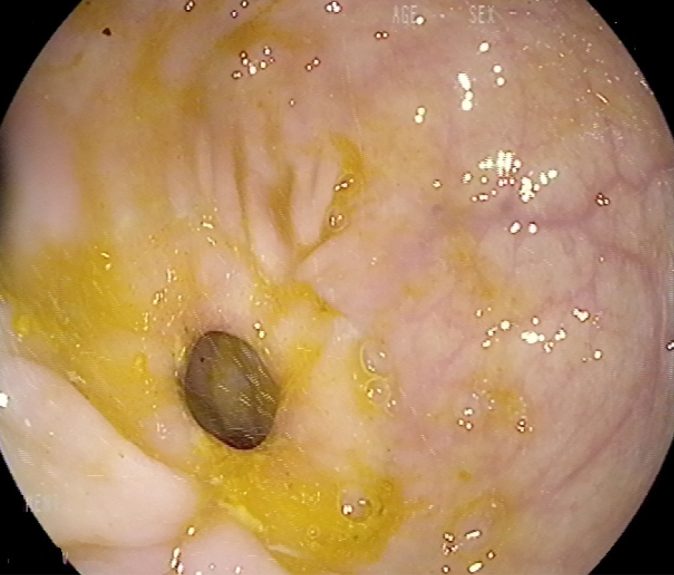
Anastomotic stricture.
Fifty-nine (6.7%) patients in whom POBAS developed during the follow-up were included in the study, and their files were retrospectively reviewed. Characteristic features such as age, sex, surgical procedure, and type, the presence of any complication following the procedure, the time of development of anastomotic stricture, localization, length and symptoms, endoscopic treatment procedure, and the number of sessions were recorded. The diagnosis of the stricture and its localization based on radiological tests and colonoscopic interventions were defined.
A histopathological evaluation was performed in the suspected cases of malignancy. Patients with malignant strictures, affecting the long segment, multiple strictures, or the ones in whom colonoscopy was contraindicated due to additional diseases were excluded from the study (n=42).
The length and diameter of the stricture was assessed by endoscopy; since the diameter of the utilized gastroscopy (Olympus GIF H190, 9.9 mm, Tokyo, Japan) or nasal scope (Olympus 5.9 mm, Tokyo, Japan) or dimensions of the needle-tipped sphincterotome (Olympus, Japan, KD-441Q Needle Knife) (diameter of the external sheet, 1.7 mm; length of knife, 5 mm) were known, dimensions of the stricture were calculated based on these values. In cases where endoscopic evaluation was not possible, the assessment was performed by barium radiography or computed tomography or magnetic resonance.
Balloon dilation
The aim was to perform dilation by concurrent application of a radial force to the full length of the stricture. First, the stricture was passed with the guidewire, and then the balloon was advanced through the running canal of the endoscope and through-the-scope balloon dilation was performed, reaching 35 millimeters. The balloon was gradually inflated with air and kept there for approximately 30 to 60 seconds. These balloons have three different insufflation steps that provide gradual dilation.
Electroincision
All electroincision dilation procedures were performed by a single gastroenterologist, experienced in endoscopic submucosal dissection and per-oral endoscopic myotomy (F.A.). Following preoperative preparation for colonoscopy, the procedure was performed under sedo-anesthesia in the endoscopy unit. The anastomosis line was examined for recurrence by using the narrow-band-imaging and chromo-endoscopic techniques (indigocarmine staining) under colonoscope (Olympus CF HQ190L/I, Tokyo, Japan). Then, we attempted to advance the colonoscopy to the proximal part of the anastomosis line. When it was not possible to pass the colonoscope through the stricture area, we would try to reach the proximal part by using gastroscopy (Olympus GIF H190, 9.9 mm, Tokyo, Japan) or a nasal scope (Olympus 5.9 mm, Tokyo, Japan). The proximal part of the stricture area was examined. The margins of the fibrosis tissue that caused the stricture of the anastomosis line were examined from both the proximal and distal part of the anastomosis line. A radial incision was, then, performed to the fibrotic margins with an insulated-tip knife (IT Knife2, Olympus, Tokio, Japan). Following the procedure, the orifice of the anastomosis line was evaluated by colonoscopy. The patients without any complications, such as perforation or bleeding, were discharged on the same day. All patients were scheduled for follow-up once every 3 weeks. In case of recurrent strictures, the procedure was repeated.
