Abstract
Gay and bisexual men (GBM) with heightened fears of human immunodeficiency virus (HIV) acquisition have reported high levels of sexual anxiety and low sexual self-esteem. Similarly, sexual satisfaction has been reported to be lower among some GBM who rely solely on condom use as HIV prevention. We sought to explore if pre-exposure prophylaxis (PrEP) had an impact on the sexual satisfaction, anxiety, and esteem of GBM. As part of a longitudinal cohort study of 1,071 GBM, participants reported at three time points on PrEP use and completed the Multidimensional Sexual Self-Concept Questionnaire. A total of 137 GBM began taking PrEP in the 24 months following baseline. Comparing their responses during times before initiating PrEP and after within adjusted multilevel models, there was a significant decrease in sexual anxiety (B = −0.27, p = 0.03) but no significant changes in sexual esteem or satisfaction. Our findings indicate important psychological improvements resulting from PrEP initiation. Further research should explore the potential for other psychological benefits to PrEP use among GBM
Keywords: sexual satisfaction, sexual anxiety, sexual self-esteem, gay and bisexual men, PrEP
An estimated 1.1 million people are living with human immunodeficiency virus (HIV) in the United States, and gay and bisexual men (GBM) currently account for approximately 67% of all new HIV diagnoses (Center for Disease Control and Prevention [CDC], 2017a, 2017b). Pre-exposure prophylaxis (PrEP) is an FDA-approved once-daily pill shown to be highly effective in the prevention of HIV transmission among GBM (Grant et al., 2010; Mugo et al., 2015; Volk et al., 2015). Since the release of PrEP, the majority of research among GBM has focused on acceptability (Brooks et al., 2011; Golub, Gamarel, Rendina, Surace, & Lelutiu-Weinberger, 2013; Grov, Whitfield, Rendina, Ventuneac, & Parsons, 2015), uptake (Parsons et al., 2017; Rendina, Whitfield, Grov, Starks, & Parsons, 2017), and adherence (Amico & Stirratt, 2014; Closson, Mitty, Malone, Mayer, & Mimiaga, 2017; Mayer et al., 2017; Simoni, Amico, Pearson, & Malow, 2008). One area that has received less attention is the psychological impact that PrEP has on its users (Collins, McMahan, & Stekler, 2017; Hojilla et al., 2016; Koester et al., 2017). Given its efficacy at reducing HIV transmission even in the absence of condoms, PrEP may confer psychological benefits to its users, such as lower sexual anxiety and enhanced sexual satisfaction and sexual esteem.
The fear of HIV acquisition among GBM has been well researched and is often linked to negative affect (e.g., anxiety). Some GBM may have anxiety for months after engagement in condomless anal sex (CAS) (Godin, Naccache, & Pelletier, 2000), and possibly avoid HIV testing altogether for fear of receiving an HIV-positive result (Kellerman et al., 2002; Lorenc et al., 2011). However, with the effectiveness of PrEP in preventing HIV infection, it is possible that such fears may decrease among PrEP users (Koester et al., 2017). To date, few published studies have examined affective changes in PrEP users (Collins et al., 2017; Hojilla et al., 2016; Koester et al., 2017; Storholm, Volk, Marcus, Silverberg, & Satre, 2017) and all observed a decrease in sexual anxiety. Among GBM on PrEP participating in an open-label extension (OLE) trial, counselor notes revealed the common theme that PrEP alleviated anxiety regarding sexual behavior and HIV infection (Hojilla et al., 2016). Similarly, interviews with GBM in another PrEP OLE trial found reduced fears of HIV acquisition and a reduction in HIV-related stress while on PrEP (Collins et al., 2017; Koester et al., 2017). Participants across studies referred to PrEP as providing an “extra layer of protection,” “safety net,” and “peace of mind,” all representing more protection and an implicit reduction in fear and anxiety about HIV acquisition. In all studies, a reduction in anxiety was reported qualitative; there do not appear to be any studies in which these changes have been quantified.
When navigating their sex lives, GBM may struggle between maintaining sexual health and experiencing a high degree of sexual satisfaction (Shernoff, 2006). GBM have reported that sex with condoms is not always as sexually satisfying (Harper, Tyler, Bruce, Graham, & Wade, 2016), and that condoms can be both inconvenient and embarrassing (Mustanski, DuBois, Prescott, & Ybarra, 2014). Condom use has also been reported as being a barrier to trust, intimacy, and spontaneity, in which case a trade-off is made where HIV infection is considered an acceptable risk for an increase in emotional satisfaction (Bauermeister, Carballo-Diéguez, Ventuneac, & Dolezal, 2009; Elam et al., 2008; Starks, Payton, Golub, Weinberger, & Parsons, 2014; Tsai, 2014). PrEP is highly effective in the prevention of HIV transmission, and thus some users may decrease condom use which could result in an increase in sexual satisfaction.
