ABSTRACT
The American Indian (AI) population suffers from significant health disparities, including nutrition-related chronic diseases (diabetes, cancer, and heart disease). Several risk factors for disease and social determinants of health have unique histories in the AI population, including historical trauma, boarding schools, adverse childhood experiences, poverty, federal food programs, and food deserts. To effectively address these disparities, a multipronged approach in collaboration with stakeholders is needed to address the upstream social determinants of health and to increase access to healthier foods. Promising practices and strategies can be considered in several focus areas, including 1) improving existing food programs, 2) promoting breastfeeding and early childhood nutrition, 3) promoting food sovereignty and access to traditional foods, 4) expanding locally cultivated foods, and 5) taxing unhealthy foods and subsidizing healthier options. As these strategies are implemented, it is vital that they are studied, evaluated, and reported to expand tribally specific evidence-based practices.
Keywords: American Indian, health disparities, social determinants, historical trauma, nutrition
Introduction
American Indian (AI) populations are diverse in terms of history, culture, disease patterns, and nutritional health. Expanded research and evaluation of individual community health and nutritional status is needed to make informed policy decisions that will appropriately apply to the multitude of AI populations. However, much is known about the broader social determinants of AI health that suggests nutrition is a significant concern. WHO (1) defines the social determinants of health as the conditions in which people are born, grow, live, work, and age. These factors are influenced by the pattern of resource distribution in a population. The social determinants of health have a significant impact on health inequities, access to healthy food, and preventable disparities in health status seen across populations. In keeping with the analytical approach of social determinants, we need to understand the systemic reasons for unhealthy diets observed in many AI populations (e.g., food deserts) so the most effective interventions can be crafted.
One major historical consideration is the forced relocation of AI people from their ancestral lands to reservations (2), thereby severely restricting access to traditional food systems that historically included regionally specific hunting, gathering, fishing, and farming (3, 4). The loss of traditional food sources also resulted in dependence on federal government programs such as the Food Distribution Program on Indian Reservations (FDPIR) that included the distribution of foods such as lard, canned meats, white flour, salt, and sugar (5, 6). Although this article focuses on the social determinants affecting the current population and the disparities that ensue, these historic policies and resultant changes in lifestyle are unique to AI people and have led to intergenerational harm to population health.
AI Demographics and Health Disparities
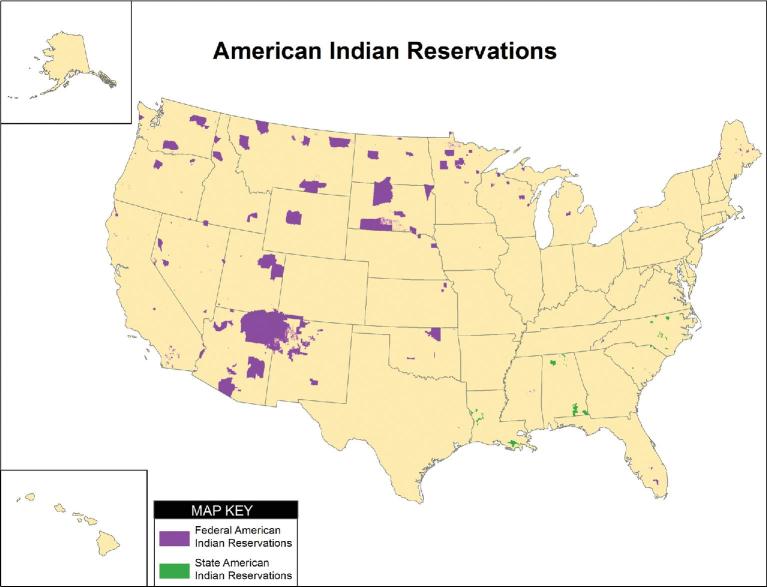
Based on the history of colonization, the Indian Removal Act of 1830 (7), and similar policies, the AI population is located primarily in the western half of the United States (Figure 1). As of the 2010 census, there were ∼5.2 million people in the United States who self-identified as AI, either alone or in combination with other races and ethnicities (8). The AI population suffers from significant health disparities. Rates of death due to unintentional injuries (9), infant mortality (10), and chronic diseases (11) are consistently higher among AIs than the general US population. According to the North Dakota Department of Health, the average age at death between 2010 and 2014 for AIs was 56.8 y compared to 76.6 y for the white population (12). AIs in many regions of the United States live in near third-world health conditions, and a significant national effort is needed to promote collaboration and solve the AI public health crisis. Social adversity, historical events, and poverty in many AI communities have led to exacerbations of health disparities resulting from decreased access to healthy foods and subsequent poor nutrition. Described in the following sections are common risk factors, social determinants of health, and nutritionally related chronic disease disparities among the AI population.