Statistical analysis
A statistical analysis was performed using the Statistical Package for Social Sciences version 11.0.1 (SPSS Inc.; Chicago, IL, USA). Categorical variables were compared between the two groups using the chi-squared or Fisher’s exact tests. Student’s test was used to compare continuous variables between the two groups. Univariate and multivariate logistic regression models were used to analyze the association between previous abdominal surgery and switching to open surgery. A p-value of <0.001 was considered statistically significant.
RESULTS
Of 59 patients included in the study, 37 (62.7%) were males, and the mean age was 59.5±16.26 (range, 30 to 86) years. Forty-nine patients (83%) were operated under elective conditions, and 10 patients (17%) were operated under emergent conditions. Thirty-three patients underwent surgery due to rectal cancer, 13 due to colon cancer, 7 due to IBD, 5 due to diverticulitis, and 1 due to penetrating trauma (stab wound). The indications for emergent surgery were diverticulitis (4 patients), IBD (4 patients), rectal cancer (1 patient), and stab wound (1 patient).
Fifteen patients with rectal cancer received neoadjuvant radiotherapy, while diverting ileostomy was performed in 12.
During the postoperative period, complications developed in 13 (22%) patients as wound infection in 5, intraabdominal bleeding in 2, and anastomosis leakage in six patients. Basic characteristics of the patients, the procedures, and the complication are summarized in Table 1. In all patients, anastomosis was performed using a stapler in different sizes (31 mm, 28 mm, circular surgical staplers).
Table 1.
Basic characteristics and operations of the patients.
| Number (n) | Percentage (%) | ||
|---|---|---|---|
| Sex | Male | 37 | 62.7 |
| Female | 22 | 37.3 | |
|
| |||
| SD (range) average±[years] | Range | ||
|
| |||
| Age | Male | 64±14.26 | (31–86) |
| Female | 52.3±17.24 | (30–68) | |
| Total | 59.5±16.26 | (30–86) | |
|
| |||
| Number (n) | Percentage (%) | ||
|
| |||
| Surgical diagnosis | Colon cancer | 13 | 22 |
| Rectum cancer | 33 | 55.9 | |
| Inflammatory bowel disease | 7 | 11.9 | |
| Diverticulum | 5 | 8.5 | |
| Stab wound | 1 | 1.7 | |
| Type of the surgery | Elective | 49 | 83 |
| Emergency | 10 | 17 | |
| Surgical procedure | Right hemicolectomy | 5 | 8.4 |
| Sigmoid resection | 10 | 17 | |
| Anterior resection | 10 | 17 | |
| Low ant. resection | 33 | 55.9 | |
| Total colectomy | 1 | 1.7 | |
| Symptoms | Constipation | 15 | 25.4 |
| Constipation, abdominal distention | 9 | 15.3 | |
| Defecation problems and irregularity | 9 | 15.3 | |
| Ileus | 5 | 8.4 | |
| Asymptomatic | 21 | 35.6 | |
| Postoperative complication (n:13/22%) | Wound infection | 5 | 38.5 |
| Intraabdominal hemorrhage | 2 | 15.4 | |
| Leakage | 6 | 46.1 | |
| Technique for dilation | Balloon dilation | 48 | 81.4 |
| Electroincision | 11 | 18.6 | |
The mean POBAS diameter was 5.6±1.65 mm (range, 2 to 10 mm), and the mean time for the development of POBAS was 8.75±4.34 months (range, 1 to 19 months). There was a statistically significant correlation between the time for POBAS development and the length and diameter of the stricture (p<0.001). Balloon dilation was successful in 48 patients (81.4%). Among these, it was possible to perform a successful balloon dilation after one session in 36 (75%), after two sessions in 6 (12.5%), and after three sessions in six patients (12.5%) (Figures 2, 3, and 4). A statistically significant difference was found between the diameter of the stricture and the number of sessions, and as the diameter decreased, the number of sessions increased (p<0.001). Endoscopic electroincision was done in 11 patients (18.6%) in whom balloon dilation failed (Video 1). No major complications, such as perforation or bleeding, were observed both during and after the procedure. A comparison between balloon dilation and electroincision has been summarized in Table 2, which shows that there is a significant difference in surgical diagnosis, surgical procedure, and symptoms at the time of admission between the groups (p<0.001).
