Abstract
Disability is a key social identity or social category that is associated with significant social disadvantage. For men, having a disability can be discordant with their masculine identity. Self-reliance is one component of masculinity that is known to be important to men with disabilities, however it is also known to be associated with adverse mental health outcomes in the broader adult male population. Intersectionality approaches offer a means of examining the way that the effect of self-reliance on mental health might vary between those with and without a disability. Among a sample of 12,052 men aged 18–55 years from the Ten-to-Men study, we used effect measure modification (EMM) to examine the way that self-reliance modifies the relationship between disability and depressive symptoms. Disability was assessed using the Washington Group Short Set of questions, which capture functional limitations. Results showed that men with disabilities who reported higher conformity to self-reliance norms had much worse mental health than non-disabled men with low conformity to self-reliance, as measured in terms of depressive symptoms (PRR: 9.40, 95%CI 7.88, 11.22, p-value<0.001). We found evidence of positive EMM of depressive symptoms by conformity to self-reliance on the additive scale (RERI: 2.84, 95%CI 1.26, 4.42, p-value<0.001). These results provide evidence that high conformity to self-reliance norms exerts a particularly damaging effect on the mental health of men with disabilities. Given that men with disabilities are more likely to rely on help and support from others, these results provide important insights for the delivery of services to men with disability.
Keywords: Intersectionality, Masculinity, Disability, Mental health, Effect measure modification, Self-reliance
Highlights
-
•
Intersectionality has not previously been applied to research among men with disabilities.
-
•
Men with disability reporting high conformity to self-reliance norms showed poorer mental health than others.
-
•
There was evidence of EMM of mental health by conformity to self-reliance on the additive scale.
1. Introduction
On almost every measure, we see health variations across different identities or social statuses such as race, class, gender and disability (Marmot, Friel, Bell, Houweling, & Taylor, 2008), and in almost every context we see that those who are of lower positions in these hierarchies have poorer health outcomes than those of more advantaged or higher positions (Wilkinson & Pickett, 2010). Examining the patterning of health and disease within society, and differences in vulnerabilities and susceptibilities, is fundamental to epidemiological and public health research (Bauer, 2014; Diderichsen, Hallqvist, & Whitehead, 2018).
Historically, examination of these health inequalities has been conducted with a focus on single categories of difference, for example differences by gender or ethnicity. However such approaches do not reflect the reality of the multiplicity of people's identities and social statuses, nor the multiple stratification systems that order these statuses and identities (Hancock, 2007). People are not contained discretely in terms of unitary categories and identities – some people identify with, and are disadvantaged on, more than one of these stratification systems (Hancock, 2007).
Approaches that treat social categories or identities as distinct entities, fail to capture the multiple and sometimes conflicting experiences of oppression and subordination that people in these social categories experience (McCall, 2005). Emerging from work of black feminist scholars (Crenshaw, 1989), intersectionality theory presents a means of understanding and interrogating the multiple axes of difference and disadvantage that different groups experience (Crenshaw, 1989; Hankivsky et al., 2010; Yuval-Davis, 2015).
While intersectionality theory has typically been applied in qualitative research, there is now a burgeoning literature discussing and using quantitative methods to examine the ways that different axes of power and difference intersect to affect health and wellbeing (Bauer, 2014; Gkiouleka, Huijts, Beckfield, & Bambra, 2018; Green, Evans, & Subramanian, 2017; Merlo, 2018; Wemrell, Mulinari, & Merlo, 2017). McCall's (2005) taxonomy of intersectional approaches distinguishes between anti-categorical; inter-categorical; and intra-categorical intersectionality. Inter-categorical approaches, typically favoured by quantitative methods, draw on existing categories to examine and document inequalities among groups, while anti-categorical approaches consider social life and context to be too irreducibly complex to be categorised. Intra-categorical intersectionality approaches, conceptually between anti- and inter-categorical approaches, focus on the margins of certain categories, and are typically deployed using qualitative methods.
Intersectionality theory has commonly been applied to examine two key structures of power and discrimination: racism and sexism. Rarely has intersectionality been applied to bring attention to other systems and structures of oppression and domination such as ableism. Ableism is one important system of marginalization that is relevant to the estimated 15% of the population worldwide who have some form of disability (World Health Organization, 2011). It is defined as “… prejudice and discrimination toward individuals simply because they are classified as disabled – regardless of whether their impairments are physical or mental, visible or invisible.” (Nario-Redmond, 2019, p. 6). Recognition of the ableist social structures and processes that impact on the lives of persons with disabilities is fundamental to conceptualisations of disability (Shakespeare, 2014). Given that disability is one key social identity or social category that is associated with significant social disadvantage King et al., 2018, Krnjacki et al., 2018, Milner et al., 2017 research on disability could benefit from intersectional approaches. Of particular relevance to intersectionality methods, the social model approach to disability emphasises the role of societal barriers such as discrimination, attitudes, and inaccessible environments in the experience of disability (Oliver, 1990; Reeve, 2006; Thomas, 1999).
There is evidence that men with a disability differ to those without a disability in terms of their conformity to certain masculine norms - in particular, men with a disability report greater conformity to self-reliance norms (King, Shields et al., 2019). Self-reliance, the belief that one should be independent and solve their own problems (Labouliere, Kleinman, & Gould, 2015), has previously been associated with greater levels of suicidal ideation ((Pirkis et al., 2017)), and poorer mental health (Milner, Kavanagh, King, & Currier, 2018) in the broader adult male population.
The intersection of disability and masculinity presents a conflict or “status inconsistency” (Gerschick, 2000, p. 1265) for men with disabilities, whereby their perceived status as having a disability is dissonant with their perceived status as men. Men with disability must therefore negotiate this intersection of two competing and sometimes discordant social categories, and interpret and enact masculinities to construct their own identity (Barrett, 2014; Shuttleworth, Wedgwood, & Wilson, 2012). Qualitative evidence among specific groups of men with disabilities indicates that they do this by drawing on different elements of masculinity that can be attained or performed, and disavowing others that are either unattainable or incompatible (Coles, 2008; Gerschick & Miller, 1995). This process varies across individuals, and across type of disability, for example groups of wheelchair rugby players have been observed to align their identity with traditional masculine norms in displays of hyper-masculinity where physical contest, strength and aggression are repeatedly enacted and asserted (Lindemann & Cherney, 2008). Some men acquiring a disability have reported experiences of grief, as they come to understand the loss of their ability to physically embody certain masculine ideals such as athleticism (Wilson, 2004).