FIGURE 1.
Map of federal- and state-recognized American Indian reservations.
Risk Factors and Social Determinants of Health
Historical trauma
Historically traumatic events have been described as “cataclysmic” events in a population that result in long-standing and intergenerational adverse outcomes. For AIs, the loss of land, traditional food systems, culture, language, traditional ceremonies, and self-sufficiency during the past several centuries has led to a collective sense of loss and social injustice. For example, prior to colonization, the entire continent was inhabited by indigenous peoples. As shown in Figure 1, the amount of tribally controlled territory is minimal. Also, the marginalization of traditional AI culture and language can be measured through the Historical Loss Associated Symptoms Scale and demonstrates a negative emotional response associated with perceived sense of historical loss among AIs (13). Several researchers have examined the effect of historical trauma and its negative impact on AI health (14, 15). Emerging evidence from epigenetic studies demonstrates the possibility that historical trauma may lead to transgenerational stress inheritance (16, 17). This area of inquiry deserves further study.
Boarding school experiences
The boarding school era in the 19th and 20th centuries encompassed multiple generations of children being taken away from their homes, communities, and families and being placed in residential schools that could be >1000 miles away (18). Unfortunately, physical, emotional, and sexual abuse was not uncommon in boarding schools, and the negative consequences include subsequent poor health status (18). In addition, the mortality rate among boarding school residents was high, and many of the schools are adjacent to large cemeteries in which dozens of AI children are buried (19). The survivors of the boarding school experience endured abuse, neglect, and the loss of playmates and friends (20). Traditional parenting and nurturing of children from a cultural perspective was disrupted, resulting in harmful impacts of boarding schools across generations (20). In addition, AI children were removed from healthy traditional food systems and were exposed for the first time to institutional nutrition programs that included simple sugars, refined carbohydrates, and less access to natural foods.
Adverse childhood experiences
The groundbreaking Adverse Childhood Experiences Study (ACE Study) showed the cumulative negative health consequences of adverse experiences in childhood (21). ACEs are classified into 10 domains among the categories of abuse, neglect, and household dysfunction. Adversity in childhood has a negative impact on neurological and social development, and subsequent behavioral challenges are correlated with worse academic, social, and health outcomes. These circumstances ultimately lead to higher prevalence of disease, lower socioeconomic status, and early death (22). The total number of ACEs a person experiences is correlated with poor adult health outcomes, including depression (21, 23), anxiety, posttraumatic stress (24), substance abuse (21, 25), diabetes (21, 25, 26), cancer (27), heart disease (21, 23), and other conditions (21). The original ACE Study included predominantly white participants; however, data from recent studies show that ACEs are more prevalent in many AI communities (28, 29). Although it is not classified as an ACE based on the original study design, food insecurity is an additional adverse childhood experience for many AI and impoverished children. Hence, the intergenerational patterns of poverty and food insecurity in AI populations may be exacerbated by ACEs.
Poverty
Poverty is correlated with poor health status. Nationally, 2.4 times as many AIs as whites live at or below the federal poverty level (30), and in some areas of the Indian Health Service (IHS), including the Great Plains, disparities in poverty are even more pronounced (31). Some of the programs designed to address the nutritional needs of impoverished communities administered by the USDA, including the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and school breakfast and lunch programs, have had a negative impact on nutritional health over time. Significant improvements in breastfeeding promotion have been made to the WIC program in recent years; however, in many AI and other impoverished communities, the population health outcome of WIC has been higher rates of formula feeding and lower rates of breastfeeding (32). It is well established in the scientific literature that children who are breastfed have lower rates of obesity and diabetes compared with children who are formula-fed (33). In addition, nutritional profiles of school breakfast and lunch programs historically have contributed to nutritionally based health disparities with historically higher intake of saturated fat (34).
Obesity
Obesity rates among AIs are higher than those of almost all other racial and ethnic groups (35). Poverty combined with the history of federally sponsored food programs, such as FDPIR operated by the USDA, have led to diets that are high in calories and have poor nutritional value (36). Foods historically available in FDPIR (also known as the commodity food program) consisted of bleached flour, refined sugar, lard, vegetable shortening, sugar-sweetened beverages, pure corn syrup, canned meat, and cheese (36). Loss of access to traditional food systems combined with limited financial opportunities on many AI reservations are key social determinants that place the AI population at higher risk for obesity and its associated chronic disease outcomes.