PrEP users are actively engaging in HIV risk prevention and thereby taking control of their sexual health, which may increase sexual esteem or the positive feelings they have about their sexual activity and ability to deal effectively with the sexual aspects of oneself (Maas & Lefkowitz, 2015). The CDC guidelines for PrEP use explicitly lays out that going on PrEP is not a one-time event, but rather a system of health care for users. Once a PrEP regimen has been initiated users are required to attend quarterly doctor’s appointments to receive HIV testing, behavioral risk assessments, adherence counseling, and an STI symptoms assessment. Additionally, users are required to receive STI testing at their bi-annual appointments (CDC, 2014). For some PrEP users, these required appointments may lead to more feelings of being in control of their sexual health and raise their sexual esteem. Changes in sexual esteem due to PrEP use have not yet been explored; however, themes have emerged in some research. A participant from one OLE reported to “feel like I’m taking care of myself” while participants in another study reported more “comfort and confidence” as they felt they were taking care of their sexual health (Storholm et al., 2017). Others stated it provided a “heightened sense of safety” (Hojilla et al., 2016) and “replaced feelings of worry” (Koester et al., 2017). To what degree these feelings of safety are internalized and associated with the belief of having the ability to protect oneself is unknown.
To date, only qualitative research has examined the impact of PrEP on psychological factors relevant to sexual health. These findings suggest there may be quantitatively measurable changes in sexual anxiety, sexual esteem, and sexual satisfaction due to PrEP uptake. In the present study, we sought to build upon these findings by measuring quantitative changes in sexual anxiety, sexual satisfaction, and sexual esteem by conducting pre-post analyses of these three variables (i.e., from the assessment immediately before participants began PrEP to the assessment immediately following their initiation of PrEP). Based on previous research, we hypothesized participants would experience a decrease in sexual anxiety and an increase in both sexual satisfaction and sexual esteem after going on PrEP.
Method
Participants and Procedures
One Thousand Strong is a longitudinal study following a U.S. national cohort of 1,071 GBM (Grov et al., 2016). The goal of recruitment for One Thousand Strong was to identify and recruit a national sample of GBM who represent the diversity and distribution of GBM across the country consistent with U.S. Census data. Potential participants were identified through Community Marketing & Insights (CMI), who have a database of over 22,000 GBM living throughout the U.S. The CMI panel is comprised of individuals drawn from over 200 sources (e.g., lesbian, gay, bisexual, and transgender events, e-mail broadcasts distributed by LGBT organizations, main stream, and social media).
Initially, 9,011 individuals were invited to complete the screening survey via e-mail. Those sent the screening survey were identified as potentially eligible having met the criteria of 18 years or older, identified as a gay or bisexual male, and had regular internet access. Participants deemed preliminarily eligible had their responses and contact information shared with the research team and were then independently contacted by the research team to be screened for full enrollment. Participants had met the following requirements to be fully enrolled in the final cohort: 1) reside in the U.S.; 2) be at least 18 years of age; 3) be biologically male; 4) identify as male; 5) report having sex with a man in the past year (e.g., oral, anal, mutual masturbation); and 6) self-identify as HIV-negative. If all criteria were met, participants were sent a link to complete an online survey and an at-home HIV and sexually transmitted infection (STI) testing kit along with a pre-paid box for submitting the specimen to a lab for testing. Participants were not fully enrolled until all steps were met and HIV-negative status confirmed.
Of the 9,011 men who were emailed an invitation to complete the screening survey, 6,371 (70.7%) did not open the email, and another 90 emails were unable to be delivered. Of the 2,550 (28.3%) who opened the email, 2,393 (93.8%) completed the screening survey, an overall response rate of 26.6%. Of these, 1,375 (57.5%) were deemed eligible, with the most common reasons for ineligibility being an HIV-positive status or not being sexually active with a man. Of the 1,375 eligible men, 1,071 (77.9%) completed all requirements of the assessment and were enrolled into the One Thousand Strong cohort. The final sample is representative of HIV-negative GBM in the U.S., which resulted in fewer men of color because of the heightened prevalence of HIV among men of color. Participants were reassessed annually (including an online survey and STI/HIV testing, and being compensated in Amazon gift cards totaling $50) and asked to complete an additional optional survey at 6 month intervals between annual assessments (online survey only and receiving compensation of a $25 Amazon gift card). All online survey data were collected via Qualtrics survey software (qualtrics.com), which offered the survey via the internet and mobile device optimization. Further details on testing and additional information on requirement can be found in Grov et al. (2016).
Data for the following analyses were collected at baseline, 12 month follow-up, and 24 month follow-up, dependent on when the participant began PrEP use, as described in more detail below. The City University of New York Institutional Review Board approved study procedures.
Measures
Demographic and background characteristics.
Participants reported demographic characteristics including race/ethnicity, education, income, age, relationship status, sexual orientation, and U.S. zip code during the baseline survey.
PrEP use (Parsons, Rendina, Whitfield, & Grov, 2016).
Participants were provided with a short definition about PrEP and then asked about current and past PrEP use. Across all time points, participants were asked: “Have you ever been prescribed HIV medications (e.g., Truvada) for use as PrEP (HIV pre-exposure prophylaxis)?” Response options included, “Yes, I am currently prescribed PrEP,” “Yes, but I am no longer prescribed PrEP, “and “No, I’ve never been prescribed PrEP.”
Multidimensional Sexual Self-Concept Questionnaire (MSSCQ) (Snell, 1998).
