Abstract
Objective
To evaluate the daily practice of pediatricians, physician-perceived reasons for unsatisfactory effects of treatment, and unmet needs in the management of acute pain and/or fever.
Methods
This was a multinational (n=13), multicenter, non interventional, cross-sectional study conducted in Latin America, Africa, and the Middle East in children under 16 years of age with fever (defined as a central body temperature ≥38°C) and/or acute pain (defined as pain lasting ≤6 weeks). Data were collected during a single visit using a structured physician-administered questionnaire and case report forms.
Results
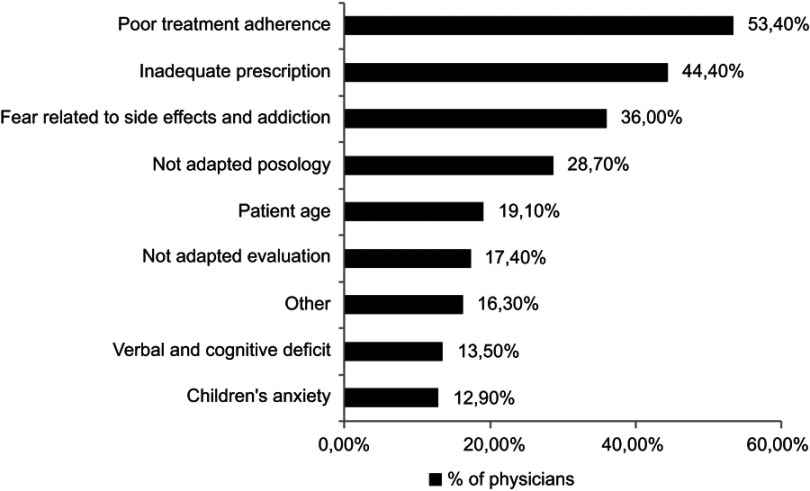
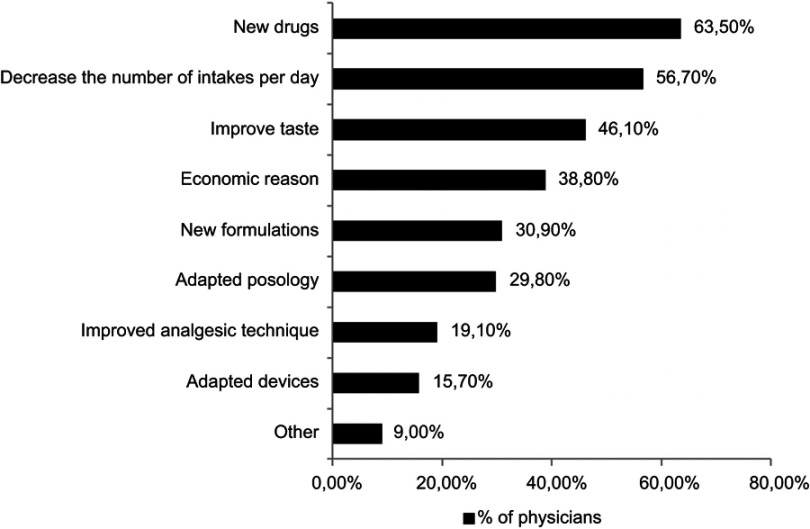
A total of 2125 patients were recruited by 178 physicians between September 2010 and September 2011. From the 2117 analyzed patients, 1856 (87.7%) had fever, 705 (33.3%) had acute pain, and 446 (21.1%) had both. Of 1843 analyzed patients with fever, 1516 (82.3%) were previously prescribed a pharmacological treatment for the management of fever concomitantly with a non pharmacological approach, while 1817/1856 patients (97.9%) were currently receiving a prescribed pharmacological treatment for fever. Paracetamol/acetaminophen was the most commonly prescribed antipyretic medication during both previous (70.8%) and current (64.1%) consultations. With regard to acute pain management, 67.2% of the patients received previous and 93.9% received current treatment for pain. The most frequently prescribed analgesic during previous consultations was paracetamol/acetaminophen (53.7%), and the current most commonly prescribed analgesics were non steroidal anti-inflammatory drugs (55.2%). Treatment patterns for patients with both fever and acute pain were similar. Overall, 53.4% of the physicians reported poor treatment compliance as a reason for the unsatisfactory effect of the pain/fever treatment, and the most common unmet need was the availability of new drugs (according to 63.5% of the physicians).
Conclusions
Adequate management of fever was observed; however, due to the complex etiology of pediatric pain, better evaluation and management of pain in pediatrics is necessary.
Keywords: acute pain, fever, non-steroidal anti-inflammatory drugs, paracetamol/acetaminophen, disease management, physician’s perception
Introduction
Fever and pain, either presenting individually or together, constitute major modulators of illness-related outcomes in pediatric medicine. Chronic pain affects 11–38% of children,1 and nearly 40% of children and adolescents complain of pain that occurs at least once weekly.2,3 Management of pain and/or fever in children is an important responsibility of physicians, and proper care results in reducing distress, treating underlying illnesses, and avoiding inappropriate medication.4
Pain experienced by children is a common outcome of injury, illness, or medical procedures and is a result of a complex interaction between sensory, emotional, cognitive, and behavioral components which are modulated by multidimensional factors, such as environmental, developmental, and sociocultural factors.4–6 Thus, our understanding of pain and the resultant suffering must transcend narratives focusing on sensory experiences, especially in pediatric patients where pain negatively impacts the overall health-related quality of life and is associated with poorer outcomes and psychological distress in both children and their primary caregivers – their parents.7–9
As per the Joint Commission on Accreditation of Healthcare Organizations standards, pain is deemed as “the fifth vital sign,” and caregivers are required to periodically monitor and address pain.2,10 However, its undertreatment in a substantial percentage of children has been well-documented.11 While a multidimensional approach to assessing care (including self-reports, behavioral, and physiological indicators) is considered necessary owing to the subjective nature of pain, a variety of age-sensitive tools are available for the assessment of pain in pediatrics, namely, facial expression-based scales such as the Neonatal Facial Coding Scale, the Children’s Revised Impact of Event Scale, the Verbal Rating Scale (VRS), and others. Appropriate management of pain in clinical settings, however, faces several barriers. According to the American Academy of Pediatrics, some of the barriers include 1) the myth that children, especially infants, do not feel pain the way adults do, or if they do, there is no untoward consequence; 2) lack of assessment and reassessment for the presence of pain; 3) misunderstanding of how to conceptualize and quantify a subjective experience; 4) lack of knowledge of pain treatment; 5) the notion that addressing pain in children takes too much time and effort; and 6) fears of adverse effects of analgesic medications, including respiratory depression and addiction with opioids.4 Written guidelines and protocols advocating the appropriate use of environmental, behavioral, and pharmacological interventions are important for the rational management of pediatric pain and will lead to the avoidance of inappropriate practices like sedation, which does not provide pain relief and may mask the response to pain.12
Fever, one of the most common symptoms of illness in children, is seen in 19–30% of patients in office-based pediatric practice.13,14 In a retrospective cohort study conducted among 5000 children in pediatric primary care practice, there were a total of 0.84 visits with fever ≥38°C per child per year and 0.24 visits per child per year with fever ≥39°C. These figures reflect the frequency of fever as a presentation of illnesses in children.15 Fever is not primarily an illness in itself but is rather a physiologic mechanism that plays an important role in fighting infection. Thus, when treating a febrile child, the focus should be on improving the child’s overall comfort rather than on normalizing the body temperature.16 Due to a perceived “fever phobia” and the concern that a child must maintain a “normal” temperature, several parents administer antipyretics even when the fever is minimal or absent.16 In a 13-question survey study of caregivers, none of the surveyed parents were able to appropriately define fever, and yet 93% mistakenly believed that high fever can cause brain damage.17
In view of the importance of the appropriate management of fever/pain in pediatric patients, meticulous documentation of their management practices could help in identifying shortcomings in current practices and formulating better treatment modalities. The main objective of this study was to evaluate the prescription patterns of analgesics, antipyretics, and NSAIDs in children with fever and/or acute pain presenting for medical care in different Latin American, African, and Middle Eastern countries.
