Abstract
Objective
To assess effects of increasing omega-3, omega-6, and total polyunsaturated fatty acids (PUFA) on diabetes diagnosis and glucose metabolism.
Design
Systematic review and meta-analyses.
Data sources
Medline, Embase, Cochrane CENTRAL, WHO International Clinical Trials Registry Platform, Clinicaltrials.gov, and trials in relevant systematic reviews.
Eligibility criteria
Randomised controlled trials of at least 24 weeks’ duration assessing effects of increasing α-linolenic acid, long chain omega-3, omega-6, or total PUFA, which collected data on diabetes diagnoses, fasting glucose or insulin, glycated haemoglobin (HbA1c), and/or homoeostatic model assessment for insulin resistance (HOMA-IR).
Data synthesis
Statistical analysis included random effects meta-analyses using relative risk and mean difference, and sensitivity analyses. Funnel plots were examined and subgrouping assessed effects of intervention type, replacement, baseline risk of diabetes and use of antidiabetes drugs, trial duration, and dose. Risk of bias was assessed with the Cochrane tool and quality of evidence with GRADE.
Results
83 randomised controlled trials (mainly assessing effects of supplementary long chain omega-3) were included; 10 were at low summary risk of bias. Long chain omega-3 had little or no effect on likelihood of diagnosis of diabetes (relative risk 1.00, 95% confidence interval 0.85 to 1.17; 58 643 participants, 3.7% developed diabetes) or measures of glucose metabolism (HbA1c mean difference −0.02%, 95% confidence interval −0.07% to 0.04%; plasma glucose 0.04, 0.02 to 0.07, mmol/L; fasting insulin 1.02, −4.34 to 6.37, pmol/L; HOMA-IR 0.06, −0.21 to 0.33). A suggestion of negative outcomes was observed when dose of supplemental long chain omega-3 was above 4.4 g/d. Effects of α-linolenic acid, omega-6, and total PUFA on diagnosis of diabetes were unclear (as the evidence was of very low quality), but little or no effect on measures of glucose metabolism was seen, except that increasing α-linolenic acid may increase fasting insulin (by about 7%). No evidence was found that the omega-3/omega-6 ratio is important for diabetes or glucose metabolism.
Conclusions
This is the most extensive systematic review of trials to date to assess effects of polyunsaturated fats on newly diagnosed diabetes and glucose metabolism, including previously unpublished data following contact with authors. Evidence suggests that increasing omega-3, omega-6, or total PUFA has little or no effect on prevention and treatment of type 2 diabetes mellitus.
Systematic review registration
PROSPERO CRD42017064110.
Introduction
Type 2 diabetes mellitus is a leading cause of death and increases risks of cardiovascular disease, blindness, kidney failure, and lower limb amputation.1 More than 400 million adults worldwide live with diabetes. This figure is rising,1 2 causing excess mortality, morbidity, and substantial economic cost. The global annual cost of diabetes is estimated at more than $800bn (£636bn; €709bn) and is increasing.1 3 Type 2 diabetes mellitus occurs as glycaemic control worsens leading to dyslipidaemia (higher triglycerides and lower concentrations of high density lipoprotein cholesterol) and is due to defects in production and/or action of insulin.4 5 The global rise in diabetes can be attributed mainly to increased body fatness and inactivity,1 6 so diet and body weight are key in treating, preventing, and delaying onset of type 2 diabetes mellitus.1
Polyunsaturated fatty acids (PUFA) include omega-3, omega-6, and omega-9 fats. Omega-3 fats include long chain omega-3 fats such as eicosapentaenoic acid and docosahexaenoic acid, commonly found in fish, and α-linolenic acid found in some plant oils (including flaxseed and rapeseed or canola). Many plant oils are rich in omega-6 fats, particularly linoleic acid. The UK government recommends that all adults should consume 6.5% of energy as PUFA and suggests eating a portion of oily fish each week (providing ~0.45 g/d long chain omega-3) but limiting oily fish in pregnancy and lactation owing to potential methylmercury contamination; supplements are not recommended.7 8 9 The American Diabetes Association endorses a Mediterranean-style diet high in polyunsaturates, long chain omega-3, and α-linolenic acid without supplements.10 Oily fish intake, but not supplementation, is also recommended in UK patients with type 2 diabetes mellitus, and reduction of total and saturated fat is recommended for prevention of diabetes, replacing saturated with polyunsaturated fats.10 11 The American Heart Association recommends supplementation for adults not eating enough oily fish.12 The Global Burden of Disease Study suggests that optimal omega-6 intake is 11% of energy, although global intakes average under 5% of energy intake; optimal intake of long chain omega-3 is 0.25 g/d, and mean global intake is 0.10 g/d.13 Despite the consistency of advice to eat oily fish, oily fish intakes in the UK have been stable for a decade at less than half of recommended levels.14 15 US adults’ intakes of long chain omega-3 are higher from dietary supplements (0.72 g/d eicosapentaenoic acid and docosahexaenoic acid) than from foods (0.41 g/d).16
Worries about effects of long chain omega-3 on control of diabetes have long existed, and experimental studies suggest that omega-3 supplementation and diets high in PUFA and omega-3 raise fasting glucose significantly.17 18 Methylmercury and polychlorinated biphenyl levels exceeding recommended thresholds have been reported in seafoods and fish oil supplements8 19 20; elevated mercury levels interrupt insulin signalling, raising fasting glucose, in mouse models.21 Body concentrations of organic pollutants are correlated with prevalence of diabetes in the US,22 but other cross sectional studies have suggested either no association with or benefits of eating fish on glycaemic control.23 24 Systematic reviews of observational studies have suggested both positive and negative associations with glucose metabolism,25 26 27 28 but strong evidence shows that omega-3 supplements reduce raised triglycerides and have little or no effect on body weight.29 Although analysis of Global Burden of Disease data suggests that both long chain omega-3 and omega-6 need to be increased globally, theories suggest that omega-3 and omega-6 fats compete in some metabolic pathways so that the omega-3/omega-6 ratio is more important than absolute intakes of either.30 A Cochrane systematic review assessed effects of omega-3 in people with diabetes, including trials randomising 1075 participants in 23 trials for a mean of nine weeks, finding reductions in triglycerides but no changes in glycated haemoglobin (HbA1c), fasting glucose, or insulin.31 A more recent review included 1209 participants with diabetes in 20 randomised controlled trials of at least two weeks’ duration and found little effect apart from an almost statistically significant rise in fasting glucose but little or no effect on HbA1c.32
Long term effects of PUFA on development and treatment of diabetes remain inconclusive. We aimed to systematically review effects of PUFA (long chain omega-3, α-linolenic acid, omega-6, total PUFA) on diabetes outcomes including diagnoses of diabetes and pre-diabetes and markers of glucose regulation (serum glucose, HbA1c, insulin resistance). We were also interested in how effects varied by intervention type, baseline glucose metabolism, dose, duration, and nutrients displaced by increased PUFA. This review is part of a series by the PUFAH Group commissioned by the World Health Organization’s Nutrition Guidance Expert Advisory Group (NUGAG) Subgroup on Diet and Health to inform and contribute to the development of updated WHO recommendations. The full set of reviews assesses effects of PUFA on cardiovascular disease, cancers, inflammatory bowel disease, neurocognitive outcomes, musculoskeletal and functional outcomes, and depression.29 33 34 35 36 37 38
Methods
This systematic review is registered on PROSPERO.39 Methods for the set of PUFAH reviews were based on Cochrane and GRADE,40 41 using RevMan and GradePRO software. Detailed methods for the set of reviews, the trials database, and flow diagrams are described elsewhere.36 The review method is briefly presented here.
Inclusion criteria
We included published and unpublished randomised controlled trials comparing higher with lower omega-3, omega-6, and/or total PUFA intake for at least 24 weeks that assessed our primary outcomes. Participants were adults (aged ≥18 years) at any risk of diabetes, including healthy adults and those with diagnosed diabetes, but we excluded trials of pregnant or acutely ill participants. Eligible interventions could be dietary advice, supplementation (taken orally as oil, foods, or capsules), or diet provided. If no clear aim to increase PUFA was stated, but it was implied, the intervention had to achieve an increase or decrease of at least 10% of baseline PUFA level. As total dose of PUFA (PUFA dose in intervention minus PUFA dose in control) was difficult to establish reliably in most studies owing to poor reporting of control interventions, we included studies in the higher versus lower total PUFA comparison only when the trial aimed to increase total PUFA or aimed to increase both omega-3 and omega-6 in the intervention compared with the control group. We excluded multifactorial interventions. Primary outcomes included new diagnosis of diabetes, new diagnosis of pre-diabetes (eg, impaired fasting glucose, impaired glucose tolerance, or impaired glucose regulation), glycaemic control (serum or plasma glucose, HbA1c), serum insulin, and insulin resistance (homoeostatic model assessment for insulin resistance (HOMA-IR)).
Methods for identification of studies
We searched Cochrane CENTRAL, Medline, and Embase to 27 April 2017 and ClinicalTrials.com and the WHO International Clinical Trials Registry Platform to September 2016, and we reassessed all ongoing trials in December 2018. We checked included trials of relevant systematic reviews and wrote to authors of included studies for additional studies and trial data, as described in detail elsewhere,36 creating a database of trials that randomised participants to increased omega-3, omega-6, or total PUFA compared with lower omega-3, omega-6, or total PUFA and assessed effects for at least 24 weeks (reflecting metabolic studies suggesting that six months is the minimum duration of supplementation needed to ensure equilibration of long chain omega-3 into most body compartments).42 From this database, we chose studies for this review that had assessed at least one primary review outcome (even when not fully reported).
Study inclusion, data extraction, and assessment of risk of bias were conducted independently in duplicate. We assessed Cochrane risk of bias tool domains,43 as well as assessing risk from compliance problems and attention bias, specific to our set of reviews.36 We considered trials to be at low summary risk of bias if we judged randomisation, allocation concealment, and blinding of participants, personnel, and outcome assessors to be adequate (we considered all other trials to be at moderate or high risk of bias).