The full MSSCQ is comprised of 100 items covering 20 psychological aspects of human sexuality. For this study participants completed three subscales measuring their sexual satisfaction, sexual esteem, and sexual anxiety using a Likert-type scale consisting of 15 items ranging from 0 (not at all characteristic of me) to 4 (very characteristic of me). A total of five items measured sexual satisfaction (e.g., “I am satisfied with the status of my own sexual fulfillment”); this scale is a sum of the items, with higher scores indicating more sexual satisfaction (α = 0.94). Five items measured sexual esteem (e.g., “I am pleased with how I handle my own sexual tendencies and behaviors”); this scale is a sum of the items, with higher scores indicating more sexual esteem (α = 0.92). Five items measured sexual anxiety (e.g., “thinking about the sexual aspects of my life leaves me with an uneasy feeling”); this scale is a sum of the items, with higher scores indicating more sexual anxiety (α = 0.91).
Analytic Plan
This study focused on all participants who reported that they were not on PrEP at the baseline assessment and subsequently reported initiating PrEP at a later assessment within the 24 months following baseline. The baseline assessment was completed by 1,071 GBM. Of those, as noted in Figure 1,137 reported that they were on PrEP at either the 12-month or 24-month assessment, or both. As such, we had at least one time point prior to PrEP uptake and at least one time point while currently on PrEP for each of these 137 participants. We analyzed data from a total of 393 time points, or an average of 2.9 time points per person, with variability between individuals in terms of the number of visits that were prior to PrEP uptake or while on PrEP.
Figure 1.
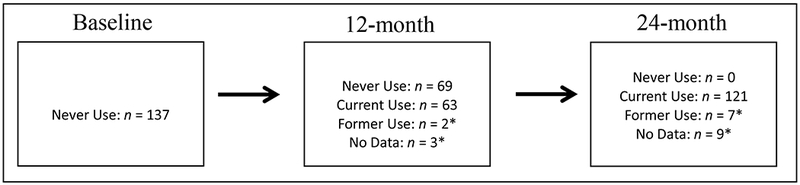
This figure shows the breakdown of PrEP use status at each assessment time point among the analytic sample, which is comprised of the 137 participants who were PrEP-naïve at baseline and initiated PrEP at some point prior to the 24-month assessment. As can be seen, there were a small number of PrEP discontinuations and assessments not completed, resulting in a total of 393 time points for analyses. The figure also illustrates that some individuals had two pre-PrEP assessments and one assessment on PrEP, while others had one pre-PrEP assessment and two assessments on PrEP, for a total of 206 pre-PrEP time points and 184 time points while on PrEP available for within-person analyses.
To make full use of the multiple time points per person, we conducted a series of multilevel models within SPSS version 25. Specifically, we ran a series of linear mixed models with visits at Level 1 nested within individuals at Level 2 and specified a random slope be estimated, with one model for each of the three outcomes of interest—sexual anxiety, esteem, and satisfaction. The primary variable of interest was a visit-level (i.e., level 1) predictor corresponding to whether, at that time point, the participant was currently (coded as 1) or not yet (coded as 0) taking PrEP. In other words, we analyzed multiple time points for each individual and statistically compared, both within and across individuals, how each outcome differed during times when the participant had never yet been on PrEP versus was actively on PrEP. To adjust for their potential confounding effects, we added the following time-varying (i.e., level 1) covariates: assessment time point (baseline, 12-month, 24-month), number of condomless anal sex (CAS) acts with casual male partners in the prior 6 months, and whether the participant was in a relationship. Additionally, at the individual level, we adjusted for whether the participant was a person of color, whether he had a college degree, and his age at the time of enrollment.
Results
Demographic characteristics of the analytic sample (n =137) at baseline are presented in Table 1. Ages ranged from 18-65 (M = 35.98, SD = 11.20). The majority of our sample was White (n = 96, 70.1%), had a 4-year college degree or higher (n = 88, 64.2%), had an income of between $20-49K per year (n = 45, 32.8%), and was employed full-time (n = 96, 70.1%). Slightly more men reported being single (n = 74, 54.0%) than in a relationship (n = 63, 46.0%). Overall, 53.2% (n = 209) of the visits analyzed were prior to PrEP uptake and 46.8% (n = 184) were while currently taking PrEP.
Table 1.
