Abstract
Purpose
Adolescents and young adults (AYAs) with cancer are known to have complex medical and psychosocial needs throughout treatment; however, information is lacking about the challenges AYA survivors face after treatment has ended. Focus groups were conducted using a concept mapping framework to better understand the most important issues these patients face in transitioning to survivorship and how prepared they felt to face them.
Methods
AYAs diagnosed between 18 and 39 years old and at least two years post-treatment participated in one of six focus groups based on age group and follow-up status. Using a concept mapping design, participants provided important issues during the transition to survivorship and appraised them on three core areas of interest.
Results
Analyses revealed salient themes shared across age and follow-up group status, particularly related to the psychosocial, emotional, and cognitive effects of treatment. Differential concerns included those related to patients’ developmental concerns – namely, finding a new identity, financial burden of treatment, and fertility concerns after treatment.
Conclusions
AYA cancer survivors continue to have a myriad of issues beyond the immediate treatment phase. Despite a complex list of challenges, these issues largely remained unaddressed by their oncology provider and left patients feeling overwhelmingly ill-prepared to manage their transition to survivorship.
Implications for Cancer Survivors
AYA cancer survivors have many unaddressed concerns as they transition out of active cancer treatment, largely related to developmental issues they are facing. Survivorship care for these patients would benefit from care planning that takes these unique concerns into account.
Keywords: adolescents and young adults, cancer, cancer survivors, concept mapping, oncology, survivorship
Background
The diagnosis and treatment of cancer is a life-changing time for most people, and can result in a wide array of physical, emotional, and practical changes for patients. There are currently over 12 million survivors of cancer, and the complexities of cancer survivorship are becoming increasingly better understood in adult populations. Within this adult population, however, are approximately 500,000 adolescents and young adults (AYAs), aged 15 to 39, who are survivors of childhood or adult-onset cancers [1,2]. These patients often have unique life circumstances that make their survivorship concerns quite different from their older counterparts. They may be just reaching developmental milestones of graduating school, attending college, starting their career, dating and marriage, or having children.
AYAs are often at high-risk for medical and psychosocial sequelae from cancer and its treatment [3–7]. Indeed, AYAs who survive cancer for more than 5 years have a higher relative risk of a secondary malignant neoplasm (SMN) compared with the general population and have a higher absolute risk of SMN compared with younger or older cancer survivors [8]. Unlike older patients, they may have concerns about fertility [9,10] and how/if they will be able to have children of their own after treatment. They are often more dependent on parents compared to their peers [11], and have difficulties in intimate relationships or obtaining full-time employment [10,12]. Young cancer patients have lower levels of well-being compared to other age groups [13,14], and have been reported to experience anxiety due to many uncertainties when transitioning from active treatment into the survivorship phase [15].
Survivorship encompasses a myriad of issues that range from late and long-term effects from cancer treatment, risk of secondary malignancies, on-going psychosocial distress, to risk of recurrence. In 2005, a seminal report from the Institute of Medicine (IOM), “From Cancer Patient to Cancer Survivor: Lost in Transition”, highlighted the need to recognize survivorship as a distinct phase in cancer care and to address the concerns of survivors [16]. The IOM strongly recommended that all patients receive at the completion of therapy a customized treatment summary and a survivorship care plan (SCP) that details a plan of ongoing care, including follow-up schedules for visits and testing, as well as recommendations for early detection and management of treatment-related effects (i.e., pain, fatigue, premature menopause, depression/anxiety) and other health problems. And yet, the majority of young adult survivors receive inadequate survivorship care with minimal surveillance for late effects [7,17].
Adherence to surveillance and follow-up care has been largely unexplored in this population. It is known that rates of treatment non-adherence are high, ranging from 27% to 60% [18,19] and are likely higher than in any other cancer population [20,21]. These issues point to the need to better understand the salient concerns and of this vulnerable population as they transition to survivorship, with the goal of improving survivorship care for AYAs by understanding and working to dismantle potential barriers to follow-up adherence.
This pilot study aimed to explore these survivorship concerns through a concept mapping analysis. Concept mapping relies on the premise that patients are the true ‘experts’ on their own experience, and uses an inductive approach to capture and analyze this experience through quantitative methods. We aimed to better understand the most salient concerns of AYAs as they transitioned from active treatment to survivorship, how well they felt that these concerns were addressed in their care, and how prepared they felt in dealing with these concerns. Participants were young adult cancer survivors of adult-onset malignancies at a single National Cancer Institute (NCI)/National Comprehensive Cancer Network (NCCN)-designated cancer center using a focus group approach.
