Abstract
Malnutrition has been proven to cause poor outcomes in many chronic diseases. We examined the association between malnutrition and immune status in HIV patients. We used the Nutritional Risk Index to evaluate the nutrition in 812 HIV patients, and correlated this variable with viral loads and CD4 counts. We found a significant correlation between nutritional status and immune status.
Introduction
Human Immunodeficiency Virus (HIV) is a serious health issue that affects individuals all around the world. In 2016, 36.7 million people were living with HIV and about 1 million died from an AIDS-related illness. In the U.S. alone, it is estimated that about 1.1 million people were living with HIV at the end of 2015. HIV is an important health condition that continues to be a persistent problem globally.1
HIV gradually weakens a patient’s immune by attacking CD4 T-cells, resulting in the development of opportunistic infections.2 Many factors, including proper nutrition, can help decrease the severity of immunosuppression. Single or multiple nutrient deficiencies impair the cell-mediated response to a greater extent than the humoral response. Nutritional deficiencies, such as protein-energy malnutrition, have been shown to decrease the numbers of helper T-cells, cytotoxic T-cells, and natural killer cells, predisposing individuals to infections.3 Nutritional status, immune expression, and HIV are intricate and intertwined.4 The “vicious cycle” of HIV and malnutrition is attributed to the fact that both conditions are associated with a decreased immunity. Decreased immunity increases the risk for infections, leading to increased nutritional demand. If this nutritional demand is not met, a more severe malnourished state can ensue.5 Malnutrition further contributes to the disease process by propagating the transition from HIV to Acquired Immunodeficiency Syndrome (AIDS).4 In fact, most patients with AIDS develop protein deficiency and experience cachexia, diarrhea, and weight loss.6 According to the World Health Organization, energy requirements increase by 10% in asymptomatic HIV positive adults and by 20–30% in symptomatic HIV positive adults, demonstrating the importance of proper diet in HIV/ AIDS.7
Cooney (2015) explained that impaired CD4+ counts, beginning early after acute HIV infection, is the hallmark of HIV infection.8 HIV patients have decreased B, CD8+, and CD4+ lymphocyte counts.8 Additionally, it has been found that HIV patients with opportunistic infections have low CD4+ levels,9 demonstrating the importance of analyzing nutrition and immune status to prevent the development of opportunistic infections and to improve patients’ outcome. Viral load has been found to be a better predictor of declining immune status when compared to CD4+ counts,9 and an increase in viral load is associated with HIV infection. For this reason, we will be using CD4+ and viral load counts as an indicator of immune status when analyzing the relationship between immune and nutritional status. The goals of this study are to determine demographics, immune status, and the percentage at risk of malnutrition of HIV patients at Truman Medical Center.
Methods
Study Subjects
Eight hundred and fifty-five outpatients at Truman Medical Centers diagnosed with HIV were included in this study. Forty-three patients were excluded because the Devine formula for ideal body weight, a variable required to determine the Nutritional Risk Index (NRI), requires that a patient’s height be over 60 inches, the albumin level was unavailable, or they identified as the race Native American, Pacific Islander, Asian, other, or unknown. Because there were only a small number of patients in each of those racial groups, they were excluded to protect their privacy. Our final sample size of 812 outpatients diagnosed with HIV (580 men and 219 women, ages 18–86) were further analyzed.
Nutritional Status
We used the Nutritional Risk Index (NRI) to determine nutritional status of 812 HIV outpatients, which was calculated from the following well-established formula:10
where sALB is the serum albumin in g/L, actual weight is in kg, and IBW is the ideal body weight in kg. The IBW was determined using the Devine formula11 for each sex:
where IBW is ideal body weight in kg and height is in inches. For the transsexual patients, we used the male IBW equation.
After calculating the IBW and NRI for each patient, they were categorized into two groups: not at risk of malnutrition (NRI > 100) and at risk of malnutrition (NRI < 100). The at-risk category was subdivided into borderline risk (NRI 97.5–100), mild risk (NRI 83.4 – 97.5), and severe risk (NRI < 83.5) of malnutrition.
We stratified the data regarding at risk and no risk for malnutrition by age, sex, and race. With regards to age, we separated the patients into the following categories: less than 40, 40–49, 50–59, and greater than 60 years old. With regards to sex, we categorized patients into male, female, and transsexual. With regards to race, we classified patients as white, black, and Hispanic.
Immune Status
We used CD4+ count and viral loads determined by PCR to assess the immune status of 812 HIV outpatients. In order to combine the CD4+ counts and viral load into one numerical value representing immune status, we ranked patients on a scale from 1 to 4 for their viral load and CD4+ count, as shown in Table 1.
Table 1.