Data synthesis
Our primary analyses assessed effects of total PUFA, omega-6, long chain omega-3, and α-linolenic acid (omega-3) separately using random effects meta-analysis, as dietary interventions are heterogeneous by their nature.44 We combined treatment-control differences in outcomes across studies by using relative risks or mean differences; we converted measures using different units to a single unit. We used data on change from baseline in each arm with standard deviations for continuous outcomes where available or endpoint data otherwise.44 We ran sensitivity analyses for all primary outcomes by using fixed effect meta-analysis, limited to studies at low summary risk of bias and at low risk of bias from compliance. We did further sensitivity analyses (limiting analyses to studies without industry funding, studies registered on a trials register if published since 2010, and trials that randomised ≥100 participants), subgrouping, and funnel plots where a meta-analysis included at least 10 trials. We noted where data were measured but not fully reported to assess potential publication bias, and we displayed partially reported data in forest plots to allow assessment of consistency with meta-analysis results. We used I2 to assess heterogeneity and considered it important when it was greater than 50%.45
Effect sizes were interpreted as agreed with WHO NUGAG and pre-specified for this set of reviews.36 We considered a relative risk below 0.92 or above 1.08 to be a relevant clinical effect (0.92-1.08 was considered “little or no effect”), and we required a mean difference between arms of at least 5% of baseline for a relevant clinical effect for continuous measures. Outcome data were interpreted using GRADE assessment, drafted by LH, and then discussed and agreed with WHO NUGAG as elaborated elsewhere.36 Where GRADE suggested data of very low quality, we did not interpret effect sizes. Where data were of low quality, we used the term “may,” and moderate quality evidence warranted “probably” in describing effect sizes.
Subgroup analysis
We subgrouped data on the basis of intervention type, dose, trial duration, replacement, age, sex, baseline diabetes risk categories (general population; ≥50% without diabetes but with elevated risk due to comorbidities such as metabolic syndrome or impaired glucose metabolism but not obesity; ≥50% existing diagnosis of type 2 diabetes mellitus) and baseline use of antidiabetes drugs. We were not able to subgroup by baseline intakes or change in omega-3/omega-6 ratio as these data were rarely provided. Instead, we added a post hoc subgroup comparing “more omega-3 versus more omega-6,” from trials with suitable data as, if the ratio theory is correct,30 increasing omega-3 at the cost of omega-6 would be more beneficial than simply boosting omega-3.
Deviations from protocol and post hoc analyses
At the request of the funders, we did an additional sensitivity analysis with respect to compliance. Our protocol stated an intention to subgroup by “recent publications;” we changed this to run a sensitivity analysis including publications before 2010 combined with all publications from 2010 onwards with a trials registry entry (even if published retrospectively). As our funders were particularly interested in effects within trials of at least 12 months, we also ran an analysis limiting to trials of at least 52 weeks’ duration. At the request of reviewers, we assessed small study bias by using formal tests (Egger’s test, Begg’s test, Harbord’s test, and Peters’ test, each used where appropriate) in addition to assessing funnel plot asymmetry, for analyses with at least 10 included trials.
Patient and public involvement
We did not involve patients or the public in this research at any stage. No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for design or implementation of the study. No patients were asked to advise on interpretation or writing up of results, but we do have plans to disseminate the results of the research to the relevant patient community.
Results
Description of studies
Results are summarised here, and a fuller account of results (supplementary text) with additional tables, forest plots and funnel plots, and details of all sensitivity analyses and subgroups, can be found in the supplementary materials. Characteristics, risk of bias assessments and bibliographic references of included studies are detailed in supplementary table A.
We included 83 randomised controlled trials that measured at least one of our primary outcomes. These 83 trials (85 comparison groups) randomised 121 070 participants. We assessed 10 randomised controlled trials as being at low summary risk of bias.46 47 48 49 50 51 52 53 54 55 Half the trials were conducted in Europe (41), 16 in North America, three in South America, 15 in Asia, six in Australia, and two across at least two continents. Twenty six studies specifically recruited participants with diabetes or impaired glucose metabolism (of which one recruited people with type 1 diabetes). We attempted to contact authors of 52 included trials, from whom we received information on methods and/or results relating to 36 trials (see acknowledgments). We found no randomised controlled trials that assessed effects of any PUFA on diagnosis of pre-diabetes.