Methods
This study utilized 6 focus groups to explore the salient concerns of AYAs during their transition to survivorship. To examine potential age-group differences survivors were stratified by age at diagnosis: 18–24, 25–30, or 31–39 years old. In addition, we examined group differences based on whether patients continued their recommended follow-up at our center or if they had been lost to follow-up ( i.e., did not adhere to suggested follow-up schedule within one calendar year from the date of the study’s recruitment).
Eligibility criteria included survivors who: 1) were diagnosed between 18 and 39 years of age, 2) were diagnosed between January 1, 2005 to December 31, 2011, 3) received all of their treatment at our center, 4) completed their planned cancer treatment, and 5) are currently living. Our institutional Tumor Registry identified 1,327 patients (827 female, 500 male) who fit the age and timeframe of diagnosis criteria for this study. Using the electronic medical record, a research associate verified how many of these potential participants met criteria 3–5 noted above. Eligible survivors were mailed a letter informing them of the study and inviting them to participate. This letter was followed up with a phone call of the same nature. This study was reviewed and approved by our hospital’s Institutional Review Board - IRB# I-253014. Written informed consent was obtained by all individual participants included in the study.
Focus groups.
Participants were stratified by age at diagnosis and follow-up status (survivors who continued to follow-up and those who no longer followed-up). These two groups were then divided by participants’ age at diagnosis: 18–24, 25–30, or 31–39. Groups were designated with labels A, B, C to designate follow-up groups, and AA, BB, CC to designate non-follow-up groups. Using a concept mapping framework, patients were asked to brainstorm responses to a prompt statement regarding important issues during the transition from active treatment to survivorship. Participants generated as many statements as they could. During a short break, all statements were written individually on 3×5 index cards.
The next phase of data generation involved participants grouping all statements into “piles that make sense to you.” They were asked to generate as many groups as they felt were necessary, to not put all cards into one group, or each card into a separate group. After all groupings were completed, participants were asked to label each group with a title or statement that captured the essence of that group.
The final phase of the focus group asked participants to rate each statement on a 1 (not at all) to 5 (very much) Likert scale on: Importance (how important was this issue to you during your transition to survivorship); Addressed (how well was this issue addressed in your medical care); and Prepared (how prepared did you feel in handling this issue as you transitioned to survivorship). The total time to complete all phases of brainstorming, sorting, and rating took approximately 90 minutes. Participants received a light breakfast during the focus group and a $50 honorarium for completion of the study.
Data analysis.
Data were analyzed using the Concept System Global Max program [22]. This analysis uses non-metric multidimensional scaling (MDS) to sort statements onto a two-dimensional point map, with those statements that are grouped together by participants being closer together and statements that are grouped together less frequently being further apart on the map. Next a cluster analysis was performed using the X-Y coordinates for each point to group statements into ‘clusters’ representing the underlying theme or structure of the grouping.
All focus groups were analyzed separately in an attempt to see whether group differences would appear according to age group or follow-up status. This resulted in 6 separate cluster analyses. Cluster solutions were examined for each focus group by examining solutions in reverse order and determining which cluster solution resulted in the least clusters while maintaining interpretability of the data. The most meaningful solution for each group was determined by consensus of the study authors as well as an additional research assistant not affiliated with the study who served as an outside validity check. Bridging values and stress values, indices of goodness-of-fit of the concept map, were also examined for each cluster solution. Lower bridging values (ranging from 0–1) indicate greater homogeneity of the cluster while lower stress values (ranging from 0.155 to 0.352) indicate a better fit. Means were calculated for each cluster theme on the Importance, Addressed, and Prepared domains. The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Results
Of 1,327 potential participants, 229 were eligible and 27 survivors participated in this study. Participant demographics are illustrated in Table 1. Six focus groups were conducted with group sizes ranging from 1–8 participants. The Brainstorming portion of each focus group resulted in an average of 46 statements (range 37–67) generated in each group. Analyses were conducted separately for each group in an effort to compare and contrast salient themes across age groups and follow-up status. Data for group CC are not included in analyses as only one survivor participated in this group.
Table 1.
