Abstract
Objective
To examine the dose-response associations between accelerometer assessed total physical activity, different intensities of physical activity, and sedentary time and all cause mortality.
Design
Systematic review and harmonised meta-analysis.
Data sources
PubMed, PsycINFO, Embase, Web of Science, Sport Discus from inception to 31 July 2018.
Eligibility criteria
Prospective cohort studies assessing physical activity and sedentary time by accelerometry and associations with all cause mortality and reported effect estimates as hazard ratios, odds ratios, or relative risks with 95% confidence intervals.
Data extraction and analysis
Guidelines for meta-analyses and systematic reviews for observational studies and PRISMA guidelines were followed. Two authors independently screened the titles and abstracts. One author performed a full text review and another extracted the data. Two authors independently assessed the risk of bias. Individual level participant data were harmonised and analysed at study level. Data on physical activity were categorised by quarters at study level, and study specific associations with all cause mortality were analysed using Cox proportional hazards regression analyses. Study specific results were summarised using random effects meta-analysis.
Main outcome measure
All cause mortality.
Results
39 studies were retrieved for full text review; 10 were eligible for inclusion, three were excluded owing to harmonisation challenges (eg, wrist placement of the accelerometer), and one study did not participate. Two additional studies with unpublished mortality data were also included. Thus, individual level data from eight studies (n=36 383; mean age 62.6 years; 72.8% women), with median follow-up of 5.8 years (range 3.0-14.5 years) and 2149 (5.9%) deaths were analysed. Any physical activity, regardless of intensity, was associated with lower risk of mortality, with a non-linear dose-response. Hazards ratios for mortality were 1.00 (referent) in the first quarter (least active), 0.48 (95% confidence interval 0.43 to 0.54) in the second quarter, 0.34 (0.26 to 0.45) in the third quarter, and 0.27 (0.23 to 0.32) in the fourth quarter (most active). Corresponding hazards ratios for light physical activity were 1.00, 0.60 (0.54 to 0.68), 0.44 (0.38 to 0.51), and 0.38 (0.28 to 0.51), and for moderate-to-vigorous physical activity were 1.00, 0.64 (0.55 to 0.74), 0.55 (0.40 to 0.74), and 0.52 (0.43 to 0.61). For sedentary time, hazards ratios were 1.00 (referent; least sedentary), 1.28 (1.09 to 1.51), 1.71 (1.36 to 2.15), and 2.63 (1.94 to 3.56).
Conclusion
Higher levels of total physical activity, at any intensity, and less time spent sedentary, are associated with substantially reduced risk for premature mortality, with evidence of a non-linear dose-response pattern in middle aged and older adults.
Systematic review registration
PROSPERO CRD42018091808.
Introduction
Physical inactivity is associated with many chronic diseases,1 premature mortality,2 and substantial economic burden.3 Increasing evidence also suggests that high levels of time spent sedentary might increase the risk of chronic diseases and mortality.4 5
The current evidence on the associations between physical activity or sedentary time and health outcomes are primarily from studies that used participant self reported physical activity and sedentary time.1 Self reports are, however, prone to recall and social desirability biases, which result in over-estimation of physical activity,6 7 are usually restricted to a limited number of physical activity domains (eg, leisure time activity), underestimate sedentary time,8 and rarely provide data on total physical activity and light physical activity.7 Furthermore, the magnitude of the association between physical activity and mortality is likely underestimated, as a result of imprecision in exposure measurements, whereas the shape of the dose-response associations for light intensity physical activity is unclear. Indeed, the US Physical Activity Guidelines advisory committee recently indicated the impact of total physical activity and light intensity physical activity for reducing mortality risk as a priority for research.1
To reduce the biases associated with self report, several recent cohort studies have used device based methods (ie, accelerometry) when examining associations between physical activity or sedentary time and mortality.9 10 11 12 13 However, the results are inconsistent, even when derived from the same dataset.13 14 This is related to differences in analytical methods. Also, most of these studies are statistically underpowered to examine the associations between dose-response and intensity specific physical activity and mortality because of their relatively short follow-up time and few deaths.
We conducted a harmonised meta-analysis to examine the association between accelerometer measured physical activity and sedentary time and all cause mortality. Specifically, we examined the dose-response relations of total physical activity, different intensities of physical activity (light, low light, high light, moderate to vigorous, and vigorous) and sedentary time and all cause mortality.
Methods
We conducted a systematic review following the guidelines for Meta-Analyses and Systematic reviews for Observational Studies15 and the PRISMA guidelines.16 The review protocol is registered with the PROSPERO database (CRD42018091808).
Data sources
We performed a systematic search in five databases (PubMed, PsycINFO, Embase, Web of Science, Sport Discus) from inception of the database to 31 July 2018. When searching for eligible articles we used the search terms (“physical activity” or “physical activities” or “physically active” or “physical exercise” or “exercise” or “walk” and “mortality” or “mortalities” or” death “or “fatal” or “accelerometer” or “activity monitor” or “motion sensor” or “device-based” or “Actigraph” or “Actical” or “Sensewear” or “Actiband” or “Actiwatch”). Forward and backwards tracking was performed by examining the reference list of studies potentially eligible for inclusion.
Study selection
Two authors (UE, JSS) independently screened the titles and abstracts. After exclusion of duplicates, one author (JSS) performed a full text review, and the final list of studies was discussed among the writing group. Inclusion criteria were prospective cohort studies that assessed sedentary time and physical activity by accelerometry, had data on individual level exposure and all cause mortality, reported effect estimates as hazard ratios, odds ratios, or relative risks with 95% confidence intervals for all cause mortality, and were published in English or Scandinavian. Owing to the noticeable variations in output from accelerometers placed at different body sites,17 which precludes harmonisation of physical activity data, we excluded three studies18 19 20 in which physical activity was assessed by monitors placed on the upper arm, wrist, and thigh. On author request one eligible study was not included in the harmonised meta-analysis.11
Data extraction
One author (UE) extracted the following information from each eligible study: name of first author, study location, and number of participants, age of participants, number of each sex, years of follow-up, number of deaths from all causes, methods of case ascertainment, assessment details for physical activity and sedentary time, and covariates included in final, adjusted models. Another author (JSS) cross checked data extraction variables.
Risk of bias
Using the Newcastle Ottawa quality assessment scale,21 two authors (UE, JT) independently assessed the studies and resolved disagreements by consensus. This semiquantitative scale uses a star system to assess the quality for eight items across three domains (selection, comparability, and exposure), with a maximum of one star for each item for high quality studies except for the comparability domain (two stars). Thus the total score ranges from 0 to 9. Supplementary table 2 provides further details of the quality rating.