Figure 2.
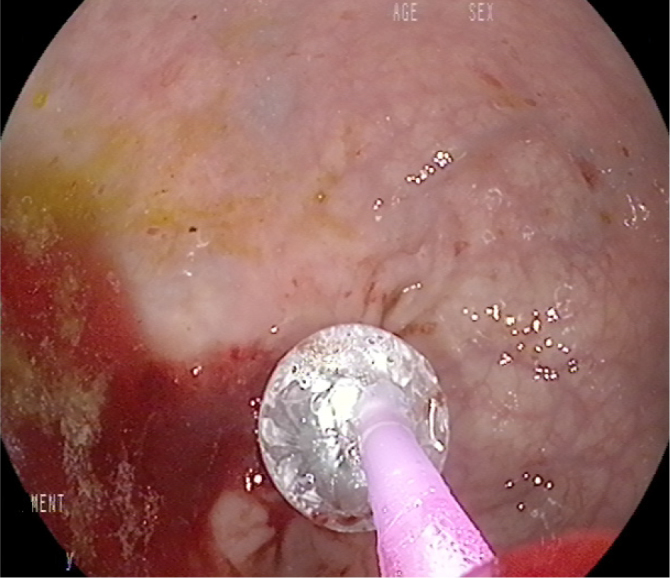
Advancement of balloon through anastomosis line with guidewire and its inflation.
Figure 3.
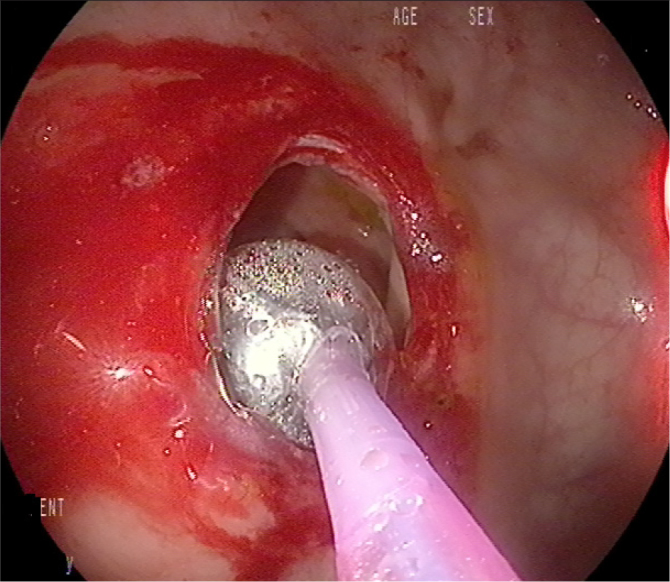
Dilation of stricture with balloon.
Figure 4.