Demographic information
| Follow-up (n= 19) | Non Follow-up (n= 8) | |
|---|---|---|
| Age at Diagnosis | ||
| 18–24 | 26% | 50% |
| 25–30 | 42% | 38% |
| 31–39 | 32% | 12% |
| Range | 18–39 | 20–36 |
| Mean | 28 | 26 |
| Gender | ||
| Male | 21% | 50% |
| Female | 79% | 50% |
| Employment Status | ||
| Full-time | 53% | 50% |
| Part-time | 21% | 25% |
| Disability | 16% | 25% |
| Stay-at-home parent | 10% | 0% |
| Race | ||
| African American | 0% | 12% |
| Asian | 5% | 0% |
| Caucasian | 95% | 75% |
| Other | 0% | 12% |
| Marital Status | ||
| Never Married | 42% | 75% |
| Married | 37% | 12% |
| Living with Partner | 10% | 12% |
| Divorced | 10% | 0% |
| Highest Level of Education | ||
| High School | 16% | 25% |
| Trade or Technical School | 5% | 0% |
| Some College | 11% | 13% |
| College | 26% | 37% |
| Postgraduate | 42% | 25% |
| Health Insurance | ||
| Insured | 100% | 100% |
| Uninsured | 0% | 0% |
| Treatment Received | ||
| Surgery | 74% | 63% |
| Chemotherapy | 58% | 50% |
| Radiation | 42% | 25% |
| Cancer Type | ||
| Leukemia/Lymphoma | 26% | 12% |
| Brain | 11% | 0% |
| Testicular | 0% | 12% |
| Gynecological | 21% | 12% |
| Thyroid | 10% | 25% |
| Other | 32% | 38% |
Multidimensional scaling and hierarchical cluster analysis.
Cluster solutions were examined for each focus group, with the most meaningful solutions ranging from 5–8 clusters. A sample cluster map is shown in Figure 1. For each group we aimed to find the cluster solution with the lowest bridging and stress values while also maintaining the integrity of the data.
Figure 1.
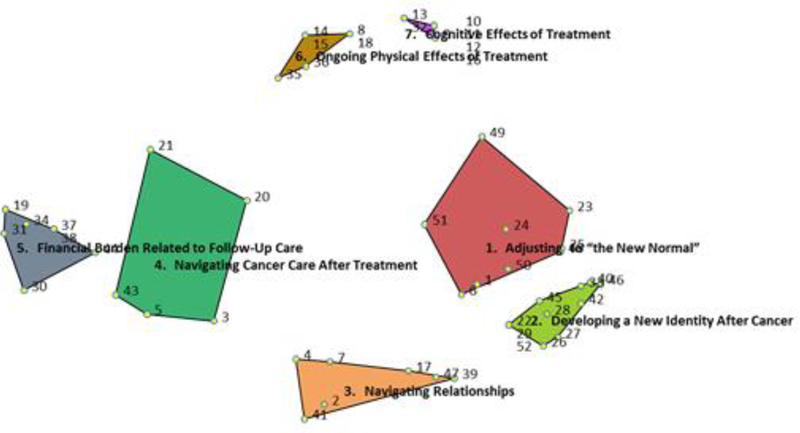
Sample concept map
The domains of Importance, Addressed, and Prepared are represented in Figure 2, with more layers on a cluster indicating a higher rating of that domain (i.e., more important, better addressed, or more prepared for). All sample figures represent data for Group B which was our largest focus group. The areas rated as most important for each group include: Group A - Factors impeding life goals; Group AA - Positive life changes after treatment; Group B - Developing a new identity; Group BB - Financial toxicity of treatment; Group C - Fears after cancer treatment. Areas participants rated as being least addressed in their transition to survivorship were: Group A - Navigating relationships; Group AA - Psychosocial difficulties; Group B - Cognitive effects of treatment; Group BB - Negative psychosocial effects of treatment; Group C - Physical effects of treatment. Finally, areas that participants rated as feeling least prepared for were: Group A - Post-treatment support; Group AA - Ongoing emotional effects of treatment; Group B - Cognitive effects of treatment; Group BB - Negative psychosocial effects of treatment; Group C - Physical effects of treatment.
Figure 2.