Methods
Study design and participants
This was a multinational, multicenter, non interventional, cross-sectional study conducted in Latin America and the Caribbean (Costa Rica, Salvador, Honduras, Panama and Trinidad and Tobago grouped in one region – Central America and the West Indies, Argentina, Mexico, and Venezuela), the Middle East (Algeria, Egypt, Iran, and Lebanon), and Africa (Senegal). All necessary regulatory submissions were ensured as per local regulations.
The target population for this study was patients between the ages of 3 months and 16 years; patients with fever and/or acute pain; and patients who attended outpatient clinics or hospital emergency departments and who were prescribed analgesics, antipyretics, and NSAIDs by attending physicians. Fever was defined as a central body temperature ≥38°C (without intense activity) in a child normally covered and at room temperature. Fever was measured using an electronic (rectal, oral, or axillary) thermometer or an infrared or liquid crystal thermometer. For the purpose of the study, acute pain was defined as any, mild, moderate, or severe pain of various origins, with a duration ≤6 weeks. Pain was evaluated using a validated scale adapted to the children’s age: 1) a behavioral scale for children between 6 months and 4 years of age; 2) a facial expression scale or the VRS for children aged between 5 and 12 years; and 3) the VRS for children between 13 and 15 years. Patients who were currently participating or had recently participated in any other study and who were unable or unwilling to give consent were excluded.
Patients who met eligibility criteria and provided informed consent were recruited by physicians at different investigation sites that were selected on the basis of the geographical location of the site within the country and the patient population served. Each physician enrolled 10–15 patients. Patients were selected using simple random sampling.
Data collection
The data were collected by two methods in one single visit: a physician-administered questionnaire and case report forms. A structured, self‑reported questionnaire administered to the participating physicians was first developed in English, and it was translated into the local languages and back-translated into English by a blinded translator for ascertaining validity. The pre tested questionnaire was designed to assess the current practices in the diagnosis and management of children with fever and/or acute pain. The 21-item questionnaire also inquired about physicians’ demographic and professional characteristics, the perceived reasons for unsatisfactory effect of pain/fever treatment, and the unmet needs in the management of fever and pain.
The information that was collected on standardized case report forms included patients’ demographic and anthropometric characteristics; their medical history; the etiology, characteristics (duration and body temperature) and management (non pharmacological and pharmacological) approaches of fever; and the etiology, characteristics (duration and intensity), and management (non pharmacological and pharmacological) approaches of acute pain.
Outcomes
Primary outcomes were the most commonly prescribed antipyretic and analgesic medications during both previous and current consultations; the most commonly used tools to assess fever and acute pain; and the proportion of children using non pharmacological methods for the management of fever and acute pain. Physicians’ perceptions regarding the reasons for unsatisfactory effects of acute pain/fever treatment and the unmet needs in the management of acute pain and/or fever, as well as the characteristics of febrile and acute pain episodes were secondary outcomes.
Sample size estimation and statistical analysis
Since this study aimed to describe the real-world treatment patterns in pediatric patients with fever and/or acute pain, most findings were reported as proportions. To detect a proportion of 50%, at a 95% CI with the maximum marginal error of estimate not exceeding 7%, a sample size of 196 patients in each study country was estimated as appropriate. Assuming that data might not be available for 15–20% of patients, the estimated number of patients in each country was 240.
Data were analyzed separately according to the reported illness (patients with fever, patients with acute pain, and patients with both fever and acute pain), and according to age (between 3 and 24 months, between 2 and 6 years, between 6 and 12 years, and between 12 and 16 years). A descriptive analysis of the categorical variables was presented as counts and percentages, and continuous variables were presented as mean and SD. Data were statistically analyzed by using the non parametric Kruskal–Wallis test (for quantitative variables), the Chi-squared test, or Fisher’s exact test (for qualitative variables), as appropriate. All tests were two-sided, and a p-value <0.05 was considered significant. Statistical analyses were conducted using SAS 9.3 (SAS Institute Inc., Cary, NC, USA).
Ethics approval and informed consent
This study was approved by the Ministry of Higher Education, Research and Innovation (France). Ethics approvals were obtained from the local institutional review committee of each participating center, and the legal guardians of all participants gave written informed consent. Every effort was made to ensure protocol standardization and adherence, including translation of the questionnaire into languages specific to each region, on-site monitoring, and centralized database management. This study was conducted in accordance with the Declaration of Helsinki and the Good Epidemiological Practice.
Results
From September 2010 to September 2011, a total of 178 physicians, all of whom completed the questionnaire, participated in the study; two (one in Egypt and one in Mexico) did not recruit any patients. In total, 2125 patients were recruited; 8 patients were excluded due to major deviations, resulting in 2117 patients whose data were analyzed (Table S1).