Commercial tobacco
Significant regional differences exist in the use of commercial tobacco among AIs. In the Northern Plains, tobacco usage is the highest, and not surprisingly, Northern Plains AIs suffer from the highest cancer mortality rates in the nation (37). A potential root cause of this disparity could include the traditional usage of tobacco and other herbs (red willow, etc.) that were smoked for ceremonial purposes and prayer (38). With a cultural connection to smoking, it is possible that AIs in the Northern Plains were more susceptible to cigarette smoking than other populations, and subsequent addiction to nicotine occurred (39). Commercial tobacco usage increased following World War II (40), during which AIs both participated in the military at higher rates than other races and ethnicities (41) and distribution of cigarettes to soldiers was commonplace.
Alcohol
Rates of binge drinking, alcohol misuse, and alcohol mortality have been higher among AIs (42). However, numerous studies also show that AIs have the highest rates of alcohol abstinence, likely due to observations of alcohol's devastating effects among many family and community members (42, 43). The caloric intake from alcohol can also lead to obesity as well as nutritional disparities for some AIs. The AI population has higher prevalence of both binge drinking and alcohol abstinence and relatively lower prevalence of social drinking compared with the non-AI population (42, 44). Perhaps future studies should determine resiliency factors that lead many individuals to abstinence in the face of challenging social circumstances.
Substance abuse
The 2005–2008 National Survey on Drug Use and Health showed a higher prevalence of substance abuse in the AI adolescent population, including marijuana and opiates (45). Addiction to prescription opioids, tranquilizers, stimulants, and sedatives is increasing as well (45). Overdose-associated emergency room visits and hospitalizations are increasing costs, and deaths due to overdose are also on the rise (46). Malnutrition is commonly observed among individuals suffering from drug addiction (47), and recovery programs should include nutritional support in addition to counseling and other support services. Solving this population health challenge and improving outcomes will require expanded collaboration among IHS, tribes, medical systems, public health systems, nutrition programs, and mental health/substance abuse stakeholder groups and providers.
Chronic Disease Disparities
Several nutritionally related chronic diseases occur at disproportionate prevalence among AIs, including diabetes, heart disease, and cancer.
Diabetes
AIs have the highest prevalence of diabetes and the highest diabetes mortality rates in the United States (48). The basis for this disparity is multifaceted in the field of social determinants, with poverty-related lack of access to healthy foods because many AI reservation communities are food deserts, less access to school- or community-based physical activity programs, and possibly genetic predisposition. In terms of population-based nutritional support, federal food programs have not resulted in improved health outcomes, and in many cases, these programs are exacerbating diabetes prevalence in the AI population.
Heart disease
As is the case in many populations, heart disease is the leading cause of death for AIs (9). This is not surprising given the elevated prevalence of obesity and diabetes nationally, unhealthy diets, and high rates of smoking among Plains Indians and Alaska Natives (9). Nationally, AI men and women have a 21% greater mortality rate from heart disease, and AIs in the Northern Plains have a 58% greater heart disease mortality rate, compared with the white population (49).
Cancer
Significant regional disparities in cancer mortality exist in the AI population. Not surprisingly, cancer incidence and mortality rates correlate closely with commercial tobacco use (50). Foods commonly consumed in AI and impoverished populations, including processed meat, red meat, and alcohol, as well as excess abdominal body fat are associated with colorectal cancer risk. Due to underfunding of the IHS and lack of access to appropriate screening, AIs are the only population in the United States with increasing mortality due to colorectal cancer (51). Poverty, lack of insurance, limited IHS resources, and cultural factors are key social determinants that have led to lower rates of colorectal cancer screening and subsequent increases in mortality among AIs (52).
Future Directions and Potential Solutions
Clearly, the AI population health challenges are significant. Improvements in primary, secondary, and tertiary prevention are needed to solve the substantial disparities in health and social determinants. To be most effective, expanded partnerships among tribes, nutritional programs, IHS, public health programs, and medical and academic professionals are needed to identify effective solutions to address the AI public health crisis. Although little can be done to address the distal determinants of health (e.g., colonialism and racism) in terms of changing the past, AI communities have opportunities to positively impact proximal and intermediate determinants of health (health behaviors, food insecurity, health systems, etc.) (53). Moving forward, a multipronged approach in collaboration with numerous stakeholders is needed to address the upstream social determinants of health and to increase access to healthier foods. Of note, specific strategies will vary based on the laws and policies at the national level. The approaches for indigenous populations in the United States will be different from those taken in Canada, Australia, and other nations. Promising practices and strategies for AI populations in the United States can be considered in several focus areas, including 1) improving existing food programs, 2) promoting breastfeeding and early childhood nutrition, 3) promoting food sovereignty and increasing access to traditional foods, 4) expanding locally cultivated foods, and 5) taxing unhealthy foods and subsidizing healthier options.