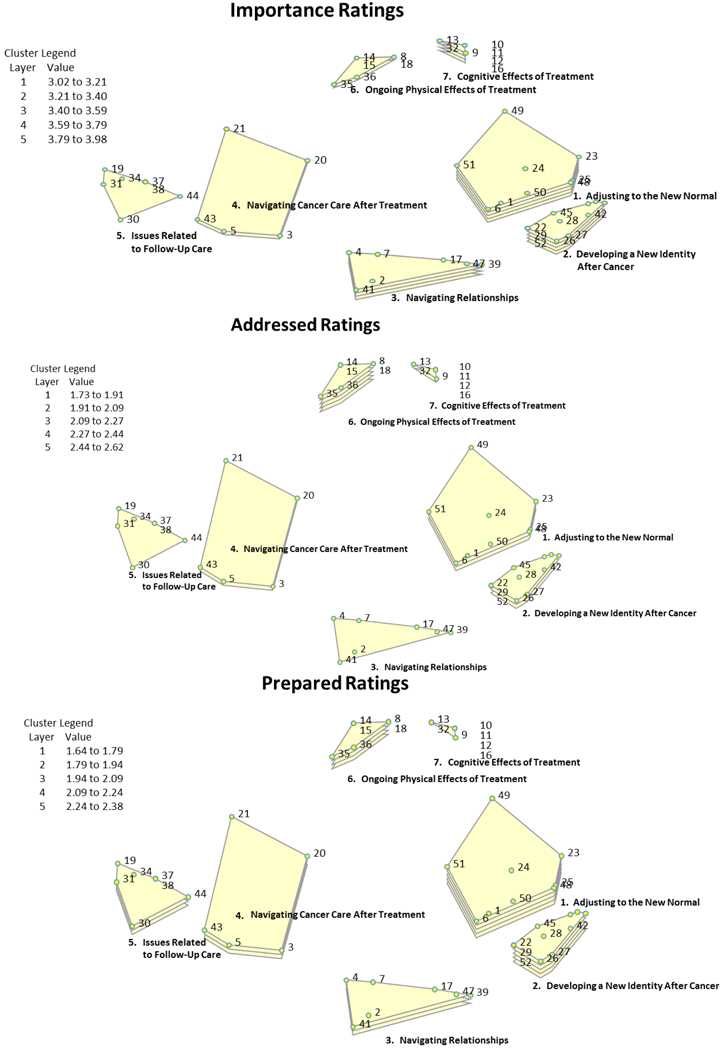
Sample concept maps of Importance, Addressed, and Prepared appraisal ratings. More layers indicate a higher rating of that domain.
For each of the five groups, analyses were conducted to compare how each concept map theme was rated on Importance versus Addressed, as well as comparisons of Importance versus Prepared. For every theme in each of the five groups, survivors rated each lower in Addressed versus Importance and lower in Prepared versus Importance with one exception - Group AA felt that “Adjusting to a new normal” was well-addressed in their care and they felt well-prepared to cope with this issue. Figure 3 shows comparisons of Importance versus Addressed appraisals, as well as Importance versus Prepared appraisals.
Figure 3.
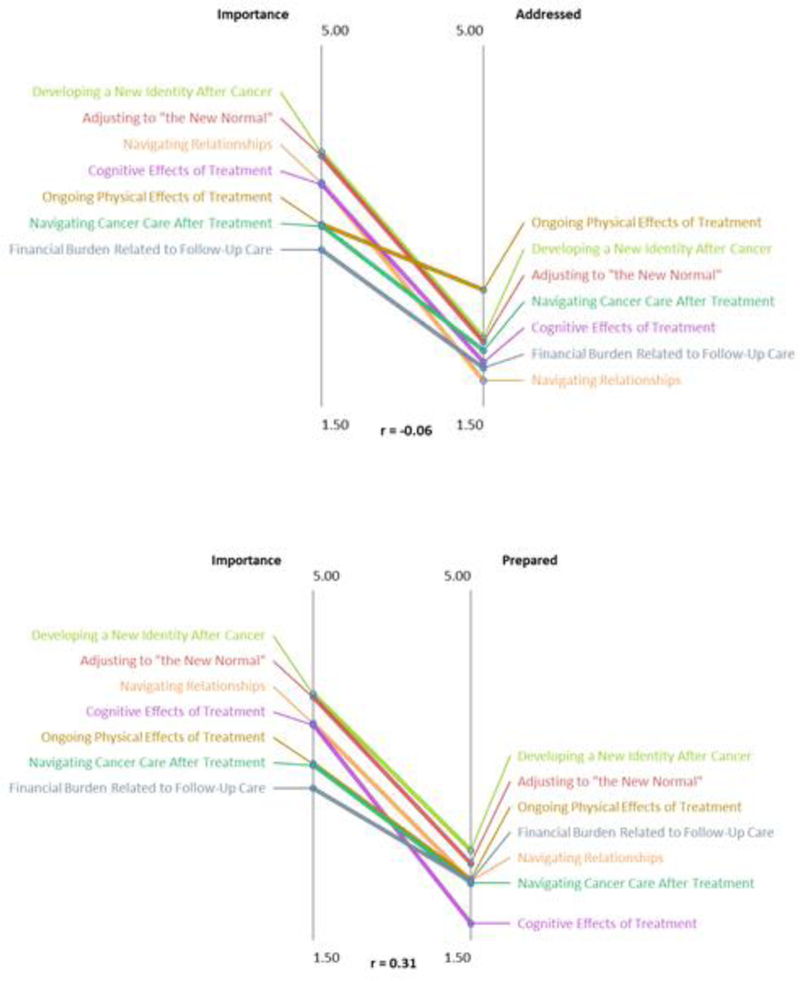
Sample comparisons of Importance versus Addressed appraisals and Importance versus Prepared appraisals
Group similarities and differences.