Demographic Characteristics (N=137)
| n | % | |
|---|---|---|
| Age (M = 35.98) | ||
| 18-24 | 22 | 16.1 |
| 25-34 | 53 | 38.7 |
| 35-44 | 31 | 22.6 |
| 45+ | 31 | 22.6 |
| Race/Ethnicity | ||
| Black | 15 | 10.9 |
| Latino | 15 | 10.9 |
| White | 96 | 70.1 |
| Other/Multiracial | 11 | 8.0 |
| Education | ||
| High school degree or less | 4 | 2.9 |
| Some college or Associate’s degree | 45 | 32.8 |
| 4-year college degree or more | 88 | 64.2 |
| Income | ||
| Less than $20k per year | 24 | 17.5 |
| $20k to 49k per year | 45 | 32.8 |
| $50k to $74k per year | 30 | 21.9 |
| $75k or more per year | 38 | 27.7 |
| Employment | ||
| Unemployed | 15 | 10.9 |
| Part-time | 26 | 19.0 |
| Full-time | 96 | 70.1 |
| Geographic Region | ||
| Northeast | 33 | 24.1 |
| Midwest | 18 | 13.1 |
| South | 55 | 40.1 |
| West | 31 | 22.6 |
| Relationship status | ||
| Single | 74 | 54.0 |
| Partnered | 63 | 46.0 |
Results of the three multilevel models can be found within Table 2. In the first model predicting sexual anxiety, none of the potential confounders adjusted for showed meaningful impact on the outcome—assessment time point, partnered status, possessing a college degree, and number of CAS acts were all non-significant. In contrast, our primary variable of interest—PrEP status—was significant and showed that participants reported significantly lower sexual anxiety at times during which they were on PrEP compared to time points prior to PrEP use. Specifically, the coefficient of −0.27 shows that the average participant reported a decrease in sexual anxiety of 0.27 points during times when they were on PrEP compared to times prior to starting PrEP. Additionally, at the individual level, we observed that participants of older age at baseline reported on average significantly lower sexual anxiety during a typical assessment time point. We did not find an effect of the other two individual-level variables, race or sexual identity.
Table 2.
Results of multilevel models investigating the role of PrEP status on sexual anxiety, esteem, and satisfaction.
| Model 1: Sexual Anxiety |
Model 2: Sexual Esteem |
Model 3: Sexual Satisfaction |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| B | S.E. | p | B | S.E. | p | B | S.E. | p | |
| Level 1 Effects | |||||||||
| Intercept | 1.46 | 0.27 | < 0.001 | 2.07 | 0.30 | < 0.001 | 2.10 | 0.31 | < 0.001 |
| Assessment Time Point (ref: baseline) | |||||||||
| 12-month | 0.05 | 0.09 | 0.62 | 0.03 | 0.10 | 0.74 | 0.09 | 0.11 | 0.40 |
| 24-month | 0.11 | 0.14 | 0.43 | 0.14 | 0.15 | 0.36 | 0.20 | 0.16 | 0.21 |
| Partnered (ref: single) | −0.03 | 0.10 | 0.78 | 0.17 | 0.11 | 0.11 | 0.36 | 0.28 | 0.001 |
| College degree (ref: no) | 0.06 | 0.13 | 0.67 | −0.04 | 0.14 | 0.79 | −0.09 | 0.15 | 0.54 |
| CAS acts with casual male partners | 0.00 | 0.01 | 0.79 | 0.01 | 0.01 | 0.13 | 0.02 | 0.01 | 0.005 |
| On PrEP (ref: Not on PrEP) | −0.27 | 0.12 | 0.025 | 0.06 | 0.13 | 0.64 | −0.01 | 0.14 | 0.96 |
| Level 2 Effects | |||||||||
| Age at enrollment | −0.01 | 0.01 | 0.04 | 0.00 | 0.01 | 0.58 | 0.00 | 0.01 | 0.57 |
| White race (ref: men of color) | 0.04 | 0.16 | 0.80 | −0.04 | 0.17 | 0.82 | −0.08 | 0.18 | 0.67 |
| Bisexual identity (ref: gay) | −0.24 | 0.24 | 0.32 | −0.41 | 0.27 | 0.13 | −0.10 | 0.28 | 0.72 |
| Random Effects | |||||||||
| Intercept variance | 0.55 | 0.08 | < 0.001 | 0.64 | 0.10 | < 0.001 | 0.72 | 0.11 | < 0.001 |
In the second model, we found no significant predictors of sexual esteem levels. In the third model, participants reported higher levels of sexual satisfaction at time points during which they were in a relationship and reported more CAS acts with casual partners; PrEP use was not a significant predictor, nor were any of the other variables included in the model.
Discussion
We examined changes in sexual anxiety, sexual esteem, and sexual satisfaction for PrEP-using GBM from before starting PrEP to while on PrEP. We found support for our hypothesis that individuals taking PrEP would experience a reduction in sexual anxiety after starting on PrEP compared to before taking PrEP. We did not find support for our hypotheses predicting an increase in both sexual satisfaction and sexual esteem while on PrEP compared to before taking PrEP. This is the first study to quantify psychological changes due to PrEP use among GBM at-risk for HIV acquisition.
All three previous qualitative studies addressing anxiety after starting on PrEP reported that users experienced less anxiety and fear pertaining to HIV acquisition while taking PrEP (Collins et al., 2017; Hojilla et al., 2016; Koester et al., 2017). Our findings support this claim quantitatively. There was a main effect for PrEP use and level of sexual anxiety while adjusting for demographic differences, the effect of time, and the number of recent CAS acts. This suggests that an additional benefit of PrEP use among GBM includes a decrease in sexual anxiety around potential HIV acquisition.
All GBM who go on PrEP do not necessarily begin taking PrEP for the same reasons, and there may be additional variables that could be examined in understanding the decrease in anxiety. For example, we included the number of CAS partners; however, we did not measure participants’ perception of their sexual risk prior and post beginning a PrEP regimen. As such, results may vary for GBM who engage in different types and frequencies of risk behavior or their perceptions of risk with each behavior. Similarly, one study noted that individuals in serodiscordant relationships reported lower anxiety in both their level of anxiety and their HIV-positive partner’s level of anxiety after beginning PrEP (Hojilla et al., 2016). Researchers from this study theorized that the role of PrEP in serodiscordant relationships may have additional effects by simultaneously lowering anxiety and allowing for an increase in intimacy. Taken together, this suggest that the psychological benefits of HIV at-risk individuals beginning a PrEP regimen may even have the potential to reach past the person taking the medication and enhance relationships where HIV transmission is a concern.
