Abstract
Acute abdominal pain is a common symptom in young women. We describe a patient with acute illness and severe lower abdominal pain. Laboratory tests were normal except for mildly deranged inflammatory markers. No abnormalities were reported on abdominal ultrasonography and MRI, whereas diagnostic laparoscopy revealed a tumour located dorsally from the uterus. We resected the tumour and pathology results showed a well-differentiated papillary mesothelioma of the peritoneum (WDPMP). Microscopy showed evidence of acute ischaemia in the resected lesion, which was likely the cause of the acute abdominal pain. WDPMP is a rare disease that arises from the serous membranes which does not seem to have a relation to asbestos exposure. Generally, WDPMP has a mild clinical course and good long-term prognosis.
Keywords: surgery, gastrointestinal surgery, pathology
Background
Acute abdominal pain is a common symptom in young women presenting to emergency rooms. The presentation of symptoms generally directs towards the underlying problem; patients with severe pain generally suffer from ischaemia (eg, ovarian torsion or incarcerated hernia) or obstruction (eg, choledochocystolithiasis or urolithiasis). Patients with nausea, vomiting, shivering and fever generally suffer from infectious disease. However, patients often present with undifferentiating abdominal signs and symptoms which require a range of investigation and often surgical intervention. We describe a patient with mildly deranged inflammatory markers and severe lower abdominal pain due to a well-differentiated papillary mesothelioma of the peritoneum (WDPMP). WDPMP is a rare disease with fewer than hundred reported cases in literature. The tumour has been described to originate from the serous membranes in the pleura, tunica vaginalis, peritoneum or pericardium and it usually shows a benign course.1–4
Case presentation
A 25-year-old otherwise healthy woman was referred to our emergency department with severe lower abdominal pain. Her pain had been present for 24 hours and was located in the right lower quadrant. There were no gastro-intestinal, urinary, pulmonary and neurological complaints. She was not sexually active and had a regular 28-day menstrual cycle without metrorrhagia. Her family history was negative for inflammatory bowel disease and gynaecological disease and she had no history of asbestos exposure.
Investigations
Physical examination demonstrated a subfebrile body temperature (37.9°C), mild tachycardia (105 beats/min) and low-normal blood pressure (95/60 mm Hg). Examination of the heart and lungs revealed no abnormalities, abdominal examination showed normal bowel sounds, no tenderness to percussion and palpation revealed severe tenderness on deep palpation in the right lower quadrant. No palpable masses or signs of peritonitis were found. Laboratory tests showed an isolated elevated C reactive protein (CRP, 21 mg/L), negative beta human chorionic gonadotropin and no signs of urinary tract infection. A gynaecology consultation was sought and ovarian torsion and pelvic inflammatory disease were thought to be unlikely. Abdominal ultrasonography showed a trace of free intra-abdominal fluid, mild distension of the ileum and jejunum and no signs of appendicitis. Since the patient was not yet sexually active no transvaginal ultrasonography was undertaken. Re-evaluation after 1 day showed similar complaints and an increased CRP (45 mg/L). MRI of the lower abdomen showed a normal sized non-inflamed appendix and only a trace of free intra-abdominal fluid around the caecum. As there were no signs of sepsis, she was admitted for observation and pain control. The next day, pain and CRP (60 mg/L) increased and a diagnostic laparoscopy was performed.
Differential diagnosis
Acute appendicitis.
Ovarian torsion.
Pelvic inflammatory disease.
Inflammatory bowel disease.
Endometriosis.
Meckel’s diverticulitis.
Intra-abdominal tumour.