The mean ± SD duration of clinical practice of physicians was 20.3±8.7 years. The majority (n=144; 80.9%) of the physicians were pediatricians.
Patient characteristics
The mean ± SD age of the patients was 4.4±3.8 years, most of whom (n=1576; 74.4%) were >6 years old, and only 5.9% were between 12 and 16 years. There was a slight gender imbalance (overall 54% boys), with significant differences in gender between the age groups (p=0.0039). The majority (92.2%) of the patients lived in an urban environment (Table 1). Upper and lower respiratory tract infections (RTIs) were the most frequently reported past (in 36.0% of the patients for upper and 13.1% for lower RTIs) and present (in 15.8% of the patients for upper and 5.7% for lower RTIs) medical conditions (Tables S2–S3).
Table 1.
Demographics and patient characteristics
| 3 to 24 months (N=702) | 2 to 6 years (N=874) | 6 to 12 years (N=415) | 12 to 16 years (N=126) | Total number of analyzed patients (N=2117) | |
|---|---|---|---|---|---|
| Age (years) | |||||
| Mean (± SD) | 1.05 (±0.45) | 3.7 (±1.1) | 8.6 (±1.8) | 14.2 (±1.7) | 4.4 (±3.8) |
| Gender (p=0.0039) | |||||
| Male; n (%) | 408 (58.1) | 454 (51.9) | 204 (49.2) | 78 (61.9) | 1144 (54.0) |
| Female; n (%) | 294 (41.9) | 420 (48.1) | 211 (50.8) | 48 (38.1) | 973 (46.0) |
| Housing location (p=0.2536) | |||||
| Urban; n (%) | 636 (90.6) | 814 (93.1) | 386 (93.0) | 115 (91.3) | 1951 (92.2) |
| Rural; n (%) | 66 (9.4) | 60 (6.9) | 29 (7.0) | 11 (8.7) | 166 (7.8) |
| Body temperature (°C; p<0.0001) | |||||
| Mean (± SD) | 38.7 (±0.7) | 38.6 (±0.8) | 38.4 (±1.0) | 38.2 (±1.0) | 38.6 (±0.8) |
| Weight (kg) | |||||
| Mean (± SD) | 9.5 (±2.3) | 15.7 (±3.8) | 28.3 (±9.4) | 48.4 (±12.5) | 18.0 (±11.7) |
| Height (cm) | |||||
| Mean (± SD) | 74.5 (±9.3) | 98.7 (±10.9) | 128.3 (±12.9) | 154.2 (±14.7) | 99.8 (±25.9) |
| BMI (kg/m2; p<0.0001) | |||||
| Mean (± SD) | 17.1 (±2.7) | 16.0 (±2.3) | 16.9 (±3.6) | 20.3 (±4.6) | 16.8 (±3.1) |
Abbreviations: BMI, Body mass index; SD, Standard deviation.
Fever
Of the patients (n=2117) whose data were analyzed, 1856 (87.7%) had fever (central body temperature ≥38°C). The proportion of patients with fever significantly (p<0.0001) decreased with age (668/702 [95.2%] in the age range 3–24 months; 784/874 [89.7%] in the age range 2–6 years; 322/415 [77.6%] in the age range 6–12 years, and 82/126 [65.1%] in the age range 12–16 years). The mean ±SD duration of the current episode of fever was 2.1±1.9 days, and RTIs represented the most commonly reported cause of fever (in 1334/1856 [71.9%] of febrile patients). Body temperature was significantly different according to the underlying disease (p=0.0009; Kruskal–Wallis test). Table S4 summarizes the characteristics (etiology and duration) of the current episode of fever in different age groups. Of note, electronic thermometer was the most widely used diagnostic tool by physicians (73/178; 41.0%), followed by the mercury thermometer (62/178; 34.8%). Temperature was most often taken using the axillary route (38/100; 38.0%).
Treatment patterns were distinguished on the basis of whether antipyretics and non pharmacological approaches had been previously prescribed before the current consultation (previous treatment) or prescribed during the current consultation (current treatments). Table 2 summarizes the previous and current treatments prescribed to patients with fever.
Table 2.
Previous and current treatments prescribed to patients with fever (N=1856)
| Treatment prescribed; n (%) | Previous | Current |
|---|---|---|
| Non-pharmacological; N | 1516 | 1817 |
| Warm water bath | 512 (33.8) | 627 (34.5) |
| Remove excess clothing and linens | 419 (27.6) | 706 (38.9) |
| Administrate oral hydration frequently | 387 (25.5) | 888 (48.9) |
| Bed rest | 159 (10.5) | 302 (16.6) |
| Ventilate room | 131 (8.6) | 311 (17.1) |
| Other | 83 (5.5) | 86 (4.7) |
| Pharmacological; N | 1516 | 1817 |
| Paracetamol/acetaminophen | 1073 (70.8) | 1165 (64.1) |
| NSAIDs | 544 (35.9) | 851 (46.8) |
| Metamizole | 61 (4.0) | 77 (4.2) |
| Aspirin | 19 (1.3) | 7 (0.4) |
Notes: Thirteen missing values were reported for patients with fever who were prescribed previous treatments, and among the remaining analyzed 1843 patients, 327 (17.7%) were not prescribed any previous treatment for their fever. A total of 39/1856 patients with fever (2.1%) were not prescribed any current treatment. Multiple pharmacological or non-pharmacological treatments were possible for each patient.
Abbreviation: NSAIDs, Non-steroidal anti-inflammatory drugs.
Overall, 1516 of 1843 analyzed patients with fever (82.3%) had been previously advised non pharmacological treatment concomitantly with a pharmacological treatment. Significant age-related differences were observed in the prescription of the removal of excess clothing and linens (p=0.0017; more frequently used in younger children) and bed rest (p<0.0001; more frequently used in older patients) (Table S5) during previous consultations. The most frequently prescribed antipyretic medications during previous consultations were paracetamol/acetaminophen (1073/1516; 70.8%) and NSAIDs (544/1516; 35.9%). Few adverse events (10/1073; 0.9% of the patients) related to a previous treatment with paracetamol were reported.