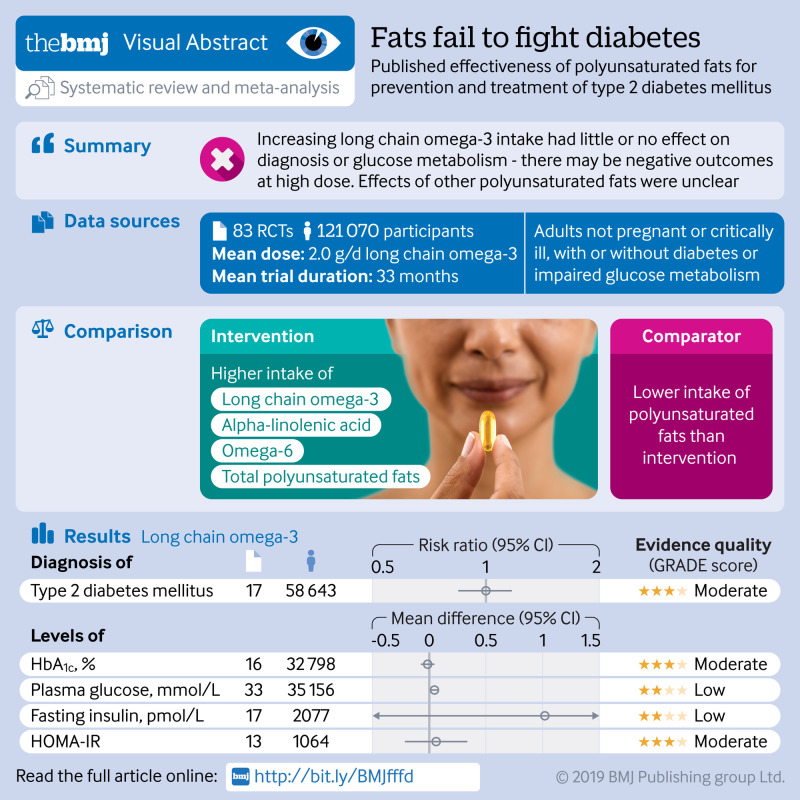
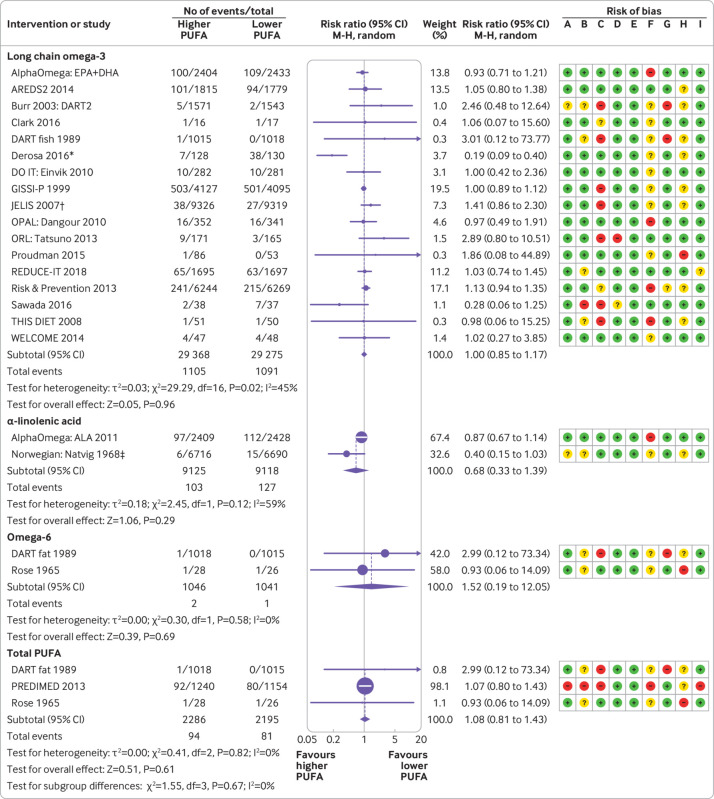
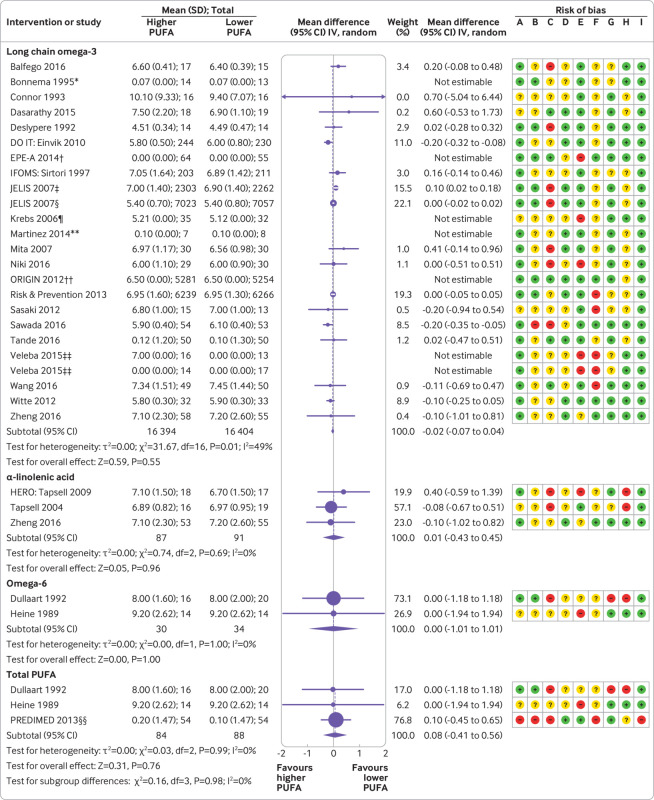
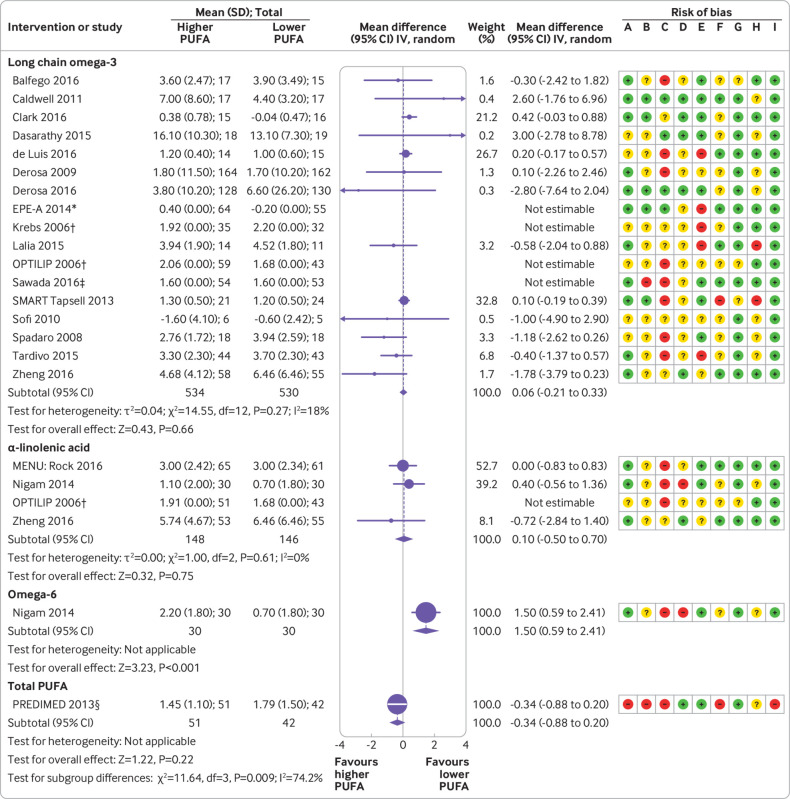
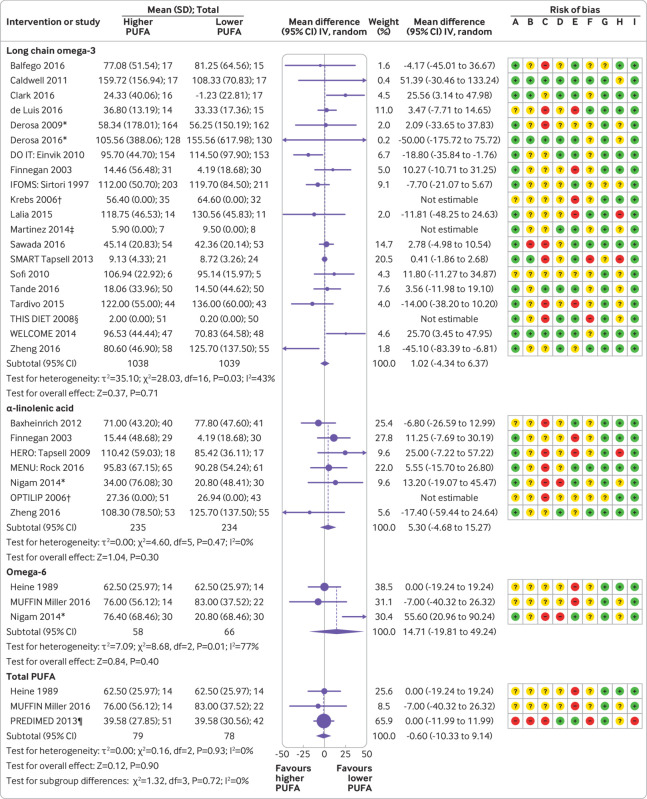
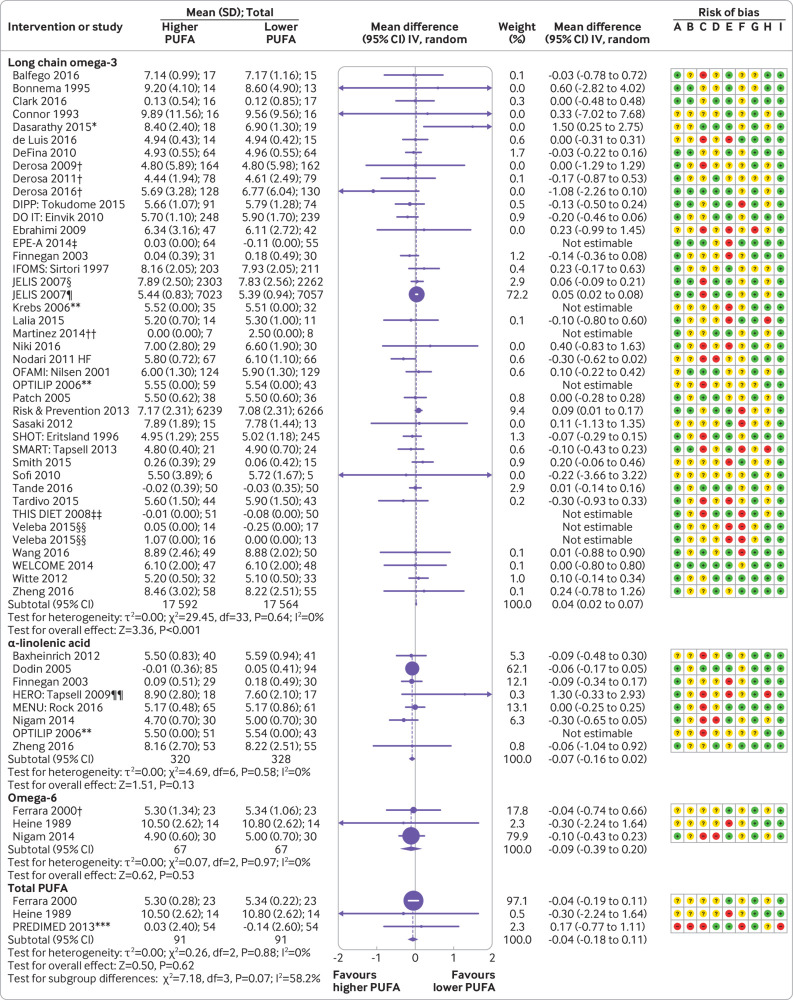
Effects of long chain omega-3
Sixty six trials assessed effects of long chain omega-3, of which 10 were at low summary risk of bias. Table 1 shows the GRADE summary of findings for long chain omega-3, with full details of long chain omega-3 meta-analyses, sensitivity analyses, and subgrouping in supplementary tables B to F. Meta-analyses, sensitivity analyses, funnel plots, and subgrouping of a large body of data suggest that long chain omega-3 probably has little or no effect on risk of diagnosis of type 2 diabetes mellitus (relative risk 1.00, 95% confidence interval 0.85 to 1.17; I2=45%; 17 trials; 58 643 participants, 2196 (3.7%) diabetes diagnoses; number need to treat=∞; moderate quality evidence) (fig 1). This is confirmed by little or no effect on HbA1c (mean difference −0.02%, 95% confidence interval −0.07% to 0.04%; I2=49%; 17 comparisons; 32 798 participants; mean baseline HbA1c 6.5%; moderate quality evidence) (fig 2), HOMA-IR (mean difference 0.06, −0.21 to 0.33; I2=18%; mean baseline HOMA-IR 4.6; moderate quality evidence) (fig 3), fasting serum insulin (mean difference 1.02, −4.34 to 6.37, pmol/L; I2=43%; 17 trials; 2077 participants; mean baseline insulin 98 pmol/L; low quality evidence) (fig 4), or fasting glucose (statistically significant increase in glucose from baseline of <1%, mean difference 0.04, 0.02 to 0.07, mmol/L; I2=0%; 35 156 participants; low quality evidence) (fig 5).
Table 1.
Summary of findings for effects of long chain omega-3 and α-linolenic acid (omega-3) on primary outcomes. High compared with low long chain omega-3 (LCn3) and α-linolenic acid (ALA) for prevention or treatment of diabetes
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) |
No of participants (studies) |
Certainty of evidence (GRADE)† |
Comments | |
|---|---|---|---|---|---|---|
| Risk with low omega-3 fats | Risk with high omega-3 fats | |||||
| Diagnosis of type 2 diabetes mellitus—LCn3 | 37 per 1000 | 37 (32 to 44) per 1000 | RR 1.00 (0.85 to 1.17) | 58 643 (17 RCTs) | ⨁⨁⨁◯ MODERATEa,b,c,d | LCn3 probably has little or no effect on diagnosis of type 2 diabetes. Downgraded once for imprecision |
| Diagnosis of type 2 diabetes mellitus—ALA | 14 per 1000 | 9 (5 to 19) per 1000 | RR 0.68 (0.33 to 1.39) | 18 243 (2 RCTs) | ⨁◯◯◯ VERY LOWb,e,f | Effect of ALA on diabetes diagnosis is uncertain as evidence is of very low quality. Downgraded once for inconsistency and twice for imprecision |
| Diagnosis of impaired glucose tolerance—LCn3 | Not pooled | Not pooled | Not pooled | (0 RCTs) | - | No RCTs assessed effects of LCn3 on diagnosis of impaired glucose tolerance |
| Diagnosis of impaired glucose tolerance—ALA | Not pooled | Not pooled | Not pooled | (0 RCTs) | - | No RCTs assessed effects of ALA on diagnosis of impaired glucose tolerance |
| Glycated haemoglobin (HbA1c, %)—LCn3 | Mean HbA1c 6.5% | Mean HbA1c 0.02% lower (0.07% lower to 0.04% higher) | - | 32 798 (16 RCTs) | ⨁⨁⨁◯ MODERATEb,g | LCn3 probably has little or no effect on glycated haemoglobin. Downgraded once for risk of bias |
| Glycated haemoglobin (HbA1c, %)—ALA | Mean HbA1c 7.0% | Mean HbA1c 0.01% higher (0.43% lower to 0.45% higher) | - | 178 (3 RCTs) | ⨁⨁◯◯ LOWg,h,i | ALA may have little or no effect on glycated haemoglobin. Downgraded once each for imprecision and risk of bias |
| Plasma glucose, fasting (mmol/L)—LCn3 | Mean plasma glucose 6.2 mmol/L | Mean plasma glucose 0.04 (0.02 to 0.07) mmol/L higher | - | 35 156 (33 RCTs) | ⨁⨁◯◯ LOWj,k | LCn3 may have little or no effect on fasting plasma glucose. Downgraded once each for risk of bias and publication bias |
| Plasma glucose, fasting (mmol/L —ALA | Mean plasma glucose 6.2 mmol/L | Mean plasma glucose 0.07 mmol/L lower (0.16 lower to 0.02 higher) | - | 648 (7 RCTs) | ⨁⨁⨁◯ MODERATEl,m | ALA probably has little or no effect on fasting plasma glucose. Downgraded once for risk of bias |
| Fasting insulin (pmol/L)—LCn3 | Mean fasting insulin 98 pmol/L | Mean fasting insulin 1.02 pmol/L higher (4.34 lower to 6.37 higher) | - | 2077 (17 RCTs) | ⨁⨁◯◯ LOWn,p | LCn3 may have little or no effect on fasting insulin. Downgraded once each for risk of bias and imprecision |
| Fasting insulin (pmol/L)—ALA | Mean fasting insulin 80 pmol/L | Mean fasting insulin 5.3 pmol/L higher (4.68 lower to 15.27 higher) | - | 469 (6 RCTs) | ⨁⨁◯◯ LOWo,p | ALA may increase fasting insulin. Downgraded once each for imprecision and risk of bias |
| HOMA-IR—LCn3 | Mean HOMA-IR 4.6 | Mean HOMA-IR 0.06 higher (0.21 lower to 0.33 higher) | - | 1064 (13 RCTs) | ⨁⨁⨁◯ MODERATEp,q,r | LCn3 probably has little or no effect on HOMA-IR. Downgraded once for imprecision |
| HOMA-IR—ALA | Mean HOMA-IR 3.4 | Mean HOMA-IR 0.1 higher (0.5 lower to 0.7 higher) | - | 294 (3 RCTs) | ⨁⨁◯◯ LOWs,t | ALA may have little or no effect on HOMA-IR. Downgraded once for imprecision and once for risk of bias and publication bias combined |
HOMA-IR=homoeostatic model assessment for insulin resistance; RCT=randomised controlled trial; RR=risk ratio.