Improving existing food programs
Many AI communities still depend on and utilize federally sponsored food programs, including FDPIR, school breakfast and lunch programs, and WIC. Although nutritional improvements have been made to these programs in recent decades (e.g., breastfeeding promotion by WIC programs) (54), increases in community engagement, participation, and buy-in are needed to ensure that healthier food offerings are provided and that better food choices are nurtured. Anecdotally, when changes are made to food programs, there can be resistance from the community and reluctance to try new options that might be healthier choices. In these settings, it is important to include a community-engaged approach to develop champions from the community who can advocate for improved nutrition. As of January 2018, 276 tribes were receiving food from FDPIR (55). The Agricultural Act of 2014 included a feasibility study of tribal management of federal nutrition assistance programs instead of state agency administration. Although many tribes are impoverished and have limited infrastructure, resources, and personnel, they generally prefer to manage programs locally (56). Further research is needed to determine the best strategies to enhance locally managed and culturally appropriate food programs. In the authors’ experience, community education regarding healthy cooking and food-tasting opportunities can be effective in promoting consumption of healthier choices. These programs need to be studied and evaluated for their effectiveness, but initial evidence is promising.
Promoting breastfeeding and early childhood nutrition
Breastfeeding is a well-established and natural way to promote health (57). Health experts and stakeholder groups, including the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists, strongly support exclusively breastfeeding (no infant formula, juice, or water) for the first 6 mo of life (58). They also support breastfeeding for a minimum of 1 y with other foods that can be started at 6 mo of age, including vegetables, grains, fruits, and proteins. Many tribes have implemented culturally tailored breastfeeding promotion and early childhood nutrition programs, recognizing the potential long-term impact of good nutrition early in life (59, 60). These programs also need to be studied and evaluated in a culturally relevant manner to demonstrate the health impact, cost analysis, and community member satisfaction. Unfortunately, there is a scarcity of AI-specific research focused on the impact of culturally relevant strategies to promote infant and early childhood nutrition (61).
Promoting food sovereignty and increasing access to traditional foods
Many tribes and tribal colleges have expanded their focus on food sovereignty—defined as “the right of peoples to healthy and culturally-appropriate food produced through ecologically-sound and sustainable methods, and their right to define their own food and agriculture systems” (62). Indigenous populations throughout the world, including AIs, have seen the detrimental impact of colonization on community health and nutrition. Dietary changes, less access to traditional foods, and subsequent poor health outcomes are well described in the health literature. However, the need exists to promote the scientific study of the impact of food sovereignty programs and related social justice initiatives among indigenous peoples. Many AI communities are reclaiming their access to traditional foods, including buffalo in the Northern Plains, “three sisters” crops (corn, beans, and squash), traditional fishing techniques, and other culturally relevant approaches. This area is ripe for expansion of appropriate research and evaluation, and it should include partnerships with tribal colleges and other tribally based stakeholder groups to promote culturally competent approaches.
Expanding locally cultivated foods
Numerous AI communities are developing farmers’ markets and similar food programs to promote access to and utilization of locally cultivated foods. These programs often include traditional foods, but other “nontraditional” foods have also been shown to be well-received in anecdotal reports. Locally cultivated foods can include meats as well as gathered and farmed foods. In the authors’ experience, many AI children have never tasted specific fruits and vegetables, including various berries, persimmon, and numerous types of squash. Tribal farmers’ markets that include tasting opportunities for families and youth have provided successful opportunities to promote healthy food diversity in some families. This is also a potential area for expanded research to examine the health impact of improved access to local foods.
Taxing unhealthy foods and subsidizing healthier options
Some tribes have started a “junk food tax” to limit poor nutritional choices much in the same manner that tobacco taxes can limit cigarette smoking. Preliminary evidence in other populations shows potential reductions in obesity associated with taxing unhealthy foods (63, 64). These programs are novel and relatively new, with taxes implemented since 2015 (65); as a result, there are no peer-reviewed analyses of outcomes to date. The tax programs are also controversial in that some community members are reluctant to change long-standing dietary habits and do not want to pay an additional tax. In addition, some tribes are providing healthier food and drink options in vending machines at a lower cost than the less healthy options. For example, higher protein snacks (nuts, jerky, and cheese) and bottled water can be subsidized and sold in vending machines at a fraction of the cost of unhealthier snacks and sugar-sweetened beverages. Health policy research could include assessing the health impact of making healthier choices easier and less expensive.
