Abstract
In postcollapse hip avascular necrosis (AVN), the femoral head cannot be salvaged, necessitating total hip replacement. We report a case of a 39-year-old woman who developed idiopathic femoral head AVN with marked symptoms and radiological evidence of articular surface collapse. We treated her with core decompression combined with the ‘diamond concept’ (implantation of bone marrow concentrate, a growth factor and bone graft substitute) and distracted the hip joint with external fixator. Four years postoperatively the articular surface has been restored and the patient reports excellent quality of life. Hip arthrodiastasis with core decompression and ‘diamond concept’ regeneration could be considered a treatment option in advanced AVN of the femoral head.
Keywords: orthopaedics, orthopaedic and trauma surgery
Background
Osteonecrosis or avascular necrosis (AVN) of the femoral head most commonly affects adults in their third or fourth decade, with 10 000–20 000 new cases being diagnosed annually in the USA.1 Core decompression of the femoral subchondral area is the most common procedure to treat early stages of femoral head osteonecrosis.2 Its success rate in non-collapsed heads has been reported in the region of 80%, decreasing significantly to 27% with articular collapse.3 If femoral head collapse occurs, total hip replacement (THR) presents as the only treatment of choice.4 Recently, it was shown that autologous bone marrow aspirate (BMA) concentrate application (autologous cell therapy) combined with core decompression is superior to core decompression alone, as it markedly decelerates progression to the collapsed stage, limits the need for THR and improves functional outcomes.5 Core decompression combined with regenerative therapies was presented last year with a cumulative survivorship of 80% in 10 years and better results compared with core decompression alone (89.9%–70.6%).6 However, it still remains unclear which element of regenerative therapy is better or whether a combinatory approach, the so-called ‘diamond concept’ for bone regeneration (simultaneous implantation of a scaffold, osteoprogenitor cells and a growth factor (optimum biological stimulation)), should be used in particular for difficult advanced cases of AVN.7 We present the case of a young woman suffering from advanced left femoral head AVN at Steinberg stage IV,8 which was successfully managed with core decompression, ‘diamond concept’ and hip distraction.
Case presentation
A 39-year-old healthy Caucasian woman was referred to our centre with a 2-year history of left groin and knee pain after the end of her pregnancy. The pain has aggravated in the last 6 months, resulting in constant limp and inability to perform her everyday activities. The initial diagnosis was postpartum musculoskeletal pain, until she was referred to an orthopaedic surgeon who diagnosed her with severe postcollapse left hip AVN at Steinberg stage IV.8 THR was recommended as the only treatment option. Radiographs showed femoral head articular surface collapse superiorly (figure 1). MRI confirmed the findings, showing in T1-weighted sequence subarticular AVN with loss of the normal fat signal and flattening of the articular surface (figure 2). The patient never smoke or took steroids and denied any medical comorbidities. Biochemical screening for coagulopathy, antiphospholipid syndrome and inflammatory arthropathy was negative. Examination revealed equal leg lengths and severely irritable left hip with painful flexion limited to 40°. The patient reported her quality of life using the EuroQol 5D-5L9 generic health instrument as 43443 in the descriptive scoring system, with severe problems in walking and in usual activities, moderate problems in self-care, severe pain and moderate anxiety, and a 10/100 Visual Analogue Scale (VAS) score.
Figure 1.
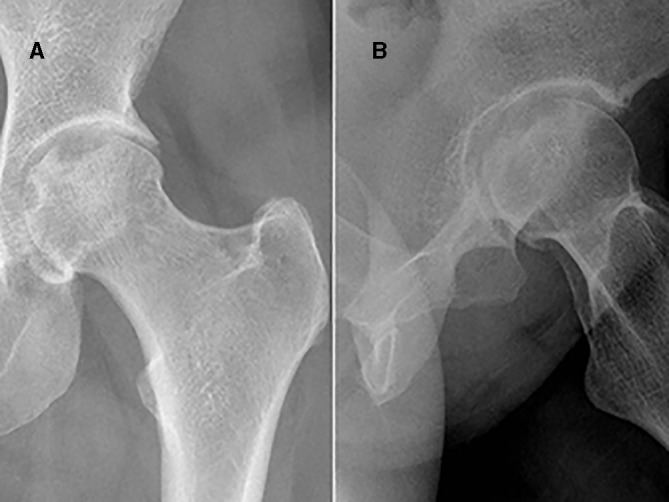
Preoperative radiographs showing the collapsed femoral head. (A) Anteroposterior view and (B) lateral view.