Patient or population: people with or without diabetes at baseline; setting: these are long term trials, so participants lived in the community; intervention: higher omega-3 intake; comparison: lower omega-3 intake.
Risk in intervention group (and its 95% CI) is based on assumed risk in comparison group and relative effect of intervention (and its 95% CI). Note that GRADE describes risk and 95% CI without using negative numbers; for example, GRADE states “0.02% lower (0.07 lower to 0.04 higher),” which would normally be described as “–0.02% (−0.07% to 0.04%).”
High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect.
a. Risk of bias: limiting studies to those suggesting good compliance and those at summary risk of bias both suggested greater protection from higher LCn3 intake, although neither was statistically significant; these protective effects were entirely due to two small trials (Derosa 2016 and Sawada 2016), and removing them removed heterogeneity and suggestion of any effect. Not downgraded.
b. Indirectness: most studies were conducted in industrialised countries, but the data from the 3 RCTs conducted in industrialising countries (Martinez 2014, Wang 2016, Zheng 2016) seem consistent. Not downgraded.
c. Imprecision: despite >55 000 participants and >2300 diagnoses, statistical significance is not suggested; 95% CI includes important benefit and important harm. Downgraded once.
d. Publication bias: funnel plot suggests that studies with fewer cases of diabetes in the higher LCn3 arm may be missing, but statistical tests did not confirm this. Not downgraded.
e. Inconsistency: I2>50%. Downgraded once.
f. Imprecision: >18 000 participants, but only 230 diagnoses reported, leading to wide confidence intervals, including very important benefits and harms. Downgraded twice.
g. Risk of bias: although the main analysis suggests no effect of LCn3 on HbA1c, no included trials were at low summary risk of bias, and those at low risk of bias from compliance suggested a reduction in HbA1c with LCn3; overall effects not clear. Downgraded once.
h. Indirectness: the largest of the included studies was carried out in China, so data from industrialising countries are well represented. Not downgraded.
i. Imprecision: 178 participants included; very wide confidence intervals did not exclude important benefits or harms. Downgraded once.
j. Risk of bias: main analysis suggests that LCn3 increases plasma glucose, whereas limiting to studies at low summary risk of bias or with low risk of bias from compliance suggests reductions in plasma glucose. Downgraded once.
k. Publication bias: although the funnel plot is not definitive, we are aware of potentially important missing data. Downgraded once.
l. Risk of bias: effects in studies at low risk of bias from compliance and in fixed effects analyses are similar to those in the main analysis (suggesting that ALA reduces fasting plasma glucose), but no studies were at low summary risk of bias. Downgraded once.
m. Imprecision: data from 648 participants included; important harms and benefits are excluded from the 95% CI; the effect was not statistically significant. Not downgraded.
n. Risk of bias: main analysis suggests little or no effect of LCn3 on fasting insulin, and this is confirmed by fixed effects and low risk of bias from compliance analyses; however, limiting studies to those at low summary risk of bias suggests that LCn3 increases fasting insulin substantially (mean difference 25.3 (95% CI 4.1 to 46) pmol/L. Downgraded once.
o. Risk of bias: main analysis suggests a small increase in fasting insulin with ALA, confirmed by fixed effects analysis (neither statistically significant), but smaller effects suggested when studies limited to those at low risk of bias from compliance, and no studies were at low summary risk of bias (and no studies were at low risk of bias from allocation concealment). Downgraded once.
p. Imprecision: 95% CI did not exclude important harms. Downgraded once.
q. Risk of bias: main analysis, fixed effects, low risk of compliance, and low summary risk of bias analyses all suggested little or no effect of LCn3 on HOMA-IR. Not downgraded.
r. Publication bias: funnel plot suggests that studies with higher HOMA-IR scores in the LCn3 arm may be missing; however, statistical tests did not confirm this. Not downgraded.
s. Imprecision: 294 participants contributed to this analysis; 95% CI did not exclude important benefit or harm. Downgraded once.
t. Risk of bias and publication bias: no included studies were at low summary risk of bias; the study with data not added to the meta-analysis suggested increased HOMA-IR with greater ALA, which may indicate publication bias. Downgraded once between the two risks.
Fig 1.
Effect of long chain omega-3, α-linolenic acid, omega-6, and total polyunsaturated fatty acids (PUFA), on new diagnosis of diabetes. *Verified: see author response. †Reported as rise in blood sugar. ‡Diabetes excluded at baseline. Risk of bias key: A=random sequence generation (selection bias); B=Allocation concealment (selection bias); C=blinding of participants and personnel (performance bias); D=blinding of outcome assessment (detection bias); E=incomplete outcome data (attrition bias); F=selective reporting (reporting bias); G=attention; H=compliance; I=other bias
Fig 2.
Effect of long chain omega-3, α-linolenic acid, omega-6, and total polyunsaturated fatty acids (PUFA) on glycated haemoglobin (%). *Units unclear. †Median change from baseline (zero in both arms). ‡In participants with impaired glucose metabolism at baseline. §In participants normoglycaemic at baseline. ¶Geometric means. **Change in medians. ††Medians only provided. ‡‡Median change. §§Barcelona hospital cohort at 5 years, Casas 2016. Risk of bias key: A=random sequence generation (selection bias); B=Allocation concealment (selection bias); C=blinding of participants and personnel (performance bias); D=blinding of outcome assessment (detection bias); E=incomplete outcome data (attrition bias); F=selective reporting (reporting bias); G=attention; H=compliance; I=other bias
Fig 3.
Effect of long chain omega-3, α-linolenic acid, omega-6, and total polyunsaturated fatty acids (PUFA) on homoeostatic model assessment for insulin resistance (HOMA-IR) score. *Median change from baseline. †Geometric means. ‡Medians. §Reus subcohort, 2 year data. Risk of bias key: A=random sequence generation (selection bias); B=Allocation concealment (selection bias); C=blinding of participants and personnel (performance bias); D=blinding of outcome assessment (detection bias); E=incomplete outcome data (attrition bias); F=selective reporting (reporting bias); G=attention; H=compliance; I=other bias
Fig 4.
Effect of long chain omega-3, α-linolenic acid, omega-6, and total polyunsaturated fatty acids (PUFA) on fasting serum insulin (pmol/L). *Reported SDs seemed to be SEs, so converted. †Geometric means. ‡Change in median. §Change, no measure of variance supplied. ¶Reus subcohort, 2 year data. Risk of bias key: A=random sequence generation (selection bias); B=Allocation concealment (selection bias); C=blinding of participants and personnel (performance bias); D=blinding of outcome assessment (detection bias); E=incomplete outcome data (attrition bias); F=selective reporting (reporting bias); G=attention; H=compliance; I=other bias
Fig 5.
Effect of long chain omega-3, α-linolenic acid, omega-6, and total polyunsaturated fatty acids (PUFA) on fasting serum or plasma glucose (mmol/L). *Numbers verified. †Reported SDs seemed to be SEs, so converted. ‡Median change. §In participants with impaired glucose metabolism at baseline. ¶In participants normoglycaemic at baseline. **Geometric means. ††Change in median. ‡‡Change (no SDs supplied). §§Median change; data reported as mean and interquartile range. ¶¶Data verified. ***Barcelona hospital cohort at 5 years, Casas 2016. Risk of bias key: A=random sequence generation (selection bias); B=Allocation concealment (selection bias); C=blinding of participants and personnel (performance bias); D=blinding of outcome assessment (detection bias); E=incomplete outcome data (attrition bias); F=selective reporting (reporting bias); G=attention; H=compliance; I=other bias
Subgrouping results need to be interpreted with caution. Subgrouping by dose did not suggest statistically significant differences between subgroups for any outcomes, but point estimates suggested negative outcomes for diagnosis of diabetes, HbA1c, HOMA-IR, and glucose at doses above 4.4g/d long chain omega-3 (type 2 diabetes mellitus diagnosis relative risk 1.86, 0.08 to 44.89; 1 trial with 139 participants; HbA1c mean difference 0.61%, −0.44% to 1.67%; 2 trials with 53 participants; HOMA-IR mean difference 3.00, −2.78 to 8.78; 1 trial with 37 participants; plasma glucose mean 1.12, 0.04 to 2.19, mmol/L; 2 trials with 69 participants) and smaller negative effects for all except HbA1c and fasting glucose at doses from 2.4 to 4.4 g/d long chain omega-3 (although few trials gave >2.4g/d long chain omega-3) (diabetes diagnosis relative risk 1.10, 0.80 to 1.51; 4 trials with 3856 participants; HOMA-IR, mean difference 0.21, −0.37 to 0.80; 4 trials with 640 participants; fasting insulin mean difference 14.31, −2.12 to 30.74, pmol/L; 5 trials with 737 participants) (full details of subgroup analyses by dose are in supplementary tables B to F). We looked for effects of duration to ensure that we did not miss important health effects not seen in shorter trials, but subgrouping did not suggest important differences between shorter and longer trials for diagnosis of diabetes or other outcomes. We found no significant differences between subgroups for type of intervention, but studies that provided oily fish or other foods were rare, so differences would be difficult to see. Effects did not vary by the nutrient replaced by long chain omega-3, antidiabetes drug use, or baseline glucose metabolism across outcomes.
Effects of α-linolenic acid
Twelve trials assessed effects of α-linolenic acid, one of which was at low summary risk of bias. Table 1 shows GRADE summary of findings for α-linolenic acid, and figures 1-5 show meta-analyses. Full details of α-linolenic acid analyses, including sensitivity analyses and subgrouping, are in supplementary tables G to K.