In an effort to examine how the salient concerns of each group may have compared and contrasted to one another, cluster map solutions were compared across all groups. Four key themes emerged that were similar across many groups: Ongoing effects of treatment (Physical/Emotional/Cognitive); Navigating follow-up care; Psychosocial concerns; and Adjusting to a new normal.
While many of our participants, regardless of age or follow-up status, expressed similar concerns in their adjustment to survivorship, a few novel concerns did emerge for certain groups, largely in line with developmental considerations for these patients. Concerns related to the financial burden of treatment were expressed by our 25–30 year old groups regardless of follow-up status, while issues related to fertility and family planning were expressed by groups BB and C. Issues related to maintaining independence and moving out of the patient role were expressed by Group BB, while factors impeding life goals and developing a new identity were expressed by Groups A and B (18–24 and 25–30 year old follow-up). Finally, group AA (18–24 year old follow-up) was the only group to describe positive life changes after treatment.
Conclusions
AYAs have complex medical and psychosocial needs throughout their cancer treatment that continue well after treatment ends [7, 23–25]. There are, however, no guidelines specific for this population regarding management of long-term treatment effects, monitoring for secondary malignancies, or preventative health measures. In contrast, pediatric cancer survivors have thorough survivorship guidelines available through the Children’s Oncology Group [26] and NCCN provides treatment and survivorship guidelines for adults [27]; however, neither specifically addresses concerns of AYAs.
Our data illustrate how AYAs continue to have many issues long after cancer treatment has ended that are related to the ongoing physical and psychosocial effects of treatment. Regardless of continued follow-up care after completing treatment, young adult cancer survivors face a myriad of issues which remain largely unaddressed by their oncologist or other healthcare provider. Though these issues vary in priority among age groups, late-effects from treatment, on-going psychosocial issues and navigating follow-up care were unifying themes. These emerging themes did not appear to relate to age group or whether continued oncology care was pursued.
Of particular interest in this study are the findings that differentiate a group of patients that are often lumped together under the AYA umbrella of 18–39 year olds. This age range encompasses a number of developmental milestones that many of their peers are moving through, yet AYAs are often delayed in achieving, if able to approach at all [28]. While many of the younger patients had concerns related to their dependence on parents, achieving life goals, and finding a new identity after cancer, our older patients described concerns related to the financial impact of treatment and issues related to family planning. Our middle group appeared to struggle the most with leaving the patient role and finding their bearings again, something that the youngest group may have had less difficulty with as they likely continued to be at least somewhat reliant on parents whereas the oldest group had firmly established their sense of adulthood before diagnosis. This group also struggled the most with the financial impact of their care, perhaps because younger patients remained on their parents’ insurance or received financial help and the oldest cohort had established insurance coverage through their own professions. In fact, the particular statements generated by this group include concerns about paying out-of-pocket for medical expenses, insurance issues, and trying to figure out job benefits. This age group had the largest mean discrepancies between issues rated as Important versus Addressed or Prepared, indicating that while their mean ratings for important issues were in line with other groups, they felt these concerns were the least addressed and they were the least prepared to deal with them compared to other age groups.
Another interesting finding relates to the positive life changes expressed by Group AA. They were the only group to share positive effects from treatment and shared quite a few - ‘Trying to see the good in life’; ‘Changed perspective on life’s problems’; ‘Feelings of gratitude’; and ‘Searching for meaning/purpose in life’. This group also ranked their concerns as being better addressed and being better able to manage them than other groups on average. This may help explain why this group did not seek follow-up care after treatment ended: a positive outlook may negate the concerns of recurrence and contribute to survivors not appreciating the importance of long-term follow-up.