While, as noted, there is a relatively established literature examining associations between self-reliance and mental health, it is not known whether this relationship is different for men with and without a disability. The extent to which self-reliance is a positive or negative attribute among men with a disability is important to understand, and may highlight particular vulnerabilities or strengths that can be drawn on when considering service provision. It is certainly possible that a sense of being able to depend on one's own resources may be advantageous to men with a disability, providing a sense of competence and autonomy in a group who are often reliant on others. Alternatively, high self-reliance may be disadvantageous for men with a disability: needing to depend on others to assist them in their daily lives may lead to internal conflict for men who endorse self-reliance norms. Identifying and understanding such differences is vital to meeting the needs of the considerable minority of the population of men who have a disability.
Intersectionality approaches offer particular utility in examining the intersection of disability and self-reliance. Effect measure modification (EMM) has been presented as one way to quantitatively apply intersectional approaches (Bauer, 2014), and Knol and VanderWeele (2012) have presented a recommended approach to interrogate EMM. We drew on the Ten to Men Study, a Longitudinal Cohort Study of over 15,000 Australian men and boys that represents the largest cohort of its kind in the world (Pirkis, Currier et al., 2017). We used EMM methods to examine the intersection of self-reliance and disability, and the effect of this on depressive symptoms. Disability was assessed using the Washington Group Short Set (WG SS), which is based on the International Classification of Functioning (ICF) Disability and Health framework (World Health Organization, 2013). The Washington Group Short Set are designed to capture common functional limitations, and identify those in the population at greatest risk of participation exclusions or restrictions (Madans, Loeb, & Altman, 2011). Given we were particularly interested in differences within the category of men with disabilities, our approach can be conceptually framed in terms of McCall's (2005) intra-categorical approach.
Based on evidence that men with disabilities report greater conformity to self-reliance norms, and that self-reliance is damaging to the mental health of the broader population of men, we sought to examine whether the relationship between disability and depressive symptoms differs between men reporting high conformity to masculine norms of self-reliance, and men reporting low conformity.
2. Methods
2.1. Data source
This study used data from the Australian Longitudinal Study on Male Health (Ten to Men), a longitudinal cohort study established in 2011 to provide evidence to combat the preventable morbidity and premature mortality experienced by Australian men (Pirkis, Currier et al., 2017). The initial wave of data collection commenced in 2013–2014 and included 15,988 men and boys aged 10–55 years. Information was collected across five health domains, including physical health, mental health, health behaviours, social determinants of health, and health service usage. Further details of Ten to Men have been published elsewhere (Currier et al., 2016).
We elected to restrict the sample to the baseline adult cohort, as we were interested in understanding masculinity enacted in an adult population, rather than among a younger cohort where masculinity is still being trialled and established.
2.2. Exposure variable: Disability Status
Disability status was classified according to the Washington Group Short Set of questions, which ask about common functional limitations. These six questions ask individuals about any difficulty experienced in functional domains, including seeing, hearing, walking, cognition, communication, and self-care. The Washington Group questions are well-used, validated internationally, and allow for cross-national comparison of disability prevalence (Madans & Loeb, 2013). Responses were coded on a four-point severity scale: no difficulty, some difficulty, a lot of difficulty, cannot do at all. Disability was considered present if a respondent answered ‘a lot of difficulty’ or ‘cannot do at all’ on one or more functional domains (Madans & Loeb, 2013).
2.3. Outcome variable: Depressive symptoms
The Patient Health Questionnaire [PHQ-9] measures depressive symptoms by asking individuals if they have experienced any of nine problems within the past two weeks, including ‘little interest or pleasure in doing things,’ ‘feeling tired or having little energy,’ and ‘trouble concentrating on things.’ Response options were: not at all, several days, more than half the days, nearly every day. Responses for each question were scored from 0 (‘not at all’) to 3 (‘nearly every day’) and summed for a maximum total score of 27. The PHQ-9 total score may be used continuously, or broken into categories corresponding to severity of depressive symptoms. A score of 10 or above represents the clinically significant threshold of probable depression (Kroenke, Spitzer, Williams, & Löwe, 2010). The PHQ-9 has shown strong validity, good sensitivity, and reasonable specificity (Kroenke, Spitzer, & Williams, 2001).
For analysis, we derived a binary variable based on the threshold of probable depression: none/mild depressive symptoms (<10); and moderate/severe depressive symptoms (10+).
2.4. Effect modifier
Conformity to self-reliance was included in our models as an effect modifier. This measure is a subscale contained within the Conformity to Masculine Norms Inventory (CMNI-22). The CMNI-22 is an abbreviated version of the original 94-item scale (Owen, 2011). Pairs of statements correspond to eleven subscales, of which self-reliance is one.
Respondents were instructed to consider their actions, feelings, and beliefs in relation to two statements focussed on self-reliance, with items assessing the respondents behavioural and affective responses to help-seeking (e.g. “I never ask for help”). Response options range from “strongly disagree” (0) to “strongly agree” (3). We summed responses to provide a conformity score ranging from 0 to 6, with higher scores indicating greater conformity (Mahalik, Talmadge, Locke, & Scott, 2005). Conformity was dichotomized at the 75th percentile, reflecting low/moderate and high conformity.
2.5. Covariates
We also included confounding variables: age (18–24 years, 25–34 years, 35–44 years, 45–55 years); country of birth (Australian born, overseas born); Indigenous status (Aboriginal or Torres Strait Islander, non-Indigenous); education (completed Year 12 (High school), did not complete Year 12); and small area socio-economic disadvantage (categorised into quintiles based on the Index of Relative Socio-Economic Disadvantage (IRSD) (Wise & Mathews, 2011).
2.6. Analytic sample
Fig. 1 presents the analytic sample, which comprised 12,052 men aged 18–55 years (n = 806 men with disability; n = 11,246 men without disability). We conducted complete case analysis, retaining almost 90% of the eligible sample in our analyses.
Fig. 1.