As these strategies are being implemented in numerous AI communities, it is vital that new ideas are studied and reported and that existing programs are appropriately evaluated. A challenge in expanding public health programming in AI populations is the dearth of tribally specific evidence-based practices (EBPs). Public health programs are frequently required to use EBPs to acquire grants and other resources. The challenge that we face in AI communities related to EBPs is “Whose evidence is it?” Food programs that work well in cities or suburbs with predominantly non-AI populations may or may not be applicable in rural, tribal populations with significant differences in culture, poverty, food preferences, access, transportation, growing seasons, and numerous other factors that can limit the effectiveness of currently accepted EBPs. The need exists to build the AI-specific evidence base and for tribes to learn from each other regarding the development and implementation of effective nutritional health programs.
Finally, an AI-specific model to frame social determinants of nutritional health in the United States should be developed. This would provide a theoretical framework to understand the impact of the unique history and social factors contributing to nutritionally influenced health inequities among AIs. Based on the growing and evolving understanding of AI nutrition and health disparities, this article provides initial considerations for this model. Strengthening academic partnerships with tribal communities could assist in this process and can promote research and programming to produce more data and EBPs. Tribal–academic partnerships can also result in expanded formal program evaluation and peer-reviewed publications of these programs to ensure that the growing list of EBPs is culturally relevant and includes AI populations.
Acknowledgments
Both authors contributed to the background research and writing of the manuscript.
Notes
The authors reported no funding received for this study.
Author disclosures: DW and SW, no conflicts of interest.
Published in a supplement to Current Developments in Nutrition. This article appears as part of the supplement “Proceedings of the First and Second Annual Conferences on Native American Nutrition,” sponsored by the Shakopee Mdewakanton Sioux Community's Seeds of Native Health campaign through a gift to the University of Minnesota. The guest editors of the supplement, Treena Delormier and Mindy Kurzer, have no conflicts of interest. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors or the publisher, Editor, or Editorial Board of Current Developments in Nutrition.
Abbreviations used: ACE, adverse childhood experience; AI, American Indian; EBP, evidence-based practice; FDPIR, Food Distribution Program on Indian Reservations; IHS, Indian Health Service; WIC, Women, Infants, and Children.
References
- 1. WHO Social determinants of health [Internet]. [cited 2 January, 2019]. Available from: https://www.who.int/social_determinants/sdh_definition/en/. [Google Scholar]
- 2. Brave Heart MYH, DeBruyn LM. The American Indian holocaust: healing historical unresolved grief. Am Indian Alsk Native Ment Health Res 1998;8(2):60–82. [PubMed] [Google Scholar]
- 3. Kuhnlein HV, Receveur O.. Dietary change and traditional food systems of Indigenous peoples. Annu Rev Nutr 16:417–42, 1996. [DOI] [PubMed] [Google Scholar]
- 4. Conti KM. Diabetes prevention in Indian country: developing nutrition models to tell the story of food-system change. J Transcult Nurs 2006;17(3):234–45. [DOI] [PubMed] [Google Scholar]
- 5. USDA Evaluation of the Food Distribution Program on Indian Reservations [Internet]. 2018. Available from: https://www.fns.usda.gov/evaluation-food-distribution-program-indian-reservations-3. [Google Scholar]
- 6. Story M, Strauss KF, Zephier E, Broussard BA. Nutritional concerns in American Indian and Alaska Native children: transitions and future directions. J Am Diet Assoc 1998;98(2):170–6. [DOI] [PubMed] [Google Scholar]
- 7. Cave AA. Abuse of power: Andrew Jackson and the Indian Removal Act of 1830. The Historian 2003;65(6):1330–53. [Google Scholar]
- 8. US Census The American Indian and Alaska Native population: 2010 [Internet]. 2012[cited 2 January, 2019]. Available from: https://www.census.gov/history/pdf/c2010br-10.pdf. [Google Scholar]