Of particular concern is that while many of these concerns were rated as quite important to these survivors, they were also rated as issues that were ill-addressed in their cancer care and that they felt unprepared in coping with in survivorship. Each of the five groups expressed psychosocial concerns/navigating relationships as being an important issue for them, yet it was consistently rated as one of the least addressed areas in their care. Physical and cognitive effects of treatment were also rated as the least-addressed areas and ones that patients felt ill-prepared in coping with.
The lack of communication about these issues with healthcare providers suggest that as survivorship care plans (SCPs) evolve from theoretical documents to standards of care across cancer centers, they may be particularly beneficial for AYAs. A recent systematic review on psychosocial outcomes of AYAs found that their experiences are nuanced and meeting their informational needs and providing treatment-related education may improve their follow-up care [29]. As AYAs continue to have a significant fear of recurrence [30], tailored SCPs may have a role in providing the communication and knowledge to allay some of these fears. SCPs may provide a wealth of information regarding one’s own risks related to treatment, as well as health information addressing the many issues shared among AYAs. What is of particular importance is the need to tailor these SCPs to cover the most salient concerns for where a particular patient may be on their developmental trajectory. It is clear from these data that much more needs to be done to address the psychosocial, cognitive and emotional effects of cancer treatment, as well as providing education and resources for those experiencing financial toxicity of cancer care.
Study limitations.
The paucity of participants in some of the focus groups is a limitation, especially for Group CC. As noted in AYA oncology literature, enrolling AYAs onto clinical studies remains challenging [31]. Despite four survivors committing to participate in Focus Group CC, only one survivor participated which does not allow for interpretation of this group. Additionally, statistical interpretation of group differences is not possible due to small sample sizes.
Clinical implications.
AYA cancer survivors have long-lasting issues beyond the immediate post-therapy phase. AYAs desire more health information about their long-term risks associated with their cancer and treatment history, and they are dealing with ongoing psychosocial issues that may impede their personal growth and development as young adults. Communication with healthcare providers is key, and survivorship care plans specific for AYAs that are tailored to their developmental needs should be considered.
Acknowledgments:
This study was funded by Institutional Research Grant #IRG-02–197-09 from the American Cancer Society.
Funding: This study was funded by the American Cancer Society (Institutional Research Grant #IRG-02–197-09).
Appendix
Table 2.
Concept map bridging and stress values
| Group | Bridging values range | Average bridging value | Stress value |
|---|---|---|---|
| A | .08–.95 | ||
| .50 | .14 | ||
| AA | .33–.62 | ||
| .50 | .30 | ||
| B | .05–.77 | ||
| .37 | .20 | ||
| BB | .00–.71 | ||
| .37 | .29 | ||
| C | .07–.65 | ||
| .37 | .21 | ||
Table 3.
Mean appraisal ratings for all groups on three domains
| Group clusters | Mean (SD) | ||
|---|---|---|---|
| Importance | Addressed | Prepared | |
| A | |||
| Navigating follow-up care | 3.30 (0.56) | 2.45 (0.59) | 2.68 (0.59) |
| Need for post-treatment support | 3.47 (0.25) | 2.42 (0.28) | 2.47 (0.22) |
| Ongoing effects of treatment | 2.91 (0.66) | 2.36 (0.37) | 2.68 (0.39) |
| Factors impeding life goals | 3.92 (0.37) | 2.50 (0.42) | 2.67 (0.62) |
| Navigating relationships | 3.42 (0.38) | 2.12 (0.30) | 2.70 (0.29) |
| AA | |||
| Psychosocial difficulties | 3.40 (0.54) | 2.40 (0.53) | 3.13 (0.69) |
| Adjusting to the new normal | 3.29 (0.45) | 3.22 (1.01) | 3.56 (0.66) |