Data synthesis and harmonisation of exposure variables
We contacted the corresponding author from each of the identified studies and asked whether he or she would be willing to contribute to a harmonised meta-analysis. To reduce heterogeneity in data cleaning and processing of accelerometer data among studies, authors of the studies reprocessed their individual participant data according to our standardised protocol. Data from the vertical acceleration axis in 60 second epochs were extracted, and we defined non-wear time as 90 consecutive minutes of 0 counts per minute (cpm), allowing up to a two minute interval of non-zero cpm if the interruption was accompanied by 30 consecutive minutes of 0 cpm either upstream or downstream.22 We included all participants who recorded a wear time of 10 or more hours each day for four or more days.23
Each study computed several exposure variables from accelerometer measurements: total volume of physical activity (total counts/wear time in minutes, cpm); time (min/day) spent in six intensity specific variables (sedentary, ≤100 cpm,24 light, 101-1951 cpm,25 low light, 101-759 cpm,13 high light, 760-1951 cpm,13 moderate to vigorous, ≥1952 cpm,25 vigorous, ≥5725cpm25; bouts of moderate-to-vigorous intensity physical activity, defined as 10 or more minutes of consecutive accelerometer readings ≥1952 cpm allowing for 1-2 minute drops below the threshold during each period of 10 or more minutes. For two studies9 26 that assessed physical activity using the Actical accelerometer, the same wear time criteria as previously described were used and physical activity intensity thresholds computed according to previous validation studies27 28: sedentary, ≤100 cpm; light, 101-1534 cpm; low light, 101-599 cpm; high light, 600-1534 cpm; moderate to vigorous >1535 cpm; and vigorous ≥3960 cpm.
Analyses
Participating studies conducted several study specific analyses to examine the associations between exposure variables with all cause mortality using Cox proportional hazards regression analyses (hazard ratios and 95% confidence intervals) restricted to participants aged 40 or more years. Exposure data were categorised into quarters, with the first quarter (least active) as referent. Associations between physical activity variables with mortality were analysed with several levels of adjustment: model A (adjusting for wear time (except cpm, as wear time is included in this calculation), sex (if applicable), and age); model B (model A+adjustment for socioeconomic status and body mass index (BMI) and mutual adjustment of sedentary time and moderate-to-vigorous-intensity physical activity); and model C (model B+adjustment for covariates included in the study’s final adjusted model, as listed in table 1). Mortality data from two studies9 12 were updated from their publication follow-up before analyses. Owing to different data processing criteria the numbers of participants and deaths slightly differ from those previously published. Before the analyses, we accounted for the sample weights and complex survey design of the National Health and Nutrition Examination Survey (NHANES).29
Table 1.
Characteristics of studies included in the meta-analysis
| Publication | Study; location; No of participants; No of cases | Year of baseline assessment; mean follow-up | Case ascertainment | Accelerometer type (location) | Covariates | Quality assessment* |
|---|---|---|---|---|---|---|
| Bakrania et al36 | Walking Away from Type 2 Diabetes (WAT2D), England; n=654 (411 men, 243 women); 26 cases | 2010-11; 5.7 years | Office for National Statistics | Actigraph GT3X+ (right hip) | Age, sex, BMI, socioeconomic status | 8 |
| Diaz et al9 | Reasons for Geographic and Racial Differences in Stroke (REGARDS); US; n=7862 (3580 men; 4282 women); 590 cases | 2003-07; 5.3 years | Review of death certificates, medical records, and administrative databases | Actical (right hip) | Age, sex, BMI, education, race, region of residence, season the accelerometer was worn, current smoking, alcohol use, diabetes, hypertension, dyslipidemia, estimated glomerular filtration rate, atrial fibrillation, history of coronary heart disease, and history of stroke | 9 |
| Dohrn et al10 | Sweden Attitude Behaviour and Change study (ABC), Sweden; n=834 (371 men, 463 women); 79 cases | 2001-02; 14.5 years | National death register | Actigraph 7164 (lower back) | Age, sex, education, BMI, smoking, history of hypertension, heart disease, cancer, and diabetes | 9 |
| Jefferis et al37 | British Regional Heart Study (BRHS), UK; n=1412 men; 250 cases | 2010-12; 6.0 years | National Health Service central registers | Actigraph GT3X+ (right hip) | Age, BMI, Social class, season of accelerometer wear, region of residence, lives alone / with others, alcohol, smoking, sleep, locomotor disability, previous MI, stroke or heart failure | 9 |
| Lee et al12 | Women’s Health Study (WHS), US; n=16738, women; n=504 | 2011-17; 4.3 years | Medical records, death certificates, or National Death Index | Actigraph GT3X+ (right hip) | Age, income, BMI, smoking; alcohol; intakes of saturated fat, fibre, fruits, and vegetables; hormone therapy; parental history of myocardial infarction; family history of cancer; general health; history of cardiovascular disease; history of cancer; and cancer screening | 9 |
| Unpublished data (Murabito et al26) | Framingham Heart Study (FHS), US; n=2621 (1225 men, 1396 women); 77 cases | 2008-11; 4.0 years | Medical records, death certificates | Actical (right hip) | Age, sex, education, BMI, ethnicity, smoking, self reported health | 9 |
| NHANES13 (data downloaded from wwwn.cdc.gov/nchs/nhanes/Default.aspx and Public-use Linked Mortality data† | National Health and Nutrition Examination Survey (NHANES), US;(n=3978 (1977 men, 2001 women); 492 cases | 2003-06; 6.5 years | National Death Index, National Center for Health Statistics | Actigraph 7164 (right hip) | Age, socioeconomic status, BMI, ethnicity, smoking, alcohol, mobility limitations, number of medical conditions (diabetes, congestive heart failure, coronary heart disease, angina pectoris, heart attack, stroke, cancer) | 9 |
| Unpublished data (Hansen et al35) | Norwegian National Physical Activity Survey 1 (NNPAS), Norway; n=2284; 131 cases | 2008-09; 8.9 years | Death certificates, Norwegian death register | Actigraph GT1M (right hip) | Age, sex, education, BMI, wear time, smoking, alcohol, number of medical conditions | 9 |
BMI=body mass index.
Quality assessment according to Newcastle-Ottawa scale (range 0-9) for cohort studies (see supplementary material for further details).
National Center for Health Statistics. Office of Analysis and Epidemiology, Public-use Linked Mortality File, 2015. Hyattsville, MD, USA (www.cdc.gov/nchs/data_access/data_linkage/mortality.htm).