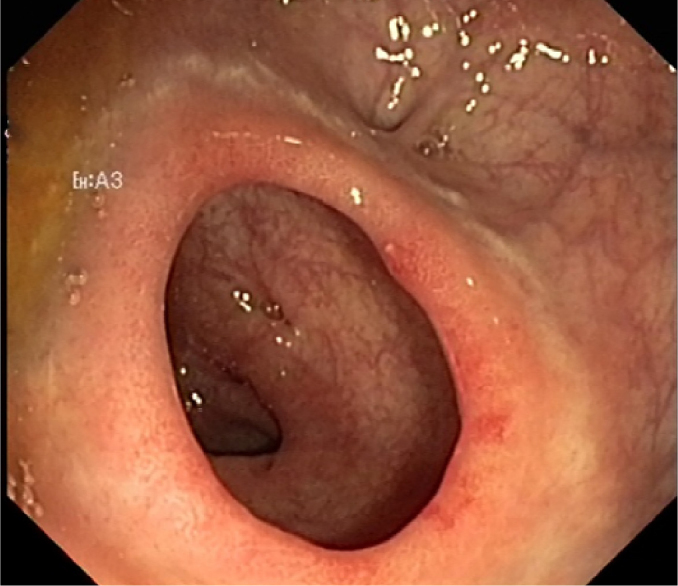
Control colonoscopy following balloon dilation (1 month after the dilation).
Video 1.
Performing electroincision.
Table 2.
Comparison of balloon dilation and electroincision.
| Balloon Dilation (n:48/81.4%) | Electroincision (n:11/18.6%) | p | ||
|---|---|---|---|---|
| Sex | Male (n:37) | 30 (62.5%) | 7 (28.6%) | 0.119 |
| Female (n:22) | 18 (37.5%) | 4 (71.4%) | ||
| Age (year) | Male | 62.9 (31–86) | 76.5 (75–78) | 0.801 |
| Female | 55.2 (30–68) | 46.6 (34–63) | ||
| Total | 60.5 (30–86) | 55.1 (34–75) | ||
| Surgical diagnosis | Colon cancer (n:13) | 13 (27%) | - | <0.001 |
| Rectum cancer (n:33) | 30 (62.5%) | 3 (27.3%) | ||
| Inflammatory bowel disease (n:7) | 2 (4.2%) | 5 (45.4%) | ||
| Diverticulum (n:5) | 2 (4.2%) | 3 (27.3%) | ||
| Stab wound (n:1) | 1 (2.1%) | - | ||
| Type of the surgery | Elective (n:49) | 43 (89.6%) | 6 (54.6%) | 0.622 |
| Emergency (n:10) | 5 (10.4%) | 5 (45.4%) | ||
| Surgical procedure | Right hemicolectomy (n:5) | 5 (10.4%) | - | <0.001 |
| Sigmoid resection (n:10) | 7 (14.6%) | 3 (27.3%) | ||
| Anterior resection (n:10) | 5 (10.4%) | 5 (45.4%) | ||
| Low ant. resection (n:33) | 30 (62.5%) | 3 (27.3%) | ||
| Total colectomy (n:1) | 1 (2.1%) | - | ||
| Symptoms | Constipation (n:15) | 13 (27.1%) | 2 (14.2%) | <0.001 |
| Constipation, abdominal distention (n:9) | 5 (10.4%) | 4 (28.6%) | ||
| Defecation problems and irregularity (n:9) | 7 (14.6%) | 2 (28.6%) | ||
| Ileus (n:5) | 2 (4.2%) | 3 (28.6%) | ||
| Asymptomatic (n:21) | 21 (43.7%) | - | ||
| Postoperative complication (n:13) | Wound infection (n:5) | 1 (20%) | 4 (50%) | 0.259 |
| Intraabdominal hemorrhage (n:2) | 1 (20%) | 1 (12.5%) | ||
| Leakage (n:6) | 3 (60%) | 3 (37.5%) |
The mean follow-up was 33.75±5.86 months (range, 6 to 81 months). Stricture recurred in seven patients who had undergone balloon dilation, four patients with IBD, and three patients with rectal cancer. Balloon dilation was successful in these patients without any need for a repeated surgical intervention.