Immune Status and Viral Load
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| Viral Load (copies/mL) | >100,000 | 50,000–100,000 | Detectable < 50,000 | Undetectable |
| CD4+ count per mL | <100 | 100–199 | 200–500 | >500 |
The rank of the viral load category and the rank of the CD4+ count category were summed to get an overall rating of immune status. The worst possible overall rating of immune status is 2 while the best possible rating is 8. The overall immune ratings 2, 3, and 4 represent a poor immune status, ratings 5 and 6 represent a moderate immune status, and ratings 7 and 8 represent a good immune status.
Statistical Analysis
For our statistical analysis, we used Statistical Packaging for the Social Sciences (SPSS) Version Stats 24. To assess the correlation between age and NRI, we performed a Pearson correlation. A 3 x 3 two-way ANOVA test was used to determine the association between race (black, white, Hispanic), sex (male, female, transsexual), and NRI. A partial Eta squared was calculated to demonstrate the strength of the relationship between NRI and our independent variables, race and sex. We performed a post-HOC test to closely analyze the groups within race and sex to determine whether these groups were statistically significant. A p-value < 0.05 was considered to be statistically significant.
To assess the correlation between NRI and immune rating, we used the Spearman correlation test. To assess the correlation between NRI and the two contributors of immune status (CD4+ and viral load) separately, we used the Pearson correlation test. Regression analysis was used to determine the extent of contribution of CD4 or viral load individually to immune status. These tests were performed for all 812 HIV outpatients as well as just the 93 malnourished HIV outpatients. For all statistical tests, a p-value of < 0.05 was considered statistically significant.
Results
Nutritional Status in HIV/AIDS and Trends in Age, Sex, and Race
Of the 812 HIV outpatients, 93 (11.45%) are at some degree of risk for malnutrition. 23 (2.83%) patients were at mild nutritional risk, 55 patients (6.77%) were at moderate nutritional risk, and 15 patients (1.85%) were at severe nutritional risk. Average NRI of all 812 patients is 114.81.
As age increased, NRI decreased (r = −0.107, p = 0.002). While both sex and race are independently statistically significant (p = 0.005, p = 0.05), there is no interaction between the two variables (p = 0.246, partial Eta squared = 0.007). Regarding sex, the NRI of females is greater than that of males (117.69 vs 113.71, p = 0.001). Regarding race, Hispanic HIV patients have greater NRI than white patients (119.72 vs 112.93, p = 0.001) and Hispanic patients have greater NRI than black patients (119.72 vs 114.95, p = 0.017). The difference in white and black patient NRIs was not statistically significant (p = 0.090).
Immune Status
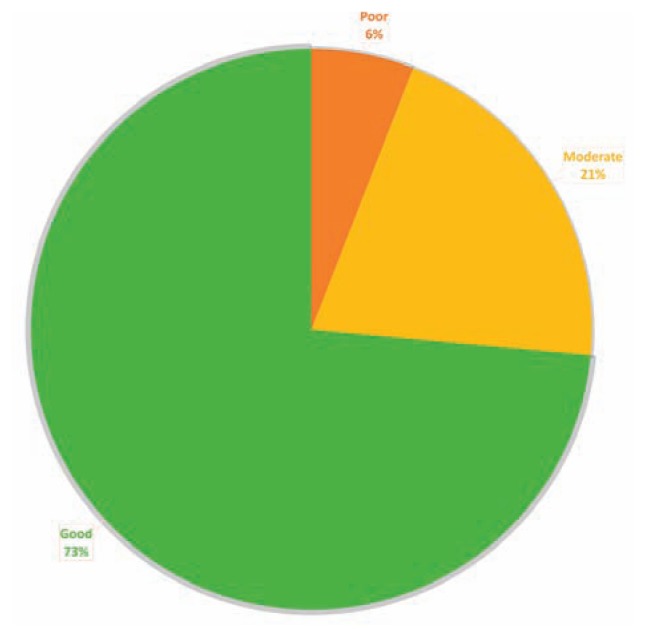
Of the 812 HIV outpatients, 48 (5.91%) are of poor immune status, 167 (20.57%) are at moderate immune status, and 597 (73.52%) are of good immune status (Figure 1). The average overall immune rating is 6.99, average CD4+ count is 298.6 cells/uL, and average viral load is 13,019.47.
Figure 1.