Effects of α-linolenic acid on diagnosis of diabetes are uncertain, as the evidence is of very low quality (relative risk 0.68, 0.33 to 1.39; I2=59%; 2 trials with 18 243 participants; 230 diabetes diagnoses) (fig 1). Other outcomes provided more data, suggesting that α-linolenic acid has little or no effect on HbA1c (mean difference 0.01%, −0.43% to 0.45%; I2=0%; 3 trials with 178 participants; low quality evidence) (fig 2), HOMA-IR (mean difference 0.10, −0.50 to 0.70; I2=0%; 4 trials with 294 participants; baseline HOMA-IR 3.4; low quality evidence) (fig 3), and fasting glucose (mean difference −0.07, −0.16 to 0.02, mmol/L glucose; I2=0%; 7 trials with 648 participants; moderate quality evidence) (fig 5). However, α-linolenic acid may increase fasting insulin (mean difference 5.3, −4.68 to 15.27, pmol/L; I2=0%; 6 trials with 469 participants; increase of 7% from 80 pmol/L baseline; low quality evidence) (fig 4).
Omega-3 versus omega-6
We considered the subgroup of studies that replaced omega-6 with omega-3 (either long chain omega-3 or α-linolenic acid; see supplementary tables L-N). If the theory that omega-3 and omega-6 fats have opposing roles is correct, we would expect to see strong effects when omega-3 replaces dietary omega-6. However, the data were weak, with limited events, no trials at low summary risk of bias, and wide confidence intervals, so effects of replacing omega-6 with omega-3 fats on diabetes diagnosis and fasting insulin were unclear. We found little or no effect for omega-3 versus omega-6 on HbA1c (mean difference −0.15%, −0.24% to −0.06%; I2=0%; 6 trials with 841 participants), HOMA-IR (mean difference −0.23, −1.35 to 0.88; I2=60%; 6 trials with 328 participants), and fasting glucose (mean difference −0.03, −0.11 to 0.05, mmol/L; I2=10%; 14 comparisons with 1641 participants).
Effects of omega-6
Eleven trials (none at low summary risk of bias) assessed effects of increasing omega-6. Figures 1 to 5 show meta-analyses, table 2 shows the GRADE summary of findings, and full details of omega-6 meta-analyses, including sensitivity analyses, are in supplementary tables O-T.
Table 2.
Summary of findings for effects of omega-6 on primary outcomes. High compared with low omega-6 fats for prevention or treatment of diabetes
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE)† | Comments | |
|---|---|---|---|---|---|---|
| Risk with low omega-6 fats | Risk with high omega-6 fats | |||||
| Diagnosis of type 2 diabetes mellitus | 1 per 1000 | 1 (0 to 12) per 1000 | RR 1.52 (0.19 to 12.05) | 2087 (2 RCTs) | ⨁◯◯◯ VERY LOWa,b,c | Effect of omega-6 fats on diagnoses of type 2 diabetes mellitus is unclear as quality of evidence is very low. Downgraded once for risk of bias and twice for imprecision |
| Diagnosis of impaired glucose tolerance | 0 per 1000 | 0 (0 to 0) per 1000 | Not estimable | (0 RCTs) | - | No RCTs assessed diagnosis of impaired glucose tolerance |
| Glycated haemoglobin (HbA1c, %) | Mean HbA1c 7.9% | Mean HbA1c 0.0% (1.01% lower to 1.01% higher) | - | 64 (2 RCTs) | ⨁⨁◯◯ LOWd,e | Omega 6 fat may have little or no effect on glycated haemoglobin. Downgraded once each for imprecision and risk of bias |
| Plasma glucose, fasting (mmol/L) | Mean plasma glucose 7.05 mmol/L | Mean plasma glucose 0.09 lower (0.39 lower to 0.20 higher) | - | 134 (3 RCTs) | ⨁◯◯◯ VERY LOWf,g,h | Effect of omega-6 fats on plasma glucose is unclear as quality of evidence is very low. Downgraded once each for imprecision, risk of bias, and publication bias |
| Insulin, fasting (pmol/L) | Mean insulin 55.4 pmol/L | Mean insulin 14.7 higher (19.8 lower to 49.2 higher) | - | 124 (3 RCTs) | ⨁◯◯◯ VERY LOWi,j,k | Effect of omega-6 on fasting insulin is unclear as data are of very low quality. Downgraded once each for imprecision, inconsistency, and risk of bias |
| HOMA-IR | Mean HOMA-IR 2.4 | Mean HOMA-IR 1.5 (0.59 to 2.41) higher | - | 60 (1 RCT) | ⨁◯◯◯ VERY LOWl,m | Effect of increasing omega-6 on HOMA-IR is unclear as data are of very low quality. Downgraded once for risk of bias and twice for indirectness |
HOMA-IR=homoeostatic model assessment for insulin resistance; RCT=randomised controlled trial; RR=risk ratio.
Patient or population: people with and without diabetes; setting: these are long term trials, so participants live in the community; intervention: high omega-6 fats; comparison: low omega-6 fats.
Risk in intervention group (and its 95% CI) is based on assumed risk in comparison group and relative effect of intervention (and its 95% CI). Note that GRADE describes risk and 95% CI without using negative numbers; for example, GRADE states “0.02% lower (0.07 lower to 0.04 higher),” which would normally be described as “–0.02% (−0.07% to 0.04%).”
High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect.
a. Risk of bias: effect size did not differ with fixed effects analysis, but neither included study was at low risk of bias from compliance, at low summary risk of bias, or at low risk of bias from allocation concealment. Downgraded once.
b. Indirectness: both studies were carried out in the UK, in men, and more than 25 years ago. Not downgraded.
c. Imprecision: 2087 randomised participants, but only 3 diagnoses reported; very limited data available. Downgraded twice.
d. Risk of bias: effect size did not differ with fixed effects analysis, but neither included study was at low summary risk of bias; 1 was at low risk of bias from allocation concealment, and 1 was at low risk of bias from compliance problems (both suggesting no effect of omega-6 on HbA1c). Downgraded once.
e. Imprecision: data included from 252 participants in 3 RCTs; confidence intervals do not exclude important harm. Downgraded once.
f. Risk of bias: effect size did not differ with fixed effects analysis; none of the 3 included trials was at low risk from allocation concealment or at low summary risk of bias; 1 trial was at low risk of bias from compliance, suggesting a small (but not statistically significant) fall in glucose with more omega-6. Downgraded once.
g. Imprecision: 134 included participants from 3 trials; 95% CI include both important benefits and harms. Downgraded once.
h. Publication bias: we are aware of a further 3 trials that measured glucose but did not report it in a way that could be included in meta-analysis. Downgraded once.
i. Risk of bias: small non-statistically significant increase in insulin with omega-6 seen also in fixed effects analysis; no trials were at low summary risk of bias or at low risk of bias from allocation concealment; 1 trial at low risk of bias from compliance suggested no effect of omega-6 on insulin. Downgraded once.
j. Inconsistency: I2=82%. Downgraded once.
k. Imprecision: data from 124 participants (2 RCTs); 95% CI included important harms and benefits. Downgraded once.
l. Risk of bias: the single study was not at low risk from compliance, allocation concealment, or summary risk of bias. Downgraded once.
m. Indirectness: small single study only. Downgraded twice.
Effects of omega-6 fats on type 2 diabetes mellitus diagnosis (only three diabetes diagnoses included) (fig 1), fasting insulin (mean difference 14.71, −19.81 to 49.24, pmol/L; I2=77%; 124 participants in 3 trials) (fig 4), HOMA-IR (mean difference 1.50, 0.59 to 2.41; 1 trial with 60 participants; mean baseline HOMA-IR 2.4) (fig 3), and plasma glucose (mean difference −0.09, −0.39 to 0.20, mmol/L; I2=0%; 134 participants in 3 trials) (fig 5) were unclear, as quality of evidence was very low. Omega-6 fats may have little or no effect on HbA1c (mean difference 0.00%, −1.01% to 1.01%; I2=0%; 64 participants in 2 trials; mean baseline HbA1c 7.9%; low quality evidence) (fig 2).
Effects of total PUFA
We included eight randomised controlled trials that aimed to increase total PUFA or both omega-3 and omega-6 fats, none of which was at low summary risk of bias. Table 3 shows the GRADE summary of findings, figures 1 to 5 show meta-analyses, and full details of PUFA analyses are in supplementary tables U-Z. Effects of increasing total PUFA on risk of type 2 diabetes mellitus (fig 1) and HOMA-IR (fig 3) were unclear, as the evidence was of very low quality. Increasing total PUFA may make little or no difference to HbA1c (mean difference 0.08%, −0.41% to 0.56%; I2=0%; 3 trials with 172 participants; mean baseline HbA1c 8.6%) (fig 2), fasting insulin (mean difference −0.60, −10.33 to 9.14, pmol/L; I2=0%; 3 trials with 157 participants; mean baseline insulin 62 pmol/L) (fig 4), or fasting glucose (mean difference −0.04, −0.18 to 0.11, mmol/L; I2=0%; 3 trials with 182 participants; mean baseline fasting glucose 8.1 mmol/L; low quality data) (fig 5).
Table 3.
Summary of findings for effects of increasing total polyunsaturated fatty acids (PUFA) on primary outcomes. High compared with low total polyunsaturated fats for prevention or treatment of diabetes
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of evidence (GRADE)† | Comments | |
|---|---|---|---|---|---|---|
| Risk with low PUFA | Risk with high PUFA | |||||
| Diagnosis of type 2 diabetes mellitus | 37 per 1000 | 40 per 1000 (30 to 53) | RR 1.08 (0.81 to 1.43) | 4481 (3 RCTs) | ⨁◯◯◯ VERY LOWa,b | Effect of increasing total PUFA on risk of diabetes diagnosis is unclear as evidence was of very low quality. Downgraded once for risk of bias and twice for imprecision |
| Diagnosis of impaired glucose tolerance | 0 per 1000 | 0 per 1000 (0 to 0) | Not estimable | (0 RCTs) | - | No RCTs assessed effect of total PUFA on diagnosis of impaired glucose tolerance |
| Glycated haemoglobin (HbA1c, %) | Mean HbA1c 8.6% | Mean HbA1c, 0.08% higher (0.41% lower to 0.56% higher) | - | 172 (3 RCTs) | ⨁⨁◯◯ LOWc,d | Increasing total PUFA may make little or no difference to glycated haemoglobin. Downgraded once each for imprecision and risk of bias |
| Plasma glucose, fasting (mmol/L) | Mean plasma glucose 8.1 mmol/L | Mean plasma glucose 0.04 mmol/L lower (0.18 lower to 0.11 higher) | - | 182 (3 RCTs) | ⨁⨁◯◯ LOWe,f | Increasing total PUFA may make little or no difference to plasma glucose. Downgraded once each for imprecision and risk of bias |
| Insulin, fasting (pmol/L) | Mean insulin 61.7 pmol/L | Mean insulin 0.6 pmol/L lower (10.33 lower to 9.14 higher) | - | 157 (3 RCTs) | ⨁⨁◯◯ LOWc,d | Increasing total PUFA may make little or no difference to fasting insulin. Downgraded once each for imprecision and risk of bias |
| HOMA-IR | Mean HOMA-IR 1.8 | Mean HOMA-IR 0.34 lower (0.88 lower to 0.2 higher) | - | 93 (1 RCT) | ⨁◯◯◯ VERY LOWg,h,i | Effect of increasing total PUFA on HOMA-IR is unclear, as evidence is of very low quality. Downgraded once each for imprecision, indirectness and risk of bias |
HOMA-IR=homoeostatic model assessment for insulin resistance; RCT=randomised controlled trial; RR=risk ratio.