Figure 2.
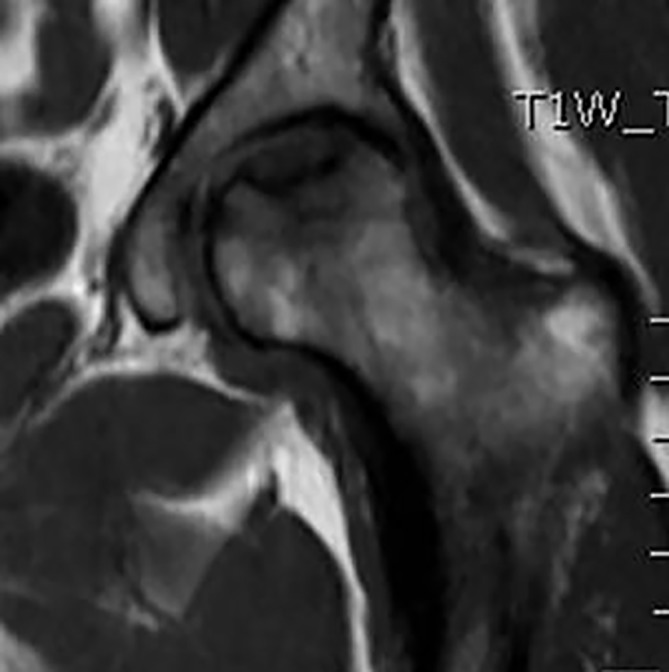
Preoperative T1-weighted MRI sequence. Subarticular avascular necrosis with loss of the normal fat signal and flattening of the articular surface.
Due to her young age, the patient declined THR and was referred to our clinic for a second opinion. She consented to the suggested salvage treatment being core decompression, ‘diamond concept’ (for optimum biological stimulation of the affected area) and hip arthrodiastasis.
In supine position and on radiolucent traction table, we proceeded to standard hip core decompression with initially 8 mm and subsequently 12 mm diameter reversed reamers (figure 3A). From her right iliac crest, 60 mL of BMA was harvested and centrifuged to create a concentrated osteoprogenitor cell volume of 8 mL. This BMA was loaded along with a growth factor (bone morphogenetic protein 7) onto a scaffold (10 cc of Vitoss BA Foam; Orthovita, Malvern, USA), which is a bioactive bone graft substitute foam strip consisting of β-tricalcium phosphate, type I bovine collagen and bioactive glass. Following targeted core decompression of the necrotic lesion, the loaded scaffold was delivered and implanted in the necrotic area through the prepared tunnel (figure 3B). The entry point of the tunnel was sealed with Tutobone (Tutogen, Neunkirchen am Brand, Germany), which is a xenograft-bovine trabecular bone, to create the so-called ‘biological chamber’ for bone-guided regeneration. At the same theatre setting, the hip was distracted up to 5 mm and held in that position with a non-articulated Hoffmann III External Fixator (Stryker) using two 5 mm Schanz screws in the ilium and two 6 mm Schanz screws in the femoral shaft. The optimal pin position and adequate hip distraction were fluoroscopically checked (figure 3C,D).
Figure 3.