Immune Status in HIV Outpatients
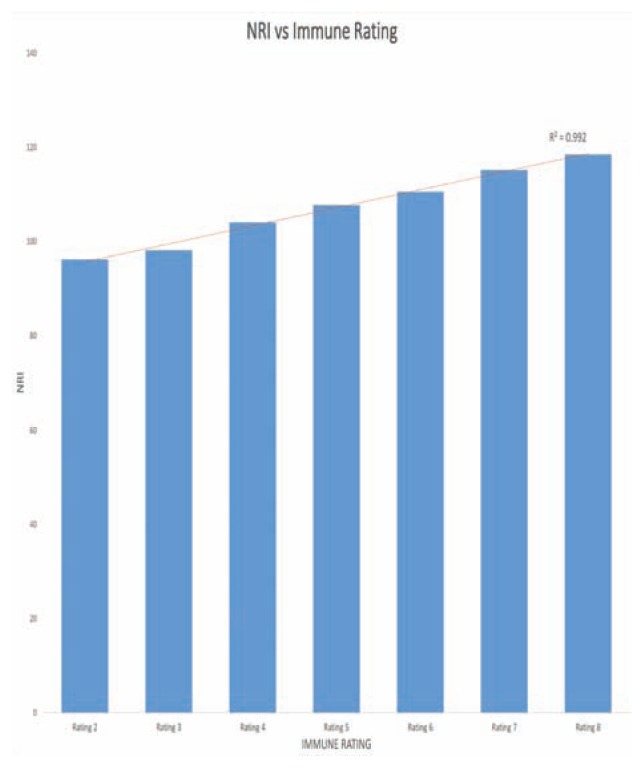
Immune status and Nutritional Risk Index
Of all 812 HIV patients, there is a significant correlation between NRI and immune rating (r = 0.302, p <0.001) (Figure 2), NRI and CD4+ (r = 0.304, p < 0.001), and NRI and viral load (r = −0.121, p < 0.001). Regression analysis shows that CD4+ and viral load are significant determinants of NRI (CD4: r = 0.304, p < 0 0.001; viral load: r = −0.121, p < 0.001). Of the 93 patients at risk of malnutrition, 22 (23.91%) patients have poor immune status, 32 (34.78%) patients have moderate immune status, and 38 (41.30%) patients have good immune status. Of the 48 patients with poor immune status, 22 (45.83%) patients are at risk of malnutrition and broken down into individual categories, 7 (14.58%) are at mild risk of malnutrition, 10 (20.83%) patients are at moderate risk of malnutrition, and 5 (10.42%) patients are at severe risk of malnutrition. 26 (54.17%) patients are not at risk of malnutrition.
Figure 2.
Immune status and Nutritional Risk Index
Conclusion
Eleven point three percent of 812 HIV outpatients are at risk of malnutrition. Findings in this group include: a) with age, NRI decreased, b) NRI of female HIV patients is greater than that of males, c) black patients have greater NRI than white patients, and d) Hispanic patients have greater NRI than black patients. Of the 812 HIV outpatients, there is a significant correlation between NRI and immune rating. The two factors that contribute to immune rating, CD4+ and viral load, also show significant correlation with NRI. CD4+, and viral load are all significant determinants of NRI in HIV outpatients.
Of the 93 patients at risk of malnutrition, 23.91% (n = 23) have poor immune status. When analyzing this subgroup, there was no significant correlation between NRI and immune rating, CD4+, and viral load.
Of the 48 patients with poor immune status, 45.83% (n = 22) are at risk of malnutrition.
There is no difference in NRI between transsexual and female patients, and transsexual and male patients. The difference in female and transsexual NRIs was not statistically significant (p = 0.063) and the difference in male and transsexual NRIs was not statistically significant (p = 0.319).
Discussion/Future Directions
Our study shows that a significant percentage of HIV/ AIDS outpatients may be at risk of malnutrition, which shows that meeting proper diet requirements is vital in this population. A study on nutritional supplementation for patients with HIV showed that oral nutritional supplements along with dietary counseling led to decreased protein catabolism and increased lean body mass.12 Nutritional supplements also increase CD4 counts, directly reflecting an improvement in immune response.13 Nutritional assessment and intensive dietary counseling at the time of diagnosis of HIV could prove beneficial in this population to minimize progression to the development of AIDS. Further nutritional supplement may be useful to improve the prognosis of HIV/AIDS.
The relationship between nutrition and HIV has been described in other studies as well. A study comparing HIV+ and HIV- adults found that HIV is associated with higher serum protein and lower serum albumin levels, and that HIV+ women have higher BMI and waist circumference, suggesting that nutrition is an important factor in this disease. Hillesheim et al. showed that in HIV+ children and adolescents, dietary energy intake correlates with CD4+ count and viral load. There is a significant relationship between a lower energy diet, and viral suppression and immune preservation.14 The World Health Organization explains that improved diet may contribute to the success of antiretroviral treatment (ARTs). Some specific ARTs interfere with the metabolism of glucose and lipids, bone metabolism, and lactic acidemia, so patients on ARTs should pay special attention to maintaining a healthy, balanced diet.7
While nutrition is a factor affecting immune status in HIV patients, our future work will focus on additional factors such as antiretroviral therapies, other underlying conditions, and other medications contributing to immune status. We also hope to increase the sample size of our transsexual population with HIV for further research as there is limited work done in this population.
