Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia and is associated with significant morbidity, increased risk of stroke, reduced quality of life, and increased mortality [1]. Catheter ablation is an important treatment option for AF. However, its success rate is below 100% [2]. In addition to concomitant risk factors such as hypertension, diabetes and sleep apnea [3], also the (in) ability to achieve lasting pulmonary vein isolation impacts the efficacy of AF ablation [4]. Therefore, efforts should be made to improve effective lesion placement (Fig. 1).
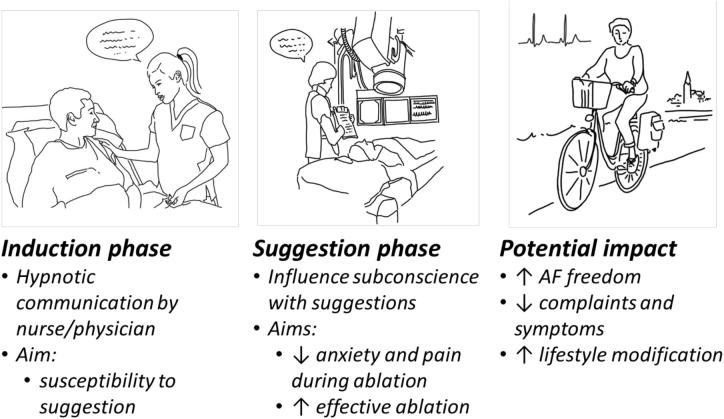
Fig. 1.
Application of hypnotic communication during atrial fibrillation (AF) ablation.
AF ablation can be a disconformable procedure. A patient that experiences pain or discomfort will not be able to remain still on the operating table. Patient movement can complicate lesion placement and limit the efficacy of the ablation. Proper pain management is therefore essential. Conscious sedation and general anesthesia are the most common techniques used for procedural analgesia. Both techniques have their inherent advantages and disadvantages. In brief, general anesthesia provides a higher level of analgesia compared to conscious sedation but is accompanied with higher costs and lower availability because of the need for an anesthesiologist or anesthesia specialist. Importantly, previous studies have suggested that the use of general anesthesia during an ablation procedure improves contact force and stability of the catheter during ablation, reduces gaps during pulmonary vein isolation and reduces AF recurrences [[5], [6], [7]]. As a consequence, the use of general anesthesia may even be cost effective when considering the re-do procedures that can be avoided [7].
In this issue of the International Journal of Cardiology Heart & Vasculatur, Scaglione et al. describe a very interesting alternative to traditional general anesthesia and conscious sedation to facilitate AF ablation, namely hypnotic communication [8]. In an observational study consisting of 140 patients, the authors studied hypnotic communication as an adjuvant analgesic strategy to traditional conscious sedation. They demonstrated that the use of adjuvant hypnotic communication was effective in three quarters of patients to achieve a pain free ablation and resulted in a reduced need for sedative drugs and a reduced need for non-invasive ventilatory support compared to traditional conscious sedation [8]. In addition, the use of hypnotic communication did not require additional personnel.
Hypnotic communication induces hypnosis: a state of consciousness involving focused attention and reduced peripheral awareness characterized by an enhanced capacity for response to suggestion [9]. During the hypnotic state, suggestions are used to prevent normally perceived experiences such as pain or anxiety from reaching the conscious mind. Previous studies demonstrated that hypnotic communication has a positive impact on pain, emotional stress, anxiety and drug consumption during surgery and child labor [10].
The present study by Scaglione et al. is the first to describe the use of hypnotic communication in pain management during AF ablation [8]. The initial results suggest that adjuvant hypnotic communication is effective as periprocedural analgesic with a low risk for adverse events. The use of hypnotic communication during AF ablation is less expensive than general anesthesia, because no additional personnel is needed to perform it. In the current study, after following an in-hospital training, hypnotic communication could be implemented autonomically by the physician performing the ablation or the nurse attending the ablation. Unfortunately, the authors do not deliberate on the exact method of hypnotic communication they have used in their hospital and the amount of time it took for their personnel to master it. In theory, the use of hypnotic communication could be more effective than conscious sedation to facilitate a higher level of analgesia to achieve a more effective pulmonary vein isolation. One could say that adjuvant hypnotic communication has the potential to ‘combine the best of both worlds’ when it comes to periprocedural analgesia during AF ablation.