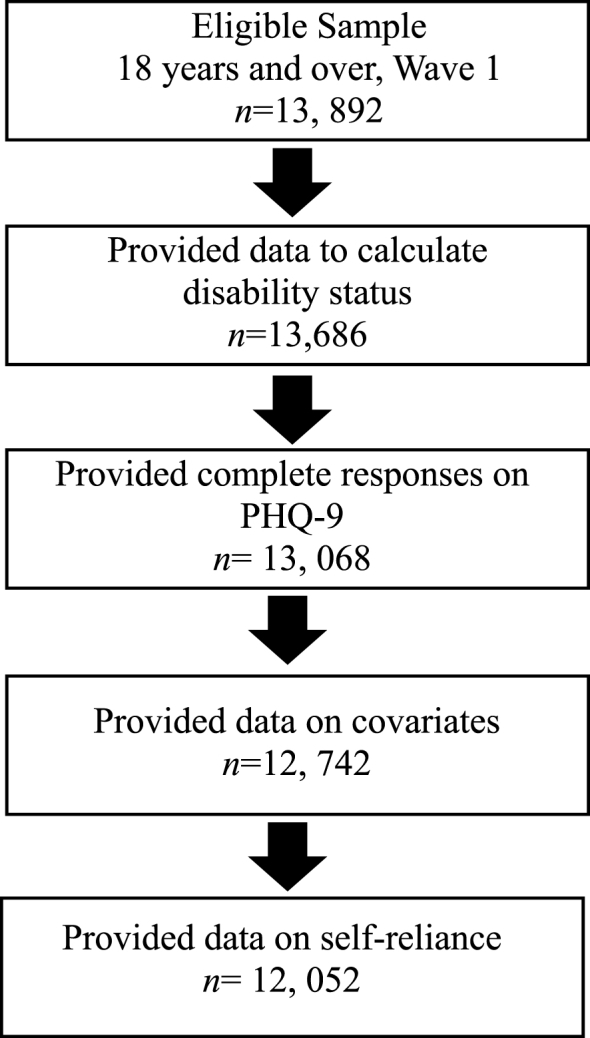
Flowchart for analytic sample.
2.7. Analytic strategy
All data were analysed in Stata using the ‘svy’ suite of commands to accommodate adjustment for sampling characteristics, such as survey weights and stratification (StataCorp, 2017). The weights used were calculated as the inverse of the individual probability of participation in the study (Spittal et al., 2016).
We firstly conducted descriptive analysis and obtained survey-weighted population proportion estimates for age, country of birth, Indigenous status, area disadvantage, education, and depressive symptoms by disability status. We then used survey-weighted adjusted Poisson regression to calculate the prevalence rate ratio (PRR) for having depressive symptoms by disability status within strata of conformity to self-reliance masculine norms. We used a single reference category of no disability/low conformity. We then calculated effect measure modification (EMM) on both the multiplicative and additive scales.
Interactions on the multiplicative scale were computed by using a cross product term; conformity to self-reliance norms*disability status. A PRR equal to 1 indicates a lack of evidence for EMM on the multiplicative scale.
Additive EMM was calculated using the relative excess risk of interaction (RERI) method detailed by VanderWeele and Knol (VanderWeele & Knol, 2014). RERI estimates the prevalence that exceeds what might be expected if the combined effects of self-reliance and disability were purely additive (Knol & VanderWeele, 2012). A RERI equal to 0 indicates no evidence of EMM on the additive scale.
3. Results
3.1. Summary characteristics
Table 1 shows the characteristics of the analytic sample. Compared to men without disability, a greater proportion of men with disability: were older (45–55 years), were born in Australia, were living in areas of greatest disadvantage, and identified as Aboriginal or Torres Strait Islander. A smaller proportion of men with disability had completed Year 12 (High School), compared to men without disability, while a greater proportion of men with disability experienced moderate or severe depressive symptoms.
Table 1.
Descriptive characteristics of analytic sample for covariates and outcomes by disability status.
| No Disability |
Disability |
|||
|---|---|---|---|---|
| n = 11, 246 |
n = 806 |
|||
| n | Percentage(CI) | n | Percentage(CI) | |
| Age | ||||
| 18–24 | 1, 563 | 13.50 (12.48, 14.60) | 109 | 12.92 (10.19, 16.26) |
| 25–34 | 2, 524 | 23.31 (21.76, 24.94) | 157 | 19.21 (15.59, 23.44) |
| 35–44 | 3, 443 | 30.72 (29.41, 32.05) | 214 | 27.34 (23.38, 31.70) |
| 45–55 | 3, 716 | 32.47 (31.03, 33.95) | 326 | 40.53 (36.23, 44.97) |
| Country of Birth | ||||
| Australian born | 8, 607 | 73.12 (71.23, 74.94) | 672 | 80.33 (76.27, 83.85) |
| Overseas born | 2, 639 | 26.88 (25.06, 28.77) | 134 | 19.67 (16.16, 23.73) |
| Indigenous Status | ||||
| Aboriginal and/or Torres Strait Islander | 218 | 1.72 (1.33, 2.24) | 38 | 4.17 (2.82, 6.14) |
| Non-Indigenous | 11, 028 | 98.28 (97.76, 98.68) | 768 | 95.83 (93.86, 97.18) |
| Area disadvantage | ||||
| Most disadvantaged 1 | 1, 997 | 19.95 (16.64, 23.74) | 220 | 28.53 (23.01, 34.78) |
| 2 | 2, 060 | 18.84 (15.62, 22.55) | 191 | 25.47 (20.42, 31.28) |
| 3 | 2, 518 | 23.57 (19.57, 28.11) | 159 | 20.24 (15.62, 25.81) |
| 4 | 2, 361 | 18.28 (14.98, 22.11) | 134 | 12.91 (9.55, 17.24) |
| Least disadvantaged 5 | 2, 310 | 19.36 (15.81, 23.49) | 102 | 12.84 (9.22, 17.62) |
| Education | ||||
| Finished Year 12 | 7, 033 | 66.40 (64.60, 68.16) | 322 | 42.86 (38.31, 47.54) |
| Didn't Finish Year 12 | 4, 213 | 33.60 (31.85, 35.41) | 484 | 57.14 (52.46, 61.70) |
| Depression | ||||
| None/Mild Depressive Symptoms | 10, 098 | 90.07 (89.30, 90.79) | 408 | 50.45 (45.64, 55.25) |
| Moderate/Severe Depressive Symptoms | 1148 | 9.93 (9.21, 10.70) | 398 | 49.55 (44.75, 54.36) |
3.2. Effect measure modification
Table 2 displays the prevalence risk ratios (PRRs) for results of the adjusted analysis of EMM. The non-disability/low self-reliance is the reference group.