Treatments were prescribed to 1817/1856 patients (97.9%) during the current consultation (current treatment). Younger children were advised removal of excess clothing and linens significantly more often (p<0.0001) than older children and older patients were advised bed rest (p<0.0001 compared to younger children). The most commonly prescribed current medication for fever was paracetamol/acetaminophen (1165/1817; 64.1%). There was a significant difference between age groups for the use of paracetamol/acetaminophen during the current consultation (p<0.0001). Although paracetamol/acetaminophen was most commonly prescribed in all age groups, it was given slightly more frequently in the 3–24 months (74.7%) and the 12–16 years (61.3%) age groups than in the 2–6 years (57.9%) and 6–12 years (58.0%) age groups.
For both previous and current treatments, syrup formulation was the most commonly prescribed pharmaceutical form of paracetamol/acetaminophen in children aged <12 years and tablets in those ≥12 years.
No laboratory test was prescribed to most patients with fever (1169/1856; 63.0%). Complete blood count was the most frequently prescribed laboratory test (488/1856; 26.3%) in all age groups.
Pain
One-third (705/2117; 33.3%) of the analyzed patients had acute pain (duration ≤6 weeks), of which the most frequent cause was abdominal pain reported in 24.3% of patients. The proportion of patients with pain significantly increased with age (106/702 [15.1%] in the age range 3–24 months, 292/874 [33.4%] in the age range 2–6 years, 218/415 [52.5%] in the age range 6–12 years, and 89/126 [70.6%] in the age range 12–16 years; p<0.0001) (Table S6). The mean ± SD duration of the episode of pain was significantly longer in older patients (1.7±1.5 days in the age range 3–24 months versus 3.3±5.4 days in the age range 12–16 years; p=0.0132). The most commonly used method to estimate pain intensity was the observation of behavioral changes (in 238/705 or 33.8% of the patients); the observation of behavioral changes and the analysis of physiological signals (used in 51/705 or 7.2% of the patients) were significantly less used in older patients (p<0.0001 for behavioral changes and p=0.006 for physiological signals). The use of the VRS, the VAS, and the Numerical Rating Scale (NRS) for pain intensity estimation increased with age (p<0.0001 for VRS and NRS and p=0.016 for VAS); in 159 patients (22.6%), no instrument was used to evaluate pain intensity (Table S7).
A total of 471/701 analyzed patients (67.2%) received a previous treatment for pain and 659/702 (93.9%) received current treatment. Among the non pharmacological measures used to alleviate pain, bed rest was the most frequently prescribed measure during both previous (103/471; 21.9%) and current (176/659; 26.7%) consultations. Significant age-group differences were observed in the recommendation of massages (p=0.0271; more often used in the age range 3–24 months) and deep breath/relaxation (p=0.0316; more often used in the age range 12–16 years) during previous consultations and in the prescription of bed rest during the current consultation (p=0.0046; prescribed less often in age range 3–24 months) (Table S8).
The most frequently prescribed analgesic during previous consultations was paracetamol/acetaminophen (253/471; 53.7%); codeine was only used in two patients aged ≥12 years. NSAIDs (364/659; 55.2%) and paracetamol/acetaminophen (251/659; 38.1%) were the most frequently prescribed pharmacological treatments during the current consultation. For both previous and current treatments, syrup was the most commonly prescribed pharmaceutical form in children aged <12 years and tablets in those aged ≥12 years. Table 3 summarizes the current and previous treatments received by patients experiencing acute pain.
Table 3.
Previous and current treatments prescribed to patients with acute pain (N=705)
| Treatment prescribed; n (%) | Previous | Current |
|---|---|---|
| Non-pharmacological, N | 471 | 659 |
| Bed rest | 103 (21.9) | 176 (26.7) |
| Other | 41 (8.7) | 66 (10.0) |
| Massages | 22 (4.7) | 25 (3.8) |
| Heat | 15 (3.2) | 18 (2.7) |
| Cold | 13 (2.8) | 28 (4.2) |
| Distraction | 8 (1.7) | 17 (2.6) |
| Plays | 6 (1.3) | 14 (2.1) |
| Deep breath/relaxation | 3 (0.6) | 5 (0.8) |
| Ultrasound | 1 (0.2) | 5 (0.8) |
| Pharmacological, N | 471 | 659 |
| Paracetamol/acetaminophen | 253 (53.7) | 251 (38.1) |
| NSAIDs | 201 (42.7) | 364 (55.2) |
| Metamizole | 33 (7.0) | 45 (6.8) |
| Local anesthetics | 13 (2.8) | 27 (4.1) |
| Tramadol | 4 (0.8) | 6 (0.9) |
| Aspirin | 2 (0.4) | 4 (0.6) |
| Codeine | 2 (0.4) | 2 (0.3) |
| Morphine | 2 (0.4) | 17 (2.6) |
| Anti-depressants | 1 (0.2) | 1 (0.2) |
| Neuromodulators | - | 3 (0.5) |
Notes: Four missing values were reported for patients with acute pain who were prescribed previous treatments, and among the remaining analyzed 701 patients, 230 (32.8%) were not prescribed any previous treatment for their pain. Three missing values were reported for patients with acute pain who were prescribed current treatments, and among the remaining analyzed 702 patients, 43 (6.1%) were not prescribed any current treatment. Multiple pharmacological or non-pharmacological treatments were possible for each patient.
Abbreviation: NSAIDs, Non-steroidal anti-inflammatory drugs.
No laboratory tests were prescribed to most patients with pain (489/705; 69.4%), and laboratory tests were more often prescribed to patients aged ≥12 years (45/89; 50.6%). Complete blood count was the most often prescribed laboratory test (165/705; 23.4%) in all age groups.
Both pain and fever
Among the 2117 patients analyzed, 446 (21.1%) suffered from both fever and acute pain. Current and previous treatments for fever received in patients with both acute pain and fever are presented in Table 4. Table S9 illustrates the treatments prescribed for fever by age group in patients with both acute pain and fever. Paracetamol/acetaminophen was prescribed in 242/356 (68.0%) and 244/439 (55.6%) patients with both acute pain and fever who received any pharmacological treatment for their fever during previous consultations and during the current consultation, respectively. NSAIDs were prescribed in 137/356 (38.5%) and 217/439 (49.4%) patients during previous and current consultations, respectively.
Table 4.