Patient or population: people with and without diabetes; setting: these are long term trials, so participants live in the community; intervention: high total PUFA; comparison: low total PUFA.
Risk in intervention group (and its 95% CI) is based on assumed risk in comparison group and relative effect of intervention (and its 95% CI). Note that GRADE describes risk and 95% CI without using negative numbers; for example, GRADE states “0.02% lower (0.07 lower to 0.04 higher),” which would normally be described as “–0.02% (−0.07% to 0.04%).”
High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect.
a. Risk of bias: no studies were at low summary risk of bias or at low risk from compliance problems. Downgraded once.
b. Imprecision: 4481 participants in 3 RCTs, 175 diagnoses; 95% CI did not exclude important benefits or harms. Downgraded twice.
c. Risk of bias: lack of effect consistent in fixed effects analysis, and sensitivity analyses on concentration, but no included trials were at low summary risk of bias. Downgraded once.
d. Imprecision: 95% CI does not exclude important harms or benefits. Downgraded once.
e. Risk of bias: effect did not alter with fixed effects analysis; the single study at low risk from compliance suggested a small reduction in glucose with increased PUFA, but no trials were at low summary risk of bias or had low risk from allocation concealment. Downgraded once.
f. Imprecision: data based on 182 participants in 3 trials; 95% CI does not exclude important benefits or harms. Downgraded once.
g. Imprecision: data reflect a single study in 93 participants (a small proportion of the participants in the whole study); 95% CI does not exclude important harm. Downgraded once.
h. Risk of bias: effect not altered in fixed effects analysis, but the single study was not at low risk from summary risk of bias or compliance. Downgraded once.
i. Indirectness: subgroup of a single trial reported. Downgraded once.
Secondary outcomes
Secondary outcomes were planned as serum lipids, adiposity, all cause mortality, and mortality due to diabetes. However, as effects of omega-3, omega-6, and total PUFA on mortality, lipids, and adiposity were formally systematically reviewed in sister reviews assessing effects in randomised controlled trials of at least 12 months’ duration,29 33 34 secondary outcomes for this review are reported only in supplementary tables M, N, T, and Z. We found no data on mortality due to diabetes.
Discussion
Long chain omega-3 fats seem to have little or no effect on type 2 diabetes or measures of glucose metabolism including insulin resistance (measured using HOMA-IR), glycated haemoglobin (HbA1c), fasting glucose, or insulin. Although effects of α-linolenic acid, omega-6, and total PUFA on diagnosis of diabetes were unclear (as the evidence was of very low quality), we found little or no effect on measures of glucose metabolism, except that increasing α-linolenic acid may increase fasting insulin (low quality evidence). We found no evidence that the omega-3/omega-6 ratio is important to type 2 diabetes mellitus or glucose metabolism.
Strengths and limitations of study
Strengths of this review include its large size (including 81 trials, with more than 95 000 randomised participants with and without diabetes, from around the world), and searching of multiple databases. Creation of a dataset of randomised controlled trials regardless of outcomes and contacting authors to request relevant data allowed inclusion of data that would otherwise have been missed or remained unpublished (particularly for diagnosis of diabetes in populations not at high risk) and also allowed us to identify the extent and sometimes the import of missing data. Our data make it clear that missing data may be a serious threat to our understanding in this review. For example, we included 48 comparisons in the meta-analysis assessing effects of long chain omega-3 on plasma glucose, but we are aware of 15 further trials with data that could not be included. This volume of missing data could considerably alter the findings of the review. Missing data sprang from trials providing some information but not offering useable variance data, trials unbalanced at baseline, provision of medians or geometric means, and trials that clearly assessed our outcomes but provided no useable data. Weaknesses of the review include limited data on effects of increasing α-linolenic acid, omega-6, and total PUFA, as well as potentially serious risk of bias in many included trials. We did not find evidence of the importance of the omega-3/omega-6 ratio, but limiting to trials comparing increased omega-3 fats with increased omega-6 limits the quantity of data (reducing our power to see any effect) and the quality (only one of the included trials was at low summary risk of bias) of the available information. Additionally, doses of omega-6 were often small, so we could be missing important effects of the ratio. Long chain omega-3 results included mostly supplementation trials, which precluded fair assessment of effects of increasing oily fish consumption. Only 10 of 83 included randomised controlled trials were at low summary risk of bias. As poorly concealed allocation is associated with a 40% greater effect size,56 and lack of blinding with additional bias,57 58 caution is needed in interpreting small effects in weaker trials.
Dose and duration effects (subgrouping)
Although subgrouping by dose did not suggest statistically significant differences between subgroups for any outcome, point estimates suggested worse outcomes for all outcomes at doses above 4.4 g/d and some outcomes at doses above 2.4 g/d long chain omega-3, suggesting that high doses may have negative effects in diabetes (but this should be interpreted with caution). We found no suggestions of greater positive or negative effects of long chain omega-3 at longer durations, by replacement, by risk of diabetes, or by intervention type such as dietary advice, food supplements, or supplementary capsules, as would be expected if different matrix effects were present.59
Comparison with other studies
The most recent Cochrane review assessing effects of omega-3 on diabetes included 23 randomised controlled trials that randomised 1075 adults with diagnosed diabetes and had a mean duration of nine weeks.31 It suggested that increasing omega-3 reduced triglycerides, increased low density lipoprotein cholesterol, and did not alter HbA1c, fasting glucose, insulin, or body weight. It found insufficient events to assess mortality, results reiterated by a later review.32 Our review updates, extends, and partially confirms these findings, but no previous reviews of randomised controlled trials have assessed effects of increasing omega-3 on diagnosis of diabetes. Results of cohort study results are mixed, with some suggesting protection, some harm, and others no effect of omega-3, or fish, on risk of diabetes.60 61 62 A systematic review of recent randomised controlled trial and observational data found inconclusive evidence for associations between omega-3 and type 2 diabetes mellitus.63 Geographical differences may exist, relating to fat type, fat quality, or background intake,28 but these were not assessed in our review. Systematic review of observational studies suggests that higher circulating α-linolenic acid was non-significantly associated with lower risk of diabetes (relative risk per 0.1% total fatty acid 0.90, 0.80 to 1.00), and circulating concentration (relative risk per 3% total fatty acids 0.94, 0.75 to 1.17) and intake (relative risk per 250 mg/d 1.04, 0.97 to 1.10) of eicosapentaenoic acid and docosahexaenoic acid were not associated with risk of diabetes.64
Although we found little suggestion that long chain omega-3 harms glucose metabolism except perhaps at very high doses, the recently completed ASCEND trial reported complications of diabetes in 33 of 7740 participants with type 2 diabetes mellitus taking 0.84 g/d long chain omega-3 over more than seven years and 20 of 7740 taking placebo (relative risk 1.65, 0.95 to 2.87).55 We hope that further details from this study of effects on glucose metabolism will be published soon.
We found limited data from randomised controlled trials on effects of omega-6 or total PUFA on diagnosis of diabetes. A consortium of 20 prospective cohort studies included 39 740 adults from 10 countries and found that higher biomarker linoleic acid was associated with 35% lower risk of type 2 diabetes mellitus (relative risk per interquartile range 0.65, 0.60 to 0.72).65 Data from the European Prospective Investigation into Cancer and Nutrition study associated both α-linolenic acid (hazard ratio per standard deviation 0.93, 0.88 to 0.98) and linoleic acid biomarkers (0.80, 0.77 to 0.83) with lower risk of type 2 diabetes mellitus; arachidonic acid and long chain omega-3 were not associated, but other omega-6 fatty acids were associated with higher risk.66 Replacing saturated fat with PUFA was associated with decreased total cholesterol and low density lipoprotein cholesterol, without associations with triglycerides, insulin, or glucose in another systematic review.63
Conclusions and policy implications
No convincing evidence suggests that altering intakes of long chain omega-3, α-linolenic acid, omega-6, or total PUFA alters glucose metabolism or risk of diabetes. Supplemental long chain omega-3 should not be encouraged for prevention or treatment of diabetes. Where supplementary long chain omega-3 is used to reduce triglyceride concentrations, or people with or at risk of type 2 diabetes mellitus choose to take supplementary long chain omega-3, doses below 4.4 g/d should be encouraged.
Unanswered questions and future research
Further randomised controlled trials of effects of α-linolenic acid, omega-6, oily fish, and total PUFA with rigorous methods (larger sample sizes, adequate and well reported allocation concealment and blinding, at least 12 months’ duration) on diagnosis of diabetes and measures of glucose metabolism would be helpful.
What is already known on this topic
Effects of omega-3, omega-6, and total polyunsaturated fatty acids on glucose metabolism and type 2 diabetes diagnosis are inconclusive
Experimental data have suggested that omega-3 worsens control of diabetes, and systematic reviews of observational studies suggest both benefit and harm
Omega-6 has been theorised to oppose effects of omega-3, and observational data have associated higher omega-6 with both improvement and worsening of glucose metabolism
What this study adds
Increasing long chain omega-3 had little or no effect on likelihood of diagnosis of diabetes or on glucose metabolism, with no difference by duration, baseline glucose metabolism, or nutrients replaced
There was a suggestion that high dose supplementation (>4.4 g/d) with long chain omega-3 may worsen glucose metabolism
Increasing α-linolenic acid, omega-6, and total polyunsaturated fatty acids had little or no effect on glucose metabolism, except that increasing α-linolenic acid may increase fasting insulin by about 7%
Acknowledgments
This review is one of a set of reviews conducted by the Polyunsaturated Fats and Health (PUFAH) Group. Members of the PUFAH Group are: Asmaa Abdelhamid, Sarah Ajabnoor, Faye Alabdulghafoor, Julii Brainard, Tracey J Brown, Daisy Donaldson, Lee Hooper, Oluseyi Florence Jimoh, Alex O’Brien, Fujian Song, Xia Wang, and Lauren Winstanley, Norwich Medical School, University of East Anglia; Lena Alkhudairy and Karen Rees, Warwick Medical School, University of Warwick; Priti Biswas, Katherine Deane, Sarah Hanson, and Gabrielle Thorpe, Health Sciences, University of East Anglia; Charlene Bridges and Nicole Martin, Cochrane Heart Group, University College London.