Individual study summary data were meta-analysed with a random effects model yielding three pooled hazard ratios with 95% confidence intervals (first quarter as referent versus second to fourth quarters) in each model. We used model B as our primary model. For two variables, moderate-to-vigorous intensity physical activity in bouts and vigorous intensity physical activity, we included all participants who recorded zero minutes in the referent group, and we categorised the remaining participants into thirds.
Based on the individual studies log transformed hazard ratios for each of the quarters in model B, we described the underlying dose-response associations with sedentary time, total physical activity, and intensity specific activity using a restricted cubic spline model to allow for potential non-linearity.30 We prespecified three knots at the 25th, 50th, and 75th centiles of the exposure variable distributions using the medians of the quarters to define the exposure levels (supplementary table 8, and see fig 2). We accounted for non-zero referent groups by centring the exposure levels.31 Departure from linearity was assessed by a Wald test examining the null hypothesis that the coefficient of the second spline was equal to zero.32 Model fit was examined visually using de-correlated residuals-versus-exposure plots and by the coefficient of determination.33 Data from two studies that assessed physical activity by the Actical accelerometer9 26 were only included for time spent in moderate-to-vigorous intensity physical activity for the dose-response analyses because of the noticeable difference in absolute output for the other exposure variables compared with the Actigraph accelerometer.34
In sensitivity analyses, we excluded deaths within the first two years of follow-up and reanalysed the data according to model B. We reanalysed data for total physical activity (cpm) excluding the two studies9 26 in which physical activity was measured by a different type of accelerometer than used in the other studies. We also reanalysed the data excluding the two studies in which data on the association between physical activity and mortality had not been previously published.26 35 We reanalysed our data and estimated summary hazard ratios across studies with fixed effects inverse variance method, and the main findings were unchanged (data not shown). We assessed heterogeneity by I2 statistics. Finally, to assess possible publication bias we created funnel plots for the individual study hazard ratios, comparing extreme exposure quarters and calculated the Egger’s test for funnel plot symmetry. Meta-analyses were performed using Matlab (R2014a, Mathworks, Natick, MA).
Patient and public involvement
No patients were involved in the planning, design, or research idea for this systematic review. Nor were they involved in the analyses or data collection for the work. We did not evaluate whether the individual studies included in the review had any patient involvement. The results from the present study will be disseminated through the institutional websites and press releases.
Results
Overall, 39 of 518 identified articles were retrieved for full text review. Ten were eligible for inclusion, three were excluded owing to harmonisation challenges (ie. monitor placements), and one study did not participate, leaving six for inclusion (fig 1).9 10 12 13 36 37 Data were publicly available from one of the identified studies13 and data were obtained from a further two studies with pertinent data available.26 35
Fig 1.
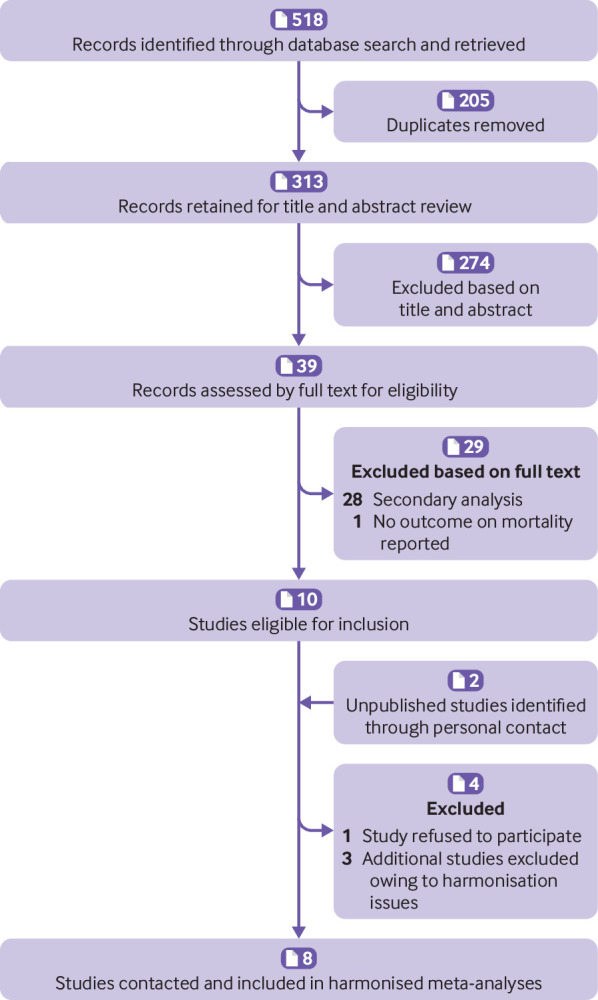
Study selection
Thus individual level data from eight studies, of which three were from nationally representative surveillance systems10 13 35 including 36 383 participants (mean age 62.6 years; 72.8% women) with a median follow-up time of 5.8 years (mean 6.7 years, range 3.0-14.5 years, 243 766 person years) were included in the meta-analyses. During follow-up, 2149 (5.9%) participants died. Table 1 summarises the characteristics of studies (participant characteristics by study are presented in supplementary table 1). The quality scores were high, at 8 or 9 (table 1 and supplementary table 2).
Compared with the referent, any level of physical activity regardless of intensity was associated with a substantially lower risk of mortality (table 2, supplementary figs 1a-f). The magnitude of lowered risk was most pronounced for total physical activity; hazard ratios (95% confidence intervals) for increasing quarter were: 1.00 (referent, least active), 0.48 (0.43 to 0.54), 0.34 (0.26 to 0.45), and 0.27 (0.23 to 0.32) (table 2, model B, supplementary fig 1a). Higher levels of light intensity physical activity, as well as low and high light intensity physical activity were also associated with substantially reduced risks of death during follow-up. The risk reductions were most pronounced when the second quarter was compared against the referent for all levels of adjustment (table 2, fig 2). For example, the risk was reduced to 0.55 (0.49 to 0.63) in the second quarter for high light intensity physical activity and additionally reduced in the third (0.38, 0.30 to 0.48) and fourth (0.37, 0.32 to 0.46) quarters compared with the referent (table 2, model B). Higher levels of moderate-to-vigorous intensity physical activity were also associated with a reduced risk of death even after adjustment for sedentary time (table 2, models B and C; fig 2). The risk of death increased with increasing time spent sedentary; hazard ratios for increasing quarters were: 1.00 (referent), 1.28 (1.09 to 1.51), 1.71 (1.36 to 2.15), and 2.63 (1.94 to 3.56) after adjustment for age, sex, BMI, socioeconomic status, wear time, and time spent in moderate-to-vigorous intensity physical activity (table 2, models B and C; fig 2).