Previous and current treatments prescribed for fever in patients with both acute pain and fever (N=446)
| Treatment prescribed, n (%) | Previous | Current |
|---|---|---|
| Non-pharmacological, N | 356 | 439 |
| Warm water bath | 121 (34.0) | 147 (33.5) |
| Administrate oral hydration frequently | 115 (32.3) | 214 (48.7) |
| Remove excess clothing and linens | 94 (26.4) | 145 (33.0) |
| Bed rest | 54 (15.2) | 100 (22.8) |
| Ventilate room | 37 (10.4) | 72 (16.4) |
| Other | 25 (7.0) | 17 (3.9) |
| Pharmacological, N | 356 | 439 |
| Paracetamol/acetaminophen | 242 (68.0) | 244 (55.6) |
| NSAIDs | 137 (38.5) | 217 (49.4) |
| Metamizole | 26 (7.3) | 36 (8.2) |
| Aspirin | 5 (1.4) | 2 (0.5) |
Notes: A total of 7/446 patients with both acute pain and fever (1.6%) were not prescribed any current treatment for their fever. Five missing values were reported for the patients with both conditions who were prescribed previous treatments, and among the remaining analyzed 441 patients, 85 (19.3%) were not prescribed any previous treatment for their fever. Multiple pharmacological or non-pharmacological treatments were possible for each patient.
Abbreviation: NSAIDs, Non-steroidal anti-inflammatory drugs.
With regard to pain management in patients with both fever and acute pain (Table 5), paracetamol/acetaminophen was prescribed in 182/322 (56.5%) and 172/419 (41.1%) treated patients during previous and current consultations, respectively. NSAIDs were prescribed in 138/322 (42.9%) and 219/419 (52.3%) patients during previous and current consultations, respectively. Table S10 summarizes the prescribed treatments used to relieve pain in patients with both acute pain and fever, by age group.
Table 5.
Previous and current treatments prescribed for pain in patients with both acute pain and fever (N=446)
| Treatment prescribed; n (%) | Previous | Current |
|---|---|---|
| Non-pharmacological; N | 322 | 419 |
| Bed rest | 83 (25.8) | 131 (31.3) |
| Other | 34 (10.6) | 38 (9.1) |
| Massages | 12 (3.7) | 12 (2.9) |
| Heat | 7 (2.2) | 11 (2.6) |
| Cold | 8 (2.5) | 14 (3.3) |
| Distraction | 2 (0.6) | 7 (1.7) |
| Plays | 2 (0.6) | 4 (1.0) |
| Deep breath/relaxation | 2 (0.6) | 1 (0.2) |
| Ultrasound | 1 (0.3) | 2 (0.5) |
| Pharmacological; N | 322 | 419 |
| Paracetamol/acetaminophen | 182 (56.5) | 172 (41.1) |
| NSAIDs | 138 (42.9) | 219 (52.3) |
| Metamizole | 31 (9.6) | 41 (9.8) |
| Local anesthetics | 11 (3.4) | 16 (3.8) |
| Morphine | 2 (0.6) | 16 (3.8) |
| Codeine | 1 (0.3) | 1 (0.2) |
| Aspirin | - | 4 (1.0) |
| Tramadol | - | 2 (0.5) |
| Neuromodulators | - | 1 (0.2) |
Notes: Three missing values were reported for the patients with both acute pain and fever who were prescribed current treatments for their pain, and among the remaining analyzed 443 patients, 24 (5.4%) were not prescribed any current treatment for their pain. Two missing values were reported for the patients with both acute pain and fever who were prescribed previous treatments for their pain, and among the remaining analyzed 444 patients, 122 (27.5%) were not prescribed any previous treatment for their pain. Multiple pharmacological or non-pharmacological treatments were possible for each patient.
Abbreviation: NSAIDs, Non-steroidal anti-inflammatory drugs.
There were no differences in age-wise trends in the management of fever and pain when data for the two were analyzed either separately (pain or fever) or together (pain and fever).
Unsatisfactory effects of treatment and unmet needs in the management of fever and acute pain
Figure 1 summarizes the physician-perceived reasons for unsatisfactory effects of acute pain/fever treatment. More than half (95/178; 53.4%) of the physicians reported bad treatment compliance as a reason for the unsatisfactory effect of the pain/fever treatment. Figure 2 summarizes the unmet needs in fever and pain management, according to physicians’ perceptions. The most common unmet needs reported by physicians were the availability of new drugs (reported by 113 or 63.5% of the physicians), a decrease in the number of daily intakes (101/178; 56.7%), and improved taste of medicines (82/178; 46.1%).
Figure 1.
Reasons for unsatisfactory treatment effects according to physicians’ perceptions.
Figure 2.
Unmet needs in fever and pain management according to physicians’ perceptions.
Country-wise analysis
Few differences were observed in this study between countries regarding the use of paracetamol/acetaminophen and NSAIDs. However, the use of mercury thermometer largely varied from a low of 3.6% in Algeria to a high of 85.7% in Venezuela.
Discussion
The current observational study was conducted to evaluate the daily practice of pediatricians in terms of acute pain and fever management in Latin America, Africa, and the Middle East. Most patients received treatment for pain and/or fever in the current as well as previous consultation; both pharmacological and non pharmacological treatments were used in their management. Finkelstein et al reported an incidence of 19–30% for fever in office-based pediatric practice.15 In the current study, fever was seen in 87.7% of children, and it was more frequent in younger children. This could reflect upon parental concerns about fever, which in medical literature has been called “fever phobia,” resulting in more frequent visits to physicians.18
Paracetamol/acetaminophen was the most widely used pharmacological agent for fever, followed by NSAIDs in the current study. This concurs with international data such as that reported by Purssell et al in a survey of 181 parents where 51% reported the use of paracetamol for home management of fever.19 Widespread use of ibuprofen and paracetamol has shown that they are both effective in the reduction of fever in the pediatric population.20 Few and minor adverse events related to a previous treatment with paracetamol were reported in this study. However, the study described in this manuscript was not aimed at or designed to assessing the safety or efficacy of any of the drugs reported on by the surveyed population.
The general lack of awareness about fever extends to the knowledge about appropriate measurement of fever intensity. Measurement of body temperature needs careful consideration as axillary and tympanic membrane temperatures have low sensitivity (50–65%);21 hence, appropriate temperature measurement in infants and young children is recommended to be rectal. Additionally, the use of mercury thermometer is not recommended due to mercury toxicity, and many countries have banned its medical use.22 In the current study, mercury thermometer was used in more than a third (34.8%) of patients, and axillary temperature was most commonly measured.