| Positive life changes after treatment | 4.17 (1.04) | 3.63 (1.0) | 2.89 (0.75) |
| Ongoing physical effects of treatment | 3.36 (0.62) | 2.81 (0.83) | 2.56 (0.80) |
| Ongoing emotional effects of treatment | 3.44 (0.61) | 2.79 (0.78) | 2.38 (0.72) |
| B | |||
| Issues related to follow-up care | 3.02 (0.47) | 1.86 (0.40) | 2.07 (0.28) |
| Ongoing physical effects of treatment | 3.27 (0.60) | 2.62 (0.42) | 2.09 (0.36) |
| Navigating cancer care after treatment | 3.25 (0.51) | 2.03 (0.73) | 2.05 (0.75) |
| Cognitive effects of treatment | 3.66 (0.70) | 1.19 (0.57) | 1.64 (0.46) |
| Adjusting to the new normal | 3.94 (0.76) | 2.11 (0.54) | 2.25 (0.65) |
| Navigating relationships | 3.68 (0.72) | 1.73 (0.62) | 2.07 (0.72) |
| Developing a new identity after cancer | 3.98 (0.73) | 2.15 (0.60) | 2.38 (0.51) |
| BB | |||
| Negative psychosocial impact of treatment | 3.93 (1.0) | 1.29 (0.48) | 1.50 (0.71) |
| Transitioning out of the patient role | 4.56 (0.46) | 1.69 (0.61) | 1.81 (0.56) |
| Desire to maintain independence | 4.07 (0.49) | 1.57 (0.68) | 1.79 (0.59) |
| Financial toxicity | 4.60 (0.20) | 1.40 (0.80) | 2.00 (0.55) |
| Frustrations with follow-up care | 4.07 (0.90) | 1.79 (0.70) | 1.79 (0.59) |
| Side effects of treatment | 4.21 (0.95) | 2.00 (0.79) | 1.71 (0.59) |
| Life changes due to diagnosis | 4.08 (0.38) | 1.76 (0.61) | 1.88 (0.52) |
| C | |||
| Physical effects of treatment | 2.08 (0.67) | 1.75 (0.59) | 1.50 (0.35) |
| Feeling unprepared for survivorship | 3.83 (0.27) | 3.03 (0.51) | 2.94 (0.57) |
| Uncertainties about life as a survivor | 3.22 (0.83) | 2.24 (0.78) | 2.35 (0.73) |
| Negative emotional aspects of cancer | 3.33 (0.68) | 2.50 (0.62) | 3.00 (0.72) |
| Challenges with medical providers | 3.31 (0.86) | 2.75 (0.74) | 2.89 (0.90) |
| Psychosocial issues | 3.62 (0.37) | 2.62 (0.50) | 3.10 (0.59) |
| Fears after cancer treatment | 3.92 (0.69) | 3.21 (0.62) | 2.92 (0.49) |
Footnotes
Conflict of Interest: Jennifer Hydeman declares that she has no conflict of interest. Odochi Uwazurike declares that he has no conflict of interest. Elizabeth Adeyemi declares that she has no conflict of interest. Lynda Beaupin declares that she has no conflict of interest.
Compliance with Ethical Standards:
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- 1.Altekruse S, Kosary CL, Rapcho M, et al. SEER Cancer Statistics Review, 1975–2007. National Cancer Institute; Bethesda MD: 2010. http://seer.cancer.gov/csr/1975_2007, based on November 2009 SEER data submission. Accessed 12 Apr 2018. [Google Scholar]
- 2.National Cancer Institute Cancer Control and Population Sciences. Estimated US Cancer Prevalence. 2010. http://cancercontrol.cancer.gov/ocs/prevalence/prevalence.html. Accessed 12 Apr 2018.
- 3.Crom DB, Lensing SY, Rai SN, et al. Marriage, employment, and health insurance in adult survivors of childhood cancer. J Cancer Survivorship 2007;1(3):237–45. [DOI] [PubMed] [Google Scholar]
- 4.Maltaris T, Boehm D, Dittrich R, et al. Reproduction beyond cancer: a message of hope for young women. Gynecol Oncol. 2006;103(3):1109–21. [DOI] [PubMed] [Google Scholar]
- 5.Mertens AC, Liu Q, Neglia JP, et al. Cause-specific late mortality among 5-year survivors of childhood cancer: the Childhood Cancer Survivor Study. J Natl Cancer Inst. 2008;100(19):1368–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oeffinger KC, Mertens AC., Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355(15):1572–82. [DOI] [PubMed] [Google Scholar]
- 7.Soliman H, Agresta SV. Current issues in adolescent and young adult cancer survivorship. Cancer Control 2008;15(1):55–62. [DOI] [PubMed] [Google Scholar]
- 8.Lee JS, Dubois SG, Coccia PF et al. Increased risk of second malignant neoplasms in adolescents and young adults with cancer. Cancer 2016; 122(1):116–123. [DOI] [PubMed] [Google Scholar]
- 9.Gray RE, Doan BD, Shermer P, et al. Psychological adaptation of survivors of childhood cancer. Cancer 1992;70:2713–2721. [DOI] [PubMed] [Google Scholar]
- 10.Teta MJ, Del Po MC, Kasl SV, et al. Psychosocial consequences of childhood and adolescent cancer survival. J Chron Dis. 1986;39:751–759. [DOI] [PubMed] [Google Scholar]