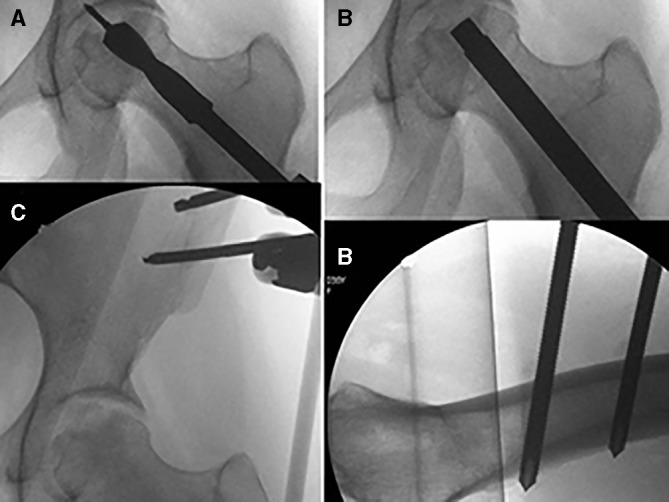
Perioperative image intensifier views. (A) Core decompression, (B) delivery of biological factors, (C) external fixator in the ilium and hip distraction, and (D) pins in the femur.
The postoperative period was uneventful. The patient remained non-weightbearing during all the distraction period, and the fixator was removed at 4-week clinic follow-up. She continued non-weightbearing for the next 8 weeks, and at 12 weeks commenced partial weightbearing. Transition to full weightbearing started at 5 months with the aid of crutches, and at 9 months she was fully weightbearing without any limitation. Due to the degree of collapse, this rehabilitation protocol was prescribed to allow sufficient time of integration and mineralisation of the implanted graft material.
Outcome and follow-up
At 1-year follow-up the patient was pain-free and the radiographs demonstrated evidence of regeneration. Recently, at 4-year follow-up, she presented with a full and painless gait pattern, and is able to walk long distances and to perform all everyday activities as she was able prior to the presentation of AVN. She scored her health as 100/100 on the EQ-5D-5L VAS, with the descriptive domain score being 11111.
The radiographs confirmed preservation of the hip joint with regeneration of the previous avascular area (figure 4). T1-weighted MRI sequence showed restoration of the normal bone fat signal within the previous area of AVN (figure 5A), whereas T2-weighted fat-suppressed sequence showed that the defect in the articular surface had been restored (figure 5B).
Figure 4.
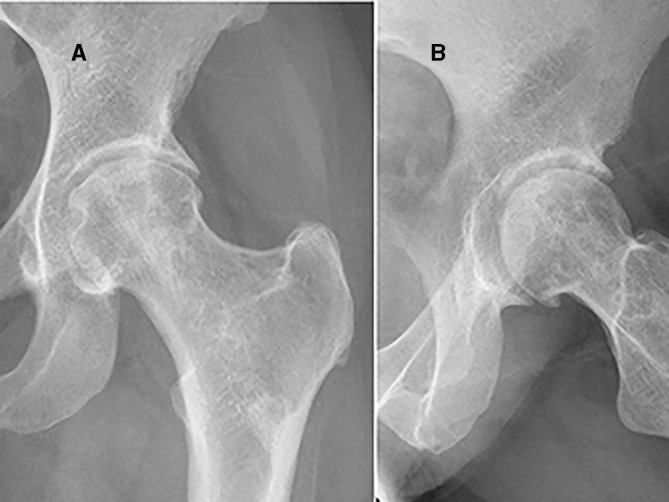
X-rays at 4-year follow-up. The lesion has been regenerated and femoral head sphericity regained. Hip joint space has been preserved. (A) Anteroposterior view and (B) lateral view.
Figure 5.
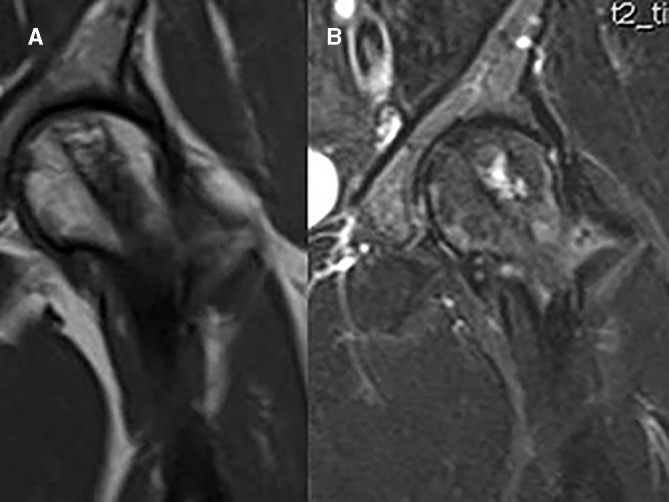
(A) T1-weighted MRI sequence 4 years postoperatively. Restoration of the normal bone fat signal within the previous area of avascular necrosis. (B) T2-weighted fat-suppressed image illustrating that the defect in the articular surface has been restored.