More than 80% of patients with fever had been previously advised non pharmacological treatment. Though indicated in the treatment of hyperthermia, the use of physical cooling methods remains debated in the treatment of fever because of their tendency to induce cutaneous vasoconstriction, shivering, sympathetic activation, and, most importantly, discomfort.23 Moreover, it has been reported that two-thirds of parents who use techniques like sponging perform the technique incorrectly, with alcohol or cool water.18 Hence, proper education of proximate caregivers to correctly administer treatment should be a prime concern in the management of fever.24
Among one-third of all patients who had pain, paracetamol and NSAIDs were the most widely used analgesics. The American Medical Association similarly reported that acetaminophen is the most commonly used analgesic agent in pediatric practice.25 Our results thus suggest that there is a need for better physician awareness of available pharmacological alternatives to current drugs. Especially, given the rapid changes in nociception in the early years of development,26 age-appropriate therapies must be used for analgesia.27 Adequate detection and mitigation of pain in pediatric patients is precluded by myths, personal beliefs, and values.4,28 In addition, health care professionals may lack awareness on the neonate’s capability of experiencing pain and fear about adverse effects related to analgesic use – this hampers neonatal pain management.12 When convincing evidence on physical pain is lacking, health care providers tend to defer treatment.29 Likewise, there is widespread tendency to give an underdose of analgesics to children, often due to fear of respiratory failure.29 In pediatric patients, analgesia (including opioids in case of severe pain) should be prescribed when indicated during medical care as adequate treatment of pain may result in decreased clinical complications and decreased mortality.30
In the current study, in contrast with the management of fever, in most patients, non pharmacological measures to alleviate pain were not used. Non pharmacological options must be considered either as substitutes or as complements. Thus, cognitive behavioral strategies that involve the use of imagery, relaxation, respiration, autohypnosis, and self-regulation can provide pain relief,31,32 and evidence-based non pharmacological strategies are reported to be frequently used and perceived as effective by the child life specialists.33
Pain intensity was evaluated through various methods in our study; the most frequently used were behavioral changes, the VRS, and facial expression scales. Systematic evaluation of pain in neonatal intensive care units has been shown to improve awareness of treating pain and to increase the use of analgesics.34,35 Despite the seeming advantages of using standardized pain assessment tools, individual self-report is often favored because pain is a subjective experience. Nonetheless, it should be ensured that children, especially those in the age group of 3–7 years, are competent to provide information, and behavioral observation should be used to complement/supplement self-report when necessary.4 Increasingly, the management and assessment of pain by specialized pain teams is being seen as a useful approach in improving clinical outcomes in conditions involving pain.29,36
While the current study affords us an opportunity to examine the clinical practices in terms of fever and pain management, the understanding gained is limited by the fact that a limited number of investigators from each country were selected. The sample of investigation sites in the study was not estimated on the basis of the size of the country. Thus, data from countries with larger populations might need further confirmation by larger, country-specific studies. Other limitations of the study include the inability to study the interregional variation in the patterns of prescription of analgesics, antipyretics, and NSAIDs. This is mainly due to the fact that most participating countries in this study were from Latin America and the Caribbean, and the number of countries in the other regions was too small to make comparisons between regions. However, analyses by country were conducted, and few differences were observed between the countries. This study is also limited by its cross-sectional nature and by the fact that it is based on self-reported evaluations rather than observed real-life practice. Furthermore, our data are observational and might be affected by a possible selection bias with regard to the investigation sites invited to participate. Nevertheless, in the absence of any other such real-world evidence from a large multinational study, the current data and findings are valuable evidence for both physicians and parents caring for children with fever and/or acute pain.
Conclusion and implications for practice
Although randomized clinical trials remain the gold standard for advancing knowledge in medicine, multinational studies of real-world data on prescription patterns, such as the present study, provide a means to better understand many aspects of fever and pain management, practice patterns, and unmet needs under daily practice conditions.
While an adequate management of fever was observed in the study, educational measures to avoid the use of mercury thermometers may be needed. Due to the complex etiology of pediatric pain, better evaluation and management of pain in pediatrics is necessary. It is also important that adequate training be provided on pain management within the undergraduate medical curriculum.
Acknowledgments