- 11.Chang PH, Nesbit ME, Youngren N, et al. Personality characteristics and psychosocial adjustment of long term survivors of childhood cancer. Psychosoc Oncol. 1987;5:43–58. [Google Scholar]
- 12.Byrne J, Fears RT, Steinhorn SC et al. Marriage and divorce after childhood and adolescent cancer. JAMA 1989;262:2693–2699. [PubMed] [Google Scholar]
- 13.Kroenke CH, Rosner B, Chen WY et al. Functional impact of breast cancer by age at diagnosis. J Clin Oncol. 2004;22(10):1849–56. [DOI] [PubMed] [Google Scholar]
- 14.Mazanec SR, Daly BJ, Douglas SL, et al. The relationship between optimism and quality of life in newly diagnosed cancer patients. Cancer Nurs. 2010;33(3):235–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duffey-Lind EC, O’Holleran E, Healey M, et al. Transitioning to survivorship: a pilot study. J Pediatr Oncol Nurs. 2006;23(6):335–43. [DOI] [PubMed] [Google Scholar]
- 16.Hewitt M, Greenfield S, Stovall E. From cancer patient to cancer survivor: Lost in transition. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 17.Landier W Survivorship care: essential components and models of delivery. Oncol. (Williston Park) 2009;23(4):46–53. [PubMed] [Google Scholar]
- 18.Butow P, Palmer S, Pai A, et al. Review of adherence-related issues in adolescents and young adults with cancer. J Clin Oncol. 2010;28(32):4800–9. [DOI] [PubMed] [Google Scholar]
- 19.Kondryn HJ, Edmondson CL, Hill J, et al. Treatment non-adherence in teenage and young adult patients with cancer. Lancet Oncol. 2011;12(1):100–8. [DOI] [PubMed] [Google Scholar]
- 20.Ruddy K, Mayer E, Partridge A. Patient adherence and persistence with oral anticancer treatment. CA Cancer J Clin. 2009;59(1):56–66. [DOI] [PubMed] [Google Scholar]
- 21.Partridge AH, Archer L, Kornblith AB, et al. Adherence and persistence with oral adjuvant chemotherapy in older women with early-stage breast cancer in CALGB 49907: adherence companion study 60104. J Clin Oncol. 2010;28(14):2418–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Trochim WMK. An introduction to concept mapping for planning and evaluation. Eval Prog Plan. 1989;12:1–16. [Google Scholar]
- 23.Zebrack BJ, Mills J, Weitzman TS. Health and supportive care needs of young adult cancer patients and survivors. J Cancer Surviv. 2007;1(2): 137–45. [DOI] [PubMed] [Google Scholar]
- 24.Nathan PC, Hayes-Lattin B, Sisler JJ, et al. Critical issues in transition and survivorship for adolescents and young adults with cancers. Cancer 2011;117:2335–2341. [DOI] [PubMed] [Google Scholar]
- 25.Zebrack BJ, Hamilton R, Smith AW. Psychosocial outcomes and service use among young adults with cancer. Semin Oncol. 2009;36(5):468–77. [DOI] [PubMed] [Google Scholar]
- 26.Children’s Oncology Group. Long-Term Follow-up Guidelines, Version 4.0. 2013. http://www.survivorshipguidelines.org/pdf/LTFUGuidelines_40.pdf. Accessed 20 Apr 2018.
- 27.Denlinger CS, Sanft T, Baker KS, et al. Survivorship, Version 2.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2017;15:1140–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zebrack BJ, Chesler M. Health-related worries, self-image, and life outlooks of long-term cancer survivors of childhood cancer. Health Soc Work 2001;26(4):245–256. [DOI] [PubMed] [Google Scholar]
- 29.Barnett M, McDonnell G, DeRosa A, et al. Psychosocial outcomes and interventions among cancer survivors diagnosed during adolescence and young adulthood (AYA): a systematic review. J Cancer Surviv. 2016;10(5):814–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shay LA, Capentier MY, Vernon SW. Prevalence and correlates of fear of recurrence among adolescent and young adult versus older adult post-treatment cancer survivors. Support Care Cancer 2016;24(11):4689–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roth ME, O’Mara AM, Seibel NL, et al. Low enrollment of adolescents and young adults onto cancer trials: Insights from the Community Clinical Oncology Program. J Onc Practice 2016;12(4):e388–e395. [DOI] [PMC free article] [PubMed] [Google Scholar]