The clinical and radiological outcome of this treatment modality is considered excellent as it preserved the patient’s hip joint and offered her return to her previous functionality.
Discussion
In the present case, core decompression combined with an optimum biological stimulation according to the ‘diamond concept’ for bone repair (implantation of osteoprogenitor cells, growth factor and osteoconductive scaffold), along with a version of mechanical stability that hip distraction offers, contributed to a successful salvage result. The beneficial effect of the diamond concept has been previously reported in such situations as fracture non-unions and bone defects.10 The application of hip distraction was felt to be appropriate as a period of stability and protection from loading of the affected femoral head area would have supported the integration of the graft material within the zone of previous necrosis.
Noteworthy, hip joint arthrodiastasis (hip distraction) was first described in 1979 by Aldegheri et al in Verona.11 In their monumental publication, they described hip arthrodiastasis as a regimen providing distraction of hip joint space and offloading of muscle and body forces by means of external fixator crossing the hip.12 Hinged external fixator was applied bridging the femur and the ilium with the hinge at the level of hip centre of rotation. Duration of distraction varied between 6 and 10 weeks depending on the patient’s tolerance. They advised that 5 mm radiographic separation should be the perceived target. The authors treated 19 patients with idiopathic AVN, with 4 at stage II (Ficat and Arlet classification), 1 at stage III and the remaining 14 at stage IV. Successful result at 5-year follow-up was found only in 5 out of 14 of stage IV (36%). None of the five patients at stage IV who received perforations had a successful result. However, it is not clear whether perforation was performed like modern core decompression. Since 1994 no other paper on arthrodiastasis and its applications in hip avascular phenomena in adults has been published. Nonetheless, papers reporting hip distraction in treating Legg-Calvé-Perthes (LCP) disease in children and adolescents have been published.13–15 Hip distraction is considered a salvage procedure in severe cases with late onset, where all other traditional methods offer poor outcomes. With arthrodiastasis, patients seem to have accelerated healing from necrosis to remodelling stage bypassing the fragmentation, resulting also in joint space increase and preventing further epiphysial collapse. We can postulate that adult osteonecrosis shares some pathophysiological elements with LCP disease, which could explain the success of our technique. Most of the studies on Perthes used articulating hip distraction (the hinge at the level of hip centre of rotation) as joint movement was thought to prevent adhesions and promote cartilage healing.16 Others thought that movement would cause pain, and as the literature was inconclusive non-articulating hip distraction was preferred.13 We did not use articulating device as the limited time of application (4 weeks) was not considered to provoke stiffness (most of paediatric cases were distracted for more than 2–3 months).
Interestingly, there are no experimental studies on hip distraction and osteonecrosis. Knee distraction has been investigated for osteoarthritis (OA). We can assume that some similar biological changes take place in the hip; however, the biomechanics in these two joints and also the pathophysiology between OA and osteonecrosis differ. Anterior cruciate ligament transection model and knee distraction were applied in dogs.17 Synovial tissue inflammation in joint distraction group was significantly lower than in the OA control group and not statistically different from the contralateral healthy joint. Knee diastasis with anterior cruciate ligament plus medial meniscus transection model of OA was applied in rats.18 Macroscopic examination in the distraction group revealed smoother cartilage and less osteophytes. Subchondral bone investigation with micro-CT showed reduced abnormal bone remodelling in the distraction group. We can postulate that hip arthrodiastasis similarly offers a favourable biological environment for regeneration.