Table 2.
Effect Measure Modification of the relationship between disability and depressive symptoms by low/high conformity to self-reliance norms.
| No Disability PRR (95% CI) | Disability PRR (95% CI) | PRR for disability within strata of conformity to self-reliance | |
|---|---|---|---|
| Low Self-Reliance | 1.00 | 4.92 (3.86, 6.27) <0.001 | 4.92 (3.86, 6.27) <0.001 |
| High Self-Reliance | 2.64 (2.25, 3.10) <0.001 | 9.40 (7.88, 11.22) <0.001 | 3.56 (3.19, 4.34) <0.001 |
EMM on multiplicative scale: 0.72 (0.55, 0.96); p-value = 0.024.
EMM on additive scale: 2.84 (1.26, 4.42); p-value<0.001.
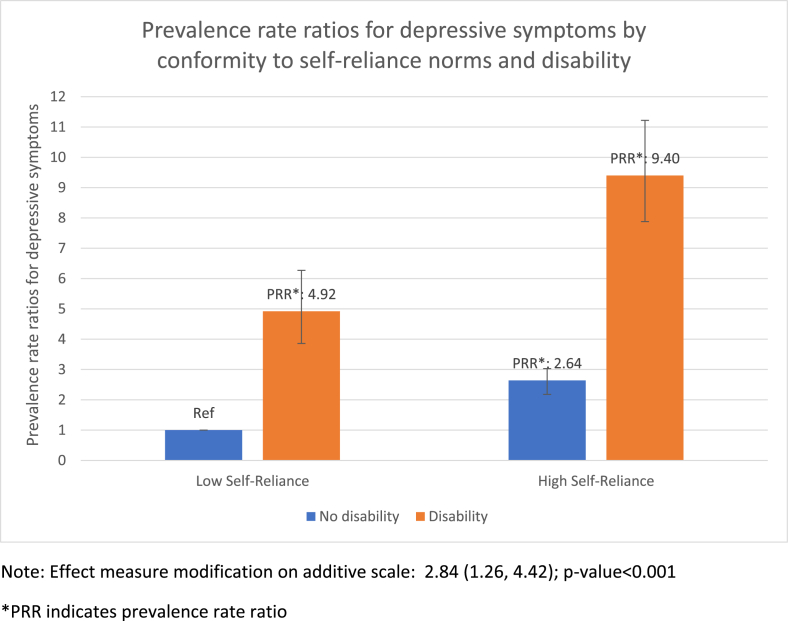
Self-reliance was associated with an increased risk of depressive symptoms. However, regardless of conformity to the self-reliance norm, depressive symptoms were worse among men with a disability. Among men without a disability, heightened conformity to self-reliance was strongly associated with increased depressive symptoms (PRR: 2.64, 95% CI 2.25, 3.10, p-value<0.001). For men with a disability, the risk of depressive symptoms was substantially greater among those reporting high conformity to self-reliance (PRR: 9.40, 95%CI 7.88, 11.22, p-value<0.001). The stratum specific estimates convey the strong effect of disability on depressive symptoms: for men with low self-reliance, those with a disability had a higher risk of having depressive symptoms than those without a disability (4.92, 95%CI 3.86, 6.27, p < 0.001). Similarly, for men reporting high self-reliance, those with a disability had a higher risk of reporting depressive symptoms than those without a disability (PRR 3.56, 95%CI 3.19, 4.34, p < 0.001).
Using EMM methods to examine the way that the intersection of these two constructs (disability and self-reliance) exerts an effect on mental health, we found evidence to support positive EMM of the relationship between disability and depressive symptoms by conformity to self-reliance on the additive scale (RERI: 2.84, 95%CI 1.26, 4.42, p-value<0.001). The additive EMM result suggests that the combined effect of disability and high conformity to self-reliance on depressive symptoms was stronger than the independent effect of having a disability and strongly conforming to self-reliance. See also Fig. 2 for a graphical representation of these associations.
Fig. 2.
Prevalence rate ratios for PHQ-9 by conformity to self-reliance norms and disability.
Note: Effect measure modification on additive scale: 2.84 (1.26, 4.42); p-value<0.001
*PRR indicates prevalence rate ratio.
The results of the EMM on the multiplicative scale however, indicates that the effect of disability and high conformity to self-reliance was smaller than the effect of disability and low conformity to self-reliance (0.72, 95%CI 0.55, 0.96, p-value = 0.024).
4. Discussion
This study is the first that we are aware of to apply an intersectional lens to examine axes of disadvantage among men with disability. Specifically, we sought to examine the way that conformity to the self-reliance masculinity norm might modify the relationship between disability and depressive symptoms. In doing this, we demonstrated that the intersection between disability and a specific dimension of masculinity, self-reliance, can exert a deleterious effect on the mental health of men with disabilities. While self-reliance is harmful to the mental health of the broad population of men, and having a disability has a negative effect on the mental health of men, the intersection of these identities and positions acts to amplify their effects on the mental health of men with disabilities.
4.1. The effect of disability
While we observed statistical evidence of EMM on the additive scale for this specific masculinity subscale in relation to disability and mental health, what is most notable in these results is the stark difference between those with and without a disability. Substantially more men with a disability were classified as having moderate or severe depressive symptoms than those without a disability. This pertained to men with both low and high conformity to the self-reliance subscale: regardless of the extent to which the self-reliance subscale was conformed to, men with a disability had an increased risk of having depressive symptoms compared to men without a disability.
These results are also concordant with previous research that has demonstrated significant associations between having a disability and poorer mental health (Emerson, Llewellyn, Honey, & Kariuki, 2012; King et al., 2018; World Health Organization, 2011). These associations have been observed across the life-course, including among adolescents (King, Milner, Aitken, & Emerson, 2019; King et al., 2018) and adults (Kavanagh et al., 2015; Lucas, 2007; Turner & Noh, 1988).