Important side-effects of general anesthesia are fluctuations in hemodynamics, electrical properties and autonomic activation. Hemodynamic changes due to general anesthesia may necessitate the use of vasoconstrictors and fluid administration to maintain adequate arterial pressure. In a minority of patients, particularly the ones with structural heart disease, this can lead to pulmonary edema and subsequently longer hospital stay. Changes in the electrical properties of the atria and autonomic activation can modify the atrial substrate during the procedure [11]. This can be especially important when the target of the ablation reaches beyond pulmonary vein isolation (e.g. non-pulmonary vein triggers, AV-node dependent reentry tachycardias and focal atrial tachycardias) [12]. Although there seems to be a concern among electrophysiologists about the impact of anesthetic drugs on the (non-) inducibility of arrhythmias in general, data on this subject are limited but do not seem to support these concerns [13]. Nevertheless, hypnotic communication as adjuvant to conscious sedation would render the use for these drugs unnecessary, thereby completely abolishing any concerns.
Additionally, “hypnotherapy” has been proposed previously as an adjunct method to treat cardiovascular risk factors such as obesity, hypertension and sleep apnea. (Self-) hypnosis might be an interesting tool weight loss and combined risk factor modification in AF patients, which has been shown to improve AF symptoms and AF ablation outcomes [14].
In conclusion, the work by Scaglione et al. [8] nicely demonstrates the potential benefits of hypnotic communication to facilitate AF ablation. However, it remains unclear whether hypnotic communication can be taught to everyone and whether it is equally effective among different hospitals and caregivers. Further studies are needed to determine the exact value of hypnotic communication and hypnotherapy in the treatment of AF during ablation procedures and as part of combined risk factor modification programs.
Declaration of Competing Interest
None.
Acknowledgements
We thank Nadine Bemelmans for the excellent figure illustrating our editorial.
References
- 1.Chang T.Y., Liao J.N., Chao T.F., Vicera J.J., Lin C.Y., Tuan T.C., Lin Y.J., Chang S.L., Lo L.W., Hu Y.F., Chung F.P., Chen S.A. Oral anticoagulant use for stroke prevention in atrial fibrillation patients with difficult scenarios. Int. J. Cardiol. Heart Vasc. 2018;20:56–62. doi: 10.1016/j.ijcha.2018.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuck K.H., Brugada J., Furnkranz A., Metzner A., Ouyang F., Chun K.R., Elvan A., Arentz T., Bestehorn K., Pocock S.J., Albenque J.P., Tondo C. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N. Engl. J. Med. 2016;374:2235–2245. doi: 10.1056/NEJMoa1602014. [DOI] [PubMed] [Google Scholar]
- 3.Ayinde H., Schweizer M.L., Crabb V., Ayinde A., Abugroun A., Hopson J. Age modifies the risk of atrial fibrillation among athletes: a systematic literature review and meta-analysis. Int. J. Cardiol. Heart Vasc. 2018;18:25–29. doi: 10.1016/j.ijcha.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nery P.B., Belliveau D., Nair G.M., Bernick J., Redpath C.J., Szczotka A., Sadek M.M., Green M.S., Wells G., Birnie D.H. Relationship between pulmonary vein reconnection and atrial fibrillation recurrence: a systematic review and meta-analysis. JACC Clin. Electrophysiol. 