Previous research theorized changes in sexual satisfaction would be due to either a decrease in fear and anxiety around potential HIV acquisition or engagement in sexual behaviors that were before limited (e.g., serosorting, receptive anal intercourse) (Collins et al., 2017; Hojilla et al., 2016; Koester et al., 2017). We found that both being in a relationship and engaging in more CAS were associated with more sexual satisfaction; however, PrEP was not predictive of this increase. The sexual satisfaction subscale used to measure this construct examines if an individual’s current sexual needs are being met and if they are sexually fulfilled and personally gratified with their sex life. For those in a relationship, they may see more positive aspects to their sex lives compared to those who are single, thus leading to higher sexual satisfaction. Taken together with the decrease in sexual anxiety, it’s possible that sexual satisfaction for these participants is not linked to simply a fear of HIV acquisition, but a deeper sense of contentment not predicted by PrEP use. Future research addressing sexual satisfaction and PrEP use would benefit from the use of a scale that measures a construct more associated with physical sexual pleasure as an increase of CAS was associated with an increase in sexual satisfaction.
Lastly, we also did not observe an increase in sexual esteem while on PrEP compared to before beginning PrEP. We expected to see an increase due to the consistent engagement in health care required to continue a PrEP regimen put forth in the CDC guidelines (CDC, 2014). However, the sexual esteem subscale we used focused on how an individual handles their sexual needs and desires being met and likely did not capture the sense of pride someone may feel in taking control of their sexual health.
We found evidence that PrEP users may also experience some psychological benefits in addition to biological protection against HIV acquisition. Individuals who are beginning PrEP use are likely already experiencing psychological discomfort regarding their sexual behavior or they wouldn’t consider PrEP use. Beginning a regimen provides users respite from their fears around potential seroconversion. It is worth noting there is research on sexual behavior changes pre- and current PrEP use showing there are increases in CAS while on PrEP (Lal et al., 2017; Newcomb, Moran, Feinstein, Forscher, & Mustanski, 2017; Oldenburg et al., 2017), which may lead to an increase in sexual satisfaction for some, but also increases in STIs. However, sexual satisfaction has been linked to other forms of behavioral change associated with decreasing HIV risk (e.g., serosorting, strategic positioning) (Grov, Rendina, Moody, Ventuneac, & Parsons, 2015; Parsons et al., 2005). Interventions aiming to increase PrEP use, as well as other safer sex methods, may find it useful to focus on the benefits of decreased fear and anxiety around HIV risk.
It is currently unknown what effect the psychological aspects of PrEP use have on adherence and discontinuation of PrEP. It is likely that those who are experiencing more positive psychological aspects of use are going to continue using PrEP; however, some research has shown that stopping a PrEP regimen is not always within the control of the user (e.g., insurance change, the medication being too expensive) (Whitfield, John, Rendina, Grov, & Parsons, 2018). The psychological change that occurs when use is discontinued has not yet been examined, but it’s possible that some of these benefits gained while taking PrEP (i.e., decreased sexual anxiety) may carry over to other safer sex practices (e.g., condom use), which would explain some findings that safer sex practices begin again after stopping PrEP for some GBM who may have stopped such practices while taking PrEP (Parsons, Whitfield, Rendina, & Grove, 2017).
Taken together these findings suggest there are some psychological benefits to taking PrEP which may be experienced differently depending on the reasons some GBM begin a regimen. Individuals who experience high levels of anxiety related to potential HIV acquisition may notice a decrease in this anxiety while taking PrEP. However, users who are expecting to feel more sexually satisfied or gain more sexual esteem are not likely to experience significant changes. To what end PrEP prescribers have a conversation with their patients about the potential psychological aspects of PrEP use is unknown, but these conversations may be beneficial in helping potential users determine if PrEP is something that is right for them. Future research should include an examination of psychological benefits to use and how they can be utilized to increase uptake for HIV at-risk individuals.
Strengths and Limitations
Among the strengths of this research is the collection of data across multiple time points. This has allowed us to assess whether psychological changes pre- and during PrEP use did occur, something other studies have not yet done. Additionally, the sample for this study comes from a larger cohort of 1,071 GBM, recruited with parameters taken from the U.S. Census. The full cohort is diverse regarding age, geographic distribution, income, relationship status, and education; however, our sample was comprised of only those who had started taking PrEP while enrolled in the study. This created a limited sample mainly comprised of White men who were highly educated, making more than $20k per year, and employed full-time. Because our sample was restricted to only those that had access to PrEP, individuals of lower socioeconomic status may have been excluded. For individuals who do not have health insurance PrEP can cost as much as $14,000 per year (Department of Health, 2012). Although Medicaid does cover at least some of the cost associated with PrEP use, the extent is dependent upon the residential state of the individual. It cannot be determined from these findings what psychological benefits PrEP may provide for those who are of lower socioeconomic statuses. Further, when recruiting for our study, we did not require that participants had recently engaged in sexual risk behavior, only that they had engaged in sex with another man in the past year. It’s possible that these findings may not be generalizable to samples that engage in more sexual risk behaviors and the psychological benefits for a higher risk cohort may be increased.