Studies among people acquiring a disability enable the assessment of the causal effect of disability on mental health, because the temporal sequencing between disability and mental health is clear. Such studies have demonstrated that the acquisition of disability is associated with a decline in mental health (Kavanagh et al., 2015; Lucas, 2007), however the effect of disability appears to be buffered by wealth (Kavanagh et al., 2015) and education (Mandemakers & Monden, 2010). This aligns with the social model of disability, which recognises that the way society is organised presents barriers that restrict participation and choices of people with disability (Oliver, 1990; Reeve, 2006; Thomas, 1999). This includes discrimination and attitudes: both of which are known to impose mental health burdens on those affected (Hatzenbuehler, Phelan, & Link, 2013; Krnjacki et al., 2018). Furthermore, men with a disability may have a negative sense of self, owing to stigma and exclusion, or due to the difficulties of life with illness or impairment.
4.2. The effect of self-reliance
Stratum specific results indicate that regardless of disability status, high conformity to self-reliance masculine norms was associated with significantly poorer mental health. This is consistent with other research that has demonstrated associations between conformity to self-reliance masculine norms and suicidal ideation (Pirkis, Spittal et al., 2017), and poorer mental health (Milner et al., 2018). High conformity to self-reliance has also been shown to be related to risky health behaviours (and less health promoting behaviours) (Mahalik, Levi-Minzi, & Walker, 2007). Self-reliance is considered to be tied to masculine norms related to independence and stoicism – characteristics that, along with physical toughness and strength, are clearly valorised in certain masculine contexts and arenas such as sport (Addis & Mahalik, 2003). The self-reliance items in the CMNI-22 reflect attitudes to help-seeking, and indeed evidence suggests that high conformity to self-reliance inhibits help-seeking (Addis & Mahalik, 2003). While self-reliance may serve men well in certain contexts, feeling unable to seek help in times of need or crisis is likely disadvantageous to mental health. It is speculated that men who conform to masculine norms related to self-reliance and emotional control may find it difficult to have positive relationships with others, and may experience patterns of social isolation due to difficulties engaging in interpersonal relationships (Mahalik et al., 2005).
4.3. The intersection of disability and self-reliance
The results of the EMM were somewhat contradictory: on the additive scale, there was evidence to support positive EMM, that is, that having a disability and strongly conforming to self-reliance was associated with greater risk of depressive symptoms than the sum of the estimated effect of disability alone, and the estimated effect of self-reliance alone. On the multiplicative scale, however, there was evidence of negative EMM: that is, the joint effect of disability and self-reliance was less than the product of the estimated effect of disability alone and the estimated effect of self-reliance alone. This however, is likely due to the substantial and detrimental effect of having a disability over-riding other axes of disadvantage. We also note that the additive scale is preferred for public health purposes, as it indicates the extent to which a risk factor exerts a greater effect on outcomes in one population compared with those of another population (Knol & VanderWeele, 2012). In terms of the results for EMM on the additive scale, it is clear that the detrimental mental health effects of conforming to self-reliance norms are greater for those men with a disability.
Applying intersectionality theory provides a useful framework upon which to view these results, as it enables assessment of the impact of simultaneous processes and systems of power and oppression, including ableism (Hankivsky et al., 2014). Notwithstanding the apparent detrimental mental health effect of conformity to self-reliance norms on all men, there are several possible reasons why the effects were particularly observed among men with disabilities. Ableism intersects with hegemonic masculine ideals, and this is the backdrop against which this population of men establishes and views their identity. Within most societies and contexts, there is a ‘currently accepted’ masculine ideal that attains a hegemonic position (Connell, 2005). The constitution of this accepted or ideal masculinity, expressed in terms of earning and being the breadwinner, as well as physical competence and strength, may exclude men who cannot meet these aspects of masculinity, including men with disabilities (Connell, 2005). For men with disabilities, this dissonance between their masculine identity, and their disability identity may exert a detrimental effect on their mental health.
It has previously been speculated that high conformity to self-reliance observed among men with disabilities may indicate that self-reliance constitutes a dimension of masculinity that is attainable for men with disabilities, and that coheres with their own construction of masculinity (King, Shields et al., 2019). While these results do not contravene the postulated attainability or importance of self-reliance for men with a disability, they suggest that if self-reliance is attainable, it is disadvantageous to men with a disability.
Other research has documented powerlessness, and a sense of frustration at perceived dependence on others among men with disabilities (Joseph & Graham, 2007; Ostrander, 2008). A sense of agency, independence and self-reliance are fundamental to normative constructions of masculinity (Barrett, 2014; Joseph & Graham, 2007). It is therefore possible that the discordance between masculine ideals of self-reliance, and perceived powerlessness or dependence acts to exert a negative effect on the mental health of men with disabilities. These effects may be compounded by norms that prevent help-seeking. Alternatively, aligning with the social model, it is possible that trying hard to be independent and self-reliant in a world which excludes and disempowers you is stressful, and has a damaging effect on the mental health of men with disabilities. Further work, ideally using qualitative methods, is needed to understand the relationship between self-reliance and mental health among men with disabilities.
4.4. Strengths and limitations
There are several limitations to this analysis. Applications of quantitative methods to intersectionality remains inchoate. Other researchers have noted the need for an eco-epidemiologic approach that allows for the simultaneous investigation of between group variation and within group variation (Green et al., 2017): the effect measure modification methods used here cannot assess such variation.
Secondly, disability can be measured in multiple ways (Simeonsson et al., 2003), and it is possible that the measure used in this study inadequately captured disability. One criticism of the Washington Group questions (used in this study) is that they do not sufficiently capture mental health conditions (Sabariego et al., 2015). However, in this analysis, this constitutes a strength as it means that potential conflation between the exposure and outcome was minimised.
Our measure of disability operationalised disability according to self-reported functioning on six domains in a way that assumes an equivalence of conditions that is unlikely to match reality. In other words, impaired functioning on one domain is not equivalent to impaired functioning on other domains. Secondly, as noted, masculinity is a contestable, shifting construct. We examined one posited construct of masculinity, self-reliance, however we note that the relationship between disability and masculinity is likely to vary by disability impairment type and domain of masculinity. There is some evidence that men who have intellectual disabilities may be less likely to conform to normative masculine ideals (Wilson, Parmenter, Stancliffe, & Shuttleworth, 2013). This research is unable to tease out the nuances of such associations. Experiences of masculinity and disability are also likely to vary depending on whether a disability is present at birth or acquired later in life– for men who acquire a disability later in life, their masculine identity precedes their disability, whereas for those born with a disability, their masculine identity is forged concurrent with their disability identity.