DISCUSSION
Our findings support that electroincision can be performed safely and successfully when other endoscopic interventions fail. Our success rate was 100% at a mean follow-up duration of 33.75 months, and none of the patients developed any complications during the intervention. In concordance with previous publications, most patients who had to receive electroincision due to resistant stenosis had inflammatory disorders (such as diverticulitis, IBD). This condition is considered to be caused by the inflammation-triggered fibrosis (7). In addition, it has lower recurrence rates compared to endoscopic interventions, and it can be combined with other methods (8,9). However, it requires advanced endoscopic experience as it is a more invasive method, and the factors such as the depth, length, and number of the incisions have to be determined by the endoscopist.
Treatment in these patients varies from conservative methods to surgical resection. As the surgical reoperation has a high risk and high morbidity, endoscopic interventions such as the balloon-bougie dilation, stent placement, steroid or mitomycin-C injection, and electroincision became increasingly popular in recent years. It is crucial to rule out the tumor recurrence by taking a biopsy from the anastomosis when endoscopic interventions are planned. Digital dilation or surgical reoperation are performed in cases where endoscopic interventions are successful (10). In the present study, all patients were successfully treated with endoscopic interventions.
An endoscopic balloon or bougie dilation with a low risk of complications and high success rates is accepted as a reliable and first-line treatment method in benign GIS strictures (11). Its success rate ranges between 59% and 100% (12). The success rate can also vary depending on the type, length, and localization of the stricture and the presence of ulcer on the stricture (13). This rate is lower, and the rate of perforation following intervention is higher in cases where the diameter of the stricture area is <5 mm, and its length is >1 cm (11). The most challenging cases are with the strictures that have developed following an anastomosis leakage, and the success rate in these cases is lower. It may be necessary to repeat dilation sessions 2 or 3 times until the clinical recovery is achieved (14). In the study by Zippi et al. (15), full recovery was achieved after a mean number of sessions of 1.5 in 12 patients with the diagnosis of colon cancer. In our study, the mean number of sessions was 1.4 (range, 1 to 3), except in three patients (37.5%) in whom the balloon dilation failed, there was a history of anastomotic leakage during the postoperative period.
In a previous study including 422 patients with rectal cancer, stricture developed in a total of 26 patients, of whom 16 were males and 10 were females (16). The median age of the patients was 66 years, and there was a history of neoadjuvant radiotherapy in 23 patients. The mean time for the stricture development was 6 months. Balloon dilation was performed in all patients in whom POBAS developed, and the success rate was 85.5% with the mean number of dilation sessions of 2. Patients’ characteristics in our study were almost similar to the aforementioned study with a success rate of 81.4%.
The risk of perforation in the balloon or bougie dilation is about 4%, whereas it is reported as 0.1%–0.4% in electroincision (17). The risk of perforation through the vulnerable wall of the anastomosis increases in common dilation methods, such as balloon and bougie, as the force is transferred in an uncontrolled way in the transverse and longitudinal planes. However, electroincision decreases the perforation risk, when the balloon dilation is required in addition to cutting the thickened mucosal collagen fibers, and it enables the dilation procedure with a lower balloon pressure (18).
POBAS is usually observed within first 4 months of surgery. The stapler use increases the risk, and the use of a narrow-diameter anvil (25–28 mm) is also an important risk factor (19). Although the ostomy does not increase the risk of POBAS, it may aggravate the existing stricture. In addition, the transmission of stool through the anastomosis is critical for the continuation of physiological calibration (19). In this study, a 28 mm anvil was used in the majority of patients with stricture. In addition, 20.3% of the patients received diverting ileostomy. We found no statistically significant difference between the patients with or without ostomy.