We thank all the authors of primary studies who kindly replied to our queries and where possible provided us with the best set of data available, including: D Kromhout, Wageningen University (AlphaOmega - ALA 2010; AlphaOmega - EPA+DHA 2010); Emily Chew, NIH (AREDS2 2014); Steen Bonnema, Odense University Hospital (Bonnema 1995); C Argo, University of Virginia (Caldwell 2011); Gerald E Lobley, The Rowett Institute of Nutrition and Health, University of Aberdeen (Clark 2016); W E Connor, Oregon Health Sciences University (Connor 1993); M L Burr, University of Wales, and A Ness, University of Bristol (DART 1989; DART2 2003); Laura F DeFina, Cooper Institute, Dallas (DeFina 2010); Daniel A de Luis Román, University of Valladolid (de Luis 2016); G Derosa and P Maffioli, University of Pavia (Derosa 2011 and 2016); P N M Demacker, University Hospital Nijmegen (Deslypere 1992); S Tokudome, National Institute of Health and Nutrition, Japan (DIPP 2015); G Einvik, Akershus University Hospital, and H Arnesen, Oslo University Hospital (DO IT 2010); S Dodin, Universite Laval (Dodin 2005); R P F Dullaart, University of Groningen, Netherlands (Dullaart 1992); A Sanyal, Virginia Commonwealth University, USA (EPE-A 2014); Vanessa Danthir, CSIRO Human Nutrition, Adelaide (EPOCH 2014); Hossein Fakhrzadeh, Tehran University of Medical Sciences (Fakhrzadeh 2010); Angela Rivellese, Institute of Internal Medicine and Metabolic Diseases, Naples (IFOMS 1997); D Nilsen, University of Bergen, Norway (OFAMI 2001); A Dangour, London School of Hygiene and Tropical Medicine (OPAL 2010); H Gerstein, McMaster University, Canada (ORIGIN 2012); M James, Royal Adelaide Hospital, Australia (Proudman 2015); C Roncaglioni and I Marzona, IRCCS-Istituto di Ricerche Farmacologiche Mario Negri, Italy (Risk and Prevention 2013); A Manni, Penn State College of Medicine, USA (Sandhu 2016); Hiroyuki Shimizu, Gunna University Hospital, Japan (Shimizu 1995); J Eritsland, Oslo University Hospital, Norway (SHOT 1996); L Tapsell, M Batterham, and E Neale, University of Wollongong, Australia (SMART 2013); K Tande, Calanus AS, Norway (Tande 2016); Linda Tapsell, University of Wollongong (Tapsell 2004); K Tuttle, Sacred Heart Medical Center, Spokane (THIS DIET 2008); M Vijayakumar, Amrita Institute of Medical Sciences, India (Vijayakumar 2014); E Scorletti, University of Southampton, UK (WELCOME 2015).
Web extra.
Extra material supplied by authors
Supplementary materials
Contributors: TJB, FS, XW, and LH designed the study in consultation with the funder. LH and AA built the search. All authors and other members of the PUFAH Group screened studies and trial registers for eligibility and extracted data. JSB, LH, AA, and TJB inputted data to RevMan, did the statistical analysis, and interpreted the results. JSB, TJB, and LH wrote the first draft of the manuscript. LH did the GRADE analysis and assembled revisions. All authors read and approved the final version. All authors had full access to all data (primary publications, trials registry entries, trial author communications, data extractions and assessments of risk of bias, and analyses) and take responsibility for the integrity and accuracy of the data. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. LH is the guarantor.
Funding: The set of reviews was commissioned by the World Health Organization’s Nutrition Guidance Expert Advisory Group (NUGAG) Subgroup on Diet and Health, to inform its guidance on polyunsaturated fatty acid intake. The subgroup requested specific inclusion criteria (including duration of trials and outcomes), some sensitivity analyses, and subgroups. The results of the reviews, including GRADE assessments, were discussed and reviewed by the WHO NUGAG Subgroup on Diet and Health as part of WHO’s guideline development process. WHO was not otherwise involved in writing this report.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: all authors had financial support via the University of East Anglia from the World Health Organization for the submitted work, and LH and AA were funded to attend WHO meetings and present review results; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Not needed.
Transparency declaration: The lead author (the manuscript’s guarantor) affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Data sharing: We are happy to share our database of trials and have published a companion paper detailing this database.36
Contributor Information
Collaborators: PUFAH Group, Asmaa Abdelhamid, Sarah Ajabnoor, Faye Alabdulghafoor, Lena Alkhudairy, Priti Biswas, Julii Brainard, Charlene Bridges, Tracey J Brown, Katherine Deane, Daisy Donaldson, Sarah Hanson, Lee Hooper, Oluseyi Florence Jimoh, Nicole Martin, Alex O’Brien, Karen Rees, Lena Alkhudairy, Fujian Song, Gabrielle Thorpe, Xia Wang, and Lauren Winstanley
References
- 1. World Health Organization Global Report on Diabetes. WHO, 2016. [Google Scholar]
- 2. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1545-602. 10.1016/S0140-6736(16)31678-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Seuring T, Archangelidi O, Suhrcke M. The Economic Costs of Type 2 Diabetes: A Global Systematic Review. Pharmacoeconomics 2015;33:811-31. 10.1007/s40273-015-0268-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2014;37(Suppl 1):S81-90. 10.2337/dc14-S081 [DOI] [PubMed] [Google Scholar]
- 5. American Diabetes Association 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2019 . Diabetes Care 2019;42(Suppl 1):S13-28. 10.2337/dc19-S002 [DOI] [PubMed] [Google Scholar]
- 6. GBD 2016 Risk Factors Collaborators Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1345-422. 10.1016/S0140-6736(17)32366-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nutrition Science Team Government Dietary Recommendations: Government recommendations for energy and nutrients for males and females aged 1 – 18 years and 19+ years. Public Health England, 2016. [Google Scholar]
- 8. Scientific Advisory Committee on Nutrition, Committee on Toxicity Advice on fish consumption: benefits and risks. The Stationary Office, 2004. [Google Scholar]
- 9. National Institute for Health and Care Excellence Cardiovascular disease: risk assessment and reduction, including lipid modification. NICE, 2014. [PubMed] [Google Scholar]
- 10. American Diabetes Association 5. Lifestyle Management: Standards of Medical Care in Diabetes-2019 . Diabetes Care 2019;42(Suppl 1):S46-60. 10.2337/dc19-S005 [DOI] [PubMed] [Google Scholar]
- 11.National Institute for Health and Care Excellence. Preventing type 2 diabetes overview. 2018. https://pathways.nice.org.uk/pathways/preventing-type-2-diabetes#path=view%3A/pathways/preventing-type-2-diabetes/preventing-type-2-diabetes-overview.xml&content=view-index.
- 12.American Heart Association. Fish and Omega-3 Fatty Acids.2017. https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/fats/fish-and-omega-3-fatty-acids.
- 13. GBD 2017 Diet Collaborators Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019;393:1958-72. 10.1016/S0140-6736(19)30041-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Public Health England Statistical Summary: National Diet and Nutrition Survey: Years 1 to 9 of the Rolling Programme (2008/09 – 2016/17): Time trend and income analyses. Public Health England, 2019. [Google Scholar]
- 15. Public Health England National Diet and Nutrition Survey Results from Years 7 and 8 (combined) of the Rolling Programme (2014/2015 to 2015/2016). Public Health England, 2018. [Google Scholar]
- 16. Papanikolaou Y, Brooks J, Reider C, Fulgoni VL., 3rd U.S. adults are not meeting recommended levels for fish and omega-3 fatty acid intake: results of an analysis using observational data from NHANES 2003-2008. Nutr J 2014;13:31. 10.1186/1475-2891-13-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Glauber H, Wallace P, Griver K, Brechtel G. Adverse metabolic effect of omega-3 fatty acids in non-insulin-dependent diabetes mellitus. Ann Intern Med 1988;108:663-8. 10.7326/0003-4819-108-5-663 [DOI] [PubMed] [Google Scholar]
- 18. Vessby B, Karlström B, Boberg M, Lithell H, Berne C. Polyunsaturated fatty acids may impair blood glucose control in type 2 diabetic patients. Diabet Med 1992;9:126-33. 10.1111/j.1464-5491.1992.tb01748.x [DOI] [PubMed] [Google Scholar]
- 19. Bourdon JA, Bazinet TM, Arnason TT, Kimpe LE, Blais JM, White PA. Polychlorinated biphenyls (PCBs) contamination and aryl hydrocarbon receptor (AhR) agonist activity of Omega-3 polyunsaturated fatty acid supplements: implications for daily intake of dioxins and PCBs. Food Chem Toxicol 2010;48:3093-7. 10.1016/j.fct.2010.07.051 [DOI] [PubMed] [Google Scholar]
- 20. Levine KE, Levine MA, Weber FX, Hu Y, Perlmutter J, Grohse PM. Determination of mercury in an assortment of dietary supplements using an inexpensive combustion atomic absorption spectrometry technique. J Autom Methods Manag Chem 2005;2005:211-6. 10.1155/JAMMC.2005.211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chen YW, Huang CF, Tsai KS, et al. The role of phosphoinositide 3-kinase/Akt signaling in low-dose mercury-induced mouse pancreatic β-cell dysfunction in vitro and in vivo. Diabetes 2006;55:1614-24. 10.2337/db06-0029 [DOI] [PubMed] [Google Scholar]
- 22. Lee D-H, Lee I-K, Song K, et al. A strong dose-response relation between serum concentrations of persistent organic pollutants and diabetes: results from the National Health and Examination Survey 1999-2002. Diabetes Care 2006;29:1638-44. 10.2337/dc06-0543 [DOI] [PubMed] [Google Scholar]
- 23. Ruidavets J-B, Bongard V, Dallongeville J, et al. High consumptions of grain, fish, dairy products and combinations of these are associated with a low prevalence of metabolic syndrome. J Epidemiol Community Health 2007;61:810-7. 10.1136/jech.2006.052126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Harding AH, Day NE, Khaw KT, et al. Habitual fish consumption and glycated haemoglobin: the EPIC-Norfolk study. Eur J Clin Nutr 2004;58:277-84. 10.1038/sj.ejcn.1601779 [DOI] [PubMed] [Google Scholar]
- 25. Zhou Y, Tian C, Jia C. Association of fish and n-3 fatty acid intake with the risk of type 2 diabetes: a meta-analysis of prospective studies. Br J Nutr 2012;108:408-17. 10.1017/S0007114512002036 [DOI] [PubMed] [Google Scholar]
- 26. Li D. Omega-3 polyunsaturated fatty acids and non-communicable diseases: meta-analysis based systematic review. Asia Pac J Clin Nutr 2015;24:10-5. [DOI] [PubMed] [Google Scholar]
- 27. Zheng JS, Huang T, Yang J, Fu YQ, Li D. Marine N-3 polyunsaturated fatty acids are inversely associated with risk of type 2 diabetes in Asians: a systematic review and meta-analysis. PLoS One 2012;7:e44525. 10.1371/journal.pone.0044525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wallin A, Di Giuseppe D, Orsini N, Patel PS, Forouhi NG, Wolk A. Fish consumption, dietary long-chain n-3 fatty acids, and risk of type 2 diabetes: systematic review and meta-analysis of prospective studies. Diabetes Care 2012;35:918-29. 10.2337/dc11-1631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Abdelhamid AS, Brown TJ, Brainard JS, et al. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev 2018;(11):CD003177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Simopoulos AP, DiNicolantonio JJ. The importance of a balanced ω-6 to ω-3 ratio in the prevention and management of obesity. Open Heart 2016;3:e000385. 10.1136/openhrt-2015-000385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hartweg J, Perera R, Montori V, Dinneen S, Neil HA, Farmer A. Omega-3 polyunsaturated fatty acids (PUFA) for type 2 diabetes mellitus. Cochrane Database Syst Rev 2008;(1):CD003205. 10.1002/14651858.CD003205.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chen C, Yu X, Shao S. Effects of Omega-3 Fatty Acid Supplementation on Glucose Control and Lipid Levels in Type 2 Diabetes: A Meta-Analysis. PLoS One 2015;10:e0139565. 10.1371/journal.pone.0139565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Abdelhamid AS, Martin N, Bridges C, et al. Polyunsaturated fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev 2018;(11):CD012345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hooper L, Al-Khudairy L, Abdelhamid AS, et al. Omega-6 fats for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev 2018;(11):CD011094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Abdelhamid A, Hooper L, Sivakaran R, Hayhoe RPG, Welch A, PUFAH Group The Relationship Between Omega-3, Omega-6 and Total Polyunsaturated Fat and Musculoskeletal Health and Functional Status in Adults: A Systematic Review and Meta-analysis of RCTs. Calcif Tissue Int 2019. 10.1007/s00223-019-00584-3 [DOI] [PubMed] [Google Scholar]
- 36. Hooper L, Abdelhamid A, Brainard J, et al. Creation of a database to assess effects of omega-3, omega-6 and total polyunsaturated fats on health: methodology for a set of reviews. BMJ Open 2019;9:e029554. 10.1136/bmjopen-2019-029554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thorpe G, Ajabnoor S, Ahmed Z, et al. Dietary polyunsaturated fat for prevention and treatment of inflammatory bowel disease. 2017. http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017068704.