Acknowledgments
We gratefully acknowledge Jennifer Quaintance, PhD for her guidance in statistical analysis.
Footnotes
Rashmi Thimmapuram, Sree Lanka, and Anthony Esswein, are at the University of Missouri - Kansas City School of Medicine, Kansas City, Mo. Lawrence Dall, MD, is Professor and Assistant Dean of Medical Student Research at the University of Missouri-Kansas City School of Medicine, Department of Internal Medicine, Infectious Disease at Truman Medical Center, Kansas City, Mo.
Contact: dalll@umkc.edu
Disclosure: None reported.
References
- 1.Basic Statistics | HIV Basics | HIV/AIDS | CDC. [Accessed November 28, 2018]. https://www.cdc.gov/hiv/basics/statistics.html. Published November 21, 2018.
- 2.About HIV/AIDS | HIV Basics | HIV/AIDS | CDC. [Accessed November 28, 2018]. https://www.cdc.gov/hiv/basics/whatishiv.html. Published October 31, 2018.
- 3.Scrimshaw NS, SanGiovanni JP. Synergism of nutrition, infection, and immunity: an overview. Am J Clin Nutr. 1997;66(2):464S–477S. doi: 10.1093/ajcn/66.2.464S. [DOI] [PubMed] [Google Scholar]
- 4.Duggal S, Chugh TD, Duggal AK. HIV and Malnutrition: Effects on Immune System. Clin Dev Immunol. 2012;2012:1–8. doi: 10.1155/2012/784740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colecraft E. HIV/AIDS: nutritional implications and impact on human development | Proceedings of the Nutrition Society | Cambridge Core. [Accessed November 28, 2018]. https://www.cambridge.org/core/journals/proceedings-of-the-nutrition-society/article/hivaids-nutritional-implications-and-impact-on-human-development/D21825E91975A8D34F61DBDC4AB6182B. [DOI] [PubMed]
- 6.Evans SK. Nutrition and AIDS. Beltsville, Md: 1991. http://hdl.handle.net/2027/umn.31951003042349d. [Google Scholar]
- 7.Nutrient Requirements for People Living with HIV/AIDS Report of a Technical Consultation. World Health Organization; Geneva: Geneva: World Health Organization; May 13–15, 2003. [Accessed November 27, 2018]. WHO Technical Consultation on Nutrient Requirements for People Living with HIV/AIDS. 2003. http://whqlibdoc.who.int/publications/2003/9241591196.pdf. [Google Scholar]
- 8.Mayer KH, Cooney EL. Clinical Indicators of Immune Restoration following Highly Active Antiretroviral Therapy. Clin Infect Dis. 2002;34(2):224–233. doi: 10.1086/323898. [DOI] [PubMed] [Google Scholar]
- 9.Verma R. Decline in CD4 counts in HIV patients. Med J Armed Forces India. 2014;70(3):301. doi: 10.1016/j.mjafi.2014.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aziz EF, Javed F, Pratap B, et al. Malnutrition as assessed by nutritional risk index is associated with worse outcome in patients admitted with acute decompensated heart failure: an ACAP-HF data analysis. Heart Int. 2011;6(1) doi: 10.4081/hi.2011.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devine B, Devine BJ. Gentamicin therapy. [Accessed November 28, 2018];Drug Intell Clin Pharm. 1974 8:650–655. [Google Scholar]
- 12.Berneis K, Battegay M, Bassetti S, et al. Nutritional supplements combined with dietary counselling diminish whole body protein catabolism in HIV-infected patients. Eur J Clin Invest. 2000;30(1):87–94. doi: 10.1046/j.1365-2362.2000.00591.x. [DOI] [PubMed] [Google Scholar]
- 13.Evans D, McNamara L, Maskew M, et al. Impact of nutritional supplementation on immune response, body mass index and bioelectrical impedance in HIV-positive patients starting antiretroviral therapy. Nutr J. 2013;12:111. doi: 10.1186/1475-2891-12-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hillesheim E, Lima LRA, Silva RCR, Trindade EBSM. Dietary intake and nutritional status of HIV-1-infected children and adolescents in Florianopolis, Brazil. Int J STD AIDS. 2014;25(6):439–447. doi: 10.1177/0956462413512808. [DOI] [PubMed] [Google Scholar]