- 9. Jacobs-Wingo JL, Espey DK, Groom AV, Phillips LE, Haverkamp DS, Stanley L. Causes and disparities in death rates among urban American Indian and Alaska Native populations, 1999–2009. Am J Public Health 2016;106(5):906–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wong CA, Gachupin FC, Holman RC, MacDorman MF, Cheek JE, Holve S, Singleton RJ. American Indian and Alaska Native infant and pediatric mortality, United States, 1999–2009. Am J Public Health 2014;104(Suppl 3):S320–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bauer UE, Plescia M, Addressing disparities in the health of American Indian and Alaska Native people: the importance of improved public health data. Am J Public Health 2014;104(Suppl 3):S255–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. North Dakota Department of Health Vital records [Internet]. 2014. Available from: http://ndhealth.gov/vital/. [Google Scholar]
- 13. Whitbeck LB, Adams GW, Hoyt DR, Chen X. Conceptualizing and measuring historical trauma among American Indian people. Am J Community Psychol 2004;33(3–4):119–30. [DOI] [PubMed] [Google Scholar]
- 14. Gone JP. A community-based treatment for Native American historical trauma: prospects for evidence-based practice. J Consult Clin Psychol 2009;77(4):751–62. [DOI] [PubMed] [Google Scholar]
- 15. Hartmann WE, Gone JP. American Indian historical trauma: community perspectives from two great plains medicine men. Am J Community Psychol 2014;54:274–88. [DOI] [PubMed] [Google Scholar]
- 16. Crews D, Gillette R, Scarpino SV, Manihham M, Savenkova MI, Skinner MK. Epigenetic transgenerational inheritance of altered stress responses. Proc Natl Acad Sci USA 2012;109(23):9143–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Babenko O, Kovalchuk I, Metz GAS. Stress-induced perinatal and transgenerational epigenetic programming of brain development and mental health. Neurosci Biobehav Rev 2015;48:70–91. [DOI] [PubMed] [Google Scholar]
- 18. Cross SL, Day AG, Byers LG. American Indian grand families: a qualitative study conducted with grandmothers and grandfathers who provide sole care for their grandchildren. J Cross Cult Gerontol 2010;25(4):371–83. [DOI] [PubMed] [Google Scholar]
- 19. Marr CJ. Assimilation through education: Indian boarding schools in the Pacific Northwest [Internet] Seattle (WA): University of Washington Libraries; 2016. Available from: http://content.lib.washington.edu/aipnw/marr.html. [Google Scholar]
- 20. Graves K, Shavings L, Rose C, Saylor A, Smith S, Easley C, Charles GP. Boarding school project: mental health outcome. Anchorage (AK): National Resource Center for American Indian, Alaska Native, and Hawaiian Elders, University of Alaska; 2007. [Google Scholar]
- 21. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998;14(4):245–58. [DOI] [PubMed] [Google Scholar]
- 22. Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the Adverse Childhood Experiences Study. Pediatrics 2003;111(3):564–72. [DOI] [PubMed] [Google Scholar]
- 23. Roh S, Burnette CE, Lee KH, Lee Y, Easton D, Lawler MJ. Risk and protective factors for depressive symptoms among American Indian older adults: adverse childhood experiences and social support. Aging Ment Health 2015;19(4):371–80. [DOI] [PubMed] [Google Scholar]
- 24. McGuinness TM, Waldrop J. Adverse childhood experiences and the mental health of veterans. J Psychosoc Nurs Ment Health Serv 2015;53(6):23–26. [DOI] [PubMed] [Google Scholar]
- 25. Campbell JA, Walker RJ, Egede LE. Associations between adverse childhood experiences, high-risk behaviors, and morbidity in adulthood. Am J Prev Med 2016;50(3):344–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Huffhines L, Noser A, Patton SR. The link between adverse childhood experiences and diabetes. Curr Diab Rep 2016;16(6):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Brown MJ, Thacker LR, Cohen SA. Association between adverse childhood experiences and diagnosis of cancer. PLoS One 2013;8(6):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Warne DK, Dulacki K, Spurlock M, Meath T, Davis M, McConnell J, Adverse childhood experiences among American Indians in South Dakota and associations with mental health conditions, alcohol use, and smoking. J Health Care Poor Underserved 2017;28(4):1559–77. [DOI] [PubMed] [Google Scholar]