The incidence of POBAS was approximately 80% in previous studies in which colonoscopic follow-up programs were carried out during the early postoperative period, and most of the POBAS cases were asymptomatic. Therefore, it is not necessary to restrict all the anastomosis when a stricture is detected during the colonoscopy since most of these strictures spontaneously recover in a period ranging from 6 months to a year following surgery. On the other hand, symptomatic patients are admitted to hospital with the obstructive symptoms, such as constipation, alteration, and/or irregularity in defecation habits and ileus. Treatment should be performed if the patient is symptomatic, or POBAS is detected before the procedure of colostomy closure or the colonoscopy, it is unable to pass the stricture (20). In the case series of Delaunay et al. (16), 78% of the patients were symptomatic, and in the case series of Placer et al. (19) 57.7% of the patients were symptomatic. In the present study, there were various symptoms in 64.4% of the patients.
A mean POBAS diameter was reported as 4.6±1.95 mm (range, 2 to 9 mm) in a previous study by Avcioglu et al., while Ambrosetti et al. reported a mean POBAS diameter of 7 mm. In addition, the mean time for POBAS development was found to be 6.85±4.31 mm (range, 1 to 17 mm) (7, 8). In our study, the mean diameter was 5.6±1.65 (range, 2 to 10 mm), and the mean time for POBAS development was 8.75±4.34 months (range, 1 to 19 months).
While it’s retrospective design represents the limitation to this study, to the best of our knowledge, it is one of the largest single-center experiences on electroinsion. In our limited experience with 11 patients who underwent electroinsion for POBAS, no adverse outcomes were observed. In addition, a video of electroincision procedure is available for the clinicians. We believe that as the experience with electroincision increases, the need for a radical surgery and/or permanent colostomy will decrease in POBAS cases.
Acknowledgements
The authors thank all the general surgery staff for their cooperation. The authors also express their gratitude to Dr. Emre Görgün, Department of Colorectal Surgery, Cleveland Clinic, for sharing his valuable recommendations.
Footnotes
This study was presented as poster presentation at the ESCP’s 13th Scientific and Annual Meeting, September 2018, Nice, France.
Ethics Committee Approval: Ethics committee approval was received from the Ethics Committee of İzmir Katip Çelebi University.
Informed Consent: Written informed consent was obtained from the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - T.A., N.A., F.A.; Design - T.A., N.A., F.A.; Supervision - E.K., B.Ü., M.H.; Materials - T.A., F.A., E.K.; Data Collection and/or Processing - N.A., B.Ü., E.K.; Analysis and/or Interpretation - B.Ü., M.H.; Literature Search - T.A., N.A., F.A.; Writing - T:A., N.A., F.A.; Critical Reviews - E.K., B.Ü., M.H.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Forshaw MJ, Maphosa G, Sankararajah D, et al. Endoscopic alternatives in managing anastomotic strictures of the colon and rectum. Tech Coloproctol. 2006;10:21–7. doi: 10.1007/s10151-006-0246-5. [DOI] [PubMed] [Google Scholar]
- 2.Schlegel RD, Dehni N, Parc R, et al. Results of reoperations in colorectal anastomotic strictures. Dis Colon Rectum. 2001;44:1464–8. doi: 10.1007/BF02234598. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen-Tang T, Huber O, Gervaz P, et al. Longterm quality of life alter endoscopic dilation of strictured colorrectal or colocolonic anastomoses. Surg Endosc. 2008;22:1660–6. doi: 10.1007/s00464-007-9679-9. [DOI] [PubMed] [Google Scholar]