Table 2.
Meta-analysis for associations between total physical activity, intensities of physical activity or sedentary time by quarters and all cause mortality
| Variables | Hazard ratios (95% CI) for all cause mortality*; No of participants; No of deaths | |||
|---|---|---|---|---|
| First quarter (least active) | Second quarter | Third quarter | Fourth quarter (most active) | |
| Model A | ||||
| Total physical activity (cpm) | 1 (ref) (n=9189; 1301) | 0.47 (0.42 to 0.53) (n=9225; 506) | 0.35 (0.26 to 0.47) (n=9207; 277) | 0.28 (0.22 to 0.34) (n=9231; 220) |
| Physical activity intensity: | ||||
| Light (min/d) | 1 (ref) (n=9191; 1188) | 0.58 (0.52 to 0.64) (n=9214; 547) | 0.42 (0.36 to 0.43) (n=9212; 332) | 0.36 (0.28 to 0.46) (n=9235; 237) |
| Low light (min/d) | 1 (ref) (n=9182; 1100) | 0.64 (0.57 to 0.72) (n=9224; 552) | 0.46 (0.38 to 0.56) (n=9229; 376) | 0.41 (0.35 to 0.50) (n=9217; 276) |
| High light (min/d) | 1 (ref) (n=9166; 1261) | 0.53 (0.47 to 0.60) (n=9241; 517) | 0.36 (0.31 to 0.42) (n=9207; 290) | 0.36 (0.25 to 0.51) (n=9227; 236) |
| Moderate to vigorous (min/d) | 1 (ref) (n=9095; 1221) | 0.54 (0.48 to 0.60) (n=9296; 525) | 0.40 (0.29 to 0.56) (n=9235; 311) | 0.35 (0.28 to 0.44) (n=9226; 247) |
| Sedentary (min/d) | 1 (ref) (n=9219; 339) | 1.32 (1.14 to 1.54) (n=9223; 432) | 1.97 (1.69 to 2.30) (n=9201; 598) | 3.22 (2.49 to 4.15) (n=9190; 935) |
| Model B† | ||||
| Total physical activity (cpm) | 1 (ref) (n=9096; 1187) | 0.48 (0.43 to 0.54) (n=9105, 483) | 0.34 (0.26 to 0.45) (n=9096, 265) | 0.27 (0.23 to 0.32) (n=9086, 214) |
| Physical activity intensity: | ||||
| Light (min/d) | 1 (ref) (n=9073; 1089) | 0.60 (0.54 to 0.68) (n=9101; 511) | 0.44 (0.38 to 0.51) (n=9090; 320) | 0.38 (0.28 to 0.51) (n=9119; 229) |
| Low light (min/d) | 1 (ref) (n=9066; 1010) | 0.66 (0.56 to 0.77) (n=9106; 518) | 0.47 (0.38 to 0.58) (n=9112; 353) | 0.42 (0.34 to 0.52) (n=9099; 268) |
| High light (min/d) | 1 (ref) (n=9054; 1159) | 0.55 (0.49 to 0.63) (n=9120; 483) | 0.38 (0.30 to 0.48) (n=9088; 278) | 0.37 (0.32 to 0.46) (n=9113; 229) |
| Moderate to vigorous (min/d) | 1 (ref) (n=9002; 1139) | 0.64 (0.55 to 0.74) (n=9153; 468) | 0.55 (0.40 to 0.74) (n=9123; 305) | 0.52 (0.43 to 0.61) (n=9105; 237) |
| Sedentary (min/d) | 1 (ref) (n=9102; 327) | 1.28 (1.09 to 1.51) n=9105; 417) | 1.71 (1.36 to 2.15) (n=9096; 562) | 2.63 (1.94 to 3.56) (n=9080; 843) |
| Model C† | ||||
| Total physical activity (cpm) | 1 (ref) (n=8971; 1122) | 0.54 (0.48 to 0.61) (n=9004; 458) | 0.41 (0.32 to 0.51) (n=8972; 259) | 0.34 (0.29 to 0.41) (n=8985; 208) |
| Physical activity intensity: | ||||
| Light (min/d) | 1 (ref) (n=8944; 1030) | 0.66 (0.58 to 0.74) (n=8979; 485) | 0.51 (0.44 to 0.57) (n=8992; 308) | 0.44 (0.34 to 0.59) (n=9017; 224) |
| Low light (min/d) | 1 (ref) (n=8939; 959) | 0.70 (0.62 to 0.79) (n=8997; 490) | 0.54 (0.48 to 0.63) (n=8999; 338) | 0.48 (0.40 to 0.57) (n=8997; 260) |
| High light (min/d) | 1 (ref) (n=8919; 1086) | 0.63 (0.56 to 0.71) (n=8990; 467) | 0.46 (0.39 to 0.54) (n=8985; 269) | 0.45 (0.31 to 0.65) (n=9028; 225) |
| Moderate to vigorous (min/d) | 1 (ref) (n=8875; 1077) | 0.69 (0.58 to 0.81) (n=9041; 441) | 0.62 (0.48 to 0.80) (n=9009; 297) | 0.61 (0.50 to 0.75) (n=9007; 232) |
| Sedentary (min/d) | 1 (ref) (n=9001; 317) | 1.21 (1.02 to 1.42) (n=9006; 403) | 1.56 (1.24 to 1.98) (n=8969; 536) | 2.18 (1.61 to 2.95) (n=8956; 791) |
cpm=counts per minute.
Model A adjusted for sex (when applicable), age, and wear time (n=36852, 2304 deaths). Model B adjusted for sex (when applicable), age, body mass index, socioeconomic position, and wear time (n=36383, 2149 deaths). Model C additionally adjusted for covariates listed in table 1 (n=35 932, 2047 deaths).
By Cox regression.
Moderate-to-vigorous physical activity and sedentary time are mutually adjusted.