The hypothesis that hip arthrodiastasis combined with osteochondral allograft plus bone marrow-derived mesenchymal stem cells may promote creeping substitution in postcollapse femoral head osteonecrosis was first published in 2014.19 The authors suggested that by combining the osteoconductive properties of bone allograft with the osteogenic factors of the bone marrow, it may well be an alternative to autologous graft. According to their hypothesis, hip distraction may create the space and minimise mechanical stress, promoting the incorporation and healing of the allograft, which was augmented with stem cells, thus restoring a congruent joint. This has been only a hypothesis, but it appears from our case to have a concrete basis.
To our knowledge this is the first case where a hip suffering from osteonecrosis at postcollapse stage was successfully treated and the femoral head was regenerated with the combination of arthrodiastasis, core decompression and regeneration according to the ‘diamond concept’, resulting in femoral head preservation. This treatment modality should be considered in the surgeon’s armamentarium when cases like the one described here are considered for hip preservation and not for joint replacement surgery.
Patient’s perspective.
Three months after the delivery of my girl I developed pain in my left hip which initially was occasional but started to become more intense. I could not remember having traumatized it and I had to put up with it in order to care for my children at that sensitive period. I was taking simple analgesia with paracetamol and ibuprofen over the counter. After one year the pain started to be worse and after 18 months or so I was suffering. I had pain when I was putting weight on it and had to use crutches, my mobility and hip movements were limited and I also developed left knee pain. My sleeping pattern was disturbed and simple movements on my hip were causing pain. I visited my GP many times and attended physio and the diagnosis I was getting initially was post-partum muscle pain. As my symptoms were aggravated I was referred to an orthopedic surgeon who diagnosed me with advanced femoral head avascular necrosis and offered me a hip replacement. This was a shock to me as I found myself very young to replace my hip joint and investigating my options I asked whether there is an option of regenerative technique. I was advised of the slim possibilities of preserving my femoral head and was referred to Leeds tertiary referral centre. After clinical examination the orthopedic surgeon advised that core decompression with bone regenerative techniques may solve the problem but as the femoral head is already collapsed we will have to protect the regeneration with a form of mechanical stability and hope that this will work. He advised me that every procedure has complications and in fact this may not work but I decided to try. After the operation an external device was applied for one month and my symptoms got significantly better from 9th month. In one year I was able to walk but with limitation in high impact activities. My movements got better and the following years I gradually got back to where I was before the onset of the problem. Today year at 4 years after the operation I feel that I have got my life back!! I can go for long walks, I do not have any pain and I am active like before. I am grateful for the care I received and I would recommend this treatment to patients having the same problem.
Learning points.
Salvage of postcollapse femoral head avascular necrosis remains a difficult clinical problem, with total hip replacement usually offered as a standard treatment option.
The biological component of the ‘diamond concept’ offers a powerful osteogenic response facilitating bone repair.
Hip joint distraction (arthrodiastasis) is performed with an external fixator bridging the femur and the ilium, and can be either articulating or non-articulating with the hinge at the hip centre of rotation.
Hip arthrodiastasis offers a favourable mechanical environment offloading the hip joint, neutralising the forces and allowing the regeneration process to evolve.
Hip arthrodiastasis combined with core decompression and with the principles of ‘diamond concept’ can regenerate and restore a collapsed osteonecrotic femoral head.