- 4.Kim PH, Song HY, Park JH, et al. Safe and effective treatment of colorectal anastomotic stricture using a well-defined balloon dilation protocol. J Vasc Interv Radiol. 2012;23:675–80. doi: 10.1016/j.jvir.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 5.Small AJ, Young-Fadok TM, Baron TH. Expandable metal stent placement for benign colorectal obstruction: outcomes for 23 cases. Surg Endosc. 2008;22:454–62. doi: 10.1007/s00464-007-9453-z. [DOI] [PubMed] [Google Scholar]
- 6.Donatelli G, Ceci V, Cereatti F, et al. Minimally invasive treatment of benign complete stenosis of colorectal anastomosis. Endoscopy. 2008;40:263–4. doi: 10.1055/s-2008-1077660. [DOI] [PubMed] [Google Scholar]
- 7.Ambrosetti P, Francis K, Peyer R, et al. Colorectal anastomotic stenosis after elective laparoscopic sigmoidectomy for diverticular disease: a prospective evaluation of 68 patients. Dis Colon Rectum. 2008;51:1345–9. doi: 10.1007/s10350-008-9319-z. [DOI] [PubMed] [Google Scholar]
- 8.Avcioglu U, Ölmez Ş, Pürnak T, et al. Evaluation of efficacy of endoscopic incision method in postoperative benign anastomotic strictures of gastrointestinal system. Arch Med Sci. 2015;11:970–7. doi: 10.5114/aoms.2015.52347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kan H, Furukawa K, Suzuki H, et al. An improvement in the quality of life after performing endoscopic balloon dilation for postoperative anastomotic stricture of the rectum. J Nippon Med Sch. 2007;74:418–23. doi: 10.1272/jnms.74.418. [DOI] [PubMed] [Google Scholar]
- 10.Curcio G, Spada M, Di Francesco F, et al. Completely obstructed colorectal anastomosis: a new non-electro surgical endoscopic approach before balloon dilation. World J Gastroenterol. 2010;16:4751–4. doi: 10.3748/wjg.v16.i37.4751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akarsu C, Unsal MG, Dural AC, et al. Endoscopic balloon dilation as an effective treatment for lower and upper benign gastrointestinal system anastomotic stenosis. Surg Laparosc Endosc Percutan Tech. 2015;5:138–42. doi: 10.1097/SLE.0000000000000090. [DOI] [PubMed] [Google Scholar]
- 12.Manta R, Mango L, Conigliaro R, et al. Endoscopic repair of post-surgical gastrointestinal complications. Dig Liver Dis. 2013;45:879–85. doi: 10.1016/j.dld.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 13.Hoffmann JC, Heller F, Faiss S, et al. Through the endoscope balloon dilation of ileocolonic strictures: prognostic factors, complications, and effectiveness. Int J Colorectal Dis. 2008;23:689–96. doi: 10.1007/s00384-008-0461-9. [DOI] [PubMed] [Google Scholar]
- 14.Dray X, Camus M, Chaput U. Endoscopic management of complications in digestive surgery. J Visc Surg. 2013;150:3–9. doi: 10.1016/j.jviscsurg.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 15.Zippi M, Traversa G, De Felici I, et al. Endoscopic therapy with balloon dilation in patients with colonic post anastomotic strictures. Personal experience. Clin Ter. 2011;162:539–42. [PubMed] [Google Scholar]
- 16.Placer C, Urdapilleta G, Markinez I, et al. Benign anastomotic strictures after oncologic rectal cancer surgery. Results of treatment with hydrostatic dilation. Cir Esp. 2010;87:239–43. doi: 10.1016/j.ciresp.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 17.Lew RJ, Kochman ML. A review of endoscopic methods of esophageal dilation. J Clin Gastroenterol. 2002;35:117–26. doi: 10.1097/00004836-200208000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Zhao H, Zhao L, Zhou Z, et al. The roles of connective tissue growth factor in the development of anastomotic esophageal strictures. Arch Med Sci. 2015;11:770–8. doi: 10.5114/aoms.2015.48147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Delaunay K, Barthelemy C, Dumas O, et al. Endoscopic therapy of benign colonic post-operative strictures: report on 27 cases. Gastroenterol Clin Biol. 2003;27:610–3. [PubMed] [Google Scholar]
- 20.Yaman İ, Derici H. Endoscopic Dilation of Benign Colonic Anastomotic Stricture. J Dis Colon Rectum. 2010;20:134–8. [Google Scholar]