The authors would like to thank the following physicians, who participated as investigators in this study – from Algeria: Pr Rachida Boukari, Dr Med Salah Djeha, Dr Nadyla Belaltech, Dr Nadiya Djabali ep Hamlaoui, Dr Karima Khabouza, Dr Ahcene Haroun, Dr Chafik Bouchene, Pr Chaouki Kadache, Dr Abdeldjalil Maoudj, Dr Farid Akloul, Dr Rawda Aboura, Dr Rachid Yamoun, Dr Samia Ait Mesbah, Dr Faîza Habbi, Dr Khaled Benyahia, Dr Naima Atif Taibi, Pr Nadia Bensadi, Dr Ismaîl Ali Pacha, and Pr Nacira Cherif; from Argentina: Dr Diego Amaral, Poujade Jorge, Moreno Vivot Eduardo Maria, Capdevila Alejandro, Albores Maria Estella, Agote Luis, Perez Colmegna Veronica, Valverde Gaston, Giglio Norberto, Tamagnini Mariana, Gil Claudia, Alduncin Jose, Botto Eduardo, Giannotti Adrian, Bourguet Solange, Lanoel Diego, Maestro Patricia, Navarra Florencia, and Fernandez Macloughlin Guillermo; from Egypt: Pr Talal Abdel Aziz, Pr Hisham Abdel Hady, Dr Assem Soliman, Pr Adel Naguib, Dr Emad El Shazly, Dr Hatem El Sayed, Dr Ali Abu Zeid, Pr Mohamed El Mazahy, Pr Hamdy Ghazaly, Pr Suzan Samir, Dr Adel Farrag, Dr Onsi Mousa, Dr Hussein Hegab, Dr Medhat El Essely, Dr Osama Edward, Dr Aymen Shasha, Dr Mary Mekhael, Dr Mohamad Talaat, Pr Bothina Abdel Sattar, Dr Mohamed Abdel Mohsen, and Dr Sherif Fam; from Iran: Pr Yaser Mali, Pr Paymaneh Alizadeh Taheri, Pr Asgar Eghbalkhah, Pr Babak Ghalehbaghi, Pr Mohammad Nabavi, Pr Saba Arshi, Pr Behnam Soboti, Pr Mohammad Faranoush, Pr Farid Imanzadeh, Pr Sedigheh Rafiee Tabatabaei, Pr Shahnaz Armin, Pr Ali akbar Sayarri, Pr Alireza Fahimzad, Pr Abdollah Karimi, Pr Darioush Fahimi, Pr Aliakbar Rahbarimanesh, Pr Delara Babaie, and Pr Behrang Tahghvaei; from Lebanon: Dr Bilan Al Yaman, Dr Antoine Harmouche, Dr Jamal Mehfara, Dr Ezzat Sbaity, Dr Antoine Aoudeh, Dr Ahmad Chatila, Dr Mariam Rajab, Dr Marie-Claude Khalifeh, and Dr Ghassan Baassiri; from Mexico: Dr María de la Soledad Calvo González, Dr Alberto Amado Linaldi Camacho, Dr José Omar Peraza Llanes, Dr Mirella Vázquez Rivera, Dr Francisco Javier Pérez Basave, Dr Carlos Leonardo Pérez Zamora, Dr José Inés Guzmán Rodríguez, Dr Eduardo Antonio Reynosa Stenner, Dr Fernando Michel Penichet, Dr Jorge Armando Fonseca Martínez, Dr Nestor Jesús Pulido Barba, Dr Ofelia Ham Mancilla, Dr Susana Guadalupe Rivera Venegas, Dr Cynthia Leticia Saldivar Zúñiga, Dr Sergio Ordóñez Domínguez, Dr José Bartolo López Gutiérrez, Dr Javier Sánchez Nava, Dr Juana Patricia Castro Escobedo, Dr María Elena Villalva Rodríguez, Dr José Rigoberto Canche Fernández, Dr Luz María Eugenia Tamargo Bello, Dr Baltazar Maldonado García, Dr Marco Antonio Batres Medina, Dr Rolando Antonio Salas Mercado, Dr María Teresa Cuevas Zamora, Dr Teresa de Jesús Careaga Vite, and Dr Juan Gabriel Flores Pérez; from Senegal: Dr Clarisse Eva Faye, Dr Lamine Fall, Dr Arame Mbengue Dieye, Dr Maty Diouf Sakho, Dr Amina Bagna, Dr Papa Mactar Faye, Dr Astou Cissé Bathily, Dr Sakaly Berrada, Dr Binetou Tall Thiam, Dr Michel Thiakane, Dr Papa Ibrahima Seye, Dr Madeleine Ndour, Dr Hassane Moussa, Dr Diame Faye, Dr Adama Toure Ly, Dr Liliane Mahou Nicoue, Dr Marieme Soumare Ndiaye, Dr Deogratias Manama, Dr Lamine Thiam, and Dr Phylonella Thiam; from Venezuela: Dr Dorys Ruiz, Dr Damarys Solorzano, Dr Arianne Gonzalez, Dr Antonia Sanchez, Dr Teresa D’Agostino, Dr Zulay Gimenez, Dr Jorge Gaiti, Dr Karolina Lopez, Dr Abraham Abraham, Dr Josefa De Campanaro, Dr Kenia Zambrano, Dr Carmen Pacheco, Dr Fabian Requena, Dr Merly Villarroel, Dr Orlando Delgado, Dr Aura Enriquez, Dr Belen Salinas, Dr Mercedes Materan, Dr Trina Sanchez, and Dr Anelsy Rivero; from Costa Rica: Dr Jorge Martínez, Dr Oscar Segreda, and Dr Priscilla Cordero; from Salvador: Dr Ismael Calderon, Dr Juan Enrique Martínez, Dr Moisés Arevalos, and Dr Maria Luisa Ventura; from Honduras: Dr Ernesto Dala Sierra, and Dr Oscar Banegas; from Panama: Dr Maryuris Patiño, Dr Mariana López, Dr Marisol Troitiño, and Dr Marisela Williams; from Trinidad and Tobago: Dr Lynnette Welch and Dr Jameel Mohamed. The authors would also like to thank Thomas Rohban, MD (Partner 4 Health, France) for providing medical writing support in accordance with Good Publication Practice (GPP3) guidelines. This study was funded by Sanofi.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
All authors, except MMA, were investigators on this clinical trial and received honoraria to participate in the study phase. There were no honoraria related to the publication itself. MMA is a Sanofi employee. The authors report no other conflicts of interest in this work.
References
- 1.King S, Chambers CT, Huguet A, et al. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. 2011;152(12):2729–2738. doi: 10.1016/j.pain.2011.07.016 [DOI] [PubMed] [Google Scholar]
- 2.Mathews L. Pain in children: neglected, unaddressed and mismanaged. Indian J Palliat Care. 2011;17(Suppl):S70–S73. doi: 10.4103/0973-1075.76247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goodman JE, McGrath PJ. The epidemiology of pain in children and adolescents: a review. Pain. 1991;46(3):247–264. [DOI] [PubMed] [Google Scholar]
- 4.American Academy of Pediatrics. Committee on Psychosocial Aspects of Child and Family Health; Task Force on Pain in Infants, Children, and Adolescents. The assessment and management of acute pain in infants, children, and adolescents. Pediatrics. 2001;108(3):793–797. doi: 10.1542/peds.108.3.793 [DOI] [PubMed] [Google Scholar]
- 5.Page MG, Stinson J, Campbell F, Isaac L, Katz J. Pain-related psychological correlates of pediatric acute post-surgical pain. J Pain Res. 2012;5:547–558. doi: 10.2147/JPR.S36614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cassel EJ. The nature of suffering and the goals of medicine. N Engl J Med. 1982;306(11):639–645. doi: 10.1056/NEJM198203183061104 [DOI] [PubMed] [Google Scholar]
- 7.Holm S, Ljungman G, Soderlund A. Pain in children and adolescents in primary care; chronic and recurrent pain is common. Acta Paediatr. 2012;101(12):1246–1252. doi: 10.1111/j.1651-2227.2012.02829.x [DOI] [PubMed] [Google Scholar]