Footnotes
Contributors: IVP: conduct of study, acquisition, analysis and interpretation of data, literature search, draft, correcting and revising the draft for important intellectual content, approved the version published, and agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. JR: acquisition, analysis and interpretation of data, planning, correcting and revising the draft for important intellectual content, approved the version published, and agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. PVG: planning, conception, design, conduct, supervision of the initial draft, correcting and revising the draft for important intellectual content, approved the version published, and agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Talathi NS, Kamath AF. Autologous stem cell implantation with core decompression for avascular necrosis of the femoral head. J Clin Orthop Trauma 2018;9:349–52. 10.1016/j.jcot.2018.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br 1985;67:3–9. [DOI] [PubMed] [Google Scholar]
- 3. Fairbank AC, Bhatia D, Jinnah RH, et al. . Long-term results of core decompression for ischaemic necrosis of the femoral head. J Bone Joint Surg Br 1995;77:42–9. 10.1302/0301-620X.77B1.7822394 [DOI] [PubMed] [Google Scholar]
- 4. Lieberman JR, Berry DJ, Mont MA, et al. . Osteonecrosis of the hip: management in the 21st century. Instr Course Lect 2003;52:337–55. [PubMed] [Google Scholar]
- 5. Papakostidis C, Tosounidis TH, Jones E, et al. . The role of “cell therapy” in osteonecrosis of the femoral head. Acta Orthop 2016;87:72–8. 10.3109/17453674.2015.1077418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Andriolo L, Merli G, Tobar C, et al. . Regenerative therapies increase survivorship of avascular necrosis of the femoral head: a systematic review and meta-analysis. Int Orthop 2018;42:1689–704. 10.1007/s00264-018-3787-0 [DOI] [PubMed] [Google Scholar]
- 7. Giannoudis PV, Einhorn TA, Marsh D. Fracture healing: the diamond concept. Injury 2007;38(Suppl 4):S3–S6. 10.1016/S0020-1383(08)70003-2 [DOI] [PubMed] [Google Scholar]
- 8. Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg Br 1995;77:34–41. 10.1302/0301-620X.77B1.7822393 [DOI] [PubMed] [Google Scholar]
- 9. Herdman M, Gudex C, Lloyd A, et al. . Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Andrzejowski P, Giannoudis PV. The ’diamond concept' for long bone non-union management. J Orthop Traumatol 2019;20:21 10.1186/s10195-019-0528-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Aldegheri R. Arthrodiatasis of the hip [in Italian]. Ortopedia e Traumatologia Oggi 1981;1:103–9. [Google Scholar]
- 12. Aldegheri R, Trivella G, Saleh M. Articulated distraction of the hip. Conservative surgery for arthritis in young patients. Clin Orthop Relat Res 1994;301:94–101. 10.1097/00003086-199404000-00016 [DOI] [PubMed] [Google Scholar]
- 13. Hosny GA, El-Deeb K, Fadel M, et al. . Arthrodiastasis of the hip. J Pediatr Orthop 2011;31(2 Suppl):S229–34. 10.1097/BPO.0b013e318223b45a [DOI] [PubMed] [Google Scholar]
- 14. Laklouk MA, Hosny GA. Hinged distraction of the hip joint in the treatment of Perthes disease: evaluation at skeletal maturity. J Pediatr Orthop B 2012;21:386–93. 10.1097/BPB.0b013e328354b0ab [DOI] [PubMed] [Google Scholar]
- 15. Kim SS, Lee CW, Kim HJ, et al. . Treatment of late-onset legg-calve-perthes disease by arthrodiastasis. Clin Orthop Surg 2016;8:452–7. 10.4055/cios.2016.8.4.452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Salter RB, Simmonds DF, Malcolm BW, et al. . The biological effect of continuous passive motion on the healing of full-thickness defects in articular cartilage. An experimental investigation in the rabbit. J Bone Joint Surg Am 1980;62:1232–51. 10.2106/00004623-198062080-00002 [DOI] [PubMed] [Google Scholar]
- 17. van Valburg AA, van Roermund PM, Marijnissen AC, et al. . Joint distraction in treatment of osteoarthritis (II): effects on cartilage in a canine model. Osteoarthritis Cartilage 2000;8:1–8. 10.1053/joca.1999.0263 [DOI] [PubMed] [Google Scholar]
- 18. Chen Y, Sun Y, Pan X, et al. . Joint distraction attenuates osteoarthritis by reducing secondary inflammation, cartilage degeneration and subchondral bone aberrant change. Osteoarthritis Cartilage 2015;23:1728–35. 10.1016/j.joca.2015.05.018 [DOI] [PubMed] [Google Scholar]
- 19. Gagala J, Tarczynska M, Gaweda K, et al. . The use of osteochondral allograft with bone marrow-derived mesenchymal cells and hinge joint distraction in the treatment of post-collapse stage of osteonecrosis of the femoral head. Med Hypotheses 2014;83:398–400. 10.1016/j.mehy.2014.07.004 [DOI] [PubMed] [Google Scholar]