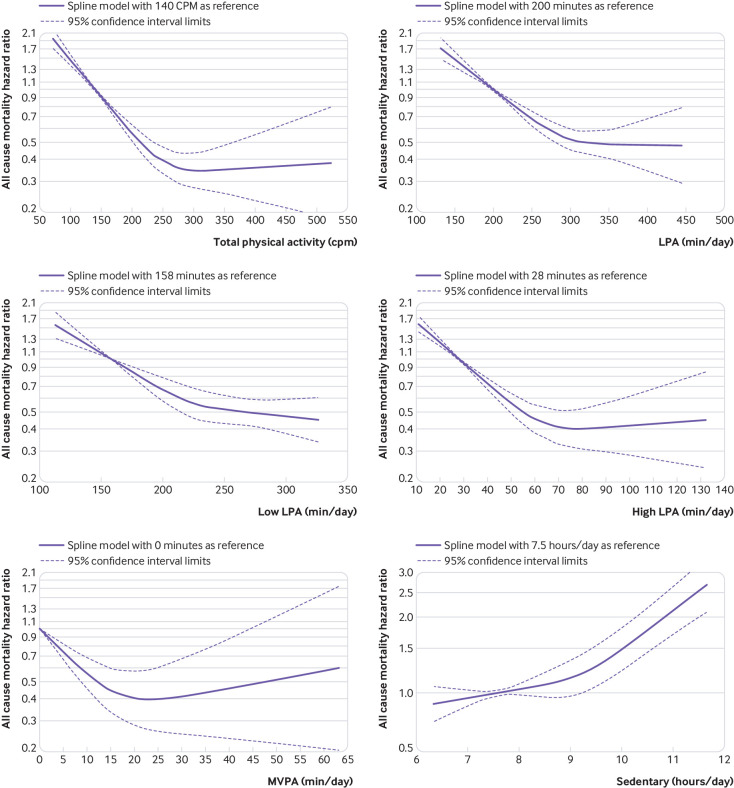
Fig 2.
Dose-response associations between total physical activity (top left), light intensity physical activity (LPA) (top right), low LPA (middle left), high LPA (middle right), moderate-to-vigorous intensity physical activity (MVPA) (bottom left), and sedentary time (bottom right, data from REGARDS (Reasons for Geographic and Racial Differences in Stroke)9 and FHS (Women’s Health Study)12 are only included for MVPA) and all cause mortality. Modelling performed using restricted cubic splines with knots at 25th, 50th, and 75th centiles of exposure specific distribution from medians of quarters (least to most active). The exposure reference is set as the median of the medians in the reference group (least active) (see supplementary table 3). Knot locations are available in supplementary table 8. cpm=counts per minute
The differences in physical activity and sedentary time (min/day) between the referent and the second quarter were broadly equal to 60 min/day of light intensity physical activity, 35 min/day of low light intensity physical activity, 25 min/day of high light intensity physical activity, 5 min/day of moderate-to-vigorous intensity physical activity, and 70 min/day of sedentary time (supplementary table 3).
Higher levels of bouts of moderate-to-vigorous intensity physical activity and any vigorous intensity physical activity were also associated with reduced risk of mortality (supplementary table 4). However, low numbers of participants undertook physical activity in bouts of moderate-to-vigorous physical activity or in any vigorous physical activity (supplementary table 4), potentially making these estimates less reliable.
We observed non-linear, dose-response associations (P values from the second spline <0.02 for each exposure variable) for the associations between all exposure variables and mortality (fig 2, supplementary table 5). The maximal risk reduction for total physical activity (hazard ratio 0.34, 95% confidence interval 0.27 to 0.43) was observed at about 300 cpm. Maximal risk reductions for light intensity physical activity (0.48, 0.38 to 0.63), low light intensity physical activity (0.45, 0.34 to 0.60), high light intensity physical activity (0.40, 0.31 to 0.52), and moderate-to-vigorous intensity physical activity (0.39, 0.26 to 0.59) were observed at about 375 min/day, 325 min/day, 80 min/day, and 24 min/day, respectively. No further risk reductions occurred with higher levels of activity except for low light intensity physical activity where the risk appeared to decrease further (supplementary table 5).
The dose-response relations between sedentary time and mortality increased gradually from about 7.5 to 9 hours and were more pronounced at greater than 9.5 hours (fig 2, supplementary table 5). Ten and 12 hours each day spent sedentary were associated with 1.48 (1.22 to 1.79) and 2.92 (2.24 to 3.83) higher risk of death, respectively.
The results did not appreciably change when excluding deaths within the first two years of follow-up, except for a small attenuation for the association between sedentary time and mortality (supplementary table 6). Similarly, sensitivity analyses excluding the two studies in which physical activity was assessed by a different monitor did not change the results (supplementary table 7). There was no evidence of publication bias; however, the plots should be interpreted cautiously owing to the small number of studies (supplementary figs 2 and 3).
Discussion
Higher levels of total physical activity at any intensity and less time spent sedentary are associated with a substantially reduced risk for premature mortality, with evidence of a non-linear dose-response pattern in middle aged and older adults. Our observations on the associations between accelerometry measured physical activity or sedentary time and all cause mortality provide important data for informing public health recommendations. Firstly, they reinforce the non-linear, dose-response relation but with considerably larger effect sizes than in studies using self reports. Secondly, the total volume of physical activity, irrespective of intensity, is associated with a substantially reduced risk of death during follow-up. Thirdly, the greatest risk reduction for mortality was observed when the second quarter was compared with the referent, for all activity intensities. Fourthly, maximal risk reductions were seen at about 375 min/day of light intensity physical activity or 24 min/day of moderate-to-vigorous intensity physical activity. Fifthly, a statistically significantly higher risk of death was observed from 9.5 or more hours per day for time spent sedentary.
Strengths and limitations of this study
Our meta-analysis has several strengths. Physical activity and sedentary time were measured using accelerometry, and all individual participant data were reanalysed in a harmonised manner. Device based measures of sedentary time and physical activity are less prone to biases usually associated with self report. However, interpreting associations with physical activity assessed by devices across studies is challenging because of variations in processing data collected from devices. Our harmonised approach substantially reduced heterogeneity among studies by applying a common and standardised definition of wear time, inclusion criteria, and definitions of thresholds for physical activity intensity and sedentary time. Furthermore, the large sample size allowed meta-analyses of the dose-response relations between various intensities of physical activity, including low and high light, and all cause mortality, as well as providing more precise results with narrower confidence intervals than in previous studies. Finally, we defined the absolute amount of time associated with maximal risk reduction for all cause mortality for different levels of physical activity intensity and identified a threshold for sedentary time where the risk of death increased more rapidly, based on the shape of the curve for the dose-response association.