2016;2:474–483. doi: 10.1016/j.jacep.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Chikata A., Kato T., Yaegashi T., Sakagami S., Kato C., Saeki T., Kawai K., Takashima S.I., Murai H., Usui S., Furusho H., Kaneko S., Takamura M. General anesthesia improves contact force and reduces gap formation in pulmonary vein isolation: a comparison with conscious sedation. Heart Vessel. 2017;32:997–1005. doi: 10.1007/s00380-017-0961-z. [DOI] [PubMed] [Google Scholar]
- 6.Di Biase L., Conti S., Mohanty P., Bai R., Sanchez J., Walton D., John A., Santangeli P., Elayi C.S., Beheiry S., Gallinghouse G.J., Mohanty S., Horton R., Bailey S., Burkhardt J.D., Natale A. General anesthesia reduces the prevalence of pulmonary vein reconnection during repeat ablation when compared with conscious sedation: results from a randomized study. Heart Rhythm. 2011;8:368–372. doi: 10.1016/j.hrthm.2010.10.043. [DOI] [PubMed] [Google Scholar]
- 7.Martin C.A., Curtain J.P., Gajendragadkar P.R., Begley D.A., Fynn S.P., Grace A.A., Heck P.M., Salaunkey K., Virdee M.S., Agarwal S. Improved outcome and cost effectiveness in ablation of persistent atrial fibrillation under general anaesthetic. Europace. 2018;20:935–942. doi: 10.1093/europace/eux057. [DOI] [PubMed] [Google Scholar]
- 8.Scaglione M.B.A., Di Donna P., Peyracchia M., Bolzan B., Mazzucchi P., Muro M., Caponi D. Hypnotic communication for periprocedural analgesia during transcatheter ablation of atrial fibrillation. Int. J. Cardiol. Heart Vasc. 2019;24:100405. doi: 10.1016/j.ijcha.2019.100405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elkins G.R., Barabasz A.F., Council J.R., Spiegel D. Advancing research and practice: the revised APA division 30 definition of hypnosis. Int. J. Clin. Exp. Hypn. 2015;63:1–9. doi: 10.1080/00207144.2014.961870. [DOI] [PubMed] [Google Scholar]
- 10.Hauser W., Hagl M., Schmierer A., Hansen E. The efficacy, safety and applications of medical hypnosis. Dtsch. Arztebl. Int. 2016;113:289–296. doi: 10.3238/arztebl.2016.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cervigon R., Moreno J., Perez-Villacastin J., Castells F. Profound sedation with propofol modifies atrial fibrillation dynamics. Pacing Clin. Electrophysiol. 2013;36:1176–1188. doi: 10.1111/pace.12137. [DOI] [PubMed] [Google Scholar]
- 12.Lo L.W., Lin Y.J., Chang S.L., Hu Y.F., Chung F.P., Chen S.A. Beyond pulmonary vein isolation: the role of additional sites in catheter ablation of atrial fibrillation. Curr. Cardiol. Rep. 2017;19:86. doi: 10.1007/s11886-017-0884-4. [DOI] [PubMed] [Google Scholar]
- 13.Mountantonakis S.E., Elkassabany N., Kondapalli L., Marchlinski F.E., Mandel J.E., Hutchinson M.D. Provocation of atrial fibrillation triggers during ablation: does the use of general anesthesia affect inducibility? J. Cardiovasc. Electrophysiol. 2015;26:16–20. doi: 10.1111/jce.12512. [DOI] [PubMed] [Google Scholar]
- 14.Middeldorp M.E., Pathak R.K., Meredith M., Mehta A.B., Elliott A.D., Mahajan R., Twomey D., Gallagher C., Hendriks J.M.L., Linz D., McEvoy R.D., Abhayaratna W.P., Kalman J.M., Lau D.H., Sanders P. PREVEntion and regReSsive effect of weight-loss and risk factor modification on atrial fibrillation: the REVERSE-AF study. Europace. 2018;20:1929–1935. doi: 10.1093/europace/euy117. [DOI] [PubMed] [Google Scholar]