- 29. Ravello LD, Abeita J, Brown P. Breaking the cycle/mending the hoop: adverse childhood experiences among incarcerated American Indian/Alaska Native women in New Mexico. Health Care for Women Int 2008;29(3):300–15. [DOI] [PubMed] [Google Scholar]
- 30. Office of Minority Health, US Department of Health and Human Services Profile: American Indian/Alaska Native [Internet] 2018[cited 9 July, 2018]. Available from: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=62. [Google Scholar]
- 31. US Department of the Interior. 2013 American Indian population and labor force report [Internet]. 2014[cited 9 July, 2018]. Available from: https://www.bia.gov/sites/bia.gov/files/assets/public/pdf/idc1-024782.pdf. [Google Scholar]
- 32. Jianga M, Fostera EM, Gibson-Davis CM. The effect of WIC on breastfeeding: a new look at an established relationship. Child Youth Serv Rev 2010;32(2):264–73. [Google Scholar]
- 33. Pettitt DJ, Forman MR, Hanson RL, Knowler WC, Bennett PH. Breastfeeding and incidence of non-insulin-dependent diabetes mellitus in Pima Indians. Lancet 1997;350(9072):166–8. [DOI] [PubMed] [Google Scholar]
- 34. Gordon AR, Devaney BL, Burghardt JA. Dietary effects of the National School Lunch Program and the School Breakfast Program. Am J Clin Nutr 1995;61(1):221S–31S. [DOI] [PubMed] [Google Scholar]
- 35. Office of Minority Health Obesity and American Indians/Alaska Natives [Internet] 2013. Available from: http://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=40. [Google Scholar]
- 36. Shanks CB, Smith T, Ahmed S, Hunts H. Assessing foods offered in the Food Distribution Program on Indian Reservations (FDPIR) using the Healthy Eating Index 2010. Public Health Nutr 2015;19(7):1315–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Brossart L, Moreland-Russell S, Andersen S, Shea A, Walsh H, Schell S, Bach L, Cameron J, Mohr A, Edison L et al.. Health equity in tobacco prevention and control: best practices users guide. Atlanta (GA): Centers for Disease Control and Prevention, US Department of Health and Human Services; 2014. [Google Scholar]
- 38. Margalit R, Wantanabe-Galloway S, Kennedy F, Lacy N, Red Shirt K, Vinson L, Kills Small J. Lakota elders’ views on traditional versus commercial/addictive tobacco use: oral history depicting a fundamental distinction. J Community Health 2013;38:538–45. [DOI] [PubMed] [Google Scholar]
- 39. Kunitz SJ. Historical influences on contemporary tobacco use by Northern Plains and Southwestern American Indians. Am J Public Health 2016;106(2):246–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jacobs M. From the first to the last ash: the history, economics & hazards of tobacco. Unknown binding, 1995. [Google Scholar]
- 41. Veterans Administration American Indian and Alaska Native veterans: 2013 American community survey [Internet] 2015. Available from: https://www.va.gov/vetdata/docs/SpecialReports/AIANReport2015.pdf. [Google Scholar]
- 42. Cunningham JK, Solomon TA, Muramoto ML. Alcohol use among Native Americans compared to whites: examining the veracity of the “Native American elevated alcohol consumption” belief. Drug Alcohol Depend 2016;160:65–75. [DOI] [PubMed] [Google Scholar]
- 43. Bezdek M, Spicer P. Maintaining abstinence in a Northern Plains tribe. Med Anthropol Q 2006;20(2):160–81. [DOI] [PubMed] [Google Scholar]
- 44. Davis MM, Spurlock M, Dulacki K, Meath T, Li HF, McCarty D, Warne DK, Wright B, McConnell KJ, Disparities in alcohol, drug use, and mental health condition prevalence and access to care in rural, isolated, and reservation areas: findings from the South Dakota Health Survey. J Rural Health 2016;32(3):287–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wu L, Woody GE, Yang C, Pan J, Blazer DG. Racial/ethnic variations in substance-related disorders among adolescents in the United States. Arch Gen Psychiatry 2011;68(11):1176–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Herzig SJ, Rothberg MB, Cheung M, Ngo LH, Marcantonio ER. Opioid utilization and opioid-related adverse events in nonsurgical patients in US hospitals. J Hosp Med 2014;9(2):73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Nazrul Islam SK, Hossain KJ, Ahmed A, Ahsan M. Nutritional status of drug addicts undergoing detoxification: prevalence of malnutrition and influence of illicit drugs and lifestyle. Br J Nutr 2002;88(5): 507–13. [DOI] [PubMed] [Google Scholar]