Another potential limitation was a large number of participants who were sent an invitation for participation into the study did not complete the initial survey. CMI is able to track if potential participants opened the e-mail based on whether the content of the e-mail was downloaded. However, individuals may have begun the e-mail and not downloaded the content, which suggests they did not open the e-mail when in fact they had. Additionally, it is also unknown how many emails were pushed to users spam boxes and not seen by the panelists. The amount of unread messages is consistent with other samples obtained via CMI’s LGBT panel (Voytek et al., 2012). Once the survey was started, our completion rate was over 90%, suggesting that those who began the survey were likely to complete it. Almost 78% of those that were eligible for the study completed all tasks and were enrolled in the final cohort. Inclusion into the final cohort included completion of a more extended survey and submitting samples for STI testing and completing an at-home HIV test. Completion of these three tasks likely contributed to this 22% drop off.
Conclusions
Our findings highlight that some GBM starting PrEP may also experience decreased sexual anxiety. The decrease in sexual anxiety may be due to a decrease in HIV risk-related fears because of PrEP use. We were unable to demonstrate a significant difference in sexual satisfaction and sexual esteem pre- to during PrEP use. More work needs to be done to determine exactly what aspects of sexual anxiety may be affected by PrEP use, and if there are other affective changes.
ACKNOWLEDGMENTS
One Thousand Strong study was funded by a research grant from the National Institute on Drug Abuse (R01-DA036466; Jeffrey T. Parsons & Christian Grov, MPIs). H. Jonathon Rendina was supported by a Career Development Award from the National Institute on Drug Abuse (K01-DA039030; H. Jonathon Rendina, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors would like to acknowledge the contributions of the other members of the One Thousand Strong Study Team (Ana Ventuneac, Demetria Cain, Mark Pawson, Ruben Jimenez, Chloe Mirzayi, Brett Millar, and Raymond Moody) and other staff from the Center for HIV/AIDS Educational Studies and Training (Chris Hietikko, Brian Salfas, Carlos Ponton, and Paula Bertone). We would also like to thank the staff at Community Marketing Inc. (David Paisley, Heather Torch, and Thomas Roth). Finally, we thank Jeffrey Schulden at NIDA, the anonymous reviewers of this manuscript, and all of our participants in the One Thousand Strong study.
Funding: Funding support was provided by the National Institute of Drug Abuse (R01-DA036466; PIs: Parsons & Grov). H. Jonathon Rendina was supported by a National Institute on Drug Abuse Career Development Award (K01-DA039030).
Footnotes
Disclosure of Potential Conflicts of Interest:
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- Amico KR, & Stirratt MJ (2014). Adherence to preexposure prophylaxis: Current, emerging, and anticipated bases of evidence. Clinical Infectious Diseases, 59, 55–60. doi: 10.1093/cid/ciu266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Carballo-Diéguez A, Ventuneac A, & Dolezal C (2009). Assessing motivations to engage in intentional condomless anal intercourse in HIV risk contexts (“bareback sex”) among men who have sex with men. AIDS Education & Prevention, 21, 156–168. doi: 10.1521/aeap.2009.21.2.156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks RA, Kaplan RL, Lieber E, Landovitz RJ, Lee S-J, & Leibowitz AA (2011). Motivators, concerns, and barriers to adoption of preexposure prophylaxis for HIV prevention among gay and bisexual men in HIV-serodiscordant male relationships. AIDS Care, 23, 1136–1145. doi: 10.1080/09540121.2011.554528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2014). Preexposure prophylaxis for the prevention of HIV infection in the United States-2014: A clinical practice guideline. U.S. Public Health Service. Retrieved from http://www.cdc.gov/hiv/pdf/prepprovidersupplement2014.pdf
- Centers for Disease Control and Prevention. (2017a). HIV among gay and bisexual men. Retrieved from https://www.cdc.gov/hiv/group/msm/index.html
- Centers for Disease Control and Prevention. (2017b). Living with HIV. Retrieved from https://www.cdc.gov/hiv/basics/livingwithhiv/index.html
- Closson EF, Mitty JA, Malone J, Mayer KH, & Mimiaga MJ (2017). Exploring strategies for PrEP adherence and dosing preferences in the context of sexualized recreational drug use among MSM: A qualitative study. AIDS Care, 30, 1–8. doi: 10.1080/09540121.2017.1360992 [DOI] [PubMed] [Google Scholar]
- Collins SP, McMahan VM, & Stekler JD (2017). The impact of HIV pre-exposure prophylaxis (PrEP) use on the sexual health of men who have sex with men: A qualitative study in Seattle, WA. International Journal of Sexual Health, 29, 55–68. doi: 10.1080/19317611.2016.1206051 [DOI] [Google Scholar]