Treatment
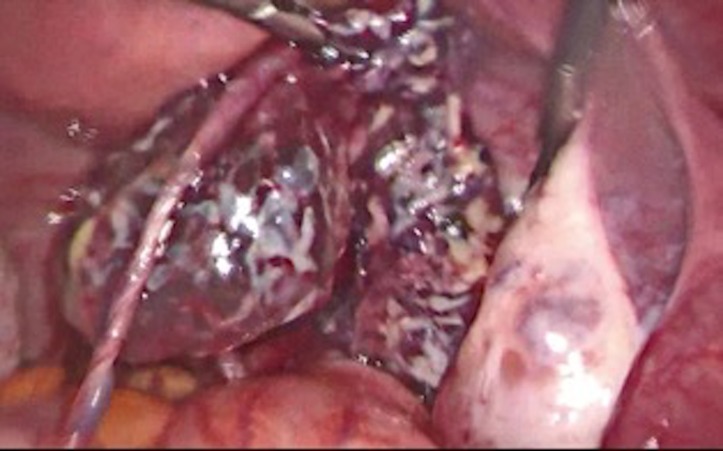
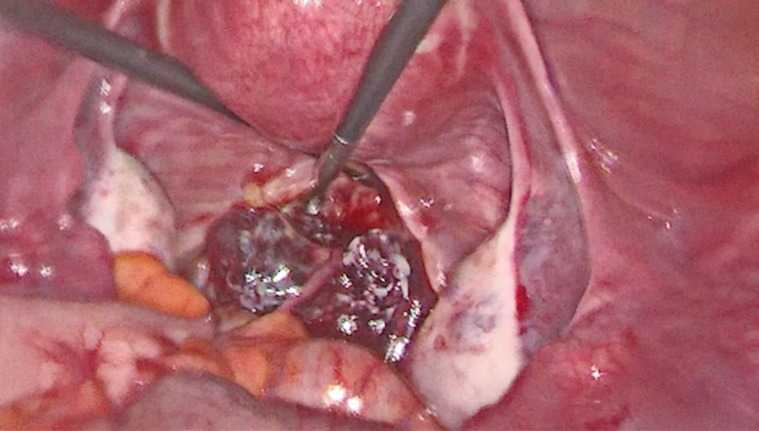
Diagnostic laparoscopy showed a lobulated purple/white coloured tumour in the pouch of Douglas. The tumour was connected to the peritoneum of the greater omentum by a cord (figures 1 and 2). The tumour and the cord were resected en-bloc and sent to the pathologist. After surgery, the pain resolved and the patient was discharged on the first postoperative day. Her recovery was uneventful.
Figure 1.
Laparoscopy view into the pelvic cavity. The round structure at the top is the uterus; the white structures to the left and right are the ovaries. The purple/white coloured tumour is visible dorsally from the uterus.
Figure 2.
Laparoscopy view of the tumour with clear vision of the cord to the peritoneum. On the right, a normal, uninvolved right ovary.
Outcome and follow-up
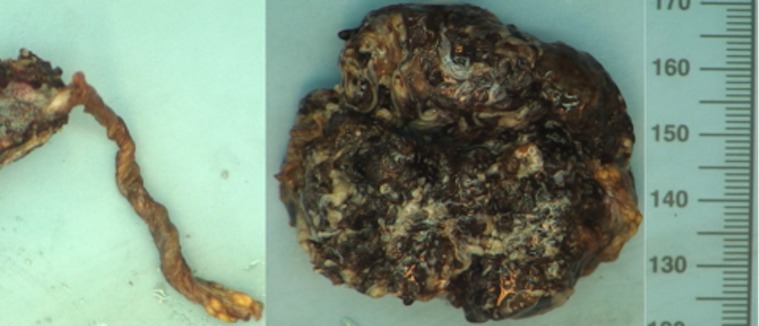
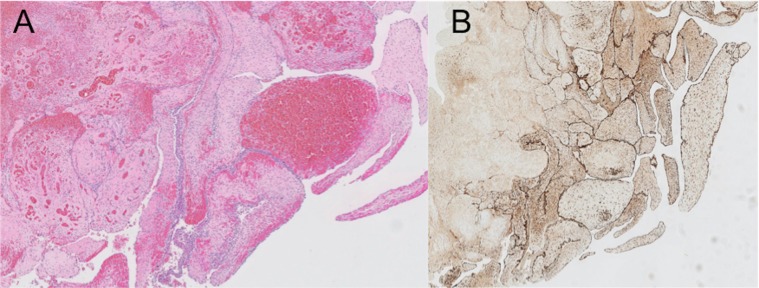
Pathology results showed a 5 by 1.8 cm haemorrhagic and irregular tissue fragment with a 5 cm long cord-like structure (figure 3). Histologic examination showed well-vascularised stroma with extensive haemorrhage. In addition, there were many papillary stromal fragments lined by partly epithelioid and partly flattened cells. Focally, there were multinucleated cells lining these papillary stromal fragments. Morphologically, it was reminiscent of placental villi. However, additional p63 staining did not show any villous trophoblasts. Furthermore, the lining cells were strongly positive for both keratin and calretinin, fitting mesothelial cells. The cord-like structure consisted of multiple dilated blood vessels. The differential diagnosis was a reactive mesothelial proliferation or a WDPMP. After additional external consultation, the prominent papillary architecture was thought to be best befitting a WDPMP (figure 4).