While the CMNI has demonstrated good psychometric properties (Mahalik et al., 2003), it was developed among white college students in the United States. There is evidence that masculinity is understood, experienced and expressed differently across different ethnic groups and cultural contexts (Griffith, Gunter, & Watkins, 2012). While our analyses controlled for Indigeneity and country of birth, the extent to which masculine norms developed to reflect mainstream American values, are applicable to Australian society, is not known.
As questionnaires for this research were self-completed it is possible that those with an intellectual disability or visual impairment may be under-represented in analyses.
We also note that the relationship between disability, masculinity and occupation is complex. While education, country of birth, Indigenous status, and age are all clearly confounders of the relationship between disability and masculinity, it is less clear that occupation is a confounder and for this reason, our regression models did not control for occupation. Disability could be a prior cause of occupation (in which case occupation is a mediator), and occupation could be a prior cause of disability (in which case it is a confounder).
We note several strengths of this paper. Firstly, the use of intersectional methods advances understanding of how different social processes and identities impact on the health and wellbeing of men with disabilities. Secondly, we used a large representative dataset. Thirdly, we used a validated measure of disability. While the Washington Group short set of questions on disability do not capture all experiences of disability, the questions have been validated in many countries, cover most common functional limitations, and permit cross-national comparisons (Madans & Loeb, 2013).
4.5. Conclusions
Taking an intersectional lens and using effect measure modification methods enabled us to extend existing knowledge and interrogate the way that disability intersects with the specific masculine norms of self-reliance, to affect mental health. Our results provide important new insights regarding this intersection of disability and self-reliance norms, and how this exerts effects on mental health. We found evidence of EMM of the relationship between disability and mental health by self-reliance, such that disabled men who reported higher conformity to self-reliance had much worse mental health, as measured in terms of depressive symptoms.
It was also clear however, that regardless of level of conformity to masculine ideals of self-reliance, men with disabilities had poorer mental health than those without.
These results have important implications for the delivery of services to men with disabilities, as they firstly highlight the mental health differences between men with and without disabilities, and further indicate that the intersection of disability and self-reliance norms exerts a particularly damaging effect on mental health. This suggests a role of practitioners and advocates in ensuring that men with disabilities have both the necessary assistive technologies, as well as enabling environments, to support them to be successfully self-reliant. A second priority for practitioners and advocates is to encourage men with disabilities to accept support where it is needed.
Given that men with disabilities are more likely to rely on help and support from others, it is important that training for disability carers, personal assistants, and support workers recognises that high conformity to self-reliance can be damaging, and that interventions respect, challenge and accommodate this.
Disclosures
Declarations of interest: none.
Ethics statement
Data for this study was drawn from the Ten to Men study, an Australian Longitudinal Study on Male Health (Pirkis, Currier et al., 2017). Ten to Men received approval from the University of Melbourne Human Research Ethics Committee and conformed to the principles embodied in the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study. Access and use of Ten to Men is available publicly. Researchers can apply to the Australian Institute of Family Studies (https://tentomen.org.au/index.php/researchers.html).
Acknowledgements
This work was supported by a Disability Research Initiative grant from the University of Melbourne, an NHMRC Centre of Research Excellence in Disability and Health grant (APP1116385), an NHMRC Partnership Project (APP1134499), a University of Melbourne, Melbourne School of Population and Global Health, Business Improvement Program (BIP) Reinvestment grant.
TLK was supported by an University of Melbourne, MDHS ECR grant.
AM was supported by a Victorian Health and Medical Research Fellowship.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2019.100464.
Contributor Information
Tania L. King, Email: tking@unimelb.edu.au.
Marissa Shields, Email: marissa.shields@unimelb.edu.au.
Tom Shakespeare, Email: tom.shakespeare@lshtm.ac.uk.
Allison Milner, Email: allison.milner@unimelb.edu.au.
Anne Kavanagh, Email: amkava@unimelb.edu.au.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Addis M.E., Mahalik J.R. Men, masculinity, and the contexts of help seeking. American Psychologist. 2003;58(1):5–14. doi: 10.1037/0003-066X.58.1.5. [DOI] [PubMed] [Google Scholar]
- Barrett T. Disabled masculinities: A review and suggestions for further research. Masculinities Social Change. 2014;3:36–61. doi: 10.4471/mcs.2014.41. [DOI] [Google Scholar]
- Bauer G.R. Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Social Science & Medicine. 2014;110:10–17. doi: 10.1016/j.socscimed.2014.03.022. [DOI] [PubMed] [Google Scholar]
- Coles T. Finding space in the field of masculinity: Lived experiences of men's masculinities. Journal of Sociology. 2008;44:233–248. doi: 10.1177/1440783308092882. [DOI] [Google Scholar]
- Connell R. Second. A&U Academic; Cambridge, UK: 2005. Masculinities. [Google Scholar]
- Crenshaw K. Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum. 1989;140:139–167. [Google Scholar]
- Currier D., Pirkis J., Carlin J., Degenhardt L., Dharmage S.C., Giles-Corti B. The Australian longitudinal study on male health-methods. BMC Public Health. 2016;16:1030. doi: 10.1186/s12889-016-3698-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diderichsen F., Hallqvist J., Whitehead M. Differential vulnerability and susceptibility: How to make use of recent development in our understanding of mediation and interaction to tackle health inequalities. International Journal of Epidemiology. 2018:1–7. doi: 10.1093/ije/dyy167. [DOI] [PubMed] [Google Scholar]