- Department of Health. (2012). Pre-exposure prophylaxis (PrEP) to prevent HIV infection: Questions and answers. Retrieved from https://www.health.ny.gov/publications/0265/
- Elam G, Macdonald N, Hickson F, Imrie J, Power R, McGarrigle C, … Evans B (2008). Risky sexual behaviour in context: Qualitative results from an investigation into risk factors for seroconversion among gay men who test for HIV. Sexually Transmitted Infections, 84, 473–477. doi: 10.1136/sti.2008.031468 [DOI] [PubMed] [Google Scholar]
- Godin G, Naccache H, & Pelletier R (2000). Seeking medical advice if HIV symptoms are suspected. Qualitative study of beliefs among HIV-negative gay men. Canadian Family Physician, 46, 861–868. doi: 10.1007/s10461-010-9794-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golub SA, Gamarel KE, Rendina HJ, Surace A, & Lelutiu-Weinberger CL (2013). From efficacy to effectiveness: Facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Patient Care and STDs, 27, 248–254. doi: 10.1089/apc.2012.0419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, … Ramirez-Cardich ME. (2010). Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. The New England Journal of Medicine, 363, 2587–2599. doi: 10.1056/NEJMoa1011205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Cain D, Whitfield TH, Rendina HJ, Pawson M, Ventuneac A, & Parsons JT (2016). Recruiting a US national sample of HIV-negative gay and bisexual men to complete at-home self-administered HIV/STI testing and surveys: Challenges and opportunities. Sexuality Research and Social Policy, 13, 1–21. doi: 10.1007/s13178-015-0212-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Rendina HJ, Moody RL, Ventuneac A, & Parsons JT (2015). HIV serosorting, status disclosure, and strategic positioning among highly sexually active gay and bisexual men. AIDS Patient Care and STDs, 29, 559–568. doi: 10.1089/apc.2015.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Whitfield TH, Rendina HJ, Ventuneac A, & Parsons JT (2015). Willingness to take PrEP and potential for risk compensation among highly sexually active gay and bisexual men. AIDS and Behavior, 19, 2234–2244. doi: 10.1007/s10461-015-1030-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper GW, Tyler AT, Bruce D, Graham L, & Wade RM (2016). Drugs, sex, and condoms: Identification and interpretation of race-specific cultural messages influencing black gay and bisexual young men living with HIV. American Journal of Community Psychology, 58, 463–476. doi: 10.1002/ajcp.12109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hojilla JC, Koester KA, Cohen SE, Buchbinder S, Ladzekpo D, Matheson T, & Liu AY (2016). Sexual behavior, risk compensation, and HIV prevention strategies among participants in the San Francisco PrEP demonstration project: A qualitative analysis of counseling notes. AIDS and Behavior, 20, 1461–1469. doi: 10.1007/s10461-015-1055-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellerman SE, Lehman JS, Lansky A, Stevens MR, Hecht FM, Bindman AB, & Wortley PM (2002). HIV testing within at-risk populations in the United States and the reasons for seeking or avoiding HIV testing. Journal of Acquired Immune Deficiency Syndromes, 31, 202–210. doi: 10.1097/00126334-200210010-00011 [DOI] [PubMed] [Google Scholar]
- Koester K, Amico RK, Gilmore H, Liu A, McMahan V, Mayer K, … Grant R. (2017). Risk, safety and sex among male PrEP users: Time for a new understanding. Culture, Health & Sexuality, 19, 1301–1313. doi: 10.1080/13691058.2017.1310927 [DOI] [PubMed] [Google Scholar]
- Lal L, Audsley J, Murphy DA, Fairley CK, Stoove M, Roth N, … Anderson PL (2017). Medication adherence, condom use and sexually transmitted infections in Australian preexposure prophylaxis users. AIDS, 31, 1709–1714. doi: 10.1097/QAD.0000000000001519 [DOI] [PubMed] [Google Scholar]
- Lorenc T, Marrero-Guillamón I, Llewellyn A, Aggleton P, Cooper C, Lehmann A, & Lindsay C (2011). HIV testing among men who have sex with men (MSM): Systematic review of qualitative evidence. Health Education Research, 26, 834–846. doi: 10.1093/her/cyr064 [DOI] [PubMed] [Google Scholar]
- Maas MK, & Lefkowitz ES (2015). Sexual esteem in emerging adulthood: Associations with sexual behavior, contraception use, and romantic relationships. Journal of Sex Research, 52, 795–806. doi: 10.1080/00224499.2014.945112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer KH, Safren SA, Elsesser SA, Psaros C, Tinsley JP, Marzinke M, … Haberer J. (2017). Optimizing pre-exposure antiretroviral prophylaxis adherence in men who have sex with men: Results of a pilot randomized controlled trial of “Life-Steps for PrEP”. AIDS and Behavior, 21, 1350–1360. doi: 10.1007/s10461-016-1606-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugo PM, Sanders EJ, Mutua G, van der Elst E, Anzala O, Barin B, … Haberer JE. (2015). Understanding adherence to daily and intermittent regimens of oral HIV pre-exposure prophylaxis among men who have sex with men in Kenya. AIDS and Behavior, 19, 794–801. doi: 10.1007/s10461-014-0958-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, DuBois LZ, Prescott