Figure 3.
Image of the resected surgical specimen as received by the pathologist.
Figure 4.
Histopathology of the WDPMP. In panel (A) an H&E staining and in panel (B) the calretinin staining (magnification 20×). WDPMP, well-differentiated papillary mesothelioma of the peritoneum.
Discussion
WDPMP is usually found in young women and generally has a mild clinical course and a good long-term prognosis. Often WDPMP is an incidental finding at laparotomy or laparoscopy. In our patient, the tumour was located dorsally from the uterus and might have been identified by transvaginal ultrasound. However, because she was not sexually active no transvaginal ultrasound was performed. In hindsight, the radiologist was able to locate the tumour on the MRI. The lesion was mostly likely missed on initial examination due to a low signal on the T2-weighted image and no diffusion restriction on the diffusion-weighted image (figure 5).
Figure 5.

MRI images. (A) T2-weighted image with low signal uptake (tumour in circle). (B) Diffusion-weighted image without diffusion restriction in the tumour (circle).
A minority of patients with WDPMP present with symptoms such as abdominal pain, ascites, bloating, weight loss, menorrhagia or dyspareunia.2 4 5 Based on the extensive haemorrhage found microscopically, we hypothesise that the severe abdominal pain in our patient was caused by torsion of the cord from the tumour to the peritoneum. This torsion could have compromised the blood supply of the tumour causing pain from venous stasis and/or ischaemia by arterial insufficiency. No standardised treatment for WDPMP has been established, although complete surgical resection is performed in most patients.2 4 6 There seems to be no clear relation to asbestos exposure, as possible exposure only has been described in three patients in one case series.4 In contrast to WDPMP, malignant peritoneal mesothelioma has a poor prognosis, mostly found in 50–60-years-old men, and is clearly associated with asbestos exposure.7 8
Learning points.
Severe abdominal pain in young women has a broad differential diagnosis and may need extensive investigation.
Well-differentiated papillary mesothelioma is a very rare disease that arises from serous membranes.
Diagnostic laparoscopy can be useful in symptomatic patients with (seemingly) normal radiology results.
Footnotes
Contributors: All authors were involved in the treatment of the patient. JEB and KMvdL drafted the manuscript, which is critically revised by SW and MMP. All authors approved the final version of the manuscript for submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Bazine A, Fetohi M, Namad T, et al. A Case of Well-differentiated papillary mesothelioma of the male peritoneum: successful treatment by systemic chemotherapy. Cureus 2017;9:e1104 10.7759/cureus.1104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nasit JG, Dhruva G. Well-differentiated papillary mesothelioma of the peritoneum. Am J Clin Pathol 2014;142:233–42. 10.1309/AJCPOTO9LBB4UKWC [DOI] [PubMed] [Google Scholar]
- 3. Malpica A, Sant’Ambrogio S, Deavers MT, et al. Well-differentiated papillary mesothelioma of the female peritoneum: a clinicopathologic study of 26 cases. Am J Surg Pathol 2012;36:117–27. 10.1097/PAS.0b013e3182354a79 [DOI] [PubMed] [Google Scholar]
- 4. Daya D, McCaughey E. Well-differentiated papillary mesothelioma of the peritoneum. Cancer 1990;65:292–6. [DOI] [PubMed] [Google Scholar]
- 5. Saha A, Mandal PK, Manna A, et al. Well differentiated papillary mesothelioma of abdomen—a rare case with diagnostic dilemma. J Lab Physicians 2018;10:248–50. 10.4103/JLP.JLP_167_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lee YK, Jun HJ, Nahm JH, et al. Therapeutic strategies for well-differentiated papillary mesothelioma of the peritoneum. Jpn J Clin Oncol 2013;43:996–1003. 10.1093/jjco/hyt117 [DOI] [PubMed] [Google Scholar]
- 7. Hoekman K, Tognon G, Risse EK, et al. Well-differentiated papillary mesothelioma of the peritoneum: a separate entity. Eur J Cancer 1996;32A:255–8. 10.1016/0959-8049(95)00574-9 [DOI] [PubMed] [Google Scholar]
- 8. Clarke JM, Helft P. Long-term survival of a woman with well differentiated papillary mesothelioma of the peritoneum: a case report and review of the literature. J Med Case Rep 2010;4:346 10.1186/1752-1947-4-346 [DOI] [PMC free article] [PubMed] [Google Scholar]