- 38.Hanson S, Thorpe G, Winstanley L, et al. Effects of supplementary dietary polyunsaturated fat on cancer incidence. 2017. http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017056109.
- 39.Brown T, Song F, Wang X, et al. Dietary polyunsaturated fat for prevention and treatment of type 2 diabetes mellitus. 2017. http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017064110.
- 40. Higgins JP, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. [Google Scholar]
- 41. Atkins D, Best D, Briss PA, et al. GRADE Working Group Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490. 10.1136/bmj.328.7454.1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Browning LM, Walker CG, Mander AP, et al. Incorporation of eicosapentaenoic and docosahexaenoic acids into lipid pools when given as supplements providing doses equivalent to typical intakes of oily fish. Am J Clin Nutr 2012;96:748-58. 10.3945/ajcn.112.041343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Higgins JP, Altman DG, Sterne JA, et al. Chapter 8: Assessing risk of bias in included studies In: Higgins JP, Green S, eds. Cochrane handbook for systematic reviews of interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. [Google Scholar]
- 44. McKenzie JE, Herbison GP, Deeks JJ. Impact of analysing continuous outcomes using final values, change scores and analysis of covariance on the performance of meta-analytic methods: a simulation study. Res Synth Methods 2016;7:371-86. 10.1002/jrsm.1196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kromhout D, Giltay EJ, Geleijnse JM, Alpha Omega Trial Group n-3 fatty acids and cardiovascular events after myocardial infarction. N Engl J Med 2010;363:2015-26. 10.1056/NEJMoa1003603 [DOI] [PubMed] [Google Scholar]
- 47. Bonds DE, Harrington M, Worrall BB, et al. Writing Group for the AREDS2 Research Group Effect of long-chain ω-3 fatty acids and lutein + zeaxanthin supplements on cardiovascular outcomes: results of the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA Intern Med 2014;174:763-71. 10.1001/jamainternmed.2014.328 [DOI] [PubMed] [Google Scholar]
- 48. Caldwell SH, Argo CK, Henry TD, et al. Dissociated histological and metabolic effects of omega-3 (3000 mg/d) versus placebo with both exercise and diet in a double-blind randomized controlled trial of NASH. J Hepatol 2011;54:S8 10.1016/S0168-8278(11)60019-6 . [DOI] [Google Scholar]
- 49. Derosa G, Cicero AF, D’Angelo A, Borghi C, Maffioli P. Effects of n-3 pufas on fasting plasma glucose and insulin resistance in patients with impaired fasting glucose or impaired glucose tolerance. Biofactors 2016;42:316-22. [DOI] [PubMed] [Google Scholar]
- 50. Danthiir V, Burns NR, Nettelbeck T, Wilson C, Wittert G. The older people, omega-3, and cognitive health (EPOCH) trial design and methodology: a randomised, double-blind, controlled trial investigating the effect of long-chain omega-3 fatty acids on cognitive ageing and wellbeing in cognitively healthy older adults. Nutr J 2011;10:117. 10.1186/1475-2891-10-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Dangour AD, Allen E, Elbourne D, et al. Effect of 2-y n-3 long-chain polyunsaturated fatty acid supplementation on cognitive function in older people: a randomized, double-blind, controlled trial. Am J Clin Nutr 2010;91:1725-32. 10.3945/ajcn.2009.29121 [DOI] [PubMed] [Google Scholar]
- 52. Bosch J, Gerstein HC, Dagenais GR, et al. ORIGIN Trial Investigators n-3 fatty acids and cardiovascular outcomes in patients with dysglycemia. N Engl J Med 2012;367:309-18. 10.1056/NEJMoa1203859 [DOI] [PubMed] [Google Scholar]
- 53. Proudman SM, Cleland LG, Metcalf RG, Sullivan TR, Spargo LD, James MJ. Plasma n-3 fatty acids and clinical outcomes in recent-onset rheumatoid arthritis. Br J Nutr 2015;114:885-90. 10.1017/S0007114515002718 [DOI] [PubMed] [Google Scholar]
- 54. Scorletti E, Bhatia B, McCormick KG, et al. Potential benefits of purified long chain omega-3 fatty acid treatment in non-alcoholic fatty liver disease (NAFLD): A potential treatment for early NAFLD in metabolic syndrome and Type 2 diabetes. Results from the WELCOME study. Diabet Med 2014;31:1. [Google Scholar]
- 55. Bowman L, Mafham M, Wallendszus K, et al. ASCEND Study Collaborative Group Effects of n-3 Fatty Acid Supplements in Diabetes Mellitus. N Engl J Med 2018;379:1540-50. 10.1056/NEJMoa1804989 [DOI] [PubMed] [Google Scholar]
- 56. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408-12. 10.1001/jama.1995.03520290060030 [DOI] [PubMed] [Google Scholar]
- 57. Savović J, Jones H, Altman D, et al. Influence of reported study design characteristics on intervention effect estimates from randomised controlled trials: combined analysis of meta-epidemiological studies. Health Technol Assess 2012;16:1-82. 10.3310/hta16350 [DOI] [PubMed] [Google Scholar]
- 58. Wood L, Egger M, Gluud LL, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ 2008;336:601-5. 10.1136/bmj.39465.451748.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Thorning TK, Bertram HC, Bonjour JP, et al. Whole dairy matrix or single nutrients in assessment of health effects: current evidence and knowledge gaps. Am J Clin Nutr 2017;105:1033-45. 10.3945/ajcn.116.151548 [DOI] [PubMed] [Google Scholar]
- 60. Alhazmi A, Stojanovski E, McEvoy M, Garg ML. Macronutrient intake and type 2 diabetes risk in middle-aged Australian women. Results from the Australian Longitudinal Study on Women’s Health. Public Health Nutr 2014;17:1587-94. 10.1017/S1368980013001870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Djoussé L, Gaziano JM, Buring JE, Lee IM. Dietary omega-3 fatty acids and fish consumption and risk of type 2 diabetes. Am J Clin Nutr 2011;93:143-50. 10.3945/ajcn.110.005603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Patel PS, Forouhi NG, Kuijsten A, et al. InterAct Consortium The prospective association between total and type of fish intake and type 2 diabetes in 8 European countries: EPIC-InterAct Study. Am J Clin Nutr 2012;95:1445-53. 10.3945/ajcn.111.029314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Schwab U, Lauritzen L, Tholstrup T, et al. Effect of the amount and type of dietary fat on cardiometabolic risk factors and risk of developing type 2 diabetes, cardiovascular diseases, and cancer: a systematic review. Food Nutr Res 2014;58. 10.3402/fnr.v58.25145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Wu JHY, Micha R, Imamura F, et al. Omega-3 fatty acids and incident type 2 diabetes: a systematic review and meta-analysis. Br J Nutr 2012;107(Suppl 2):S214-27. 10.1017/S0007114512001602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Wu JHY, Marklund M, Imamura F, et al. Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) Fatty Acids and Outcomes Research Consortium (FORCE) Omega-6 fatty acid biomarkers and incident type 2 diabetes: pooled analysis of individual-level data for 39 740 adults from 20 prospective cohort studies. Lancet Diabetes Endocrinol 2017;5:965-74. 10.1016/S2213-8587(17)30307-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Forouhi NG, Imamura F, Sharp SJ, et al. Association of Plasma Phospholipid n-3 and n-6 Polyunsaturated Fatty Acids with Type 2 Diabetes: The EPIC-InterAct Case-Cohort Study. PLoS Med 2016;13:e1002094. 10.1371/journal.pmed.1002094 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary materials