This study also has some limitations. All studies were conducted in the US and western Europe limiting generalisability beyond these populations. All study data were analysed with men and women combined and after adjustment for sex. Thus we cannot exclude different associations between sexes; however, the results from the two studies of men and women separately12 37 are in agreement, suggesting the observed associations are similar. Residual confounding might exist, although the studies adjusted their analyses for several covariates (often including pre-existing illness, mobility limitations; all studies adjusted for smoking) in the final model and results were similar to those from the primary model, including sex, age, BMI, socioeconomic status, and wear time. We attempted to minimise bias from reverse causation by excluding all deaths within the first two years in sensitivity analyses. The hazard ratios were materially unchanged for the associations of total physical activity and light intensity or moderate-to-vigorous intensity physical activity with mortality, and slightly attenuated for sedentary time. However, bias from reverse causation might persist.38 All studies in our analysis included middle aged and older adults who were at least 40 years old; it is unclear whether the estimates of the absolute physical activity levels associated with maximal risk reduction apply to younger people. For the purposes of harmonisation, only data recorded from a single (vertical) axis were analysed; this tends to detect less time in light and moderate intensity activity and more time being sedentary compared with data recorded from three axes of newer generation devices.39 Intensity thresholds are influenced by participant age and activities included in any calibration study and there is currently no consensus about standard intensity thresholds. We used thresholds derived during locomotor activities (ie, walking and jogging) in young adults when defining time spent in light, moderate, and vigorous physical activity,25 that are higher than those derived in older women in a range of activities, including sitting and standing.40 This could affect the absolute time spent in vigorous physical activity and in prolonged bouts of moderate-to-vigorous physical activity. Furthermore, results were combined from studies using two different brands of accelerometers; however, when we restricted analyses to the six studies using the same accelerometer brand, similar findings were observed. Risk of bias was assessed using the Newcastle-Ottawa scale suggested as an alternative to the Risk of Bias in Non-randomised Studies of Interventions.41 Finally, physical activity and sedentary time were only measured once, therefore changes in these behaviours might affect the observed associations.
Comparison with other studies
Higher levels of total physical activity, which combine the frequency, duration, and intensity of activity, were associated with a substantially reduced risk of death in a dose-response fashion. In spline analyses, the maximal risk reduction was observed at about 300 counts per minutes (cpm, fig 2, supplementary table 5). This value mirrors the median total physical activity for the third quarter across studies (supplementary table 3). It is also similar to the mean value observed in US men, between 10-15% higher than in US women and about 10-15% lower than in the population based samples from Norway and Sweden (supplementary table 1). The amount of total physical activity required for maximal risk reduction thus seems achievable for large segments of the population. For those unable to accumulate this amount, it is encouraging to note that the largest risk reduction was observed between the second quarter and the referent (least active). The observed magnitude of risk reduction (about 60-70%) is more than twice as large as previously reported from studies assessing total physical activity by self report.42 Our findings extend previous observations from individual studies on device assessed total physical activity10 12 and those reported for total physical activity in community dwelling elderly people,43 44 by reducing the uncertainty in the effect estimates in a much larger and more heterogeneous sample.
Our results also suggest substantial risk reductions from light intensity physical activity, in a dose-response fashion. A recent meta-analysis45 that combined self reported and device based measures of light intensity physical activity observed a pooled risk reduction of 29% when extreme groups were compared, smaller in magnitude than the estimate reported here (about 60% when the fourth quarter was compared with the referent). Time accumulated in moderate-to-vigorous intensity physical activity was also associated with reduced mortality risk in a dose-response manner. It should be noted, however, that the definition of intensity1 46 is based on absolute intensity (ie, as customary, light intensity=1.5-2.9 metabolic equivalents of task (METs); moderate-to-vigorous intensity ≥3 METs). In older people, who constitute most of the participants in our meta-analysis, maximal cardiorespiratory fitness may not exceed 6 or 7 METs.47 Thus high light intensity physical activity as defined in the present analyses might actually represent moderate-to-vigorous intensity physical activity, relative to the fitness level of these older adults. Future calibration studies aimed at identifying intensity thresholds for light and moderate intensity physical activity from tri-axial accelerometry based on relative intensity (ie, % maximal cardiorespiratory fitness) are needed, especially for use in older populations. Owing to the low numbers of people with high levels of time spent in moderate-to-vigorous intensity physical activity, wide confidence intervals were observed at this part of the dose-response curve warranting cautious interpretation. The maximal risk reduction was seen at about 24 min/day, congruent with the minimum recommended level of physical activity for Americans46 and the proposed draft of the new UK physical activity guidelines48 of at least 150 minutes of moderate intensity physical activity each week. Similar to total physical activity and light intensity physical activity, the maximal risk reduction observed for moderate-to-vigorous physical activity (about 60%), is about twice the magnitude as previously reported in a meta-analysis, where physical activity was assessed by self report.49 We observed smaller magnitudes of risk reduction for bouts of moderate-to-vigorous intensity physical activity and vigorous intensity physical activity compared with the other physical activity exposure variables. Most participants, however, did not record any minutes at these intensity levels, limiting the interpretation of these observations.
Higher sedentary time was positively associated with higher risk of death, and the risk increased at levels greater than 9.5 hours each day. This estimate is higher than a proposed threshold of 6 to 8 hours each day identified in a recent meta-analysis examining the association between primarily self reported sitting time and mortality.5 Given the strong association between total physical activity and mortality, it is plausible that findings for sedentary time reflect the “flip side” of a coin.50
Implications and future research
Recent national51 and international52 strategies to improve public health through physical activity in populations are supported by our results. Additionally, these results reinforce the new physical activity recommendations for Americans to limit sedentary time and that moderate-to-vigorous intensity physical activity need not occur in 10 minute bouts.46 Furthermore, the findings are important for policymakers and can inform future guideline development by also recognising the role of light intensity physical activity and hence total physical activity for reducing the risk of premature death. Thus, the public health message might simply be “sit less and move more and more often.”
We only investigated associations with all cause mortality. Thus more work is needed to determine the associations between physical activity and sedentary time with cause specific mortality and for other chronic morbidities such as type 2 diabetes, which may manifest at a younger age than the age of our cohorts. Future studies using repeated measures of physical activity with device based methods such as acclerometry are also needed to examining the associations between changes in physical activity and sedentary time with clinical health outcomes. Finally, data on the association between device based assessment of physical activity and mortality from low and middle income countries are currently unavailable.
Conclusion
Our findings provide clear scientific evidence that higher levels of total physical activity—regardless of intensity level—and lesser amounts of sedentary time are associated with lower risk for premature mortality, with evidence of non-linear, dose-response patterns in middle aged and older people.
What is already known on this topic.
Physical inactivity is associated with many chronic diseases and premature mortality and increasing evidence also suggests that high levels of sedentary time may increase the risk of chronic diseases and mortality
Current physical activity guidelines are, however, informed primarily by self reported physical activity studies, which are susceptible to error
Thus the magnitude of associations is likely underestimated and the shape of dose-response relations, particularly for light intensity activity, is unclear
What this study adds
All intensities of physical activity, including light intensity, are associated with a substantially reduced risk of death in a dose-response manner
The observed effect sizes for the associations between physical activity and the risk of death are about twice as large compared with those previously reported in studies assessing physical activity by self report
A statistical significantly higher risk of death was observed for sedentary times of 9.5 or more hours daily
Web extra.