TL, & Ybarra ML (2014). A mixed-methods study of condom use and decision making among adolescent gay and bisexual males. AIDS and Behavior, 18, 1955–1969. doi: 10.1007/s10461-014-0810-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Moran K, Feinstein BA, Forscher E, & Mustanski B (2017). Pre-exposure prophylaxis (PrEP) use and condomless anal sex: Evidence of risk compensation in a cohort of young men who have sex with men. Journal of Acquired Immune Deficiency Syndromes, 77, 358–364. doi: 10.1097/QAI.0000000000001604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldenburg CE, Nunn AS, Montgomery M, Almonte A, Mena L, Patel RR, … Chan PA. (2017). Behavioral changes following uptake of HIV pre-exposure prophylaxis among men who have sex with men in a clinical setting. AIDS and Behavior, 22, 1075–1079. doi: 10.1007/s10461-017-1701-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Rendina HJ, Lassiter JM, Whitfield TH, Starks TJ, & Grov C (2017). Uptake of HIV pre-exposure prophylaxis (PrEP) in a national cohort of gay and bisexual men in the United States. Journal of Acquired Immune Deficiency Syndromes, 74, 285–292. doi: 10.1097/QAI.0000000000001251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Rendina HJ, Whitfield TH, & Grov C (2016). Familiarity with and preferences for oral and long-acting injectable HIV pre-exposure prophylaxis (PrEP) in a national sample of gay and bisexual men in the US. AIDS and Behavior, 20, 1390–1399. doi: 10.1007/s10461-016-1370-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Schrimshaw EW, Wolitski RJ, Halkitis PN, Purcell DW, Hoff CC, & Gómez CA (2005). Sexual harm reduction practices of HIV-seropositive gay and bisexual men: Serosorting, strategic positioning, and withdrawal before ejaculation. AIDS, 19, S13–S25. doi: 10.1097/01.aids.0000167348.15750.9a [DOI] [PubMed] [Google Scholar]
- Parsons JT, Whitfield TH, Rendina HJ, & Grov C (2017, July). Differences in biological and behavioral HIV risk before, during, and after PrEP use among a national sample of gay and bisexual men in the United States. Paper presented at the Annual International AIDS Society Conference, Paris, France. [Google Scholar]
- Rendina HJ, Whitfield TH, Grov C, Starks TJ, & Parsons JT (2017). Distinguishing hypothetical willingness from behavioral intentions to initiate HIV pre-exposure prophylaxis (PrEP): Findings from a large cohort of gay and bisexual men in the US. Social Science & Medicine, 172, 115–123. doi: 10.1016/j.socscimed.2016.10.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shernoff M (2006). Condomless sex: Gay men, barebacking, and harm reduction. Social Work, 51, 106–113. doi: 10.1093/sw/51.2.106 [DOI] [PubMed] [Google Scholar]
- Simoni JM, Amico KR, Pearson CR, & Malow R (2008). Strategies for promoting adherence to antiretroviral therapy: A review of the literature. Current Infectious Disease Reports, 10, 515–521. doi: 10.1007/s11908-008-0083-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snell WE (1998). The Multidimensional Sexual Self-Concept Questionaire In Davis CM, Yarber WL, Bauserman R, Schreer G, & David SL (Eds.). Handbook of sexuality-related measures, pp. 521–524. Sage Publications: NY. [Google Scholar]
- Starks TJ, Payton G, Golub SA, Weinberger CL, & Parsons JT (2014). Contextualizing condom use: Intimacy interference, stigma, and unprotected sex. Journal of Health Psychology, 19, 711–720. doi: 10.1177/1359105313478643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storholm ED, Volk JE, Marcus JL, Silverberg MJ, & Satre DD (2017). Risk perception, sexual behaviors, and PrEP adherence among substance-using men who have sex with men: A qualitative study. Prevention Science, 18, 737–747. doi: 10.1007/s11121-017-0799-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai MC-M (2014). The impact of HIV to intimacy and sexual behaviours of gay couples in serodiscordant relationships in Taiwan: A qualitative pilot study. Journal of Therapy & Management in HIV Infection, 2, 24–32. doi: 10.12970/2309-0529.2014.02.01.4 [DOI] [Google Scholar]
- Volk JE, Marcus JL, Phengrasamy T, Blechinger D, Nguyen DP, Follansbee S, & Hare CB (2015). No new HIV infections with increasing use of HIV preexposure prophylaxis in a clinical practice setting. Clinical Infectious Diseases, 61, 1601–1603. doi: 10.1093/cid/civ778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voytek C, Jones K, Curtis B, Fiore D, Dunbar D, Frank I, … Network NHVT (2012). Using an internet consumer marketing strategy to reach men who have sex with men for participation in a preventive HIV vaccine clinical trial. Retrovirology, 9, 119. doi: 10.1186/1742-4690-9-S2-P119 [DOI] [Google Scholar]
- Whitfield TH, John SA, Rendina HJ, Grov C, & Parsons JT (2018). Why I quit pre-exposure prophylaxis (PrEP)? A mixed-method study exploring reasons for PrEP discontinuation and potential re-initiation among gay and bisexual men. AIDS and Behavior, 22, 3566–3575. doi: 10.1007/s10461-018-2045-1 [DOI] [PMC free article] [PubMed] [Google Scholar]