- Emerson E., Llewellyn G., Honey A., Kariuki M. Lower well-being of young Australian adults with self-reported disability reflects their poorer living conditions rather than health issues. Australian & New Zealand Journal of Public Health. 2012;36:176–182. doi: 10.1111/j.1753-6405.2011.00810.x. [DOI] [PubMed] [Google Scholar]
- Gerschick T. Toward a theory of disability and gender. Signs: Journal of Women in Culture and Society. 2000;25:1263–1268. doi: 10.1086/495558. [DOI] [Google Scholar]
- Gerschick T., Miller A. Coming to terms: Masculinity and physical disability. In: Sabo D.F., Gordon D.F., editors. Research on men and masculinities series, vol. 8. Men's health and illness: Gender, power, and the body. SAGE Publications, Inc.; Thousand Oaks, CA: 1995. pp. 183–204. [DOI] [Google Scholar]
- Gkiouleka A., Huijts T., Beckfield J., Bambra C. Understanding the micro and macro politics of health: Inequalities, intersectionality & institutions - a research agenda. Social Science & Medicine. 2018;200:92–98. doi: 10.1016/J.SOCSCIMED.2018.01.025. [DOI] [PubMed] [Google Scholar]
- Green M.A., Evans C.R., Subramanian S.V. Can intersectionality theory enrich population health research? Social Science & Medicine. 2017;178:214–216. doi: 10.1016/j.socscimed.2017.02.029. [DOI] [PubMed] [Google Scholar]
- Griffith D.M., Gunter K., Watkins D.C. Measuring masculinity in research on men of color: Findings and future directions. American Journal of Public Health. 2012;102 doi: 10.2105/AJPH.2012.300715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hancock A.-M. When multiplication doesn't equal quick addition: Examining intersectionality as a research paradigm. Perspectives on Politics. 2007;5:63–79. doi: 10.1017/S1537592707070065. [DOI] [Google Scholar]
- Hankivsky O., Colleen R., Cormier R., Varcoe C., Clark N., Benoit C. Exploring the promised of intersectionality for advancing women's health research. International Journal for Equity in Health. 2010;9:1–15. doi: 10.1186/1475-9276-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankivsky O., Grace D., Hunting G., Giesbrecht M., Fridkin A., Rudrum S. An intersectionality-based policy analysis framework: Critical reflections on a methodology for advancing equity. International Journal for Equity in Health. 2014;13 doi: 10.1186/s12939-014-0119-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler M.L., Phelan J.C., Link B.G. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health. 2013;103:813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph L., Graham L. The construction of adolescent masculinity by visually impaired adolescents. Psychology, Society. 2007;35:73–90. [Google Scholar]
- Kavanagh A.M., Aitken Z., Krnjacki L., LaMontagne A.D., Bentley R., Milner A. Mental health following acquisition of disability in adulthood—the impact of wealth. PLoS One. 2015;10 doi: 10.1371/journal.pone.0139708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King T., Aitken Z., Milner A., Emerson E., Priest N., Karahalios A. To what extent is the association between disability and mental health in adolescents mediated by bullying? A causal mediation analysis. International Journal of Epidemiology. 2018;47:1402–1413. doi: 10.1093/ije/dyy154. [DOI] [PubMed] [Google Scholar]
- King T., Milner A., Aitken Z., Emerson E.K.A. Mental health of adolescents: Variations by disability and borderline intellectual functioning. European Child & Adolescent Psychiatry. 2019:1–10. doi: 10.1007/s00787-019-01278-9. [DOI] [PubMed] [Google Scholar]
- King T., Shields M., Milner A., Vaughan C., Shakespeare T., Currier D. Conformity to masculine norms: Differences between men with and without a disability. Psychology of Men & Masculinities. 2019 In press. [Google Scholar]
- Knol M.J., VanderWeele T.J. Recommendations for presenting analyses of effect modification and interaction. International Journal of Epidemiology. 2012;41:514–520. doi: 10.1093/ije/dyr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krnjacki L., Priest N., Aitken Z., Emerson E., Llewellyn G., King T. Disability-based discrimination and health: Findings from an Australian-based population study. Australian & New Zealand Journal of Public Health. 2018;42:172–174. doi: 10.1111/1753-6405.12735. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W., Löwe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. General Hospital Psychiatry. 2010;32:345–359. doi: 10.1016/J.GENHOSPPSYCH.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Labouliere C., Kleinman M., Gould M. When self-reliance is not safe: Associations between reduced help-seeking and subsequent mental health symptoms in suicidal adolescents. International Journal of Environmental Research and Public Health. 2015;12:3741–3755. doi: 10.3390/ijerph120403741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindemann K., Cherney J.L. Communicating in and through “Murderball”: Masculinity and disability in wheelchair rugby. Western Journal of Communication. 2008;72:107–125. doi: 10.1080/10570310802038382. [DOI] [Google Scholar]
- Lucas R.E. Long-term disability is associated with lasting changes in subjective well-being: Evidence from two nationally representative longitudinal studies. Journal of Personality and Social Psychology. 2007;92:717–730. doi: 10.1037/0022-3514.92.4.717. [DOI] [PubMed] [Google Scholar]
- Madans J.H., Loeb M. Methods to improve international comparability of census and survey measures of disability. Disability & Rehabilitation. 2013;35:1070–1073. doi: 10.3109/09638288.2012.720353. [DOI] [PubMed] [Google Scholar]
- Madans J.H., Loeb M.E., Altman B.M. Measuring disability and monitoring the UN convention on the rights of persons with disabilities: The work of the Washington group on disability statistics. BMC Public Health. 2011;4:1–8. doi: 10.1186/1471-2458-11-S4-S4. Supp. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahalik J.R., Levi-Minzi M., Walker G. Masculinity and health behaviors in Australian men. Psychology of Men and Masculinity. 2007;8:240–249. doi: 10.1037/1524-9220.8.4.240. [DOI] [Google Scholar]
- Mahalik J.R., Locke B.D., Ludlow L.H., Diemer M.A., Scott R.P.J., Gottfried M. Development of the conformity to masculine norms inventory. Psychology of Men and Masculinity. 2003;4:3–25. doi: 10.1037/1524-9220.4.1.3. [DOI] [Google Scholar]