Extra material supplied by authors
Supplementary information: additional tables and figures
Contributors: UE and I-ML conceived and designed the study. All authors acquired the data. UE, JT, BHH, JS-J, SAA, BJ, and I-ML analysed and interpreted the pooled data. UE and JT drafted the manuscript. All authors critically revised the manuscript for important intellectual content. MWF and JT carried out the statistical analysis of the pooled data. UE is the guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: There was no specific funding for this work. The individual studies contributing to this harmonised meta-analysis were funded: the ABC-study was funded by Stockholm County Council, Swedish National Centre for Research in Sports, and project ALPHA, which received funding from the European Union in the framework of the Public Health Programme and Folksam Research Foundation, Sweden; the British Regional Heart Study was funded by project and programme grants from the British Heart Foundation (PG/13/86/30546 and RG/13/16/30528); the Framingham Heart Study’s data collection and analysis was funded by the National Institutes of Health, National Heart, Lung, and Blood Institute (NHLBI)-N01-HC25195; Health and Human Services (N268201500001I; R01-AG047645; R01-HL131029); and American Heart Association (15GPSGC24800006); the Norwegian National Physical Activity Surveillance Study was supported by the Norwegian Directorate for Public Health and the Norwegian School of Sport Sciences. JT is funded by the Research Council of Norway (249932/F20); the REGARDS study was supported by a cooperative agreement U01-NS041588 and investigator initiated grant R01-NS061846 from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health. Additional funding was provided by an unrestricted research grant from the Coca-Cola Company; the Walking Away from type 2 Diabetes study was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care East Midlands; the Women’s Health Study was funded by the National Institutes of Health (NIH) grants; CA154647, CA047988, CA182913, HL043851, HL080467, and HL099355. The funders of the individual studies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Competing interests: All authors have completed the ICMJE uniform disclosure form and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Not required.
Data sharing: The study specific summary data included in the meta-analysis can be obtained from the corresponding author; ulf.ekelund@nih.no
The lead author (UE) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
References
- 1. 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. U.S. Department of Health and Human Services, 2018. [Google Scholar]
- 2. Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, Lancet Physical Activity Series Working Group Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380:219-29. 10.1016/S0140-6736(12)61031-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ding D, Lawson KD, Kolbe-Alexander TL, et al. Lancet Physical Activity Series 2 Executive Committee The economic burden of physical inactivity: a global analysis of major non-communicable diseases. Lancet 2016;388:1311-24. 10.1016/S0140-6736(16)30383-X [DOI] [PubMed] [Google Scholar]
- 4. Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med 2015;162:123-32. 10.7326/M14-1651 [DOI] [PubMed] [Google Scholar]
- 5. Patterson R, McNamara E, Tainio M, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol 2018;33:811-29. 10.1007/s10654-018-0380-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act 2008;5:56. 10.1186/1479-5868-5-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Warren JM, Ekelund U, Besson H, Mezzani A, Geladas N, Vanhees L, Experts Panel Assessment of physical activity - a review of methodologies with reference to epidemiological research: a report of the exercise physiology section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil 2010;17:127-39. 10.1097/HJR.0b013e32832ed875 [DOI] [PubMed] [Google Scholar]
- 8. Clark BK, Lynch BM, Winkler EAH, et al. Validity of a multi-context sitting questionnaire across demographically diverse population groups: AusDiab3. Int J Behav Nutr Phys Act 2015;12:148. 10.1186/s12966-015-0309-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Diaz KM, Howard VJ, Hutto B, et al. Patterns of Sedentary Behavior and Mortality in U.S. Middle-Aged and Older Adults: A National Cohort Study. Ann Intern Med 2017;167:465-75. 10.7326/M17-0212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dohrn IM, Sjöström M, Kwak L, Oja P, Hagströmer M. Accelerometer-measured sedentary time and physical activity-A 15 year follow-up of mortality in a Swedish population-based cohort. J Sci Med Sport 2018;21:702-7. 10.1016/j.jsams.2017.10.035 [DOI] [PubMed] [Google Scholar]
- 11. LaMonte MJ, Buchner DM, Rillamas-Sun E, et al. Accelerometer-Measured Physical Activity and Mortality in Women Aged 63 to 99. J Am Geriatr Soc 2018;66:886-94. 10.1111/jgs.15201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lee IM, Shiroma EJ, Evenson KR, Kamada M, LaCroix AZ, Buring JE. Accelerometer-Measured Physical Activity and Sedentary Behavior in Relation to All-Cause Mortality: The Women’s Health Study. Circulation 2018;137:203-5. 10.1161/CIRCULATIONAHA.117.031300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Matthews CE, Keadle SK, Troiano RP, et al. Accelerometer-measured dose-response for physical activity, sedentary time, and mortality in US adults. Am J Clin Nutr 2016;104:1424-32. 10.3945/ajcn.116.135129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Evenson KR, Wen F, Herring AH. Associations of Accelerometry-Assessed and Self-Reported Physical Activity and Sedentary Behavior With All-Cause and Cardiovascular Mortality Among US Adults. Am J Epidemiol 2016;184:621-32. 10.1093/aje/kww070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008-12. 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 16.Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. http://www.prisma-statement.org/ (Accessed 15 Januari 2018)
- 17. Hildebrand M, VAN Hees VT, Hansen BH, Ekelund U. Age group comparability of raw accelerometer output from wrist- and hip-worn monitors. Med Sci Sports Exerc 2014;46:1816-24. 10.1249/MSS.0000000000000289 [DOI] [PubMed] [Google Scholar]
- 18. Ensrud KE, Blackwell TL, Cauley JA, et al. Osteoporotic Fractures in Men Study Group Objective measures of activity level and mortality in older men. J Am Geriatr Soc 2014;62:2079-87. 10.1111/jgs.13101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Koolhaas CM, Dhana K, van Rooij FJ, et al. Sedentary time assessed by actigraphy and mortality: The Rotterdam Study. Prev Med 2017;95:59-65. 10.1016/j.ypmed.2016.11.021 [DOI] [PubMed] [Google Scholar]