- 8.Anand KJ, Scalzo FM. Can adverse neonatal experiences alter brain development and subsequent behavior? Biol Neonate. 2000;77(2):69–82. doi: 10.1159/000014197 [DOI] [PubMed] [Google Scholar]
- 9.Lynch-Jordan AM, Kashikar-Zuck S, Szabova A, Goldschneider KR. The interplay of parent and adolescent catastrophizing and its impact on adolescents’ pain, functioning, and pain behavior. Clin J Pain. 2013;29(8):681–688. doi: 10.1097/AJP.0b013e3182757720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Phillips DM. JCAHO pain management standards are unveiled. Joint Commission on Accreditation of Healthcare Organizations. JAMA. 2000;284(4):428–429. [DOI] [PubMed] [Google Scholar]
- 11.Fortier MA, MacLaren JE, Martin SR, Perret-Karimi D, Kain ZN. Pediatric pain after ambulatory surgery: where’s the medication? Pediatrics. 2009;124(4):e588–e595. doi: 10.1542/peds.2008-3529 [DOI] [PubMed] [Google Scholar]
- 12.Anand KJ. Consensus statement for the prevention and management of pain in the newborn. Arch Pediatr Adolesc Med. 2001;155(2):173–180. [DOI] [PubMed] [Google Scholar]
- 13.Wright PF, Thompson J, McKee KT Jr, Vaughn WK, Sell SH, Karzon DT. Patterns of illness in the highly febrile young child: epidemiologic, clinical, and laboratory correlates. Pediatrics. 1981;67(5):694–700. [PubMed] [Google Scholar]
- 14.Eskerud JR, Laerum E, Fagerthun H, Lunde PK, Naess A. Fever in general practice. I. Frequency and diagnoses. Fam Pract. 1992;9(3):263–269. doi: 10.1093/fampra/9.3.263 [DOI] [PubMed] [Google Scholar]
- 15.Finkelstein JA, Christiansen CL, Platt R. Fever in pediatric primary care: occurrence, management, and outcomes. Pediatrics. 2000;105(1 Pt 3):260–266. [PubMed] [Google Scholar]
- 16.Sullivan JE, Farrar HC, Sullivan JE, Farrar HC. Fever and antipyretic use in children. Pediatrics. 2011;127(3):580–587. doi: 10.1542/peds.2010-3852 [DOI] [PubMed] [Google Scholar]
- 17.Wallenstein MB, Schroeder AR, Hole MK, et al. Fever literacy and fever phobia. Clin Pediatr (Phila). 2013;52(3):254–259. doi: 10.1177/0009922812472252 [DOI] [PubMed] [Google Scholar]
- 18.Crocetti M, Moghbeli N, Serwint J. Fever phobia revisited: have parental misconceptions about fever changed in 20 years? Pediatrics. 2001;107(6):1241–1246. doi: 10.1542/peds.107.6.1241 [DOI] [PubMed] [Google Scholar]
- 19.Purssell E. Treatment of fever and over-the-counter medicines. Arch Dis Child. 2007;92(10):900–901. doi: 10.1136/adc.2007.118810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van den Anker JN. Optimising the management of fever and pain in children. Int J Clin Pract Suppl. 2013;67(178):26–32. doi: 10.1111/ijcp.12056 [DOI] [PubMed] [Google Scholar]
- 21.Baraff LJ. Management of infants and young children with fever without source. Pediatr Ann. 2008;37(10):673–679. [DOI] [PubMed] [Google Scholar]
- 22.Blumenthal I. Should we ban the mercury thermometer? Discussion paper. J R Soc Med. 1992;85(9):553–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Axelrod P. External cooling in the management of fever. Clin Infect Dis. 2000;31(Suppl 5):S224–S229. doi: 10.1086/317516 [DOI] [PubMed] [Google Scholar]
- 24.Sherman JM, Sood SK. Current challenges in the diagnosis and management of fever. Curr Opin Pediatr. 2012;24(3):400–406. doi: 10.1097/MOP.0b013e32835333e3 [DOI] [PubMed] [Google Scholar]
- 25.American Medical Association. Module 6 pain management: pediatric pain management; 2012. Available from: http://files.sld.cu/anestesiologia/files/2012/01/pediatric-pain-management.pdf. Accessed December22, 2018.
- 26.Berde CB, Sethna NF. Analgesics for the treatment of pain in children. N Engl J Med. 2002;347(14):1094–1103. doi: 10.1056/NEJMra012626 [DOI] [PubMed] [Google Scholar]
- 27.Srouji R, Ratnapalan S, Schneeweiss S. Pain in children: assessment and nonpharmacological management. Int J Pediatr. 2010;2010 pii: 474838. doi: 10.1155/2010/474838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McGrath PJ, Frager G. Psychological barriers to optimal pain management in infants and children. Clin J Pain. 1996;12(2):135–141. [DOI] [PubMed] [Google Scholar]
- 29.Sandler AN. Acute pain–guidelines for care. Can J Anaesth. 1997;44(5 Pt 2):R137–R145. [DOI] [PubMed] [Google Scholar]
- 30.Twycross A. Why managing pain in children matters In: Dowden SJ, Bruce E, editors. Managing Pain in Children. United Kingdom: Wiley-Blackwell; 2009:1–15. [Google Scholar]
- 31.Zeltzer LK, Altman A, Cohen D, LeBaron S, Munuksela EL, Schechter NL. American Academy of Pediatrics report of the subcommittee on the management of pain associated with procedures in children with cancer. Pediatrics. 1990;86(5 Pt 2):826–831. [PubMed] [Google Scholar]
- 32.Wente SJ. Nonpharmacologic pediatric pain management in emergency departments: a systematic review of the literature. J Emerg Nurs. 2013;39(2):140–150. doi: 10.1016/j.jen.2012.09.011 [DOI] [PubMed] [Google Scholar]
- 33.Bandstra NF, Skinner L, Leblanc C, et al. The role of child life in pediatric pain management: a survey of child life specialists. J Pain. 2008;9(4):320–329. doi: 10.1016/j.jpain.2007.11.004 [DOI] [PubMed] [Google Scholar]
- 34.Walker SM. Pain in children: recent advances and ongoing challenges. Br J Anaesth. 2008;101(1):101–110. doi: 10.1093/bja/aen097 [DOI] [PubMed] [Google Scholar]
- 35.Allegaert K, Tibboel D, Naulaers G, et al. Systematic evaluation of pain in neonates: effect on the number of intravenous analgesics prescribed. Eur J Clin Pharmacol. 2003;59(2):87–90. doi: 10.1007/s00228-003-0585-3 [DOI] [PubMed] [Google Scholar]
- 36.Chidambaran V, Sadhasivam S. Pediatric acute and surgical pain management: recent advances and future perspectives. Int Anesthesiol Clin. 2012;50(4):66–82. doi: 10.1097/AIA.0b013e31826f3284 [DOI] [PubMed] [Google Scholar]