- Mahalik J.R., Talmadge W.T., Locke B.D., Scott R.P.J. Using the conformity to masculine norms inventory to work with men in a clinical setting. Journal of Clinical Psychology. 2005;61:661–674. doi: 10.1002/jclp.20101. [DOI] [PubMed] [Google Scholar]
- Mandemakers J.J., Monden C.W.S. Does education buffer the impact of disability on psychological distress? Social Science & Medicine. 2010;71:288–297. doi: 10.1016/J.SOCSCIMED.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Marmot M., Friel S., Bell R., Houweling T.A., Taylor S. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet. 2008;372:1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- McCall L. Vol. 30. 2005. pp. 1771–1800. (The complexity of intersectionality. Signs (chic)). [DOI] [Google Scholar]
- Merlo J. Multilevel analysis of individual heterogeneity and discriminatory accuracy (MAIHDA) within an intersectional framework. Social Science & Medicine. 2018;203:74–80. doi: 10.1016/j.socscimed.2017.12.026. [DOI] [PubMed] [Google Scholar]
- Milner A., Kavanagh A., King T., Currier D. The influence of masculine norms and occupational factors on mental health: Evidence from the baseline of the Australian longitudinal study on male health. American Journal of Men's Health. 2018;12:696–705. doi: 10.1177/1557988317752607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milner A., King T.L., Lamontagne A.D., Aitken Z., Petrie D., Kavanagh A.M. Underemployment and its impacts on mental health among those with disabilities: Evidence from the HILDA cohort. Journal of Epidemiology & Community Health. 2017;71:1198–1202. doi: 10.1136/jech-2017-209800. [DOI] [PubMed] [Google Scholar]
- Nario-Redmond M. Wiley-Blackwell; Hoboken, NJ: 2019. ABLEISM: The causes and consequence of disability prejudice. [Google Scholar]
- Oliver M. Macmillan; London: 1990. The politics of disablement. [Google Scholar]
- Ostrander R.N. When identities collide: Masculinity, disability and race. Disability & Society. 2008;23:585–597. doi: 10.1080/09687590802328451. [DOI] [Google Scholar]
- Owen J. Assessing the factor structures of the 55- and 22-item versions of the conformity to masculine norms inventory. American Journal of Men's Health. 2011;5:118–128. doi: 10.1177/1557988310363817. [DOI] [PubMed] [Google Scholar]
- Pirkis J., Currier D., Carlin J., Degenhardt L., Dharmage S.C., Giles-Corti B. Cohort profile: Ten to men (the Australian longitudinal study on male health) International Journal of Epidemiology. 2017;46:dyw055. doi: 10.1093/ije/dyw055. [DOI] [PubMed] [Google Scholar]
- Pirkis J., Spittal M.J., Keogh L., Mousaferiadis T., Currier D. Masculinity and suicidal thinking. Social Psychiatry and Psychiatric Epidemiology. 2017;52:319–327. doi: 10.1007/s00127-016-1324-2. [DOI] [PubMed] [Google Scholar]
- Reeve D. Towards a psychology of disability: The emotional effects of living in a disabling society. In: Goodley D., Lawthom R., editors. Disability and psychology: Critical introductions and reflections. Palgrave MacMillan; Hampshire, UK: 2006. pp. 94–108. [Google Scholar]
- Sabariego C., Oberhauser C., Posarac A., Bickenbach J., Kostanjsek N., Chatterji S. Measuring disability: Comparing the impact of two data collection approaches on disability rates. International Journal of Environmental Research and Public Health. 2015;12:10329–10351. doi: 10.3390/ijerph120910329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakespeare T. Second. Routledge; Abingdon, Oxon, UK: 2014. Disability rights and wrongs revisited. [Google Scholar]
- Shuttleworth R., Wedgwood N., Wilson N. The dilemma of disabled masculinity. Men and Masculinities. 2012;15:174–194. doi: 10.1177/1097184X12439879. [DOI] [Google Scholar]
- Simeonsson R.J., Leonardi M., Lollar D., Bjorck-Akesson E., Hollenweger J., Martinuzzi A. Applying the international classification of functioning, disability and health (ICF) to measure childhood disability. Disability & Rehabilitation. 2003;25:602–610. doi: 10.1080/0963828031000137117. [DOI] [PubMed] [Google Scholar]
- Spittal M.J., Carlin J.B., Currier D., Downes M., English D.R., Gordon I. The Australian longitudinal study on male health sampling design and survey weighting: Implications for analysis and interpretation of clustered data. BMC Public Health. 2016;16(S3):1062. doi: 10.1186/s12889-016-3699-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp . Vol 15. 2017. (Stata statistical software: Release). [Google Scholar]
- Thomas C. Open University Press; Buckingham, UK: 1999. Female forms : Experiencing and understanding disability. [Google Scholar]
- Turner R.J., Noh S. Physical disability and depression: A longitudinal analysis. Journal of Health and Social Behavior. 1988;29:23. doi: 10.2307/2137178. [DOI] [PubMed] [Google Scholar]
- VanderWeele T.J., Knol M.J. A tutorial on interaction. Epidemiologic Methods. 2014;3:33–72. doi: 10.1515/em-2013-0005. [DOI] [Google Scholar]
- Wemrell M., Mulinari S., Merlo J. An intersectional approach to multilevel analysis of individual heterogeneity (MAIH) and discriminatory accuracy. Social Science & Medicine. 2017;178:217–219. doi: 10.1016/j.socscimed.2017.02.040. [DOI] [PubMed] [Google Scholar]
- Wilkinson R., Pickett K. Penguin; London, UK: 2010. The spirit level: Why equality is better for everyone. [Google Scholar]
- Wilson D. Fighting polio like a man: Intersections of disability, masculinity, and aging. In: Smith B.G., Hutchison B., editors. Gendering disability. Rutgers UP; New Brunswick, NJ: 2004. pp. 199–233. [Google Scholar]
- Wilson N., Parmenter T., Stancliffe R., Shuttleworth R. From diminished men to conditionally masculine: Sexuality and Australian men and adolescent boys with intellectual disability. Culture, Health and Sexuality. 2013;15:738–751. doi: 10.1080/13691058.2013.780262. [DOI] [PubMed] [Google Scholar]
- Wise P., Mathews R. Getting a Handle on Individual Diversity Within Areas; Canberra: 2011. Socio-economic indexes for areas. [Google Scholar]
- World Health Organization . WHO; Geneva: 2011. World report on disability. [PubMed] [Google Scholar]
- World Health Organization . WHO; Geneva: 2013. How to use the ICF: A practical manual for using the international classification of functioning, disability and health (ICF) [Google Scholar]
- Yuval-Davis N. Situated intersectionality and social inequality. Raisons Politiques. 2015;58:91. doi: 10.3917/rai.058.0091. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.