- 20. Klenk J, Dallmeier D, Denkinger MD, Rapp K, Koenig W, Rothenbacher D, ActiFE Study Group Objectively Measured Walking Duration and Sedentary Behaviour and Four-Year Mortality in Older People. PLoS One 2016;11:e0153779. 10.1371/journal.pone.0153779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed January 15 2018)
- 22. Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc 2011;43:357-64. 10.1249/MSS.0b013e3181ed61a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc 2005;37(Suppl):S531-43. 10.1249/01.mss.0000185657.86065.98 [DOI] [PubMed] [Google Scholar]
- 24. Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol 2008;167:875-81. 10.1093/aje/kwm390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc 1998;30:777-81. 10.1097/00005768-199805000-00021 [DOI] [PubMed] [Google Scholar]
- 26. Murabito JM, Pedley A, Massaro JM, et al. Moderate-to-vigorous physical activity with accelerometry is associated with visceral adipose tissue in adults. J Am Heart Assoc 2015;4:e001379. 10.1161/JAHA.114.001379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Colley RC, Tremblay MS. Moderate and vigorous physical activity intensity cut-points for the Actical accelerometer. J Sports Sci 2011;29:783-9. 10.1080/02640414.2011.557744 [DOI] [PubMed] [Google Scholar]
- 28. Wong SL, Colley R, Connor Gorber S, Tremblay M. Actical accelerometer sedentary activity thresholds for adults. J Phys Act Health 2011;8:587-91. 10.1123/jpah.8.4.587 [DOI] [PubMed] [Google Scholar]
- 29.Johnson CL, Paulose-Ram R, Ogden CL, et al. National Health and Nutrition Examination Survey: Analytic guidelines, 1999-2010. National Center for Health Statistics. Vital Health Stat 2013;2(161). www.cdc.gov/nchs/data/series/sr_02/sr02_161.pdf [PubMed]
- 30. White IR. Multivariate random-effects meta-analysis. Stata J 2009;9:40-56 10.1177/1536867X0900900103. [DOI] [Google Scholar]
- 31. Liu Q, Cook NR, Bergström A, et al. A two-stage hierarchical regression model for meta-analysis of epidemiologic nonlinear dose-response data. Comput Stat Data Anal 2009;53:4157-67 10.1016/j.csda.2009.05.001 www.sciencedirect.com/science/article/pii/S0167947309001765 [DOI] [Google Scholar]
- 32. Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 2012;175:66-73. 10.1093/aje/kwr265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Discacciati A, Crippa A, Orsini N. Goodness of fit tools for dose-response meta-analysis of binary outcomes. Res Synth Methods 2017;8:149-60. 10.1002/jrsm.1194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Duncan S, Stewart T, Bo Schneller M, Godbole S, Cain K, Kerr J. Convergent validity of ActiGraph and Actical accelerometers for estimating physical activity in adults. PLoS One 2018;13:e0198587. 10.1371/journal.pone.0198587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hansen BH, Kolle E, Dyrstad SM, Holme I, Anderssen SA. Accelerometer-determined physical activity in adults and older people. Med Sci Sports Exerc 2012;44:266-72. 10.1249/MSS.0b013e31822cb354 [DOI] [PubMed] [Google Scholar]
- 36. Bakrania K, Edwardson CL, Khunti K, et al. Associations of objectively measured moderate-to-vigorous-intensity physical activity and sedentary time with all-cause mortality in a population of adults at high risk of type 2 diabetes mellitus. Prev Med Rep 2017;5:285-8. 10.1016/j.pmedr.2017.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Jefferis BJ, Parsons TJ, Sartini C, et al. Objectively measured physical activity, sedentary behaviour and all-cause mortality in older men: does volume of activity matter more than pattern of accumulation? Br J Sports Med 2018. Feb 12. pii: bjsports-2017-098733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Allison DB, Heo M, Flanders DW, Faith MS, Williamson DF. Examination of “early mortality exclusion” as an approach to control for confounding by occult disease in epidemiologic studies of mortality risk factors. Am J Epidemiol 1997;146:672-80. 10.1093/oxfordjournals.aje.a009334 [DOI] [PubMed] [Google Scholar]
- 39. Keadle SK, Shiroma EJ, Freedson PS, Lee IM. Impact of accelerometer data processing decisions on the sample size, wear time and physical activity level of a large cohort study. BMC Public Health 2014;14:1210. 10.1186/1471-2458-14-1210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Evenson KR, Wen F, Herring AH, et al. Calibrating physical activity intensity for hip-worn accelerometry in women age 60 to 91 years: The Women’s Health Initiative OPACH Calibration Study. Prev Med Rep 2015;2:750-6. 10.1016/j.pmedr.2015.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.ROBINS-I tool. Cochrane Methods https://methods.cochrane.org/robins-i-tool assessed June 8th 2019.
- 42. Lear SA, Hu W, Rangarajan S, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet 2017;390:2643-54. 10.1016/S0140-6736(17)31634-3 [DOI] [PubMed] [Google Scholar]
- 43. Manini TM, Everhart JE, Patel KV, et al. Daily activity energy expenditure and mortality among older adults. JAMA 2006;296:171-9. 10.1001/jama.296.2.171 [DOI] [PubMed] [Google Scholar]
- 44. Buchman AS, Yu L, Boyle PA, Shah RC, Bennett DA. Total daily physical activity and longevity in old age. Arch Intern Med 2012;172:444-6. 10.1001/archinternmed.2011.1477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chastin SFM, De Craemer M, De Cocker K, et al. How does light-intensity physical activity associated with adult cardiometabolic health and mortality? Systematic review with meta-analysis of experimental and observational studies. Br J Sports Med 2018; Apr 25. pii: bjsports-2017-097563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA 2018;320:2020-8. 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kaminsky LA, Arena R, Myers J. Reference standards for cardio-respiratory fitness measured with cardio-pulmonary exercise testing: data from the fitness registry and the importance of exercise national database. Mayo Clin Proc 2015;90:1515-23. 10.1016/j.mayocp.2015.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Working paper: Draft review and recommendation for adults www.bristol.ac.uk/sps/research/projects/current/physical-activity/final-working-group-papers/ accessed December 28th 2018.
- 49. Arem H, Moore SC, Patel A, et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med 2015;175:959-67. 10.1001/jamainternmed.2015.0533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Stamatakis E, Ekelund U, Ding D, Hamer M, Bauman A, Lee IM. Is it time for quantitative public health guidelines on sitting? A narrative review of sedentary behaviour research paradigms and findings. Br J Sports Med 2018. Jun 10. pii: bjsports-2018-099131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Centers for Disease Control and Prevention. Active people, healthy nation www.cdc.gov/physicalactivity/activepeoplehealthynation/index.html accessed April 1st 2019.
- 52. Global action plan on physical activity 2018-2030: more active people for a healthier world. World Health Organization, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information: additional tables and figures