- 48. Cho P, Geiss LS, Rios Burrows N, Roberts DL, Bullock AK, Toedt ME. Diabetes-related mortality among American Indians and Alaska Natives, 1990–2009. Am J Public Health 2014;104(Suppl 3):S496–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Veazie M, Ayala C, Schieb L, Dai J, Henderson JA. Trends and disparities in heart disease mortality among American Indians/Alaska Natives, 1990–2009. Am J Public Health 2014;104(S3):359–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wiggins CL, Espey DK, Wingo PA, Kaur JS, Taylor Wilson R, Swan J, Miller BA, Jim MA, Kelly JJ, Lanier AP. Cancer among American Indians and Alaska Natives in the United States, 1999–2004. Cancer 2008;113(5 Suppl):1142–52. [DOI] [PubMed] [Google Scholar]
- 51. Perdue DG, Haverkamp D, Perkins C, Makosky Daley C, Provost E. Geographic variation in colorectal cancer incidence and mortality, age of onset, and stage at diagnosis among American Indian and Alaska Native people, 1990–2009. Am J Public Health 2014;104(S3):S404–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Maly AG, Steel TL, Lieberman DA, Becker TM. Colorectal cancer screening among American Indians in a Pacific Northwest tribe: Cowlitz Tribal BRFSS Project, 2009–2010. Public Health Rep 2014;129(3):280–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Reading C, Wien F. Health inequalities and the social determinants of aboriginal peoples’ health. Prince George (Vancouver, Canada): National Collaborating Centre for Aboriginal Health; [Internet] 2009. Available from: http://lfs-ubcfarm.sites.olt.ubc.ca/files/2018/02/Reading-C.L.-Wien-F.-2009.pdf. [Google Scholar]
- 54. Khoury AJ, Hinton A, Mitra AK, Carothers C, Foretich C. Improving breastfeeding knowledge, attitudes, and practices of WIC clinic staff. Public Health Rep 2002;117(5):453–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. USDA Food distribution programs on Indian reservations [Internet] Washington (DC): USDA; 2018[cited 3 January, 2019]. Available from: https://fns-prod.azureedge.net/sites/default/files/fdpir/pfs-fdpir.pdf. [Google Scholar]
- 56. USDA Feasibility of tribal administration of federal nutrition assistance programs [Internet]. Washington (DC): USDA; 2018[cited 3 January, 2019]. Available from: https://www.fns.usda.gov/feasibility-tribal-administration-federal-nutrition-assistance-programs. [Google Scholar]
- 57. Victora CG, Bahl R, Barros AJD, Franca GVA, Horton S, Krasevec J, Murch S, Sankar MJ, Walker N, Rollins NC. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet North Am Ed 2016;387(10017):475–90. [DOI] [PubMed] [Google Scholar]
- 58. American Academy of Pediatrics Itasca (IL): American Academy of Pediatrics; [Internet]. [cited 3 January, 2019]. Available from: https://pediatrics.aappublications.org/content/129/3/e827. [Google Scholar]
- 59. Wilhelm S, Rodehorst-Weber K, Aguirre T, Stepans MB, Hertzog M, Clarke M, Herboldsheimer A. Lessons learned conducting breastfeeding intervention research in two Northern Plains tribal communities. Breastfeed Med 2012;7(3):167–72. [DOI] [PubMed] [Google Scholar]
- 60. Rhodes KL, Hellerstedt WL, Davey CS, Pirie PL, Daly KA. American Indian breastfeeding attitudes and practices in Minnesota. Matern Child Health J 2008;12(Suppl 1):46. [DOI] [PubMed] [Google Scholar]
- 61. Spieler L. American Indians and Alaska Natives: breastfeeding disparities and resources. Breastfeed Med 2010;5(5):219–20. [DOI] [PubMed] [Google Scholar]
- 62. US Food Sovereignty Alliance Food sovereignty [Internet]. [cited 10 July, 2018]. Available from: http://usfoodsovereigntyalliance.org/what-is-food-sovereignty/. [Google Scholar]
- 63. Sacks G, Veerman JL, Moodie M, Swinburn B “Traffic-light” nutrition labelling and “junk-food” tax: a modelled comparison of cost-effectiveness for obesity prevention. Int J Obes 2011;35:1001–9. [DOI] [PubMed] [Google Scholar]
- 64. Mytton OT, Clarke D, Rayner M. Taxing unhealthy food and drinks to improve health. BMJ 2012;344:e2931. [DOI] [PubMed] [Google Scholar]
- 65. Time This place just became the first part of the U.S. to impose a tax on junk food [Internet]. 2015[cited 4 January, 2018. Available from: http://time.com/3762922/junk-food-tax-obesity-navajo-nation/. [Google Scholar]